Abstract
Importance:
Although the trends in obesity in Wisconsin overall are well described, less is known about characteristics and health consequences of different degrees of obesity. The Survey of the Health of Wisconsin is a novel population-based health examination survey that provides reliable and valid objective measurements of body mass index.
Objective:
Data from the Survey of the Health of Wisconsin is used to characterize the prevalence and consequences of different levels of obesity and track trends over time.
Methods:
A total of 3,384 participants age 21-74 years and living in Wisconsin at the time of data collection were surveyed in 2008-2013. Participants completed computer-assisted interviews and physical exams. Predictors and comorbidities of different levels of obesity were measured as prevalence, odds ratios, and population-attributable prevalence.
Results:
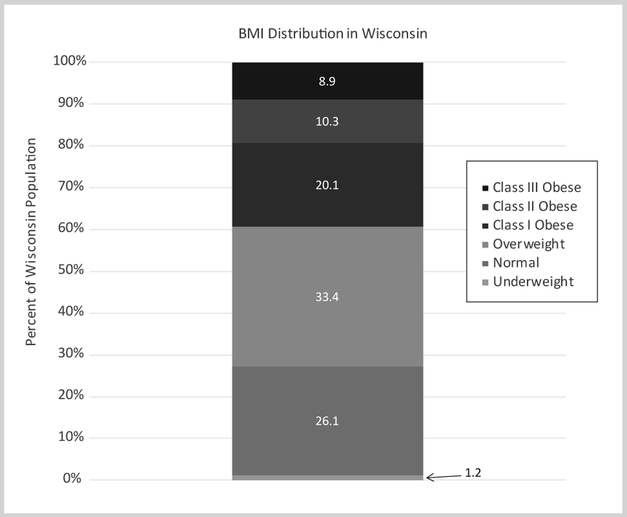
Of Wisconsin adults, 1.2% (CI, 0.7-1.7) are underweight, 26.1% (CI, 23.8-28.4) are normal weight, 33.4% (CI, 31.0-35.7) are overweight, and 39.4% (CI, 35.0-43.7) are obese—with 20.1 % (CI, 18.4-21.9), 10.3% (CI, 9.0-11.7), and 8.9% (CI, 7.6-10.2) in Class I, Class II, and Class III obesity categories, respectively. Obesity rates are higher in people who are older, poor, less educated, minorities, or who live in a community with high economic hardship. There is a dose response relationship between level of obesity and prevalence of all 9 comorbidities that were examined.
Conclusions and Relevance:
Measured rates of obesity in Wisconsin adults are higher than previously reported for the state, and obesity accounts for a significant proportion of chronic diseases.
INTRODUCTION
It is well established that the growing obesity epidemic is associated with a host of complex chronic conditions and rising health care costs.1-3 Despite extensive information that the obesity epidemic continues to pose significant health threats, there is limited population-specific data by which to characterize populations at greatest risk of both obesity and its complications. Self-reported data are known to underestimate the population-based burden of disease, and reliable and valid data are needed in order to generate targeted, effective, and efficient prevention programs and policies.4 Further, surveillance systems that focus on reporting singular outcomes without examining obesity in relationship to other comorbidities often fail to truly capture the magnitude of deleterious effects that obesity poses to population health.
While some estimates suggest that overall efforts to reduce obesity in the United States may be experiencing some success, there has been an increased focus on understanding the health impacts among individuals with different degrees (or “classes”) of obesity. The most common definition classifies individuals as obese if they have a body mass index (BMI, in kg/m2) greater than 30. Within the category of obesity, the risks of poor health outcomes are not uniform among Class I (mild), Class II (severe), and Class III (morbid) obese individuals.5 Understanding the burden of different degrees of obesity also is important to estimate the additional risk and costs of obesity, particularly in a population with a high prevalence of individuals with Class II and Class III obesity. Despite the value to policy and planning, few surveillance systems are systematically tracking objectively assessed obesity prevalence by degree of severity.
This study aims to provide more accurate statewide estimates of obesity prevalence overall and by degree of obesity, using data collected by the Survey of the Health of Wisconsin (SHOW). SHOW is a population-based health survey that includes a physical exam to measure height and weight to determine objective BMI estimates in a statewide representative sample.6 By examining the relationship between obesity and its determinants and comorbidities in Wisconsin, this study provides a baseline for evaluation of public health efforts in the state. Additionally, this study provides novel estimates of the burden of each degree of obesity in Wisconsin.
