Abstract
Objective
The purpose of this qualitative study was to examine relations between psychological factors, particularly perceived control, and voice symptoms in adults seeking treatment for a voice problem.
Methods
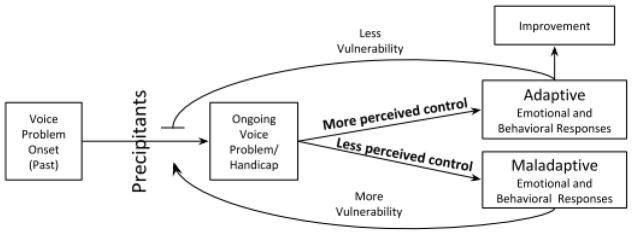
Semi-structured interviews of adult patients with a clinical diagnosis of muscle tension dysphonia were conducted and transcribed. Follow-up interviews were conducted as needed for further information or clarification. A multidisciplinary team analyzed interview content using inductive techniques. Common themes and subthemes were identified. A conceptual model was developed describing the association between voice symptoms, psychological factors, precipitants of ongoing voice symptoms, and perceived control.
Results
Thematic saturation was reached after 23 interviews. No participants reported a direct psychological cause for their voice problem, although half described significant life events preceding voice problem onset (e.g., miscarriage and other health events, interpersonal conflicts, and family members’ illnesses, injuries, and deaths). Participants described psychological influences on voice symptoms that led to rapid exacerbation of their voice symptoms. Participants described the helpfulness of speech therapy and sometimes also challenges of applying techniques in daily life. They also discussed personal coping strategies that included behavioral (e.g., avoiding triggers, seeking social support) and psychological (e.g., mind-body awareness, emotion regulation) components. Voice-related perceived control was associated with adaptive emotional and behavioral responses, which appeared to facilitate symptom improvement.
Conclusions
In this qualitative pilot study, participant narratives suggested that psychological factors and emotions influence voice symptoms, facilitating development of a preliminary conceptual model of how adaptive and maladaptive responses develop and how they influence vocal function.
Keywords: Voice, Dysphonia, Distress, Psychosocial, Perceived control, Psychology, Qualitative study
Introduction
Voice problems are common,1 can be disabling,2 and significantly reduce work productivity3,4 and quality of life.5 Prior work has suggested that psychological factors (such as anxiety, stress, and somatization) and voice problems are associated,6–8 both in patients with a broad range of voice disorders and in those with specific benign voice pathologies such as muscle tension dysphonia. This has led to suggestions that, for some patients, a psychologically oriented approach to treatment may be helpful.7 To take such an approach, a nuanced understanding of these relationships is needed.
Recent studies have shown a meaningful relationship between a psychological construct called perceived control and voice-related handicap.9,10 Present perceived control, the extent to which patients feel they can control their voice problems or their reactions to their voice problems in the present, had a moderate negative relationship with voice-related handicap (measured by the Voice Handicap Index -1011). In addition, perceived control moderated the relation between voice-related handicap and psychosocial distress, such that voice-related handicap and psychosocial distress were more strongly related among those with lower perceived control.9 These studies were primarily cross-sectional and assessed perceived control, distress, and voice-related handicap with structured scales. These studies did not allow for in-depth exploration of patient perspectives on how these factors are related, or of potential complexities in the relationships between these factors.
Prior literature has suggested that psychological factors may precipitate communication disorders (vulnerability model), that communication disorders may lead to psychological distress (disability model), and/or that these two mechanisms may both occur (integrated model).12 It has also been noted that qualitative methodologies have the potential to add insights that are not otherwise obtainable.13 The objective of this study was to elicit patient perceptions on potential mechanistic relationships between psychological factors (perceived control, distress, and emotions) and voice symptoms, using a semi-structured qualitative interview approach. This represents an early step in our efforts to find meaningful patterns in heterogeneous relationships between the complex topics of psychology and voice and propose a preliminary conceptual model describing those relationships from the patient perspective.
Methods
Participants were adult patients at an academic medical center voice clinic who were seen with a voice complaint, had no structural laryngeal lesions identified on clinical laryngoscopy, and received a clinical diagnosis of muscle tension dysphonia.14 We did not exclude patients with concurrent problems such as irritable larynx, allergies, and reflux (as mentioned by the patient, medical record, or diagnosed at the visit) to maintain ecological validity given the frequent overlap of these diagnoses with muscle tension dysphonia.15 Respondents were invited to participate approximately 4 weeks following an initial visit to the voice clinic. This time frame allowed patients to have potentially initiated speech pathology treatment and/or experienced some changes in their symptoms. Semi-structured qualitative interviews were performed by a professional interviewer using an interview guide. The professional interviewer was hired through the Office of Measurement Services at the University of Minnesota. This approach was taken to minimize potential bias and place the interviewer and participant on relatively equal footing for the initial interview (as compared to an interview conducted by a content expert). The interviewer was oriented to the overall focus of the study on the potential influence of voice symptoms on emotions and vice versa. The guide was developed by the first and last authors as a starting point and as a resource for the interviewer to ensure that the main topic areas were covered. The interviewer was instructed to allow participants to speak freely, such that the topic areas did not have to be covered sequentially, and participants were free to elaborate on aspects of their experience that they felt were particularly important. The interview guide included prompts to use if needed to help start the conversation, such as “When did your symptoms first begin?” and “What are they like now?”. Conversations were recorded and transcribed by a professional transcription service. As they were completed, transcripts were read and text was coded into main themes related to the primary interview topics. Follow-up interviews were invited when members of the team analyzing the transcripts felt that more detailed information or descriptions from the participants might allow us to understand their experience more accurately or vividly. The follow-up interviews (n=6) were conducted by an advanced psychology graduate student (C.H.) with prior qualitative interview experience.
