Key Clinical Message
Eccrine spiradenoma is a benign and rare adnexal tumor originating from cutaneous eccrine sweat glands. It usually presents as a solitary lesion. It can have different presentations, including a blaschkoid arrangement which is rare. Malignant transformation is possible and usually occurs after a long period of latency in multifocal types.
Keywords: blaschkoid pattern, multiple spiradenomas, segmental arrangement, spiradenocarcinoma
1. INTRODUCTION
Spiradenoma is a rare and benign cutaneous tumor of unknown etiology. It is thought to develop from eccrine sweat glands and most often presents as a solitary and painful nodule. We report a rare and original case of spiradenoma, presenting with multiple lesions in a segmental and blaschkoid arrangement with a secondary malignant transformation.
2. CASE REPORT
We report a case of a 30‐year‐old man, with no significant past medical history, who presented with a 20‐year history of multiple asymptomatic nodular lesions on the left side of his body. He presented to our dermatology clinic due to a recent change in two of these lesions. The clinical examination revealed multiple nodular and painless firm lesions, measuring 1.5‐3 cm in diameter, with a segmental arrangement according to Blaschko lines on the left side of the body (Figure 1). The lesions which had prompted the patient to present to dermatology included a 3 × 2 cm painful, firm, supraorbital nodule, deforming the eyebrow (Figure 2A); and a 3.5 × 3.5 cm painful paraumbilical ulcerated and oozing nodule(Figure 2B). There was no evidence of lymph node enlargement, and the rest of the clinical examination was normal.
Figure 1.

Multiple nodular and painless firm lesions, measuring 1.5‐3 cm in diameter, with a segmental arrangement according to Blaschko lines on the left side of the body
Figure 2.

A, 3 × 2 cm painful, firm, supraorbital nodule, deforming the eyebrow. B, 3.5 × 3.5 cm painful, firm, paraumbilical ulcerated and oozing nodule
Histological examination of three similar nodular lesions was in favor of a benign eccrine spiradenoma. However, the histological aspect of the two suspicious lesions showed poorly differentiated tumors not connected to the epidermis (Figure 3A), made of a double cell proliferation: light‐core cells and smaller cells with a dense nucleus, with the presence of 4‐5 mitoses/10 fields and without vascular emboli (Figure 3B). The immunohistochemical study of these two tumors revealed a proliferation index at 20% (by ki67 antibody), and a moderate labeling of 30% of the tumor cells by anti‐P53 antibody, a proliferation marker. The histological study and the immunohistochemical profile were consistent with a bifocal indolent spiradenocarcinoma. Radiological assessment did not reveal any distant metastases. Total excision of the two lesions was performed under local anesthesia with 1‐cm margins. The patient showed a good evolution without recurrence after a follow‐up of 18 months.
Figure 3.
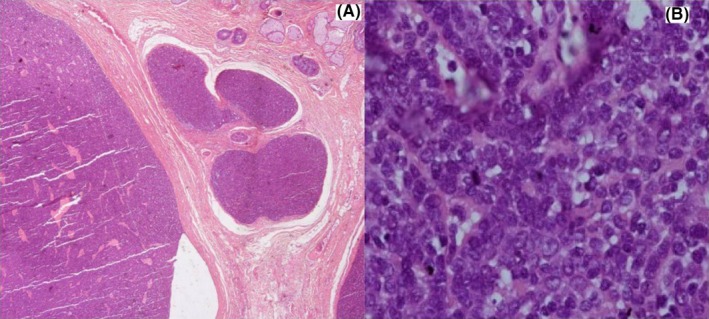
A, hematoxylin‐eosin, original magnifications ×40. Badly limited tumor not connected to the epidermis. B, hematoxylin‐eosin, original magnifications × 600. Moderate to marked cytonuclear atypia with mitoses
3. DISCUSSION
Eccrine spiradenoma is a rare and benign adnexal tumor originating from the cutaneous eccrine sweat glands. Its exact etiology is unknown. It usually presents as a single solitary and painful nodule with only 3% of the cases being multiple nodules.1 Our patient presented with multiple nodules with a blaschko‐linear segmental arrangement most likely evoking an underlying cutaneous mosaicism according to the classic dichotomous pattern of Happle.2 No similar cases were noticed in his family. Twenty‐three cases of segmental spiradenomas have been described in the literature, of which only three cases have a blaschko‐linear distribution of the lesions.3 Autosomal dominant transmission has been suggested but not confirmed. These tumors occur in young subjects with an average age of 29.8 years.
Eccrine spiradenoma is among the most painful skin tumors. Pain is present in 91% of patients and helps in establishing the diagnosis. Pain is discontinuous and intermittent, but its absence does not eliminate the diagnosis as in the case of our patient.4
Tumor growth is considered to be extremely slow. Malignant transformation is possible after a long latency period of 20‐30 years, most commonly involving multifocal eccrine spiradenomas.5 Cases of de novo spiradenocarcinomas have been described in the literature.6
Spiradenocarcinoma is a very rare and aggressive tumor of eccrine sweat glands, described for the first time in 1972 by Kersting & Helwig.7 It mainly affects young adults and can occur anywhere on the body with a predilection for the trunk and cephalic areas.8 Clinically, the lesion presents a progressive change in its characteristics and the pain remains inconstant. The diagnosis is based on histology and immunohistochemistry. The evolution is aggressive with local recurrences and the possibility of metastases, especially to the lymph nodes, bones, lungs, liver, and brain.8 The management of spiradenocarcinoma is not consensual, the treatment of choice is surgical excision with wide margins of 1‐3 cm. External radiotherapy may be useful in preventing local recurrences, but the role of chemotherapy and hormonotherapy is not yet established.9 The follow‐up of patients with spiradenocarcinoma should be very regular because of their poor prognosis; up to 39% of mortality is noticed in the absence of treatment.10
CONFLICT OF INTEREST
None declared.
AUTHORS CONTRIBUTION
HB: is a resident doctor in Dermatology and Venereology Department of Ibn Sina University Hospital, Rabat, Morocco. She contributed in the writing of this manuscript. MEA: is a resident doctor in Dermatology and Venereology Department of Mohammed V Military Training Hospital, Rabat, Morocco. He contributed in the writing of this manuscript. AB: is a doctor in “Les Nations Unies” Histopathology Center, Rabat, Morocco. She read the skin biopsies of our patient. KS: is a professor in Dermatology and Venereology Department of Ibn Sina University Hospital, Rabat, Morocco. She supervised and corrected this work. BH: is a professor and head of Dermatology and Venereology Department of Ibn Sina University Hospital, Rabat, Morocco. He supervised and validated this work.
Salim S, Bounniyt H, El Amraoui M, Benzekri A, Senouci K, Hassam B. Malignant transformation of a spiradenoma with blaschkoïd pattern. Clin Case Rep. 2018;6:2086–2088. 10.1002/ccr3.1789
REFERENCES
- 1. Sorin T, Vignaud JM, Colson T, et al. Zosteriform configuration of multiple eccrine spiradenomas of the scalp. Ann Chir Plast Esthet. 2016;61(1):65‐68. [DOI] [PubMed] [Google Scholar]
- 2. Happle R. The categories of cutaneous mosaicism: a proposed classification. Am J Med Genet. 2016;170A(Part A):452‐459. [DOI] [PubMed] [Google Scholar]
- 3. Ren F, Hu Z, Kong Q, Sang H. Multiple segmental eccrine spiradenoma with a zosteriform pattern: a case report and literature review. Ann Dermatol. 2015;27(4):435‐438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Revis P, Chyu J, Medenica M. Multiple eccrine spiradenoma: case report and review. J Cutan Pathol. 1988;15:226‐229. [DOI] [PubMed] [Google Scholar]
- 5. Rahim RR, Rajan N, Langtry JA. Infiltrative recurrent eccrine spiradenoma of the anterior neck treated using Mohs micrographic surgery. Dermatol Surg. 2013;39:1711‐1714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hantash BM, Chan JL, Egbert BM, Gladstone HB. De novo malignant eccrine spiradenoma: a case report and review of the literature. Dermatol Surg. 2006;32:1189‐1198. [DOI] [PubMed] [Google Scholar]
- 7. Kersting DW, Helwig EB. Eccrine spiradenoma. AMA Arch Dermatol. 1956;73(3):199‐227. [DOI] [PubMed] [Google Scholar]
- 8. Subha D, Sekhar DR. A rare case of eccrine spiradenoma—treatment and management. Eur J Plast Surg. 2016;39:143‐146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rebegea LF, Firescu D, Dumitru M, Patrascu A. Skin spiradenocarcinoma – case presentation. Rom J Morphol Embryol. 2016;57(1):327‐330. [PubMed] [Google Scholar]
- 10. Hantash BM, Chan JL, Egbert BM, Gladstone HB. De novo malignant eccrine spiradenoma: a case report and review of the literature. Dermatol Surg. 2006;32(9):1189‐1198. [DOI] [PubMed] [Google Scholar]