METHODS
Data Source
Data included were from 3,384 adults age 21 to 74, from the annual (2008-2013) serial cross-sections of SHOW households. Details of SHOW methods have been published previously.6 Briefly, households are selected using a 2-stage cluster method to ensure both geographic and demographic representation of the study sample. Households are randomly selected and all age eligible adults in the household are invited to participate. Data are gathered via an in-home interview in which tracking information, demographics, housing characteristics, and health history are collected. Participants also travel to a mobile exam or local clinic for bio-specimen collection, and additional personal and health history data are collected via audio computer-assisted interviews. A sample of blood is processed by the Marshfield laboratories for various health measurements, including hemoglobin A1c (HbA1c). The clinic visit also includes a physical exam to gather objective measurements of height, weight, blood pressure, and lung function (FEV1) using a peak flow meter. The SHOW protocol was approved by the University of Wisconsin Institutional Review Board, and all participants consented to study participation.
Variables
Measures of Obesity
The measures of obesity were determined using BMI, calculated by the ratio of weight (in kg) divided by height (in m2) square derived from standardized anthropometric measurements obtained during the in-person exam, completed by a total of 2930 participants. We used standard cut-points for BMI-based weight classifications as defined by the Centers for Disease Control and Prevention and using the National Heart, Lung and Blood Institute definitions to classify obesity severity (Table 1).7,8
Table 1.
Range of Body Mass Index (BMI) Included in Each Category
| Category | BMI (kg/m2) Range |
|---|---|
| Underweight | < 18.5 |
| Normal | 18.5-24.9 |
| Overweight | 25-29.9 |
| Class I (mildly obese) | 30-34.9 |
| Class II (severely obese) | 35-39.9 |
| Class III (morbidly obese) | ≥ 40 |
Determinants
To describe the distribution of obesity across the population, demographic variables included gender, race/ethnicity, and highest level of education. Family income was determined by total income reported by each person in the household divided by the total number of individuals reported in the household. This number was then divided by the federal poverty level (FPL), provided by the Wisconsin Department of Health Services, and multiplied by 100 to get a percentage. Walkability is based on the neighborhood Walk Score® and divided into tertiles.9
Community-level determinants of socioeconomic status are operationalized using a census block group level estimate of the Economic Hardship Index. The Index was derived using data from the 2000 US Census and includes a combination of 6 metrics: crowded housing, poverty status, employment, education, dependency, and individual annual income.10,11 Crowded housing is the percentage of occupied housing with more than 1 person per room. The poverty status measurement is the percentage of people living below 100% of the FPL. The employment metric is the percentage of individuals over age 16 who are unemployed. Education is the percentage of people over age 25 without a high school education. Dependency is the percentage of the population under 18 years or over 64 years of age. Individual annual income is reported in categories of < $20,000, $20,000 to $44,900, and ≥ $45,000. Once census block groups are scored, they are then ranked and split into tertiles of hardship.
Health Outcomes
—Comorbid conditions, all of which previously have been associated with obesity,12–15 were defined using data from the interview and physical exam. Self-rated health was dichotomized as fair or poor health (yes vs no) using the question, “In general would you say your health is: Excellent, Very Good, Good, Fair, Poor.” Sleep apnea is based on self-report of physician diagnosis. Occasional or frequent snoring was based on the question, “In the past 12 months, how often did you snore while you were sleeping?” Depression, anxiety, and stress were measured using the Depression Anxiety Stress Scales instrument, an assessment tool commonly used in surveillance and epidemiologic studies.16 Participants’ responses regarding symptoms of depression, anxiety, and stress over the last 7 days were scored and then categorized into normal, mild, moderate, severe, or extremely severe—the latter 3 categories being the event of interest for each variable.
Hypertension was defined as a measured systolic blood pressure ≥ 140, diastolic blood pressure ≥ 90 mmHg, or self-report of any antihypertensive medication use. Asthma is classified as having a previous diagnosis of asthma, or FEV1 < 80% of predicted value. Diabetes mellitus is classified as having a previous diagnosis of type 1 or 2 diabetes or HgbA1c ≥6.5%. Analysis of comorbid conditions did not examine underweight individuals, as etiology of disease is likely different.