Interview topics were centered around (1) associations between emotions and vocal function and (2) perceived control related to voice problems. To begin the interview, all participants were invited to talk about their voice symptoms and circumstances related to symptom initiation. Participants were asked to comment on whether and how stress or distress affected their vocal function and any associated physical sensations or discomfort. In keeping with the methodologic approach in phenomenologic research, which encourages participants to describe their experiences in their own words, the concepts of “stress” and “distress” were not specifically defined. To maintain the naturalness and spontaneity of the conversations, specific definitions were not solicited. To observe how voice symptoms and emotions evolve over time in a typical episode or event, participants were invited to describe a recent voice event. All participants were asked to describe strategies they had used to manage their voice symptoms and emotions, which we expected would enlighten understanding of the relationship between perceived control and voice improvements. Respondents were also invited to comment on approaches that were helpful and/or counterproductive for feeling they had control over their voice problems. The interviewer used study-approved prompts, such as “During the most recent event, what kinds of emotions were you feeling along with your physical symptoms?” and “What have you learned over time with this voice problem about what is out of your control and what is in your control to change?” only if participants needed assistance to begin or continue exploring any particular topical area.
All transcripts were read by four authors (S.M., C.H., L.M., E.H.) to identify themes within the two main topic areas and to consider emerging themes outside of those topics. While the study included elements of grounded theory, the scope of the study was focused on expressed lived experiences from the individuals interviewed; therefore, we applied phenomenological research methods.16(p141) The phenomenologic approach, which is often used to study “moods, feelings, emotions, subjectivities” was taken to provide a window into the patient’s experience within their individual culture and community.16(p141) Because this was a new direction of inquiry, we sought to describe the patient perspective without necessarily expecting to be able to comprehensively describe the layers of context surrounding their experience. Transcripts were interpreted and coded (units = sections of text, sentences, and paragraphs) for meaning by two advanced psychology graduate students (C.H. and L.M.) using inductive reasoning. Coding was recorded in NVivo (version 11, Burlington, MA, USA). Partial coding was also completed by the other authors (S.M., A.S., and E.H.) to assess for themes. Analyses primarily focused on how emotions influenced vocal function and how vocal function affected emotions. Themes were developed with consensus among the psychology graduate students (L.M. and C.H.), otolaryngology research specialist (A.S.), qualitative methodology expert (E.H.), and a laryngologist (S.M.). Seven identified themes were then distributed among these members of the research team to develop sub-themes with input from the entire research team. Differences of opinion were resolved by discussion and development of study team consensus.
As frequently necessary in qualitative study methodology, analysis required interpretation by the researchers to map conversational content to study terms.17 For example, language describing increased control over voice symptoms was interpreted as representing increased perceived control even if the participant did not specifically state that they observed greater “perceived control.” Likewise, distinctions between adaptive and maladaptive responses required some interpretation; categorizations in this well-established topic in health psychology18 were made by the psychology graduate students on the team, with senior psychology consultation (P. F.) available as needed. Emotional responses to the voice problem were categorized according to the terminology used by the participants; for example, excerpts using words such as “depressed” and “depressing” were categorized under an umbrella term “depression.” These terms were not interpreted to imply formal psychiatric diagnoses.
After clarifying the main themes of the study, four authors (S.M., C.H., L.M., E.H.) individually developed draft conceptual models representing the interview content. Through an iterative and interactive consensus-based process, the study team combined components of the drafted models into one that conceptualized relationships among the high-level constructs of voice and emotional/behavioral factors and the role of perceived control in those relations. Two speech-language pathologists (L.B., D.M.), each with at least a decade of voice care experience and 35 years experience in total, then reviewed the model for clinical fidelity. A senior psychologist (P. F.) also reviewed the model in the context of prior studies on perceived control and health.
Study size was anticipated to be n=35 with additional recruitment as needed to reach thematic saturation,19 but was reached by the 23rd interview, at which time recruitment was ended. Patients were given a $25 gift card in appreciation of their time and participation. The study was approved by the University of Minnesota Institutional Review Board, with study ID #1201M09533.
Results
A total of 56 patients who met study inclusion criteria were informed that the study was open for enrollment via phone message or email; 22 did not respond, 7 declined, 27 completed informed consent, and 23 participated. Participants’ age range was broad (19–74), with a mean age of 50 (SD 15.4) years old; most (87%) were female, Caucasian/white, and non-Hispanic/Latino, with a distribution of incomes skewing towards the wealthy (Table 1). No obvious differences in perspectives were identified along age, gender, racial, or ethnic categories, aside from some retirees commenting that their voice problems were less concerning to them because they were no longer working and/or that retirement led to decreased overall stress. The duration of voice problem ranged from 3 months to “as long as I can remember.” Participants reported a range from 1–11 prior speech-language pathology (SLP) visits, 0–5 prior voice-related physical therapy (PT) visits, and 1–2 laryngology visits prior to interview participation (Table 2).
Table 1.
Sociodemographic characteristics of study participants.
| Characteristic | n | percentage |
|---|---|---|
| Age (in years) | ||
| < 40 | 5 | 22% |
| 40 to 60 | 12 | 52% |
| > 60 | 6 | 26% |
|
| ||
| Gender | ||
| Male | 3 | 13% |
| Female | 20 | 87% |
|
| ||
| Race | ||
| Caucasian/white | 22 | 96% |
| Black/African American | 1 | 4% |
|
| ||
| Hispanic, Latino/Latina, Spanish Origin | ||
| Yes | 1 | 4% |
| No | 21 | 91% |
| Unknown | 1 | 4% |
|
| ||
| Income | ||
| < $80,000 per year | 11 | 48% |
| ≥ $80,000 per year | 10 | 43% |
| Unknown | 2 | 9% |
Table 2.
