Key Clinical Message
High index of suspicion for adenovirus infection is required in renal graft dysfunction, especially in the setting of hematuria. Histology can mimic acute rejection, which creates a diagnostic dilemma. Tissue adenovirus immunostains, though usually reliable, may not be always positive like in our case.
Keywords: adenovirus, interstitial nephritis, rejection, transplant
1. QUIZ QUESTION: WHAT IS THE DIAGNOSIS AND MANAGEMENT?
A 33‐year‐old woman with a history of deceased donor kidney transplantation 16 months prior was admitted for acute kidney injury with a serum creatinine of 8 mg/dL (baseline~1.3). Her maintenance immunosuppressive therapy (IST) consisted of mycophenolate mofetil, tacrolimus, and prednisone. Her early post‐transplant course was complicated by BK viremia that resolved with reduction in IST. This time, BK virus serology was negative and she was empirically given methylprednisolone 1 g/d for 3 days for suspected rejection. She later developed fever and hematuria and deteriorated despite receiving broad‐spectrum antibiotics. Serum adenovirus polymerase chain reaction (PCR) was positive with 10 million copies/mL. Allograft biopsy demonstrated severe interstitial inflammation with tubulitis, suggestive of acute cell‐mediated rejection (Figure 1, top panel). Immunohistochemistry staining was negative for adenovirus.
Figure 1.
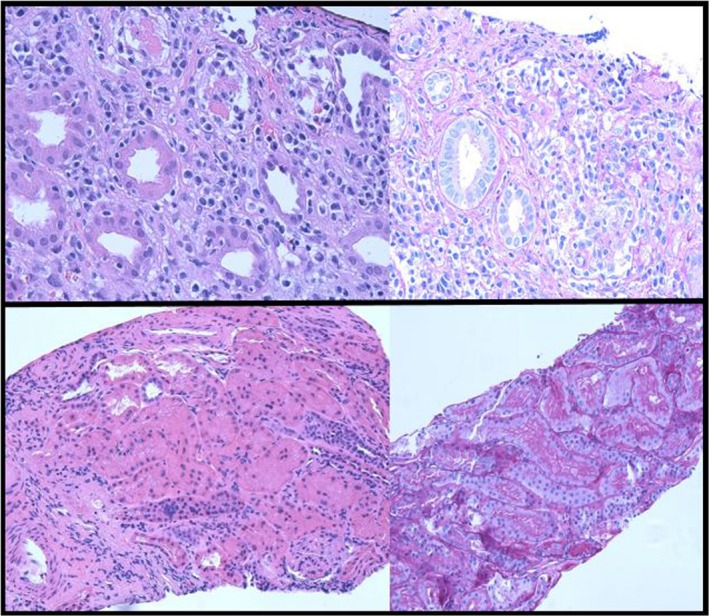
[Top panel] Initial renal biopsy demonstrating severe interstitial inflammation with T cells, mononuclear cells and plasma cells with severe tubulitis. [Bottom Panel] Repeat renal biopsy demonstrating no evidence of rejection. There were mild interstitial fibrosis and tubular atrophy and no glomerulosclerosis
Her respiratory status worsened, and adenovirus PCR was positive in bronchial washings and in the urine suggestive of adenovirus pulmonary and renal allograft involvement. Mycophenolate was held, and she received treatment with intravenous immunoglobulin and cidofovir. Adenovirus PCR in the blood was undetectable after three doses of Cidofovir 1 mg/kg. Patient clinically improved, and creatinine was 1.5 mg/dL at discharge, which retrospectively confirms the diagnosis of adenovirus nephropathy. A repeat biopsy at follow‐up visit showed mild interstitial fibrosis and tubular atrophy (Figure 1, bottom panel).
2. HUMAN AND ANIMAL RIGHTS (WITH IRB APPROVAL NUMBEr)
This article does not contain any studies with human participants or animals performed by any of the authors. IRB approval is not applicable for a single case study.
INFORMED CONSENT
It was obtained for the publication of this case study. No identifiable patient information included.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interest.
AUTHORSHIP
The authors have made substantial contribution to the preparation of this manuscript. KA, KL, AS: drafted the initial version of the manuscript, participated in patient care. XZ: provided pathology images and pertinent input. AK: reviewed and revised the manuscript for critically important intellectual content.
Alquadan KF, Womer KL, Santos AH, Zeng X, Koratala A. Not all inflammation in a renal allograft is rejection. Clin Case Rep. 2018;6:2285–2286. 10.1002/ccr3.1825
Funding information
This work was supported by the Gatorade Trust through funds distributed by the University of Florida, Division of Nephrology, Hypertension, and Renal Transplantation, and the Central Florida Kidney Center, Inc.


