Key Clinical Message
Enteric duplication cyst is a very rare condition, the affected individual may be asymptomatic. It has serious complications, on top of which is a malignant transformation tendency. To avoid these complications, resection of the duplication seems to be mandatory, even if it is an incidental finding.
Keywords: acute intestinal obstruction, enteric duplication cyst, laparotomy
1. INTRODUCTION
Enteric duplication is a very rare condition, although it might lead to major morbidities. We present an exceptional case about a 13‐year‐old girl who presented with symptoms and signs of acute intestinal obstruction. With an unsual medical history and unique radiological features, intraoperatively, it was found that she has a blind‐ended tubular duplication of 54 cm and two appendices. Details of the case's clinical presentation, management, histopathology report, and outcome are discussed.
Enteric duplication cyst (EDC) is an abnormal extra primitive gut segment. It may be tubular or cystic; the former is less common than the later.1 It is an infrequent congenital condition that presents in early childhood, affecting more males than females.1 Autopsy reflected a prevalence of 1 per 100 000, and only 29 cases have been reported with EDC in English literature.2 EDC could be situated anywhere throughout the gastrointestinal tract (GIT) from the esophagus to the anus.2 Its commonest site is the small intestine (47%), followed by the colon (20%), esophagus (17%), stomach (8%) and duodenum (2%).2 Pylorus and cervical duplications were not reported. 2
2. CASE REPORT
A 13‐year‐old Sudanese girl presented with colicky abdominal pain, absolute constipation, and vomiting of everything she eats for 2 days. Since the age of 5 years, she was experiencing recurrent attacks of abdominal pain mainly at night, aggravated by spicy foods. In addition to frequent episodes of yellowish diarrhea and dyspepsia. Interestingly, this girl used to experience daily excessive audible bowel sounds that could be clearly heard by anyone close to her. She is the seventh of 10 siblings, of whom two have died in their early childhood. Furthermore, there were unexplained four deaths among her nephews (According to Seijo Ríos et al. there is no familial aggregation of EDC3, yet this significant mortality is to be studied). On physical examination, she looked ill, in pain, tachypnic and had a low‐grade fever and a distended tender abdomen. Laboratory investigations were within the normal ranges. Supine abdominal X‐ray showed a tubular structure originating from the right iliac fossa, crossing obliquely upward reaching the left hypochondrium (Figure 3). Multiple air‐fluid levels were detected in the erect abdominal X‐ray (Figure 3). Hence, a diagnosis of acute intestinal obstruction was considered. The patient and her relatives were counselled and consented for an emergency exploratory laparotomy.
Figure 3.

The appearance of the tubular enteric duplication cyst in the supine and erect abdominal X‐rays
Intraoperative findings revealed a long blind‐ended necrotic tubular structure arising from the mesenteric border of the terminal ileum, 4 cm proximal to the ileocecal valve, with no attached mesentery. This loop was twisted multiple times around its base, leaving a very narrow neck, above which a coiled appendix was situated (Figures 1A and 2A). Beyond this base, the loop was progressively dilated and ascended obliquely across the abdomen toward the left hypochondrium. It traversed anterior to the small bowel, the transverse colon and arched over the gastric fundus. Terminally, a free much‐distended blind end was located just below the left crus of the diaphragm (Figures 1A and 2B). This loop was gently mobilized (Figure 1B); then, formal laparotomy was performed. No abnormalities detected apart from multiple enlarged lymph nodes, one of which was excised and was sent for histopathology examination. The cecum was carefully inspected, to look for the normal appendix which was found at the posteromedial aspect of the cecum with a healthy appearance (ie, there were two appendices: the normal one on the cecum and an extra one at the base of the duplication cyst) (Figure 1C). Thus, a diagnosis of duplication was suspected. Differential diagnosis of a huge Meckel's diverticulum and a third supernumerary giant appendix were considered. Then, entire resection of this necrotic tubular duplication was performed with a healthy tissue of 5 cm below its base. Then, a continuous double‐layered longitudinal closure of the defect of 8 cm was performed with an absorbable suture (VICRYL).
Figure 1.
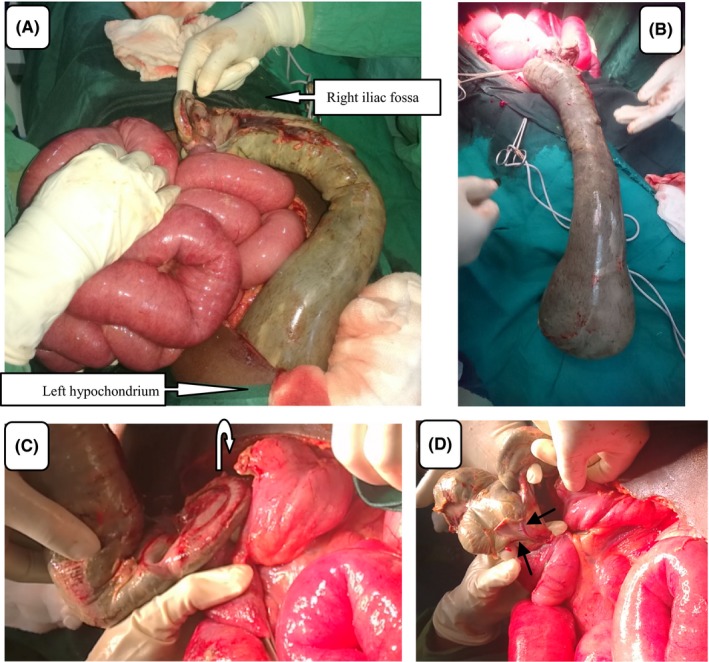
A, The origin and end of the duplicated cyst. B, The duplication post‐gentle mobilization. C, The curved arrow is pointing for the two appendices. D, The black arrows are pointing for the duplication's sharing of the GIT blood supply
Figure 2.
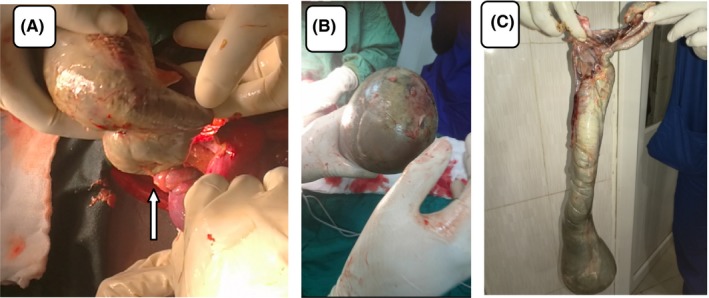
A, The twisted, very narrow neck (arrow). B, The blind distended end. C, Appearance of the duplication postsurgery
The loop was examined postoperatively, and it was found to be 54 × 18 cm at its widest region (Figure 2C). The site of its origin was separated from the ileal lumen by a membranous structure (ie, noncommunicating). Then, it was sent for histopathology examination. The patient was discharged home in 7 days postoperation. Neither immediate complications nor during the next 10 months were noted.
The histopathology report confirmed the diagnosis of EDC, with no evidence of malignant changes. The lymph node sample showed a reactive hyperplasia.
Follow‐up notes of this patient 10 months postoperation exhibited that all previous symptoms (eg, abdominal pain, audible bowel sounds and diarrhea) have totally disappeared. Up to date, she is very well and has very good bowel habits and regular activities. Regarding the follow‐up of the mortality among her siblings and nephews, unfortionately, it could not be carried out as the genetic analysis tests are not affordable.