Clinical characteristics of participants
| Study ID | Duration of voice disorder | SLP visits (n) | PT visits (n) | Laryngologist visits (n) |
|---|---|---|---|---|
| 1 | 6 years | 11 | 0 | 1 |
| 2 | 11 months | 4 | 0 | 1 |
| 4 | >8 years overall; 5 months for | 8 | 0 | 1 |
| current episode | ||||
| 5 | 4 months | 2 | 0 | 2 |
| 6 | 4 years | 1 | 0 | 1 |
| 7 | 2 years | 1 | 0 | 1 |
| 8 | 10 months | 1 | 0 | 1 |
| 9 | 1 year | 1 | 0 | 1 |
| 10 | 3 years | 5 | 0 | 2 |
| 11 | 2 years | 3 | 0 | 1 |
| 12 | 2 years, 2 months | 4 | 0 | 1 |
| 14 | 14 years | 9 | 0 | 2 |
| 15 | 8–9 years | 3 | 5 | 1 |
| 16 | 2 years | 2 | 0 | 1 |
| 17 | 1 years | 2 | 0 | 1 |
| 18 | 4–5 years | 5 | 0 | 1 |
| 19 | 3 months | 5 | 0 | 1 |
| 20 | 5–10 years | 2 | 0 | 2 |
| 22 | Unknown | 4 | 1 | 1 |
| 23 | 2 years | 7 | 0 | 1 |
| 24 | 9 years | 3 | 4 | 1 |
| 26 | 15 years | 4 | 0 | 1 |
| 27 | "As long as I can remember" | 4 | 0 | 1 |
Duration of voice disorder and number of speech-language pathology (SLP), physical therapy (PT), and laryngologist visits prior to interview participation.
Study team consensus after analysis of transcript narratives revealed seven main themes that roughly follow the interview topics and a logical sequence of events as follows: (1) trauma and life events preceding problem onset, (2) symptoms of the voice problem, (3) triggers for symptom exacerbation, (4) emotional responses to the voice problem, (5) impact on identity and life function, (6) prescribed and recommended therapy and medications, and (7) personal coping strategies. Although symptoms and impact on identity/life function were not a central focus of this study, they were coded to confirm that the sub-themes were consistent with clinical experience and prior literature.8
Trauma and life events preceding onset
Although participants were not directly asked to draw links between their voice problems and preceding or concurrent life events and trauma, nearly all participants noted them in one way or another. Events varied widely and fell into predictable categories: job changes; illness, injury, and death of family member and friends; personal separation and divorce; housing relocation; conflicts with others; and personal illness, other medical problems, injury, surgery, and miscarriage. Along with onset of voice problems, these types of events understandably triggered emotions such as anxiety, sadness, and fear as described by these participants: “It definitely started around the time I was having a lot of anxiety [related to conflicts with neighbors]… the anxiety is still there.” and “I’m going through a divorce… I get emotional; when I start feeling like that, like I’m going to cry or whatever, I can feel all the muscles in my neck and my throat, and even into my chest, tighten up...” Another contributing factor was heavy vocal demand (in 7/23 participants).
Symptoms of the voice problem
All participants were asked to talk about their voice symptoms. Their typical (>50%) responses referred to tangible indicators like these: pain and soreness; hoarseness; voice exertion, pitch, projection, “very shaky,” “gives out” when speaking or singing; and tightness, strain, or a lump “in my throat right here”. Often full symptom descriptions sounded vague, as though the patient was unsure and could only compare it to something “like” something else, as in these quotes: “Usually I don't notice it initially when I...get together with people. I start to notice a fullness, like a tightness in my throat, and then it just felt like a straining to speak.”
Triggers for symptom exacerbation
After describing an initial event identified as the beginning of their voice symptoms, participants were asked to identify triggers that exacerbated symptoms, caused recurrence of, or led to new voice/throat symptoms. Two sub-themes captured these triggers. One was encounters with external conditions such as work deadlines, congested traffic, physical environment (ambient loud noise, weather, air pollution) and expressed by one participant in this way: “I am trying to make myself heard over crowd noise...then I find myself straining to be heard, and eventually I have problems projecting my voice and being heard.” The second sub-theme was internal reactions, identified by narratives that described globus sensation (‘feeling like a lump in my throat’), anxiety related to experiences with past and current voice symptoms (“...whenever I speak to people, the anxiety is there about my voice”), fear, and frustration, and, in a small minority of patients, associated symptoms such as coughing or laryngospasm.
Emotional responses to voice problem
Most participants did not volunteer a direct link between emotions and initial voice/throat symptoms but, in their narratives, some described psychological responses directly related to symptoms. Sub-themes of psychological or emotional responses seemed to fall roughly along a continuum of hope. For some, hope came with knowledge: “Knowing that my vocal cords were not permanently damaged gave me so much hope,” while hopelessness was a sense that things will never get better: “I feel hopeless...like when is this ever going to be ok?” Between hope and hopelessness patients expressed acceptance, frustration, and anger as can be heard in these example quotes from several participants: “I’ve gotten so used to it now that I just kind of accept it.” (acceptance); “I feel the pain but I’m not depressed. I avoid...the fun things I used to do.” (avoidance); “Not having a voice has really made my job stressful.” (stress); “Oh yeah it creates anxiety.” (anxiety); “It makes me depressed, because I didn't have this before.” (depression); “I don't know, just that I'm frustrated and I sound terrible and I feel incompetent.” (frustration, decreased self-worth and self-esteem); “I get depressed...then frustrated…[and] I guess angry.” (accelerating to anger). Some patients expressed a sense of little agency: “It’s sort of out of my control.”