Data Analysis
Descriptive estimates of the burden of obesity were determined using prevalence, adjusted odds ratios, and population-attributable prevalence, using obesity cut-points previously described for each of the demographic and health conditions. Adjusted odds ratios were calculated using logistic regression, and adjusted for age and gender. Percent popoulation attributable prevalence was calculated using the following formula:
Where Pi is the prevalence of each category of excess BMI, PRi is the unadjusted prevalence ratio of the category of BMI compared to the normal BMI level, and k references the 4 categories of excess BMI.17
All calculations were weighted to represent the population of Wisconsin and to adjust for spatial clustering and survey designbased factors. Statistical analysis was performed using SAS version 9.3 (SAS Institute Inc., Cary, North Carolina, USA) and Microsoft Excel 2013 (Microsoft Corp, Redmond, Washington, USA).
RESULTS
Figure 1 illustrates the prevalence of BMI categories in Wisconsin. Only about a quarter of Wisconsin residents are in the normal weight range, while around three-fourths are overweight or obese. A very small percent of the population is underweight. Among the proportion of the population that are classified as obese, the prevalence decreases as degree of obesity increases.
Figure 1.
The Prevalence of Each Body Mass Index Category, Survey of the Health of Wisconsin 2008-2013
Table 2 shows the prevalence of obesity among demographic and socioeconomic factors. Generally, as age increases, so does obesity prevalence, with the highest prevalence in the 65-74 age group. With regard to race and ethnicity, prevalence is highest in non-Hispanic African Americans and lowest in the “other” category. Prevalence of obesity across regions of the state were similar, with the southern region having the lowest prevalence, and the northeastern region having the highest. There were no notable differences in prevalence among year of survey participation. We see the highest prevalence of obesity for the lowest family income level and lowest obesity in the highest family income level. Prevalence is highest among those living in communities with the median economic hardship, with the lowest prevalence in census block groups with the least hardship. Estimated prevalence of obesity was similar across the 3 tertiles of walkability. Expanded statistics by BMI category are available upon request.
Table 2.
Prevalence of Obesity (BMI ≥ 30%) by Demographic and Socioeconomic Factors, N=2930, Survey of the Health of Wisconsin (SHOW) 2008-2013.
| Demographics | |||
|---|---|---|---|
| Total (n) | BMI ≥30 (%) | SE | |
| Overall | 1188 | 39.4 | 1.3 |
| Age | P=0.001 | ||
| 21-24 | 52 | 25.5 | 3.3 |
| 25-34 | 168 | 33.0 | 2.8 |
| 35-44 | 200 | 42.0 | 3.2 |
| 45-54 | 305 | 42.3 | 2.5 |
| 55-64 | 261 | 40.8 | 2.6 |
| 65-74 | 202 | 45.0 | 3.3 |
| Gender | P=0.843 | ||
| Male | 493 | 39.3 | 1.7 |
| Female | 695 | 39.7 | 1.7 |
| Race/Ethnicity | P=0.067 | ||
| Non-Hispanic white | 1015 | 38.9 | 1.3 |
| Non-Hispanic African American | 91 | 54.9 | 6.1 |
| Hispanic | 35 | 44.9 | 7.4 |
| Other | 47 | 34.3 | 7.3 |
| Health Region | P=0.315 | ||
| Southeastern | 356 | 40.9 | 2.7 |
| Southern | 228 | 35.1 | 2.5 |
| Western | 171 | 40.2 | 3.3 |
| Northern | 178 | 39.0 | 3.4 |
| Northeastern | 255 | 42.6 | 2.5 |
| Year | P=0.768 | ||
| 2008-2009 | 201 | 38.4 | 2.4 |
| 2010 | 327 | 38.2 | 1.9 |
| 2011 | 340 | 41.3 | 2.1 |
| 2012-2013 | 320 | 40.4 | 2.7 |
| Socioeconomic Factors | |||
| Family Income | P=0.001 | ||
| <100% FPL | 140 | 48.3 | 3.8 |
| 100%-199% FPL | 229 | 44.6 | 2.8 |
| 200%-399% FPL | 434 | 42.6 | 2.1 |
| ≥ 400% FPL | 339 | 32.5 | 2.1 |
| Unknown | 44 | 39.5 | 5.9 |
| Education | P=<0.001 | ||
| ≤ High school | 384 | 48.0 | 2.5 |
| Some college | 272 | 44.0 | 2.4 |
| ≥ college | 531 | 33.8 | 1.7 |
| Community Economic Hardship | P=0.013 | ||
| Least Hardship (bottom tertile) | 355 | 34.8 | 2.4 |
| Median Hardship | 414 | 43.0 | 2.0 |
| Most hardship (top tertile) | 419 | 41.5 | 2.1 |
| Neighborhood Walkability | P=0.445 | ||
| Least walkability (bottom tertile) | 403 | 37.0 | 1.8 |
| Median walkability | 405 | 39.7 | 2.1 |
| Most walkability (top tertile) | 374 | 40.7 | 2.4 |
P-value shown is from Rao-Scott chi-square test.
Abbreviations: BMI, body mass index; SE, standard error; FPL, federal poverty level.
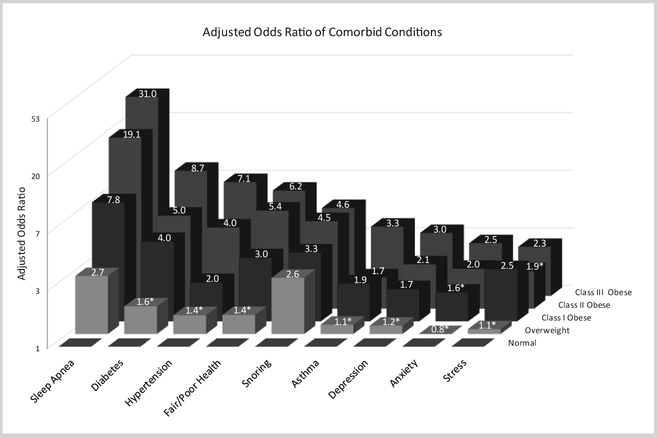
Figure 2 illustrates the burden of obesity in Wisconsin by reporting adjusted odds ratios of various comorbid conditions by BMI category. Increasing degrees of obesity are associated with increased risk of comorbid conditions, particularly those conditions previously associated with metabolic syndrome such as asthma, diabetes, and hypertension. The odds of having these conditions among individuals with Class III obesity vs those with normal BMI is approximately double the odds of individuals with Class I obesity having these conditions compared to those with normal BMI. The association between obesity and reporting fair or poor health, a standard quality-of-life measure, is similar in magnitude to having hypertension and diabetes among morbidly obese.
Figure 2.
Odds Ratio of Having Each Comorbid Condition in Each Body Mass Index (BMI) Category Compared to the Normal BMI Category, SHOW 2008-2013
Odds ratios are adjusted for age and gender, and shown on the natural log scale. * Indicates that the 95% CI crosses 1.0.
There is a clear dose-response relationship of odds of having a comormid condition for every health outcome examined as severity of obesity increases. Obesity status is strongly associated with sleep apnea in the study population, with dramatically increasing odds as BMI level increases. While overall odds of depression, anxiety, and stress symptoms appear to be greater in obese vs non-obese, degree of obesity only slightly appears to increase odds of symptoms.
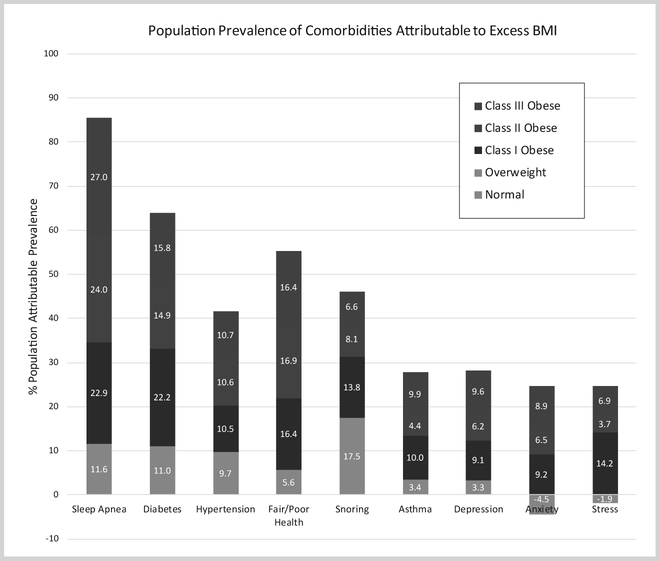
Class I and Class III obese have the largest unadjusted population-attributable prevalence (Figure 3) for most comorbidities. This is fairly expected as Class I obesity has a high overall prevalence with moderately high prevalence of comorbidities, and the Class III obesity group has lower overall prevalence than the other obesity groups but much higher prevalence of comorbidities.
Figure 3.
Percent Crude Population-Attributable Prevalence Due to Excess BMI, shown by BMI Category, SHOW 2008-2013
DISCUSSION
Data from this study are important to set a basis for monitoring trends and addressing population health over time. These baseline objective estimates of obesity from the ongoing SHOW program are important in that they illustrate the true magnitude of the obesity epidemic and related health conditions across Wisconsin. BMI is a standard and consistent measure used across most studies of obesity, making it a useful indicator for examining trends and identifying risk in a population.18 Results from the statewide survey can serve as a basis for comparison for future statewide obesity prevention initiatives, as well as community-specific comparisons. The quality and precision of SHOW data in comparison to less granular national data sets provide an accurate baseline for future community- and statespecific obesity research. While efforts are underway at the state, local, and national levels to address obesity, analysis of future survey waves will provide important data for measuring and tracking the efficacy of these efforts.
The objective measurement of obesity and its classes along with comorbidities helps illustrate the true magnitude of the obesity epidemic in Wisconsin. Comparing the SHOW population estimates to those of the National Health and Nutrition Examination Survey (NHANES) suggests obesity rates across all racial and ethnic subgroups are higher in Wisconsin compared to the nation as a whole.19,20 While obesity rates are widely reported, few studies describe how classes of obesity modify risk. Our results, while not consistently significant for all categories of comorbidities, did find a dose-dependent relationship between prevalence of comorbid condition and degree of obesity. Wisconsin’s high prevalence of Class III obesity (8.6%) suggests Wisconsin has a greater burden than nationally (7.7%).19 We confirmed individuals with Class III obesity are at much higher risk of comorbidities and a potential source of increased health care expenditures in Wisconsin.21,22 Thus, as we look towards prevention and intervention, a focus on reducing obesity among these high-risk individuals can be considered a priority.
Despite the strengths and contributions to understanding the burden of obesity in Wisconsin, there are some limitations to this analysis. The data were collected cross-sectionally, and longitudinal trends were not investigated. Aditionally, the calculation used to estimate population-attributable prevalence, while helping to illustrate the health burden of obesity in the Wisconsin population, is unadjusted for potential confounders, some of which we show to be significantly different between groups. The data used for this study were limited to adults only. In 2014, SHOW started collecting data for children as well as adults, and we hope to evaluate the data around obesity in Wisconsin children in the coming years. However, given that environmental factors play a major role in obesity, and parents are an essential part of a child’s microenvironment, examining the burden of obesity in adults can be a helpful indication of obesity in children as well.
CONCLUSION
Obesity prevalence in Wisconsin adults is higher than previously reported from telephone surveys for the state and higher than national prevalence. Obesity in Wisconsin is associated with people who are older, poor, less educated, minorities, or who live in a community with high economic hardship. Similar to the National Health and Nutrition Examination Survey (NHANES), this is a statewide issue that affects both urban and rural communities alike. The concurrence of obesity with high chronic disease burden suggests the growing obesity epidemic is affecting health and well-being and can be attributable to high health care costs and loss of productivity.2,3 Wisconsin needs more concerted efforts to prevent and reduce obesity, particularly for the most severely obese, minorities, and those with fewer resources.
Acknowledgements:
The authors would like to thank the SHOW administrative, field, and scientific staff, as well as all SHOW participants for their contributions to this study. We would also like to thank the Obesity Prevention Initiative’s Evaluation and Surveillance Group for its valuable feedback.
Funding/Support: Funding for this project was provided by the University of Wisconsin School of Medicine and Public Health through the Wisconsin Partnership Program. Funding for the Survey of the Health of Wisconsin is provided by the National Institutes of Health (#1RC2HL101468-01), the University of Wisconsin School of Medicine and Public Health through the Wisconsin Partnership Program (06012009), and the UW Institute for Clinical and Translational Research (KL2RR025012).
Footnotes
Financial Disclosures: None declared.
Contributor Information
Shoshannah Eggers, Population Health Institute, University of Wisconsin School of Medicine and Public Health (UWSMPH), Madison, Wis.
Patrick L. Remington, Population Health Institute, University of Wisconsin School of Medicine and Public Health (UWSMPH), Madison, Wis.
Karissa Ryan, Population Health Institute, University of Wisconsin School of Medicine and Public Health (UWSMPH), Madison, Wis.
F. Javier Nieto, Department of Population Health Sciences, UWSMPH.
Paul Peppard, Department of Population Health Sciences, UWSMPH.
Kristen Malecki, Department of Population Health Sciences, UWSMPH.
REFERENCES
- 1.Fontaine KR, Redden DT, Wang C, Westfall AO, Allison DB. Years of life lost due to obesity. JAMA. 2003;289(2):187–193. doi: 10.1001/|ama.289.2.187. [DOI] [PubMed] [Google Scholar]
- 2.Finkelstein EA, Trogdon JG, Cohen JW, Dietz W. Annual Medical Spending Attributable To Obesity: Payer-And Service-Specific Estimates. Health Aff (Millwood). 2009;28(5):w822–w831. doi: 10.1377/hlthaff.28.5.w822. [DOI] [PubMed] [Google Scholar]
- 3.Wang YC, McPherson K, Marsh T, Gortmaker SL, Brown M. Health and economic burden of the projected obesity trends in the USA and the UK. The Lancet. 2011;378(9793):815–825. doi: 10.1016/S0140-6736(11)60814-3. [DOI] [PubMed] [Google Scholar]
- 4.Merrill RM, Richardson JS. Validity of self-reported height, weight, and body mass index: findings from the National Health and Nutrition Examination Survey, 2001–2006. Prev Chronic Dis 2009;6(4). [PMC free article] [PubMed] [Google Scholar]
- 5.Aronne LJ. Classification of Obesity and Assessment of Obesity-Related Health Risks. Obes Res 2002;10(S12):105S–115S. doi: 10.1038/oby.2002.203. [DOI] [PubMed] [Google Scholar]
- 6.Nieto FJ, Peppard PE, Engelman CD, et al. The Survey of the Health of Wisconsin (SHOW), a novel infrastructure for population health research: rationale and methods. BMC Public Health. 2010;10:785. doi: 10.1186/1471-2458-10-785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.NHLBI Obesity Education Initiative Expert Panel on the Identification, Evaluation, and Treatment of Obesity in Adults (US) Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: The Evidence Report. Bethesda, MD: National Heart, Lung, and Blood Institute; 1998. [Google Scholar]
- 8.About Adult BMI. Centers for Disease Control and Prevention. http://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html. Updated May 15, 2015. Accessed Sept. 27, 2016.
- 9.Walk Score. https://www.walkscore.com/. Accessed Sept. 27, 2016.
- 10.Nathan RP, Adams CF. Four perspectives on urban hardship. Polit Sci Quart 1989:483–508. [Google Scholar]
- 11.Montiel LM, Nathan RP, Wright DJ, Nelson A. An Update on Urban Hardship. Albany, NY: The Nelson A. Rockefeller Institute of Government, State University of New York; 2004. [Google Scholar]
- 12.Mokdad AH, Ford ES, Bowman BA, et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA. 2003;289(1):76–79. doi: 10.1001/jama.289.1.76. [DOI] [PubMed] [Google Scholar]
- 13.Young T, Palta M, Dempsey J, Peppard PE, Nieto FJ, Hla KM. Burden of Sleep Apnea: Rationale, Design, and Major Findings of the Wisconsin Sleep Cohort Study. WMJ. 2009;108(5):246–249. [PMC free article] [PubMed] [Google Scholar]
- 14.Luppino FS, de Wit LM, Bouvy PF, et al. Overweight, obesity, and depression: A systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2010;67(3):220–229. doi: 10.1001/archgenpsychiatry.2010.2. [DOI] [PubMed] [Google Scholar]
- 15.Gariepy G, Nitka D, Schmitz N. The association between obesity and anxiety disorders in the population: a systematic review and meta-analysis. Int J Obes 2010;34(3):407–419. doi: 10.1038/ijo.2009.252. [DOI] [PubMed] [Google Scholar]
- 16.Lovibond SH, Lovibond PF. Manual for the Depression Anxiety Stress Scales. 2nd ed. Sydney: Psychology Foundation; 1995. [Google Scholar]
- 17.Rockhill B, Newman B, Weinberg C. Use and misuse of population attributable fractions. Am J Public Health. 1998;88(1):15–19. doi: 10.2105/AJPH.88.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gelber RP, Gaziano JM, Orav EJ, Manson JE, Buring JE, Kurth T. Measures of obesity and cardiovascular risk among men and women. J Am Coll Cardiol 2008;52(8):605–615. doi: 10.1016/j.jacc.2008.03.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Flegal KM, Kruszon-Moran D, Carroll MD, Fryar CD, