Abstract
Objective:
To determine if unhealthy weight control behaviors or binge eating behaviors among young adults with overweight/obesity are associated with BMI change and cardiometabolic risk at seven-year follow-up.
Methods:
We used longitudinal cohort data from 5,552 young adults with overweight/obesity at baseline (18–24 years) with seven-year follow-up (24–32 years) from the National Longitudinal Study of Adolescent to Adult Health. Baseline predictors were: 1) unhealthy weight control behaviors such as vomiting, fasting, skipping meals, or laxative/diuretic use to lose weight or 2) binge eating behaviors. Participants reporting either unhealthy weight control behaviors or binge eating behaviors were considered to engage in any disordered eating behavior (DEB). Outcomes at seven-year follow-up were BMI change, incident diabetes, incident hypertension, and incident hyperlipidemia.
Results:
Young adults with overweight/obesity reporting unhealthy weight control behaviors at baseline had higher BMI and weight at seven-year follow-up than those without unhealthy weight control behaviors. In regression models adjusting for baseline BMI, race/ethnicity, age, and education, unhealthy weight control behaviors were associated with greater change in BMI in both sexes and binge-eating behavior at baseline was associated with greater odds of incident hyperlipidemia (OR 1.90, 95% CI 1.29–2.79) at seven-year follow-up in males.
Conclusions:
The higher risk for increased BMI (in both males and females) and incident hyperlipidemia (in males) over time in young adults with overweight/obesity who engage in DEBs underscores the need to screen for DEBs in this population and provide referrals and tailored interventions as appropriate.
Keywords: eating behaviors, obesity, overweight, hyperlipidemia, young adult, body mass index
Introduction
By national estimates in the United States, 60.3% of younger adults aged 20–39 have a weight status classified as overweight or obese (Ogden, Carroll, Kit, & Flegal, 2014). Studies have also demonstrated that over 40% of female and over 20% of male young adults engage in disordered eating behaviors (DEBs) (Goldschmidt et al., 2018) including binge-eating behavior or unhealthy weight control behaviors such as vomiting, fasting, skipping meals, and laxative/diuretic use (Stephen, Rose, Kenney, Rosselli-Navarra, & Weissman, 2014). DEBs are associated with poor psychosocial health including increased risk for eating disorders (McKnight Investigators, 2003; Striegel-Moore & Bulik, 2007), alcohol and tobacco use (French, Story, Downes, Resnick, & Blum, 1995), and depression (Neumark-Sztainer, Wall, Larson, Eisenberg, & Loth, 2011).
Longitudinal studies have the ability to determine long-term health consequences of DEBs, but data are limited in young adulthood. Prior longitudinal studies have focused on the adolescent age group and found that dieting in adolescence is associated with future weight gain (Field et al., 2003; Stice, Presnell, Shaw, & Rohde, 2005; Viner & Cole, 2006); however, findings have not been consistent across all studies (Klesges, Klem, Epkins, & Klesges, 1991; Tiggemann, 1994). One Minnesota-based longitudinal study found that adolescents using DEBs had increased body mass index (BMI) and a greater risk for being overweight at five-year (Neumark-Sztainer et al., 2006) and 10-year (Neumark-Sztainer, Wall, Story, & Standish, 2012) follow-up. The association between DEBs and cardiometabolic risk has not been well studied, particularly in the context of young adults with overweight/obesity. Young adulthood represents an under-researched developmental period that is distinct from adolescence (Stroud, Walker, Davis, & Irwin, 2015) during which persons can begin to develop cardiometabolic risk factors (Skinner, Perrin, Moss, & Skelton, 2015). Young adults have a worse health profile and are less likely to eat breakfast, exercise, and get regular physical and dental checkups than adolescents (Stroud et al., 2015).
The present study aims to fill the gap in scientific knowledge on the longitudinal effects of DEBs in young adulthood. The objective of this study is to determine the association in a large national sample of young adults with overweight/obesity between DEBs, BMI gain, and increased cardiometabolic risk at seven-year follow-up. We specifically examined associations with incident diabetes, hypertension, and hyperlipidemia.
Methods
Sample
We used data from the National Longitudinal Study of Adolescent to Adult Health (Add Health), a longitudinal cohort study of a nationally representative sample of adolescents in the United States who were followed into adulthood (Harris et al., July 2017). The original adolescent sample (1994–1995, 11–18 years old, Wave I) used systematic sampling methods and implicit stratification to ensure that the high schools (n=80) and middle schools (n=52) were representative of US schools with respect to region of country, urbanicity, size, type, and ethnicity. There have been five waves of data collection, which is coordinated by the Carolina Population Center. For this study, we used restricted-use data from Wave III (defined as baseline for this study), collected from 2001 to 2002 when subjects were 18–24 years old, and Wave IV (defined as seven-year follow-up for this study), collected in 2008 when subjects were 24–32 years old. Wave III was the only wave that collected detailed information about DEBs, and Wave IV was the only wave that collected laboratory data for diabetes and cholesterol. Further details about the study design can be found elsewhere (Harris et al., 2017). The University of North Carolina Institutional Review Board approved all Add Health study procedures, and the University of California, San Francisco Institutional Review Board deemed this specific project exempt.
We included all young adults in Add Health with overweight or obesity at baseline. We excluded young adults who were missing data for the outcomes including BMI change, incident diabetes, hypertension, and hyperlipidemia (n=1,350). We also excluded women who were pregnant at seven-year follow-up (n=188) since this could affect their BMI change and other laboratory measurements.
Procedures
At baseline and seven-year follow-up, an interviewer traveled to the home or another suitable location for the research subject. Written informed consent was obtained from the subject. Interviews lasted approximately 90 minutes. Computer-assisted self-interview technology was used by participants to answer potentially sensitive questions. At seven-year follow-up, immediately following the interview, interviewers took physical measurements and collected biological specimens.
Measures
Baseline measures
Unhealthy weight control behaviors:
Individuals who self-reported behaviors such as, “made yourself vomit, fasted or skipped meals, took laxatives, or diuretics” during the past seven days in order to keep from gaining weight (yes versus no) were coded as having unhealthy weight control behaviors. Exercise and dieting behaviors alone were not considered “unhealthy” weight control behaviors. Our measurement of unhealthy weight control behaviors mirrors previous studies using Add Health data (see Stephen et al., 2014; Tabler & Utz, 2015). These questions were adapted from validated eating behavior measures such as in the Adolescent Health Survey and similar to Project Eating Among Teens (85% agreement ≥1 behavior, r=0.76) (Neumark-Sztainer, Story, Resnick, & Blum, 1998; Neumark-Sztainer, 2010), except that the time frame was seven days to be consistent with the seven day time frame of other validated questions in the Add Health survey on nutrition and physical activity.
Binge-eating behaviors:
Individuals who self-reported “eaten so much in a short period of time that [they] would have been embarrassed if others had seen them do it” in the past seven days were coded as having binge-eating behavior. This question was adapted from validated eating behavior measures such as in the Adolescent Health Survey and similar to Project Eating Among Teens (89% agreement) (Neumark-Sztainer et al., 1998; Neumark-Sztainer, 2010), except that the time frame was seven days to be consistent with the seven day time frame of other validated questions in the Add Health survey on nutrition and physical activity.
Disordered eating behaviors (DEBs):
Participants who self-reported unhealthy weight control behaviors or binge-eating behaviors in the past seven days were considered to have DEBs.
Seven-year follow-up measures
Incident diabetes:
Respondents were classified as having incident diabetes if they had a fasting glucose ≥ 126 mg/dl, non-fasting glucose ≥ 200 mg/dl, hemoglobin A1c ≥ 6.5% (American Diabetes Association, 2014), self-reported history of diabetes except during pregnancy, or used anti-diabetic medication in the past four weeks at follow-up, and a negative self-reported history of diabetes, except during pregnancy, at baseline.
Incident hypertension:
Incident hypertension was defined as a measured systolic blood pressure ≥140 mmHg or a measured diastolic blood pressure ≥90 mmHg (Chobanian et al., 2003) using the average of two measurements 30 seconds apart from a factory calibrated, Microlife BP3MC1-PC-IB oscillometric blood pressure monitor (MicroLife USA, Inc.; Dunedin, FL) or an affirmative response to the question “have you ever been diagnosed with high blood pressure or hypertension” at follow-up, and a negative response to the question “have you ever been diagnosed with high blood pressure or hypertension” at baseline.
Incident hyperlipidemia:
Incident hyperlipidemia was defined as total cholesterol decile corresponding to the proportion of young adults with total cholesterol ≥240 mg/dL in the National Health and Nutrition Examination Surveys (Gooding et al., 2016; Shay et al., 2012) or an affirmative response to the question “have you ever been diagnosed with high cholesterol, triglycerides, or lipids” at follow-up, and a negative response to the question “have you ever been diagnosed with high cholesterol, triglycerides, or lipids” at baseline.
Measured at both baseline and seven-year follow-up
Body mass index (BMI) was calculated using the standard formula weight (kilograms) divided by height (meters) squared (BMI = weight/height2). Weight (Health-o-meter 844KL High Capacity Digital Bathroom Scale; Jarden Corporation; Rye, NY) and height (Carpenter’s square, steel tape measure) were measured by the interviewer. Self-reported height or weight was used if not measured by the interviewer (n=712). Change in BMI was defined as BMI at seven-year follow-up subtracted from baseline BMI.
Weight status:
Young adults with underweight (BMI <18.5), normal weight (18.5 ≤ BMI < 25), overweight (25 ≤ BMI < 30), or obesity (BMI ≥ 30), including severe obesity (BMI ≥ 40), were classified in accordance with guidelines from the US Centers for Disease Control and Prevention (Centers for Disease Control (CDC)., 2012).
Covariates
Age and sex were based on self-report.
Race/ethnicity was based on self-report, based on the categories created by the Add Health survey design: non-Hispanic White; non-Hispanic Black/African American; Hispanic/Latino; non-Hispanic Asian or Pacific Islander; American Indian/Native American; or other.
Education was based on self-report and dichotomized into high school or less versus more than high school, similar to other large population-based studies in young adults (Hudson, Puterman, Bibbins-Domingo, Matthews, & Adler, 2013; Wang et al., 2009). Of socioeconomic markers (i.e., education, income, and occupation) education is found to be most robustly associated with a variety of mental and physical health outcomes. For this reason, education is often the standard socioeconomic proxy utilized in epidemiological studies (Araya, Lewis, Rojas, & Fritsch, 2003; Geyer, Hemstrom, Peter, & Vagero, 2006; Winkleby, Jatulis, Frank, & Fortmann, 1992) including in young adults (Hudson et al., 2013; Wang et al., 2009) and in eating disorders (Hay, Girosi, & Mond, 2015; Tabler & Utz, 2015).
Statistical analysis
Data analysis was performed in 2017 using STATA 15.0. Given sex differences in the presentation of DEBs (Murray et al., 2017; Murray, Accurso, Griffiths, & Nagata, 2018), all analyses were stratified by sex. We compared unadjusted differences in outcomes at seven-year follow-up by baseline presence and absence of DEBs using independent samples t-tests for continuous variables and Chi-square tests for categorical variables. We assessed the association between DEBs and cardiometabolic risk at seven-year follow-up using regression models, adjusting for potential confounding variables. Linear regression analysis was used to identify the association between change in BMI as the continuous dependent variable, and 1) unhealthy weight control behaviors, 2) binge-eating behaviors, or 3) either unhealthy weight control behaviors or binge-eating behaviors (defined as DEBs) as the independent variables, adjusting for race/ethnicity, age, baseline BMI, and education. Logistic regression analysis was used to identify associations with incident diabetes, incident hypertension, and incident hyperlipidemia as the dependent variables, and DEBs, unhealthy weight control behaviors, or binge-eating behavior as the independent variables, adjusting for race/ethnicity, age, baseline BMI, and education. DEBs that were significantly associated with cardiometabolic outcomes after adjusting for the prior covariates were also adjusted for change in BMI (in addition to baseline BMI). In a sensitivity analysis, we performed multiple imputation of missing outcome data at seven-year follow-up (Sterne et al., 2009). P<0.05 was considered statistically significant.
Results
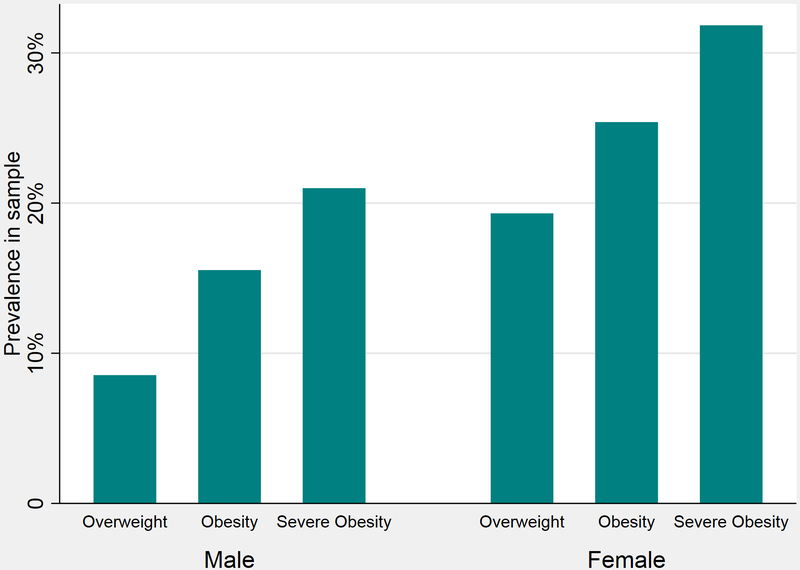
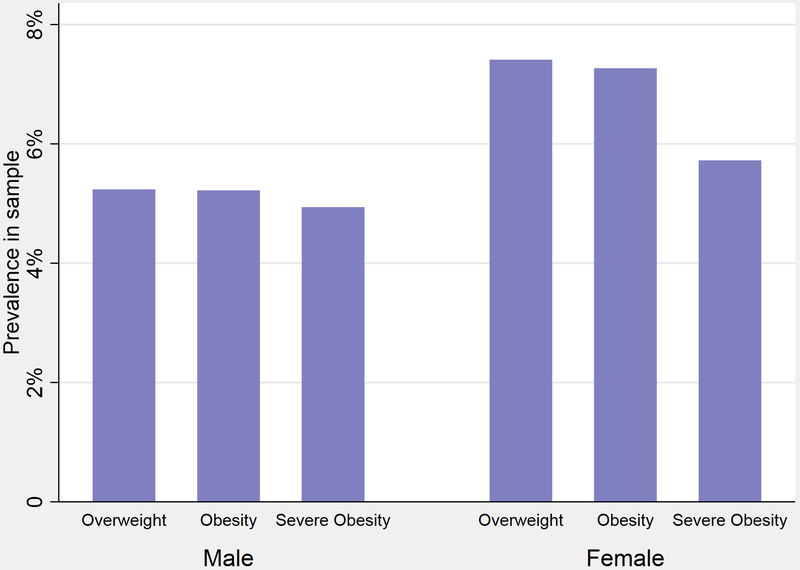
Overall, 5,552 of 7,444 eligible young adults with overweight/obesity at baseline met inclusion criteria (Online Appendix A). Baseline demographic and health characteristics of the young adults included in the sample are presented in Table 1, by sex and absence or presence of DEBs. Overall, 23% reported DEBs, with 17.6% reporting unhealthy weight control behaviors to lose weight and 7.9% reporting binge-eating behaviors. Young adults with overweight/obesity reporting DEBs at baseline had higher BMI and higher weight at baseline than those without DEBs in both males and females. The prevalence of DEBs by weight status is shown in Figure 1 (unhealthy weight control behaviors) and Figure 2 (binge-eating behaviors). Persons of non-White race/ethnicity make up a majority of young men and women who engage in DEBs.
Table 1.
Baseline demographic, health, and eating behavior characteristics of sample, by sex and absence or presence of baseline disordered eating behaviors (DEB)
| na | Total |
Males |
Females |
|||||
|---|---|---|---|---|---|---|---|---|
|
|
No DEB at baseline |
DEB at baseline |
p | No DEB at baseline |
DEB at baseline |
p | ||
| N | 5,552 | 2,269 | 456 | 2,003 | 824 | |||
| Demographic characteristics | Mean ± SD / % | Mean ± SD / % | Mean ± SD / % | Mean ± SD / % | Mean ± SD / % | |||
| Age | 5,552 | 21.92 ± 1.78 | 22.23 ± 1.76 | 22.24 ± 1.75 | 0.906b | 21.94 ± 1.71 | 21.99 ± 1.76 | 0.461b |
| Race/ethnicity | 5,548 | 0.001c | 0.129c | |||||
| White (non-Hispanic) | 57.5% | 58.0% | 48.3% | 53.8% | 49.2% | |||
| Black/African American (non-Hispanic) | 20.0% | 16.1% | 19.5% | 25.7% | 26.2% | |||
| Hispanic/Latino | 15.2% | 18.4% | 19.7% | 15.6% | 17.7% | |||
| Asian/Pacific Islander (non-Hispanic) | 6.0% | 5.9% | 10.1% | 3.4% | 4.3% | |||
| American Indian/Native American | 0.5% | 0.6% | 0.9% | 0.8% | 1.1% | |||
| Other | 0.8% | 1.1% | 1.5% | 0.8% | 0.4% | |||
| Education | 5,548 | 0.103c | 0.030c | |||||
| High school or less | 54.2% | 52.8% | 48.6% | 51.4% | 47.1% | |||
| More than high school | 45.8% | 47.2% | 51.4% | 48.6% | 52.9% | |||
| Health characteristics | ||||||||
| Body mass index (BMI), kg/m2 | 5,552 | 31.29 ± 5.64 | 30.22 ± 4.91 | 31.70 ± 5.47 | <0.001b | 31.75 ± 5.89 | 32.89 ± 6.42 | <0.001b |
| BMI classification | 5,552 | <0.001c | <0.001c | |||||
| Overweight (25 ≤ BMI < 30) | 53.0% | 60.9% | 48.7% | 49.8% | 41.1% | |||
| Obese (BMI ≥ 30) | 47.0% | 39.1% | 51.3% | 50.2% | 58.9% | |||
| Weight, kg | 5,552 | 91.43 ± 19.00 | 96.26 ± 17.93 | 100.20 ± 19.23 | <0.001b | 85.16 ± 17.81 | 88.51 ± 18.99 | <0.001b |
| Diabetes diagnosis, self-report | 5,552 | 1.5% | 0.6% | 1.3% | 0.081c | 1.9% | 3.0% | 0.063c |
| Hypertension diagnosis, self-report | 5,552 | 8.7% | 6.8% | 12.1% | <0.001c | 9.1% | 10.9% | 0.135c |
| Hyperlipidemia, self-report | 5,552 | 5.5% | 5.3% | 7.5% | 0.063c | 4.7% | 6.9% | 0.014c |
| Eating behaviors, self-report (whole cohort) | ||||||||
| Unhealthy weight control behavior (UWCB) | 5,552 | 17.6% | 11.4%d | 23.3%e | ||||
| Binge-eating behavior | 5,552 | 6.2% | 5.2%d | 7.2%e | ||||
| Disordered eating behavior (DEB = UWCB or binge) | 5,552 | 22.0% | 15.8%d | 28.0%e | ||||
SD = standard deviation
Group n may not sum to total N because of missing data
Independent samples T-test
Fisher's exact test
Percentage among all included males
Percentage among all included females
Figure 1.
Prevalence of unhealthy weight control behaviors among young adults with overweight/obesity from the National Longitudinal Study of Adolescent to Adult Health, by weight status
Figure 2.
Prevalence of binge-eating behaviors among young adults with overweight/obesity from the National Longitudinal Study of Adolescent to Adult Health, by weight status
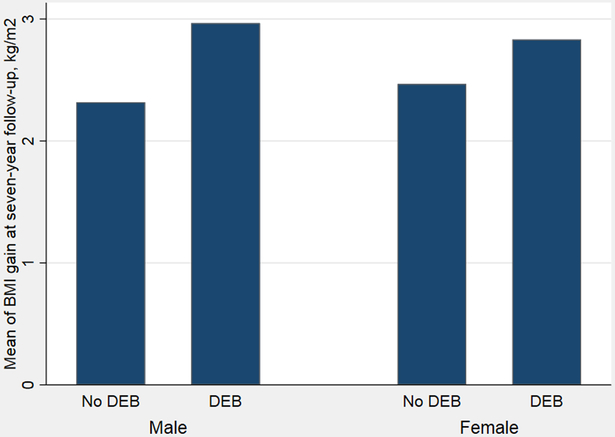
Unadjusted comparisons of cardiometabolic outcomes at seven-year follow-up by presence or absence of baseline DEBs are presented in Table 2. Male young adults with overweight/obesity reporting DEBs at baseline had greater BMI increase than males without DEBs at baseline (2.97 kg/m2 versus 2.32 kg/m2, p=0.005, Figure 3) in unadjusted comparisons. Female young adults with overweight/obesity reporting DEBs at baseline had greater BMI increase than females without DEBs at baseline; however, the difference was not statistically significant in unadjusted comparisons (2.83 kg/m2 versus 2.47 kg/m2, p=0.108). There were no statistically significant differences in incident diabetes, hypertension, or hyperlipidemia by presence or absence of baseline DEBs in males or females in unadjusted comparisons.
Table 2.
Comparison of health outcomes at seven-year follow-up among young adults with overweight/obesity, by sex and absence or presence of baseline disordered eating behaviors (DEB)
| Males |
Females |
|||||
|---|---|---|---|---|---|---|
| No DEB at baseline |
DEB at baseline |
p | No DEB at baseline |
DEB at baseline |
p | |
| N | 2,295 | 430 | 2,036 | 791 | ||
| Health outcomes at seven-year follow up (24-32 years old) | Mean ± SD / % | Mean ± SD / % | Mean ± SD / % | Mean ± SD / % | ||
| Body mass index (BMI), kg/m2 | 32.56 ± 6.34 | 34.67 ± 7.12 | <0.001a | 34.25 ± 7.27 | 35.69 ± 8.20 | <0.001a |
| Body mass index (BMI) change, kg/m2 | 2.32 ± 4.25 | 2.97 ± 5.20 | 0.005a | 2.47 ± 5.26 | 2.83 ± 5.80 | 0.108a |
| BMI classification | <0.001b | <0.082b | ||||
| Underweight (BMI <18.5) | 0.0% | 0.0% | 0.1% | 0.0% | ||
| Normal weight (18.5 ≤ BMI < 25) | 4.9% | 2.6% | 6.5% | 5.2% | ||
| Overweight (25 ≤ BMI < 30) | 34.3% | 25.1% | 24.7% | 21.5% | ||
| Obese (BMI ≥ 30) | 60.8% | 72.3% | 68.7% | 73.3% | ||
| Weight, kg | 102.58 ± 21.42 | 108.32 ± 23.92 | <0.001a | 91.59 ± 20.92 | 95.75 ± 22.85 | <0.001a |
| Weight change, kg | 6.33 ± 12.54 | 7.86 ± 14.87 | 0.024a | 6.35 ± 13.45 | 7.31 ± 14.50 | 0.093a |
| Incident diabetes (self-report or HbA1c ≥ 6.5)c | 8.7% | 11.6% | 0.051d | 9.7% | 11.8% | 0.110d |
| Incident hypertension (self-report or SBP≥140 or DBP≥90)c |
35.4% | 34.2% | 0.634d | 19.4% | 19.7% | 0.847d |
| Incident hyperlipidemia (self-report or total cholesterol≥240)c |
17.2% | 20.2% | 0.126d | 14.6% | 14.8% | 0.890d |
SD = standard deviation
Independent samples T-test
Fisher's exact test
Baseline information based on self-report only
Pearson's chi square test
Figure 3.
Mean body mass index gain at seven-year follow-up among young adults with overweight/obesity from the National Longitudinal Study of Adolescent to Adult Health, by sex and baseline disordered eating behavior (DEB)
Unadjusted comparisons of cardiometabolic outcomes at seven-year follow-up by presence or absence of baseline unhealthy weight control behaviors are presented in Table 3. Young adults with overweight/obesity reporting unhealthy weight control behaviors had greater BMI gain and higher rates of incident diabetes than those without unhealthy weight control behaviors in unadjusted comparisons. There were no statistically significant differences in incident hypertension or hyperlipidemia by presence or absence of baseline unhealthy weight control behaviors in males or females in unadjusted comparisons.
Table 3.
Comparison of health outcomes at seven-year follow-up among young adults with overweight/obesity, by sex and absence or presence of baseline unhealthy weight control behaviors (UWCB) or binge-eating behaviors
| Males |
Females |
|||||
|---|---|---|---|---|---|---|
| No UWCB at baseline |
UWCB at baseline |
p | No UWCB at baseline |
UWCB at baseline |
p | |
| Health outcomes at seven-year follow up (24-32 years old) | Mean ± SD / % | Mean ± SD / % | Mean ± SD / % | Mean ± SD / % | ||
| Body mass index (BMI) change, kg/m2 | 3.07 ± 4.97 | 2.33 ± 4.33 | 0.005a | 2.42 ± 5.23 | 3.05 ± 5.96 | 0.010a |
| Incident diabetes (self-report or HbA1c ≥ 6.5)b | 8.7% | 12.5% | 0.026c | 9.5% | 12.9% | 0.011c |
| Incident hypertension (self-report or SBP≥140 or DBP≥90)b | 35.2% | 34.3% | 0.962c | 19.1% | 19.5% | 0.384c |
| Incident hyperlipidemia (self-report or total cholesterol≥240)b | 17.6% | 17.8% | 0.936c | 14.3% | 15.8% | 0.336c |
| No binge eating at baseline |
Binge eating at baseline |
p | No binge eating at baseline |
Binge eating at baseline |
p | |
| Body mass index (BMI) change, kg/m2 | 2.40 ± 4.34 | 2.82 ± 5.57 | 0.266a | 2.56 ± 5.43 | 2.74 ± 5.21 | 0.635a |
| Incident diabetes (self-report or HbA1c ≥ 6.5)b | 9.1% | 10.6% | 0.546c | 10.2% | 10.4% | 0.110c |
| Incident hypertension (self-report or SBP≥140 or DBP≥90)b | 35.4% | 31.0% | 0.284c | 19.8% | 15.8% | 0.172c |
| Incident hyperlipidemia (self-report or total cholesterol≥240)b | 17.1% | 28.2% | 0.001c | 14.8% | 12.4% | 0.341c |
SD = standard deviation
Independent samples T-test
Baseline information based on self-report only
Pearson's chi square test
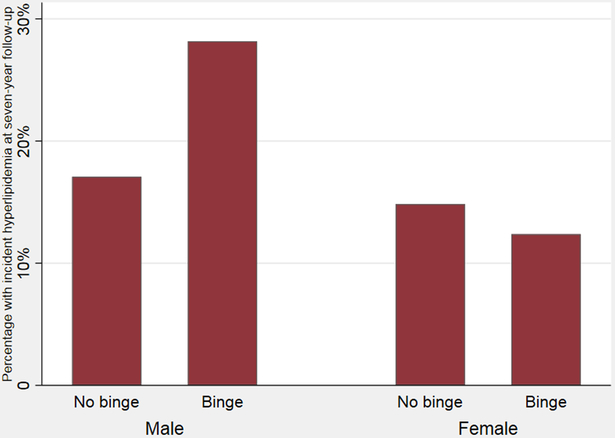
Unadjusted comparisons of cardiometabolic outcomes at seven-year follow-up by presence or absence of binge-eating behaviors are presented at the bottom of Table 3. There were no statistically significant differences in BMI gain, incident diabetes, or incident hypertension by presence or absence of baseline binge-eating behaviors in males or females in unadjusted comparisons. In unadjusted comparisons for BMI, 28.2% of males reporting binge-eating behavior had incident hyperlipidemia compared to 17.1% males who did not report binge-eating behavior (Pearson chi square 11.38, p=0.001, Figure 4). There were no statistically significant differences in incident hyperlipidemia by presence or absence of baseline binge-eating behaviors in females in unadjusted comparisons for BMI.
Figure 4.