3. DISCUSSION
Etiology of the EDC is unknown4, 5, 8; however, the accepted theories that may explain its pathophysiology are “persistence of the fetal gut diverticula” and “defect in the recanalization of the primitive gut”.4 Evolution of duplication cyst may be due to a failure of the alimentary canal transition from a solid stage into a tube during the 6th and 8th weeks of fetal life.4
Clinical presentation of EDC is manifested in the early childhood more than in the adults.6 The patient may be symptomatic or asymptomatic.7 The symptoms vary according to the defect site; it may include dysphagia,8 anorexia, vomiting, diarrhea, abdominal pain and distention.9 Some cases—as have been reported—may present with EDC complications, for example, infection, perforation,2 malignant transformation,2, 10 acute intestinal obstruction,5 rectal bleeding,6 intussusception,9 and volvulus.11
Differential diagnosis of EDC is suspected with the radiological and intraoperative findings of a defect in a cyst form that derived from the GIT. Huge Meckel's diverticulum was our main differential, as the defect in this case was about two inches (5 cm) proximal to the ileocecal valve. However, in this case, the loop arose from the mesenteric aspect of the bowel, while Meckel's diverticulum emerges from the antimesenteric aspect of the intestine.13 A giant supernumerary appendix was another possible differential diagnosis in this case, as the patient has an extra appendix (see intraoperative findings above). Other probable differential diagnoses of EDC may be mesenteric cysts (eg, enteric, mesothelial, or omental cysts).12 A gastrointestinal stromal tumor (GIST) is a soft tissue mass; it may turn into a cyst form if it is complicated by necrosis or cavitation.1 Gastrointestinal teratomas are rare tumors that perhaps affect young children.1
Diagnosis of EDC is usually achieved by the radiological techniques which prove the cyst and its origin from the GIT.12 Ultrasonography (USG) can demonstrate the cystic defect and muscular layer in its wall. So USG can differentiate EDC from other solid masses.4, 12 Abdominal X‐ray shows a gas‐filled cyst that is separated from the normal hollow (Figure 3). CT scan and MRI can show the exact anatomical site of the cyst and its dimensions. Contrast enema and colonoscopy will be helpful if the cyst is communicating with alimentary tract hollow.6 Technetium scintigraphy detects heterotopic gastric mucosa within the EDC,6, 12 and this is a useful test for a patient presents with unexplained rectal bleeding especially if he or she is in early childhood.
Classic criteria to diagnose the duplication cyst are as follows: (a) intimate attachment to the GIT, (b) a layer of smooth muscle in its wall, and (c) an epithelial lining resembling any part of the GIT.4 Other criteria of EDC are that it originates from the mesenteric border of the bowel.13 Moreover, it shares GIT blood supply1 (Figure 1D).
Management is entire resection of the duplicated cyst,1, 2, 4, 5, 6, 13 even if it is asymptomatic or incidental finding, so as to avoid its complications (one of which was a hazard to our patient). Heather R. Nolan et al.6 prescribed the first laparoscopic duplication excision, this is a good alternative approach to a laparotomy, as pain and wound complications will be less.
Teaching points of this case: The patient's medical history is of teaching values and might help in EDC diagnosis. It includes daily loud excessive bowel sounds; this point was not found in any literature. Likewise, this is the longest EDC among reported duplications which 54 cm in its length, while the longest previously reported EDC was 26.5 cm.2
In conclusion, an acute abdomen is seldom due to EDC. This should be borne in mind, as accurate diagnosis leads to targeted surgical access and proper outcome. To avoid its complications, duplication cyst resection seems to be mandatory. In this case, the patient presented with an acute intestinal obstruction. Intraoperatively, It was found that she has a long, twisted, distended, necrotic, tubular enteric duplication cyst and an extra appendix on its base. This was successfully resected without immediate or delayed complications.
CONSENT
Written informed consent was obtained from the patient and her family for publication of this case report with accompanying images.