While we identified participant-reported psychological triggers around the onset of voice symptoms and described psychological responses to voice symptom events, most participants found it difficult to say which came first when asked outright to do so. “It’s really the chicken and the egg situation,” summed up one participant who continued, “What came first? What’s causing the other?” Here are few examples of how that confusion is manifested in narrative responses to the interviewer’s request to “walk me through the sequence.” After attempting to remember the details of a recent episode, this participant struggled - “I’m trying to think,” and eventually admitted, “I don’t know. In the moment, I don’t really notice.” Another admitted up front, “I don’t know,” and that their process is, “probably pretty messy.” A few, somewhat more clear, passages in this area come closer to describing the conundrum:
“The more I had to strain my voice, then the more stressed I got; and, the more stressed I got, then the more my voice would just give out.”
“I’ve had instances of both situations where it’s happened where...my voice is acting up and then I get stressed; and then I’ve had instances where I’m stressed out and then my voice acts up.”
“I have anxiety because of [unpredictable voice symptoms and timing] and that makes it worse so I think during those times that I’m especially anxious that it’s definitely worse.”
In the end, participants did not find causal links easy to define: “I don't [know] which is the cause of which, if it's the anxiety causing the voice issues, or if it's the voice issues causing the anxiety. So, I definitely think that they're linked, that they're connected. Yes, absolutely.”
Impact on identity and life functions
Nearly all participants described effects of voice symptoms on their identity, often related to their ability to function at work. Some singers said they curtailed or ended their singing careers and avocations; “More and more I can’t sing anymore. I don’t do it professionally anymore,” and “My feelings of self worth [come] from my singing. It was such a big part of my life.” Participants whose jobs required frequent talking were as stressed and frustrated as singers: “I have lots of meetings...and I’m in trainings; so not having a voice has really made my job stressful.” “It’s embarrassing in my work...totally embarrassing.” Many participants found their social identity and life negatively affected by their voice symptoms as seen from these examples: “I’m a volleyball player and I’ve really had to adjust how I talk and yell because it’s a really vocal sport.” “I’m a pretty outgoing person, but I would rather not talk because I don’t want to have [my friends and family] listen to the way I sound.” “It makes me very self-conscious.”
Prescribed and recommended therapy and medications
When discussing treatments they had been prescribed or recommended, nearly all participants commented on voice therapy and a third mentioned medications. A few also mentioned physical therapy. Most who received voice therapy found it helpful, though a few found it difficult to implement the techniques in their daily lives. Therapy experiences were varied, including “increased awareness” about what “can work” (i.e., muscle relaxation, applying “pressure there [circumlaryngeal massage],” “us[ing] more breath” when speaking, and speaking more slowly) that helped patients feel “happy with the [results],” though a minority was dissatisfied because “some voice exercises weren’t fun.” Even when they found speech therapy helpful, some commented that daily application was difficult or they “totally forget about [using] it.”
When they talked about medications, participants mentioned having tried nasal steroid sprays, acid reflux medications (predominantly proton pump inhibitors), and allergy medications for the voice problem, and frequently reported mild or no benefit. Hard candies were also frequently mentioned.
Coping strategies
All participants in the study mentioned personal, self-management strategies for coping with their symptoms. These strategies were categorized into two sub-themes as behavioral and psychological. Behavioral change tactics included “drinking a lot of water” or alcohol (“I feel like [alcohol] helps,” a beer made it “so much better...just feeling relaxed”), “icing it,” rest, and physical actions such as “removing myself from the [stressful or environmental] situation.”
Psychological strategies mentioned related to adaptive thinking, mind-body awareness, and emotion regulation. Adaptive thinking strategies included acceptance and hope, as noted in the “Emotional responses” section above. Mind-body awareness20 was represented by statements like, “I make sure I’m taking deep breaths.” Emotion regulation21,22 was manifested in approaches such as change of cognition (thinking “calmer thoughts,” self-reminders to “not panic” and “just deal with [it],”) and attentional deployment such as “not dwell[ing] on it,” focusing more on “work and the next thing [to do] in the day.” Finally, while many found socializing frustrating because of their inability to communicate as easily, a very small proportion of participants found social support helpful for coping, especially if it came from others who had similar voice experiences as expressed by this participant, “It’s really encouraging to know [from others] that you can actually get through it and it’s going to be better in the long run.”
In general, participants who reported greater success with self-management strategies that focused on controllable aspects of their circumstances also seemed to express less distress about their voice symptoms. In these patients, their general coping approach was also reflected in a sense of voice-specific control, which was also improved by receiving information about their voice problem. This will be further described below.
Conceptual Model linking perceived control and voice symptoms
In the consensus conceptual model (Figure 1), voice change occurs through cycles of individual-level adaptive or maladaptive emotional and behavioral responses that are influenced by perceived level of control (more vs. less) over voice symptoms and problems. Vulnerability (e.g., ongoing vocal demands, life stressors) to, and precipitants (e.g., environmental irritants, reflux) of, voice problems also contributed to perpetuation or resolution of voice problems.
Figure 1.