Incident hyperlipidemia at seven-year follow-up among young adults with overweight/obesity from the National Longitudinal Study of Adolescent to Adult Health, by sex and baseline binge-eating behavior
Regression models with type of disordered eating behavior as the independent variable and cardiometabolic risk as the dependent variable, adjusted for baseline BMI, race/ethnicity, age, and education, are presented in Table 4. In linear regression models, unhealthy weight control behaviors and any disordered eating behavior but not binge-eating behaviors at baseline were associated with greater BMI increase in males and females at seven-year follow-up, adjusting for baseline BMI, race/ethnicity, age, and education (Table 4). In adjusted logistic regression models, there was no statistically significant association between unhealthy weight control behaviors, binge-eating behavior, or any DEB, and incident diabetes. In adjusted logistic regression models, there was no statistically significant association between unhealthy weight control behaviors, binge-eating behavior, or any DEB, and incident hypertension. In logistic regression models, binge-eating behavior at baseline was associated with greater odds of incident hyperlipidemia in males (OR 1.90, 95% confidence interval 1.29–2.79) but not in females (OR 0.81, 95% CI 0.52–1.24) at seven-year follow-up, adjusting for baseline BMI, age, race/ethnicity, and education (Table 4). Binge-eating behavior at baseline remained associated with greater odds of incident hyperlipidemia in males (OR 1.88, 95% confidence interval 1.28–2.76) at seven-year follow-up, even when adjusting for change in BMI and baseline BMI, in addition to age, race/ethnicity, and education.
Table 4.
Cardiometabolic risk at seven-year follow-up for young adults with overweight/obesity, by sex and type of disordered eating behavior at baseline
| Change in BMI, adjusteda |
Incident diabetes,b adjusteda |
Incident hypertension,b adjusteda |
Incident hyperlipidemia,b adjusteda |
|||||
|---|---|---|---|---|---|---|---|---|
| B (SE)c | p | OR (95% CI)d | p | OR (95% CI)d | p | OR (95% CI)d | p | |
| Males | ||||||||
| Unhealthy weight control behavior (UWCB) | 0.85 (0.26) | 0.001 | 1.11 (0.75 - 1.63) | 0.606 | 0.92 (0.71 - 1.18) | 0.590 | 0.98 (0.72 - 1.34) | 0.912 |
| Binge-eating behavior | 0.43 (0.38) | 0.254 | 1.10 (0.62 - 1.95) | 0.746 | 0.81 (0.56 - 1.17) | 0.130 | 1.90 (1.29 - 2.79) | 0.001 |
| Any disordered eating behavior (UWCB or binge) | 0.72 (0.23) | 0.002 | 1.07 (0.76 - 1.52) | 0.698 | 0.88 (0.71 - 1.10) | 0.268 | 1.20 (0.93 - 1.57) | 0.166 |
| Females | ||||||||
| Unhealthy weight control behavior (UWCB) | 0.80 (0.24) | 0.001 | 1.24 (0.94 - 1.63) | 0.133 | 1.01 (0.80 - 1.26) | 0.962 | 1.12 (0.88 - 1.44) | 0.346 |
| Binge-eating behavior | 0.17 (0.39) | 0.656 | 1.02 (0.63 - 1.65) | 0.934 | 0.77 (0.52 - 1.14) | 0.192 | 0.81 (0.52 - 1.24) | 0.329 |
| Any disordered eating behavior (UWCB or binge) | 0.51 (0.22) | 0.024 | 1.10 (0.84 - 1.44) | 0.484 | 0.95 (0.77 - 1.17) | 0.610 | 1.01 (0.80 - 1.28) | 0.935 |
Bold indicates p<0.05
Analyses are adjusted for baseline BMI, race/ethnicity, age, and education
Baseline information based on self-report only
B = Estimated coefficient from linear regression; SE = standard error
OR = odds ratio from logistic regression; CI = confidence interval
The full regression models for the unhealthy weight control or binge-eating behaviors that had statistically significant associations with cardiometabolic outcomes are listed in Appendix B. Black/African American race/ethnicity was associated with greater change in BMI in males (B=0.52, p=0.027) and females (B=1.11, p<0.001) but protective of incident hyperlipidemia in males (OR 0.74, 95% CI 0.55–1.00) in models adjusting for DEBs, education, age, and baseline BMI. In a sensitivity analysis (not shown), results with multiple imputation of missing outcome data were consistent with results that excluded missing outcome data.
Discussion
We find that young adults with overweight/obesity gain weight, regardless of whether or not they engage in DEBs, but engaging in DEBs at baseline is associated with greater BMI increase at seven-year follow-up in adjusted analyses. In particular, engagement in vomiting, fasting, skipping meals, or using diuretics/laxatives to lose weight were the DEBs that were specifically associated with higher BMI seven years later, not binge eating. These findings are important because many young adults engage in DEBs with the intention to lose weight in the long term. Furthermore, we find that young adult males with overweight/obesity who report binge-eating behaviors have greater odds of incident hyperlipidemia than those who do not report binge-eating behaviors. Identifying young adults who engage in these DEBs and providing interventions and referrals for support may therefore be important for their future adult health.
Although previous longitudinal studies have shown that dieting and DEBs in adolescence may be predictive of weight gain in most (Neumark-Sztainer et al., 2006; Neumark-Sztainer et al., 2012; Stice et al., 2005; Viner & Cole, 2006) but not all (Klesges et al., 1991; Tiggemann, 1994) studies, these studies have not linked DEBs to cardiometabolic risk in young adulthood. This study examines this question in young adults, an understudied population who have been shown to have a worse health profile and to be less likely to eat breakfast, exercise, and get regular physical and dental checkups than adolescents (Stroud et al., 2015). Finally, we use a large national sample generalizable to young adult populations in the United States.
The mechanisms by which unhealthy weight control behaviors lead to weight gain may be multifactorial (Dulloo, Jacquet, Montani, & Schutz, 2015). Studies have found that unhealthy weight control behaviors themselves contribute to weight gain (Pietilainen, Saarni, Kaprio, & Rissanen, 2012). One study examined monozygotic twin pairs discordant for intentional weight loss, finding that the twin with at least one weight loss episode gained 0.4 kg/m2 greater BMI than their non-dieting sibling at 25 years of age, despite similar baseline BMI levels (Pietilainen et al., 2012). Unhealthy weight control behaviors may themselves predispose to eating disorders, disinhibition, and compensatory eating, leading to weight gain (Neumark-Sztainer, Wall, Haines, Story, & Eisenberg, 2007; Viner & Cole, 2006). Dietary restraint and hunger are known to increase both the incentive salience and reward processing of food, particularly calorically dense foods, which turn can facilitate greater consumption of these foods (Epstein, Truesdale, Wojcik, Paluch, & Raynor, 2003; Siep et al., 2009).
We found that binge-eating behaviors among young adult males with overweight/obesity were associated with incident hyperlipidemia at seven-year follow-up. Binge-eating disorder has been shown to be associated with dyslipidemia in children (Tanofsky-Kraff et al., 2012) and older adults (Hudson et al., 2010; Succurro et al., 2015), but this has not been noted in young adults in non-clinical samples. The greater hyperlipidemia incidence in males but not females who reported binge-eating behavior may be explained by sex differences in eating disorders, DEBs, and cardiometabolic risk (Murray et al., 2017; Murray et al., 2018). Young adult males in the US (Shay et al., 2012) and in this sample have higher rates of hyperlipidemia than females overall. Males are also more likely to have truncal (abdominal) obesity than females, and abdominal obesity has been linked to higher triglycerides (Tresaco et al., 2009). Higher levels of triglycerides and metabolic syndrome have been reported in men compared to women with history of binge-eating disorder (Udo et al., 2013). This was thought to potentially be due to lower treatment seeking behavior in males and more active and earlier attempts to address health and weight status by females (Udo et al., 2013). Finally, since disordered eating is more common in females than males, perhaps the males who reported binge-eating behaviors were overall more disordered than the females who reported these behaviors (Murray et al., 2017). Better understanding the etiologies of sex differences in eating disorders and cardiometabolic risk is an important area of future research.
We found higher rates of diabetes in young adults with overweight/obesity reporting unhealthy weight control behaviors compared to those not reporting unhealthy weight control behaviors in comparisons not adjusted for BMI. However, this relationship was no longer significant after adjusting for BMI. Prior studies in middle-aged men and women found that the association between weight cycling and diabetes was no longer significant after adjustment for overall weight status (Field et al., 2004; Waring, Eaton, Lasater, & Lapane, 2010). While the effects of the eating behavior on diabetes may be explained by the greater weight gain in these individuals, it is unclear if there is a direct impact on worsening insulin resistance and degradation of beta cell secretory capacity.
We did not see an association between binge-eating behavior and diabetes or hypertension that has been reported in an older adult (mean age 47 years) sample with binge-eating disorder (Hudson et al., 2010), possibly because 1) our sample was much younger and may develop more cardiometabolic risk later in life, 2) other studies examined clinical samples with binge-eating disorder whereas ours was a community sample with self-reported binge-eating behavior (but not binge-eating disorder), and 3) the seven-day timeframe may have been too short to develop cardiometabolic risk. Future research may examine the effect of DEBs over a longer time period on cardiometabolic risk. It is also possible that due to publication bias other studies with negative findings have not been published.
We found that Black/African American race/ethnicity was associated with greater BMI gain but protective of incident hyperlipidemia in males at seven-year follow-up. A larger proportion of Black/African American younger adults (ages 20–39) live with obesity but a smaller proportion have hyperlipidemia compared to White younger adults in the National Health and Nutrition Examination Surveys (Shay et al., 2012). We also found that persons of non-White race/ethnicity make up a majority of young adult men and women who engage in DEBs and may be important populations for screening and future research.
Given that DEBs are associated with important health consequences such as weight gain and hyperlipidemia in males, health care providers should screen for and discourage these practices particularly in adolescent and young adult populations. This is especially important as recent studies suggest that clinicians often overlook screening for DEBs, especially among young adults with overweight/obesity (Goldschmidt, Wall, Loth, & Neumark-Sztainer, 2015). Overweight/obesity and DEBs are often studied and treated separately as contrasting entities at opposite ends of the weight spectrum; however, DEBs are actually more common among adolescents and young adults with overweight/obesity compared to young adults with normal weight (Neumark-Sztainer et al., 2007). The American Academy of Pediatrics has recently published guidelines on preventing both obesity and eating disorders in adolescents, recommending discouraging DEBs, promoting a positive body image, encouraging more frequent family meals, encouraging families not to talk about weight but rather healthy eating, inquiring about a history of mistreatment or bullying, and carefully monitoring weight loss in an adolescent who needs to lose weight (Golden et al., 2016). However, we are unaware of similar guidelines specifically for young adults.
Our study has several limitations that merit acknowledgement. Objective cardiometabolic measures were not collected at baseline; therefore, some subjects may have had hypertension, diabetes, or hyperlipidemia at baseline but been unaware of these diagnoses and therefore unable to self-report a previous diagnosis. However, we did have baseline and follow-up BMI and some young adults did have self-reported hypertension, diabetes, or hyperlipidemia at baseline that had been diagnosed by a physician. Total cholesterol was recorded in deciles, but we used procedures established by other Add Health investigators that corresponded to total cholesterol ≥240 mg/dL (Gooding et al., 2016). We only had blood pressure measurement from one day at seven-year follow-up, whereas three would be required for a medical diagnosis of hypertension. There was the possibility for selection bias since we excluded subjects with missing data on the outcome measures (n=1,350) or due to pregnancy (n=188). Although there were no statistically significant differences in age or baseline cardiometabolic measures of those included versus excluded (Appendix A), a higher proportion of White subjects compared to Black/African American or Hispanic/Latino subjects and subjects with higher education compared to lower education (in males) were retained. This is a substantial limitation given that these data included a large portion of the racial/ethnic diversity in the sample. However, we performed a sensitivity analysis (not shown) and found consistent results when using multiple imputation versus exclusion of missing outcome data. While there are many strengths of longitudinal surveys, one pervasive issue is that of attrition, which was the primary driver of missing data at time of follow-up (outcome measures). Self-reported height or weight was used in 712 subjects (13% of sample); however the correlation between self-reported height and weight and clinician-administered measures is 0.98–0.99 in general population samples (Pursey, Burrows, Stanwell, & Collins, 2014). Due to the design of the Add Health survey, we were unable to measure the severity or duration of reported DEBs. DEBs were based on self-report, a method that is may be subject to reporting bias. The timeframe used for measuring DEBs in Add Health was shorter (past seven days) than is often asked in other measures of DEBs such as the Eating Disorder Examination Questionnaire (past 28 days) (Fairburn & Beglin, 2008), which may have underestimated the prevalence of DEBs compared to other measures. Although “overweight” and “obesity” are based on definitions from the CDC, these terms may be considered stigmatizing.
Nonetheless, the limitations were offset by several strengths. The study used national longitudinal data with over 5,000 young adults in the community, and therefore did not contain limitations inherent to studies of clinical samples. We used objective measures of the outcomes via direct measurement of laboratory, blood pressure, and anthropometric data.
Conclusion
We find that despite their efforts to lose weight, young adults with overweight/obesity who engage in vomiting, fasting, skipping meals, or using diuretics/laxatives to lose weight are likely to gain weight in the long-run, and binge-eating behaviors are associated with greater odds of incident hyperlipidemia in males. Given that DEBs are associated with serious medical consequences, health care providers should screen for and discourage these practices in young adults. This is particularly important given that DEBs may be under detected in young adults with overweight/obesity. Future research may compare the association between DEBs and cardiometabolic risk in young adults with normal weight versus overweight/obesity and explore what interventions may prevent the onset of both obesity and eating disorders, promoting healthful eating as a long-term lifestyle behavior.
Supplementary Material
Acknowledgments:
Thanks to Nicole Capdarest-Arest for help with literature searches and Holly Gooding and Carly Milliren for help with interpretation of cholesterol data. This research uses data from Add Health, a program project directed by Kathleen Mullan Harris and designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill, and funded by grant P01-HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with cooperative funding from 23 other federal agencies and foundations. Special acknowledgment is due Ronald R. Rindfuss and Barbara Entwisle for assistance in the original design. Information on how to obtain the Add Health data files is available on the Add Health website (http://www.cpc.unc.edu/addhealth). No direct support was received from grant P01-HD31921 for this analysis.
Funding source: Dr. Nagata is a fellow in the Pediatric Scientist Development Program (K12HD00085033), with funding from the American Academy of Pediatrics, the American Pediatric Society, and the Norman Schlossberger Research Fund from the University of California, San Francisco. Dr. Garber was supported by NIH 5R01HD082166–02. Dr. Murray was supported by NIH K23 MH115184.
Footnotes
Disclosure: The authors declared no conflict of interest.
References
- American Diabetes Association. (2014). Diagnosis and classification of diabetes mellitus. Diabetes Care, 37 Suppl 1, S81–90. doi: 10.2337/dc14-S081 [doi] [DOI] [PubMed] [Google Scholar]
- Araya R, Lewis G, Rojas G, & Fritsch R (2003). Education and income: Which is more important for mental health? Journal of Epidemiology and Community Health, 57(7), 501–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control (CDC). (April 27, 2012). Defining adult overweight and obesity. (). Retrieved from http://www.cdc.gov/obesity/adult/defining.html [Google Scholar]
- Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, . . . National High Blood Pressure Education Program Coordinating Committee. (2003). The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: The JNC 7 report. Jama, 289(19), 2560–2572. doi: 10.1001/jama.289.19.2560 [doi] [DOI] [PubMed] [Google Scholar]
- Dulloo AG, Jacquet J, Montani JP, & Schutz Y (2015). How dieting makes the lean fatter: From a perspective of body composition autoregulation through adipostats and proteinstats awaiting discovery. Obesity Reviews : An Official Journal of the International Association for the Study of Obesity, 16 Suppl 1, 25–35. doi: 10.1111/obr.12253 [doi] [DOI] [PubMed] [Google Scholar]
- Epstein LH, Truesdale R, Wojcik A, Paluch RA, & Raynor HA (2003). Effects of deprivation on hedonics and reinforcing value of food. Physiology & Behavior, 78(2), 221–227. doi:S0031938402009782 [pii] [DOI] [PubMed] [Google Scholar]
- Fairburn CG, & Beglin S (2008). Eating disorder examination questionnaire In Fairburn CG (Ed.), Cognitive behavior therapy and eating disorders (pp. 309–313). New York: Guilford Press. [Google Scholar]
- Field AE, Austin SB, Taylor CB, Malspeis S, Rosner B, Rockett HR, . . . Colditz GA (2003). Relation between dieting and weight change among preadolescents and adolescents. Pediatrics, 112(4), 900–906. [DOI] [PubMed] [Google Scholar]
- Field AE, Manson JE, Laird N, Williamson DF, Willett WC, & Colditz GA (2004). Weight cycling and the risk of developing type 2 diabetes among adult women in the united states. Obesity Research, 12(2), 267–274. doi: 10.1038/oby.2004.34 [doi] [DOI] [PubMed] [Google Scholar]
- French SA, Story M, Downes B, Resnick MD, & Blum RW (1995). Frequent dieting among adolescents: Psychosocial and health behavior correlates. American Journal of Public Health, 85(5), 695–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geyer S, Hemstrom O, Peter R, & Vagero D (2006). Education, income, and occupational class cannot be used interchangeably in social epidemiology. empirical evidence against a common practice. Journal of Epidemiology and Community Health, 60(9), 804–810. doi:60/9/804 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golden NH, Schneider M, Wood C, COMMITTEE ON NUTRITION, COMMITTEE ON ADOLESCENCE, & SECTION ON OBESITY. (2016). Preventing obesity and eating disorders in adolescents. Pediatrics, 138(3), 10.1542/peds.2016–1649. Epub 2016 Aug 22. doi: 10.1542/peds.2016-1649 [doi] [DOI] [PubMed] [Google Scholar]
- Goldschmidt AB, Wall MM, Choo TJ, Evans EW, Jelalian E, Larson N, & Neumark-Sztainer D (2018). Fifteen-year weight and disordered eating patterns among community-based adolescents. American Journal of Preventive Medicine, 54(1), e21–e29. doi:S0749-3797(17)30496-8 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldschmidt AB, Wall MM, Loth KA, & Neumark-Sztainer D (2015). Risk factors for disordered eating in overweight adolescents and young adults. Journal of Pediatric Psychology, 40(10), 1048–1055. doi: 10.1093/jpepsy/jsv053 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gooding HC, Milliren C, Shay CM, Richmond TK, Field AE, & Gillman MW (2016). Achieving cardiovascular health in young adulthood-which adolescent factors matter? The Journal of Adolescent Health : Official Publication of the Society for Adolescent Medicine, 58(1), 119–121. doi: 10.1016/j.jadohealth.2015.09.011 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris KM, Halpern CT, Witsel E, Hussey J, Tabor J, Entzel P, & Udry JR (July 2017). The national longitudinal study of adolescent to adult health: Research design. (). Retrieved from http://www.cpc.unc.edu/projects/addhealth/design [Google Scholar]
- Hay P, Girosi F, & Mond J (2015). Prevalence and sociodemographic correlates of DSM-5 eating disorders in the australian population. Journal of Eating Disorders, 3, 19–015-0056–0. eCollection 2015. doi: 10.1186/s40337-015-0056-0 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudson DL, Puterman E, Bibbins-Domingo K, Matthews KA, & Adler NE (2013). Race, life course socioeconomic position, racial discrimination, depressive symptoms and self-rated health. Social Science & Medicine (1982), 97, 7–14. doi: 10.1016/j.socscimed.2013.07.031 [doi] [DOI] [PubMed] [Google Scholar]
- Hudson JI, Lalonde JK, Coit CE, Tsuang MT, McElroy SL, Crow SJ, . . . Pope HG Jr. (2010). Longitudinal study of the diagnosis of components of the metabolic syndrome in individuals with binge-eating disorder. The American Journal of Clinical Nutrition, 91(6), 1568–1573. doi: 10.3945/ajcn.2010.29203 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klesges RC, Klem ML, Epkins CC, & Klesges LM (1991). A longitudinal evaluation of dietary restraint and its relationship to changes in body weight. Addictive Behaviors, 16(5), 363–368. [DOI] [PubMed] [Google Scholar]
- McKnight Investigators. (2003). Risk factors for the onset of eating disorders in adolescent girls: Results of the McKnight longitudinal risk factor study. The American Journal of Psychiatry, 160(2), 248–254. doi: 10.1176/ajp.160.2.248 [doi] [DOI] [PubMed] [Google Scholar]
- Murray SB, Accurso EC, Griffiths S, & Nagata JM (2018). Boys, biceps, and bradycardia: The hidden dangers of muscularity-oriented disordered eating. The Journal of Adolescent Health : Official Publication of the Society for Adolescent Medicine, 62(3), 352–355. doi:S1054-139X(17)30492-5 [pii] [DOI] [PubMed] [Google Scholar]
- Murray SB, Nagata JM, Griffiths S, Calzo JP, Brown TA, Mitchison D, . . . Mond JM (2017). The enigma of male eating disorders: A critical review and synthesis. Clinical Psychology Review, 57, 1–11. doi:S0272-7358(17)30137-X [pii] [DOI] [PubMed] [Google Scholar]
- Neumark-Sztainer D (2010). Project EAT 2010 and F-EAT surveys - derived variables and scales. Retrieved from http://docs.sph.umn.edu/epich/eat/EAT2010_FEAT_Psychometrics.pdf
- Neumark-Sztainer D, Story M, Resnick MD, & Blum RW (1998). Lessons learned about adolescent nutrition from the minnesota adolescent health survey. Journal of the American Dietetic Association, 98(12), 1449–1456. doi:S0002-8223(98)00329-0 [pii] [DOI] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Wall M, Guo J, Story M, Haines J, & Eisenberg M (2006). Obesity, disordered eating, and eating disorders in a longitudinal study of adolescents: How do dieters fare 5 years later? Journal of the American Dietetic Association, 106(4), 559–568. doi:S0002-8223(06)00004-6 [pii] [DOI] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Wall M, Haines J, Story M, & Eisenberg ME (2007). Why does dieting predict weight gain in adolescents? findings from project EAT-II: A 5-year longitudinal study. Journal of the American Dietetic Association, 107(3), 448–455. doi:S0002-8223(06)02680-0 [pii] [DOI] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Wall M, Larson NI, Eisenberg ME, & Loth K (2011). Dieting and disordered eating behaviors from adolescence to young adulthood: Findings from a 10-year longitudinal study. Journal of the American Dietetic Association, 111(7), 1004–1011. doi: 10.1016/j.jada.2011.04.012 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Wall M, Story M, & Standish AR (2012). Dieting and unhealthy weight control behaviors during adolescence: Associations with 10-year changes in body mass index. The Journal of Adolescent Health : Official Publication of the Society for Adolescent Medicine, 50(1), 80–86. doi: 10.1016/j.jadohealth.2011.05.010 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumark-Sztainer DR, Wall MM, Haines JI, Story MT, Sherwood NE, & van den Berg PA (2007). Shared risk and protective factors for overweight and disordered eating in adolescents. American Journal of Preventive Medicine, 33(5), 359–369. doi:S0749-3797(07)00498-9 [pii] [DOI] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Kit BK, & Flegal KM (2014). Prevalence of childhood and adult obesity in the united states, 2011–2012. Jama, 311(8), 806–814. doi: 10.1001/jama.2014.732 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietilainen KH, Saarni SE, Kaprio J, & Rissanen A (2012). Does dieting make you fat? A twin study. International Journal of Obesity (2005), 36(3), 456–464. doi: 10.1038/ijo.2011.160 [doi] [DOI] [PubMed] [Google Scholar]
- Pursey K, Burrows TL, Stanwell P, & Collins CE (2014). How accurate is web-based self-reported height, weight, and body mass index in young adults? Journal of Medical Internet Research, 16(1), e4. doi: 10.2196/jmir.2909 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shay CM, Ning H, Allen NB, Carnethon MR, Chiuve SE, Greenlund KJ, . . . Lloyd-Jones DM (2012). Status of cardiovascular health in US adults: Prevalence estimates from the national health and nutrition examination surveys (NHANES) 2003–2008. Circulation, 125(1), 45–56. doi: 10.1161/CIRCULATIONAHA.111.035733 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siep N, Roefs A, Roebroeck A, Havermans R, Bonte ML, & Jansen A (2009). Hunger is the best spice: An fMRI study of the effects of attention, hunger and calorie content on food reward processing in the amygdala and orbitofrontal cortex. Behavioural Brain Research, 198(1), 149–158. doi: 10.1016/j.bbr.2008.10.035 [doi] [DOI] [PubMed] [Google Scholar]
- Skinner AC, Perrin EM, Moss LA, & Skelton JA (2015). Cardiometabolic risks and severity of obesity in children and young adults. The New England Journal of Medicine, 373(14), 1307–1317. doi: 10.1056/NEJMoa1502821 [doi] [DOI] [PubMed] [Google Scholar]
- Stephen EM, Rose JS, Kenney L, Rosselli-Navarra F, & Weissman RS (2014). Prevalence and correlates of unhealthy weight control behaviors: Findings from the national longitudinal study of adolescent health. Journal of Eating Disorders, 2, 16–2974-2–16. eCollection 2014. doi: 10.1186/2050-2974-2-16 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sterne JAC, White IR, Carlin JB, Spratt M, Royston P, Kenward MG, . . . Carpenter JR (2009). Multiple imputation for missing data in epidemiological and clinical research: Potential and pitfalls. The BMJ, 338, b2393. doi: 10.1136/bmj.b2393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Presnell K, Shaw H, & Rohde P (2005). Psychological and behavioral risk factors for obesity onset in adolescent girls: A prospective study. Journal of Consulting and Clinical Psychology, 73(2), 195–202. doi:2005-02854-001 [pii] [DOI] [PubMed] [Google Scholar]
- Striegel-Moore RH, & Bulik CM (2007). Risk factors for eating disorders. The American Psychologist, 62(3), 181–198. doi:2007-04834-005 [pii] [DOI] [PubMed] [Google Scholar]
- Stroud C, Walker LR, Davis M, & Irwin CE Jr. (2015). Investing in the health and well-being of young adults. The Journal of Adolescent Health : Official Publication of the Society for Adolescent Medicine, 56(2), 127–129. doi: 10.1016/j.jadohealth.2014.11.012 [doi] [DOI] [PubMed] [Google Scholar]
- Succurro E, Segura-Garcia C, Ruffo M, Caroleo M, Rania M, Aloi M, . . . Arturi F (2015). Obese patients with a binge eating disorder have an unfavorable metabolic and inflammatory profile. Medicine, 94(52), e2098. doi: 10.1097/MD.0000000000002098 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabler J, & Utz RL (2015). The influence of adolescent eating disorders or disordered eating behaviors on socioeconomic achievement in early adulthood. The International Journal of Eating Disorders, 48(6), 622–632. doi: 10.1002/eat.22395 [doi] [DOI] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Shomaker LB, Stern EA, Miller R, Sebring N, Dellavalle D, . . . Yanovski JA (2012). Children’s binge eating and development of metabolic syndrome. International Journal of Obesity (2005), 36(7), 956–962. doi: 10.1038/ijo.2011.259 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiggemann M (1994). Dietary restraint as a predictor of reported weight loss and affect. Psychological Reports, 75(3 Pt 2), 1679–1682. doi: 10.2466/pr0.1994.75.3f.1679 [doi] [DOI] [PubMed] [Google Scholar]
- Tresaco B, Moreno LA, Ruiz JR, Ortega FB, Bueno G, Gonzalez-Gross M, . . . AVENA Study Group. (2009). Truncal and abdominal fat as determinants of high triglycerides and low HDL-cholesterol in adolescents. Obesity (Silver Spring, Md.), 17(5), 1086–1091. doi: 10.1038/oby.2008.626 [doi] [DOI] [PubMed] [Google Scholar]
- Udo T, McKee SA, White MA, Masheb RM, Barnes RD, & Grilo CM (2013). Sex differences in biopsychosocial correlates of binge eating disorder: A study of treatment-seeking obese adults in primary care setting. General Hospital Psychiatry, 35(6), 587–591. doi: 10.1016/j.genhosppsych.2013.07.010 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viner RM, & Cole TJ (2006). Who changes body mass between adolescence and adulthood? factors predicting change in BMI between 16 year and 30 years in the 1970 british birth cohort. International Journal of Obesity (2005), 30(9), 1368–1374. doi:0803183 [pii] [DOI] [PubMed] [Google Scholar]
- Wang EA, Pletcher M, Lin F, Vittinghoff E, Kertesz SG, Kiefe CI, & Bibbins-Domingo K (2009). Incarceration, incident hypertension, and access to health care: Findings from the coronary artery risk development in young adults (CARDIA) study. Archives of Internal Medicine, 169(7), 687–693. doi: 10.1001/archinternmed.2009.26 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waring ME, Eaton CB, Lasater TM, & Lapane KL (2010). Incident diabetes in relation to weight patterns during middle age. American Journal of Epidemiology, 171(5), 550–556. doi: 10.1093/aje/kwp433 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winkleby MA, Jatulis DE, Frank E, & Fortmann SP (1992). Socioeconomic status and health: How education, income, and occupation contribute to risk factors for cardiovascular disease. American Journal of Public Health, 82(6), 816–820. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.