ACKNOWLEDGMENT
With all pleasure I would like to express my special thanks of gratitude to my journal Clinical Case Report for supporting the developing countries in publishing their work and for giving me a golden opportunity to publish this rare case, as well my sincere thanks and appreciation for my teachers and colleagues who helped me a lot in the photographing and adjustments to complete this report, namely: Mr. Abdelaziz Eltayb, Ahmed M. A. Abdelrahman, Dr.Azza Satir, Mr.Abubakr Awad, Ibrahim Elhag, Azzain Mahadi, Safe Ali, Abdalla Shareef, Shuhal Hassan Eltayb, Aya Elhag, Watheer Elfatih, Eltaib Ameer, Mahil Shareef, Mohamed A. Algaali, Osama Eltayb, Omer Mosa, Hosam M. Osman, Elshandawi M.Nasr, Hiba Manmoon, Naji M. Elfatih, Khalid Abd‐Alati, Yousif Fadolelmola, Mr.Mohamed Elfatih, Razaz Basheer and Haytham I. M. Alhourani.
AUTHORSHIP
MEABE: is the first and corresponding author. YAS and IAB: are second authors (contributed equally).
CONFLICT OF INTEREST
None declared.
Elhasan MEAB, Sirdab YA, Bakheit IA. 54‐cm enteric duplication cyst in a 13‐year‐old female. Clin Case Rep. 2018;6:2099–2102. 10.1002/ccr3.1751
REFERENCES
- 1. Tsai SD, Sopha SC, Fishman EK. Isolated duodenal duplication cyst presenting as a complex solid and cystic mass in the upper abdomen. J Radiol Case Rep. 2013;7(11):32‐37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Nguyen PT, Simper NB, Childers CK. Isolated omentalduplication cyst with respiratory epithelium and pancreatic glands: case report and review of literature. J Pediatr Surg Case Rep. 2016;11(17):21. [Google Scholar]
- 3. Seijo Ríos S, Lariño Noia J, Abdulkader Nallib I, et al. Adult gastric duplication cyst: diagnosis by endoscopic ultrasound‐guided fine‐needle aspiration (EUS‐FNA). Rev Esp Enferm Dig. 2008;100(9):586‐590. [DOI] [PubMed] [Google Scholar]
- 4. Yadav KS, Sali PA, Bhole B, Tampi C, Mehta H. Ileal duplication cyst in the elderly complicated by appendicitis: a rare case report and review of literature. Int J Surg Case Rep. 2016;27:24‐27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Dombale V, Patil BV, Kadam SA, Kerudi BH. Enteric duplication cyst of Caecum presenting with intestinal obstruction ‐ a case report. JKIMSU. 2012;1(2): Kerudi Hospital, Bagalkot ‐ 587102 (Karnataka), India. http://www.jkimsu.com/jkimsu-vol1no2/jkimsu-vol1no2-CR-2-147-149 [Google Scholar]
- 6. Nolan HR, Wengler C, Hartin CW, Glenn JB. Laparoscopic excision of an ascending colon duplication cyst in an adolescent. J Pediatr Surg Case Rep. 2016;4:32‐34. [Google Scholar]
- 7. Liu R, Adler DG. Duplication cysts: diagnosis, management, and the role of endoscopic ultrasound. Endosc Ultrasound. 2014;3(3):152‐160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Baumann JL, Patel C. Enteric duplication cystcontaining squamous and respiratory epithelium: an interesting case of a typically pediatric entity presenting in an adult patient. Case Rep in Gastrointest Med. 2014;2014:790326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sharma S. Enteric duplication cysts in children: a clinicopathological dilemma. J Clin Diagn Res. 2015;9:EC08–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. You HS, Bin Park S, Hee Kim J, et al. A case of duodenal duplication cyst manifested by duodenal polyp. Clin Endosc. 2012;45(4):425‐427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Chadha R, Agarwal K, Choudhury S, Pant N, Grover J, Madan N. Completely isolated enteric duplication cyst associated with a classic enterogenous duplication cyst. J Indian Assoc Pediatr Surg. 2012;17(2):68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Atalar MH, Cankorkmaz L, Ozer H, Koyluoglu G. A huge duplication cyst of the ileum. Pol J Radiol. 2013;78(3):70‐73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Andrew K, Douglas B. Fundamentals of surgical practice (3rd edn). New York: Cambridge University Press; 2011:579‐580. [Google Scholar]