Whether more or less control is perceived may influence whether emotional/behavioral responses are adaptive or maladaptive. Maladaptive responses were associated with heightened vulnerability to develop worsened voice symptoms in response to precipitants (e.g., physical, emotional stressors), whereas adaptive responses were associated with lower vulnerability and greater possibility for improvement
Respondents who described emotional and behavioral responses reflecting their perception of less control over the voice problem and their reactions to the voice problem tended to report ongoing maladaptive emotional and behavioral responses. We did not observe any instances of patients concurrently reporting maladaptive responses and symptom improvement. Following are narratives excerpted from a participant who reported difficulty managing her symptoms. Her narratives illustrate maladaptive responses to perceptions of a loss of or general sense of little control over her situation:
-
The following narrative illustrates her use of alcohol as a coping mechanism, the temptation of vocal strain even though it may be counterproductive and painful, and negative emotional responses to this difficult situation.
“It’s hard to speak over other people when I’m at a bar. It happens a lot when I’m out with friends and I know I’m not supposed to drink to make it feel better but I feel like that helps. … I can feel it coming on and I have to strain more and I know I shouldn’t but I want to be heard and it doesn’t necessarily hurt immediately. Then after I’ve been talking or talking to someone it gets to that point where it really hurts a couple of minutes later. … I feel the tightness and I’m trying to make myself heard and I get depressed pretty quickly, pretty much all at the same time.” -
This excerpted narrative shows avoidance, ongoing emotional distress, and difficulty with acceptance.
“The pain really makes me aware that I’m depressed because I can’t sing anymore and I can’t do some of the fun things I used to do anymore. ... I sometimes avoid those situations too and maybe that’s not good. I’m not sure. I know I should let it go and move on and accept that I have the problem but it’s really hard.” -
In this next narrative, instead of feeling encouraged that good results are possible, the patient’s attention is more drawn to the difficulty of independently maintaining those results. Her comments also show how she does not perceive control over her emotional reactions to symptom persistence.
“I’m in the [speech therapy] office and we’re going through what I’m supposed to be doing and it makes sense and it’s working and I feel good. And, then I go home and it’s like it doesn’t work anymore and I get depressed and I keep trying but it just doesn’t work. … I keep doing these things over and over and feeling like I should be getting better and I’m not.”
Another factor for some participants was that maladaptive responses led to an expanding list of precipitants. For example, the husband of one patient, who was invited by his wife to participate in the interview, commented on her sensitivity to smell and its effect on her voice: “We don’t go places any more because every time she goes someplace it’s a reaction to something. There’s even grocery stores we don’t go into.” That is, the extrapolation from some environments being problematic to the expectation that many environments will be problematic led to increasing use of avoidance strategies, associated with lessened perceived control over the voice symptoms.
Respondents who described coping strategies reflecting their perception of having some control over their voice problem generally tended to adopt adaptive emotional and behavioral responses, typically leading to symptom improvement. For some patients, strategies such as voice treatment/speech therapy and changing how they thought about the voice problem appeared to allow them to transition from a low perceived control state to a high perceived control state, facilitating symptom improvement. The following excerpts were from a patient who described increasing perceived control related to the voice problem and associated adaptive emotional and behavioral responses:
-
After describing an initial lack of perceived control, the patient, in this narrative, talked about her expectation that this context would always be challenging for communication, even though symptom severity might vary.
“We go to breakfast almost every Sunday at a café where there is always lots of background noise and that was, you know, knowing that that was going to be a rough situation.” -
In these excerpts, the patient expressed increased sense of control derived from knowing more about the problem and having faith that following expert recommendations would be helpful.
“Once I was told by experts that my vocal cords were not permanently damaged that gave me so much hope. It allowed me to find out what the problem was and once I knew what it was I knew what I could do to make it better and to listen to the experts so that I could keep getting better. That helped everything. It changed my outlook and it reduced my stress level. … It helped my depression too.” “When the stress comes on from that stuff that’s when I forget to do the deep breathing and the things I’m supposed to do to make talking easier. If I take control of those situations and concentrate, then I know I can get it together and take the deep breaths and eventually be able to talk in the conversation again.“
Another participant communicated high perceived control and optimism about benefits of voice treatment: “I’m pretty good. And whatever it is, I’ve lived with it this long, so if I can make it better, I can.” One participant who was part-way through a course of speech therapy spoke with tentative, but potentially helpful, self-awareness and insight as she noted, “Probably in the best of all possible worlds I probably would be recognizing that I had stress before it got to the point where I was having the problems.”
Discussion
The findings from these qualitative interviews suggest an important role for perceived control in leading to adaptive or maladaptive responses to a voice problem. This is consistent with the role of perceived control in other medical problems.23,24 In general, patients did not directly identify psychological factors as precipitants for the initial onset of voice problems but they did report ways in which voice problems led to psychological distress that, in turn, exacerbated voice symptoms. Among these patients, for whom speech therapy could reasonably be expected to be helpful, most did find at least partial relief. Patients also reported using behavioral and psychological personal coping strategies.
The preliminary conceptual model presented here represents our interpretations of connections between common themes across participants, in which participants reported heterogeneous onsets of voice problems, which were then maintained when precipitants (such as vocal, physical, and/or emotional stressors) led to ongoing vocal difficulties. Perceptions of having some control tended to be associated with adaptive emotional and behavioral responses and subsequent improvement; for those who seemed to perceive little or no control their responses tended to be maladaptive and symptoms persisted. We observed no instances of maladaptive responses leading directly to improvement, but did note that the feedback loop in the model could lead back to a branch that would potentially allow a change to an adaptive response that could give rise to improvement. As Nichol et al. have noted, “factors producing a dysphonic voice are often a complex mixture of organic, psychological, and social features, any one of which may be predisposing, precipitating, or perpetuating agents.”25 Despite the complexity of our proposed model, this is a relatively limited representation of relationships that are likely to be more multifactorial and multifaceted than what could be explored in the interviews for this study. For example, factors such as personality,26 stress responses/reactivity,27,28 self-regulation,29 and emotional state,30 as well as perhaps other factors and contextual characteristics still to be identified, are likely to play important roles in the relationships between voice and psychological state.
The interpretation of vulnerability being a potential explanation for how maladaptive vs adaptive coping influences subsequent voice symptoms was drawn from the totality of the interviews, and was not explicitly described by participants, who did not tend to take a mechanistic approach to the conversations. The current data do not allow us to definitively determine whether vulnerability acts as a mediator or moderator.31 Based on the observation that whether coping is adaptive or maladaptive seems to influence the degree to which participants were vulnerable to precipitants such as vocal demand and other environmental or psychological factors, we would lean towards considering vulnerability to function as a mediator. However, given the non-quantitative nature of the study, and the fact that vulnerability was not the primary focus of this study, this categorization is offered with caution.
The focus on perceived control in our preliminary conceptual model overlaps with other health behavior change theories such as the Health Belief Model,32,33 Theory of Planned Behavior,34 and Social Cognitive Theory.35 Each of these well-known theories suggest that how individuals perceive their health problems, their possible coping strategies, and/or their abilities to take productive actions (e.g., self-efficacy) influences their subsequent behavior. Thus, these theories are consistent in suggesting that, in addition to the nature and severity of the problems, individuals’ perceptions and coping abilities can play a major role in their behavior, and potentially, outcomes.36 Our preliminary conceptual model also differs from other health behavior change theories in a few important ways. First, our conceptual model was developed for a specific clinical population and may have particular applicability in multidisciplinary voice clinics. Second, our model suggests that an individual’s perceived control in the present may directly influence their subsequent voice-related behavior. Voice patients may benefit from working with health professionals to facilitate more adaptive appraisals of their stressors. Our preliminary model was developed based on a phenomenologic approach and will need to be refined and edited with the collection of additional quantitative and qualitative data.
Although general locus of control and perceived control are related,37,38 participants in this study spoke more about voice-specific perceived control than general control over life events. This was particularly reflected in comments related to speech therapy but also in the personal psychological tactics (such as emotion regulation) that were described. Important distinctions have also been drawn between past control (control over an event in the past), present control (what one can do now), and future perceived control (control over events in the future).37 Although comments about the past and future did come up during the interviews, many patients, especially those who perceived control over their voice symptoms, focused their discussion on present control.
A characteristic of qualitative analysis is that it necessarily reflects biases of the analyzers.39 For this study, we intentionally created a team of researchers with diverse perspectives, which generated themes that represented both the clinical voice perspective and those based in psychological and counseling theory. In addition, expertise of the senior author in qualitative methodology ensured that these perspectives were incorporated with rigor. All interpretations presented here were reached with consensus from the authors through critical, thoughtful discussion.40 A reflection of the effectiveness of this team analysis is that, when analysis was complete, authors without prior experience with voice patients were able to describe the patients’ perspectives plausibly to those with prior experience.
Although conducted with attention to rigor and achieving thematic saturation, this study does have limitations. Study participants were all seen at one academic medical center voice clinic, implying a certain level of desire and ability to access specialized care. Thus, findings cannot necessarily be generalized to other settings or all patients with voice problems. There was a stronger female preponderance in this small sample than in other studies of voice disorders;8 gender was not a criterion for participation and patients were invited to enroll as they were identified through the clinic. Some participants reported concurrent irritable larynx symptoms, which they saw as being part of a continuum of symptoms affecting their voices. Participants were also heterogeneous with respect to duration of voice disorder and participation in prior or current voice therapy. Examination of interactions between these important factors with the central study questions was beyond the scope of this study but would be appropriate for follow up studies. Finally, qualitative research designed to glean deep and unstructured information is conducted with small numbers of patients; its use is not intended for, nor does it allow, quantitative comparisons or conclusions. Nonetheless this type of data offers valuable insights into patient perspectives and thus informs our understanding of how complex concepts may interact.
Future studies on this topic may benefit from a longitudinal study design incorporating scales that measure behavioral, emotional, and perceptual constructs such as those mentioned above. Mixed methods approaches integrating standardized studies of voice and psychological state with additional in-depth qualitative investigation may also prove enlightening.
Conclusions
In this qualitative study, 23 participants with a clinical diagnosis of muscle tension dysphonia participated in semi-structured interviews exploring relationships between emotional/psychological factors and voice problems. Voice problems were described as leading to emotional distress, which in turn often exacerbated the severity of voice symptoms. Speech therapy was seen as a generally positive experience, with a minority of patients reporting frustration with carryover. Perceived control--the perceived ability of the patient to control either the voice problem or their responses to it--appeared to influence whether participants’ emotional and behavioral responses were adaptive or maladaptive. Future studies using mixed methods, and focusing on patients at specific points along their treatment process, may further characterize these pathways.
Acknowledgments
We appreciate the gracious assistance of Mark Miazga, J.D. for interviews through the Office of Measurement Services, Meaghan House, M.P.H. for study coordination, and George S. Goding Jr, M.D. for welcoming study recruitment in the clinic.
Footnotes
Disclosures
Research reported in this publication was supported by the National Institute on Deafness and other Communication Disorders of the National Institutes of Health under award number K23DC016335 (Misono). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Stephanie Misono, Email: smisono@umn.edu, Assistant Professor, Otolaryngology, University of Minnesota, Minneapolis, MN, Phone (612) 625-3200, fax (612) 625-2101.
Caroline Haut, Email: hautx009@umn.edu, Research Coordinator, Psychiatry, University of Minnesota, Minneapolis, MN.
Liza Meredith, Email: mere0032@umn.edu, Contract Assistant Professor, Psychology, University of Minnesota, Minneapolis, MN.
Patricia A. Frazier, Email: pfraz@umn.edu, Associate Chair, Distinguished McKnight University Professor, Department of Psychology, University of Minnesota, Minneapolis, MN 55455.
Ali Stockness, Email: nicho656@umn.edu, Research Manager, Otolaryngology, University of Minnesota, Minneapolis, MN.
Deirdre D. Michael, Email: micha008@umn.edu, Assistant Professor, Otolaryngology, University of Minnesota, Minneapolis, MN.
Lisa Butcher, Email: Lbutcher10@umphysicians.umn.edu, Speech-Language Pathologist - Lions Voice Clinic, Otolaryngology, University of Minnesota Health, Minneapolis, MN.
Eileen M. Harwood, Email: harwo002@umn.edu, Associate Professor, School of Public Health, Division of Epidemiology and Community Health, University of Minnesota - Twin Cities, Room 381 West Bank Office Building (WBOB), 1300 South Second Street, Minneapolis MN 55454.
References
- 1.Cohen SM. Self-reported impact of dysphonia in a primary care population: an epidemiological study. Laryngoscope. 2010;120:2022–2032. doi: 10.1002/lary.21058. [DOI] [PubMed] [Google Scholar]
- 2.Ruben RJ. Redefining the survival of the fittest: communication disorders in the 21st century. Int J Pediatr Otorhinolaryngol. 2000;49(Suppl 1)(2 Pt 1):241–245. doi: 10.1016/s0165-5876(99)00129-9. [DOI] [PubMed] [Google Scholar]
- 3.Titze IR, Lemke J, Montequin D. Populations in the U.S. workforce who rely on voice as a primary tool of trade: a preliminary report. J Voice. 1997;11:254–259. doi: 10.1016/s0892-1997(97)80002-1. [DOI] [PubMed] [Google Scholar]
- 4.Cohen SM, Kim J, Roy N, Asche C, Courey M. Direct health care costs of laryngeal diseases and disorders. Laryngoscope. 2012;122:1582–1588. doi: 10.1002/lary.23189. [DOI] [PubMed] [Google Scholar]
- 5.Cohen SM, Dupont WD, Courey MS. Quality-of-life impact of non-neoplastic voice disorders: a meta-analysis. Ann Otol Rhinol Laryngol. 2006;115(2):128–134. doi: 10.1177/000348940611500209. [DOI] [PubMed] [Google Scholar]
- 6.Dietrich M, Verdolini Abbott K, Gartner-Schmidt J, Rosen CA. The frequency of perceived stress, anxiety, and depression in patients with common pathologies affecting voice. J Voice. 2008;22:472–488. doi: 10.1016/j.jvoice.2006.08.007. [DOI] [PubMed] [Google Scholar]
- 7.Siupsinskiene N, Razbadauskas A, Dubosas L. Psychological distress in patients with benign voice disorders. Folia Phoniatr Logop. 2011;63:281–288. doi: 10.1159/000324641. [DOI] [PubMed] [Google Scholar]
- 8.Misono S, Peterson CB, Meredith L, et al. Psychosocial distress in patients presenting with voice concerns. J Voice. 2014;28(6):753–761. doi: 10.1016/j.jvoice.2014.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Misono S, Meredith L, Peterson CB, Frazier PA. New Perspective on Psychosocial Distress in Patients with Dysphonia: The Moderating Role of Perceived Control. J Voice. 2016;30(2):172–176. doi: 10.1016/j.jvoice.2015.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Frazier P, Merians A, Misono S. Brief Report: Perceived Control and Voice Handicap in Patients with Voice Disorders. Health Psychol. 2017 doi: 10.1037/hea0000520. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rosen CA, Lee AS, Osborne J, Zullo T, Murry T. Development and validation of the voice handicap index-10. Laryngoscope. 2004;114(9):1549–1556. doi: 10.1097/00005537-200409000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Conture EG, Kelly EM, Walden TA. Temperament, speech and language: an overview. J Commun Disord. 2013;46:125–142. doi: 10.1016/j.jcomdis.2012.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kollbrunner J, Seifert E. Encouragement to Increase the Use of Psychosocial Skills in the Diagnosis and Therapy of Patients With Functional Dysphonia. J Voice. 2016 Jan; doi: 10.1016/j.jvoice.2015.11.021. [DOI] [PubMed] [Google Scholar]
- 14.Verdolini K, Rosen CA, Branski RC, Andrews ML. Classification Manual for Voice Disorders-I. Lawrence Erlbaum; 2006. p. 249. [Google Scholar]
- 15.Misono S, Marmor S, Roy N, Mau T, Cohen SM. Multi-institutional Study of Voice Disorders and Voice Therapy Referral: Report from the CHEER Network. Otolaryngol Head Neck Surg. 2016;155(1):33–41. doi: 10.1177/0194599816639244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Plummer K. Documents of Life 2: An Invitation to a Critical Humanism. Sage Publications; 2001. [Google Scholar]
- 17.Leung L. Validity, reliability, and generalizability in qualitative research. J Family Med Prim Care. 2015;4(3):324–327. doi: 10.4103/2249-4863.161306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rippetoe PA, Rogers RW. Effects of components of protection-motivation theory on adaptive and maladaptive coping with a health threat. J Pers Soc Psychol. 1987;52(3):596–604. doi: 10.1037//0022-3514.52.3.596. [DOI] [PubMed] [Google Scholar]
- 19.Mason M. Sample Size and Saturation in PhD Studies Using Qualitative Interviews. Forum Qual Soc Res. 2010;11(3) http://www.qualitative-research.net/index.php/fqs/article/view/1428. [Google Scholar]
- 20.Hölzel BK, Lazar SW, Gard T, Schuman-Olivier Z, Vago DR, Ott U. How Does Mindfulness Meditation Work? Proposing Mechanisms of Action From a Conceptual and Neural Perspective. Perspect Psychol Sci. 2011;6(6):537–559. doi: 10.1177/1745691611419671. [DOI] [PubMed] [Google Scholar]
- 21.Gross JJ. The emerging field of emotion regulation: An integrative review. Rev Gen Psychol. 1998;2(3):271. [Google Scholar]
- 22.Guendelman S, Medeiros S, Rampes H. Mindfulness and Emotion Regulation: Insights from Neurobiological, Psychological, and Clinical Studies. Front Psychol. 2017;8:220. doi: 10.3389/fpsyg.2017.00220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Johnston M, Gilbert P, Partridge C, Collins J. Changing perceived control in patients with physical disabilities: an intervention study with patients receiving rehabilitation. Br J Clin Psychol. 1992;31( Pt 1):89–94. doi: 10.1111/j.2044-8260.1992.tb00972.x. [DOI] [PubMed] [Google Scholar]
- 24.Nguyen-Feng VN, Frazier PA, Greer CS, et al. A randomized controlled trial of a web-based intervention to reduce distress among students with a history of interpersonal violence. Psychol Violence. 2015;5(4):444. [Google Scholar]
- 25.Nichol H, Morrison MD, Rammage LA. Interdisciplinary approach to functional voice disorders: the psychiatrist’s role. Otolaryngol Head Neck Surg. 1993;108(6):643–647. doi: 10.1177/019459989310800604. [DOI] [PubMed] [Google Scholar]
- 26.Roy N, Bless DM. Personality traits and psychological factors in voice pathology: a foundation for future research. J Speech Lang Hear Res. 2000;43:737–748. doi: 10.1044/jslhr.4303.737. [DOI] [PubMed] [Google Scholar]
- 27.Dietrich M, Verdolini Abbott K. Vocal function in introverts and extraverts during a psychological stress reactivity protocol. J Speech Lang Hear Res. 2012;55(3):973–987. doi: 10.1044/1092-4388(2011/10-0344). [DOI] [PubMed] [Google Scholar]
- 28.Helou LB, Wang W, Ashmore RC, Rosen CA, Abbott KV. Intrinsic laryngeal muscle activity in response to autonomic nervous system activation. Laryngoscope. 2013;123(11):2756–2765. doi: 10.1002/lary.24109. [DOI] [PubMed] [Google Scholar]
- 29.Vinney LA, van Mersbergen M, Connor NP, Turkstra LS. Vocal Control: Is It Susceptible to the Negative Effects of Self-Regulatory Depletion? J Voice. 2016 Jan; doi: 10.1016/j.jvoice.2015.07.016. [DOI] [PubMed] [Google Scholar]
- 30.van Mersbergen M, Lyons P, Riegler D. Vocal Responses in Heighted States of Arousal. J Voice. 2016 Feb; doi: 10.1016/j.jvoice.2015.12.011. [DOI] [PubMed] [Google Scholar]
- 31.Frazier PA, Tix AP, Barron KE. Testing moderator and mediator effects in counseling psychology research. J Couns Psychol. 2004;51:115. [Google Scholar]
- 32.Becker MH. The Health Belief Model and Sick Role Behavior. Health Educ Monogr. 1974;2(4):409–419. [Google Scholar]
- 33.Rosenstock IM. Historical Origins of the Health Belief Model. Health Educ Monogr. 1974;2(4):328–335. doi: 10.1177/109019817800600406. [DOI] [PubMed] [Google Scholar]
- 34.Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50(2):179–211. [Google Scholar]
- 35.Bandura A. Self-Efficacy: The Exercise of Control. Macmillan; 1997. [Google Scholar]
- 36.Behlau M, Madazio G, Oliveira G. Functional dysphonia: strategies to improve patient outcomes. Patient Relat Outcome Meas. 2015;6:243–253. doi: 10.2147/PROM.S68631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Frazier P, Keenan N, Anders S, Perera S, Shallcross S, Hintz S. Perceived past, present, and future control and adjustment to stressful life events. J Pers Soc Psychol. 2011;100:749–765. doi: 10.1037/a0022405. [DOI] [PubMed] [Google Scholar]
- 38.Reed GM, Taylor SE, Kemeny ME. Perceived control and psychological adjustment in gay men with AIDS. J Appl Soc Psychol. 1993;23(10):791–824. [Google Scholar]
- 39.Anderson C. Presenting and evaluating qualitative research. Am J Pharm Educ. 2010;74(8):141. doi: 10.5688/aj7408141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Barbour RS. Checklists for improving rigour in qualitative research: a case of the tail wagging the dog? BMJ. 2001;322(7294):1115–1117. doi: 10.1136/bmj.322.7294.1115. [DOI] [PMC free article] [PubMed] [Google Scholar]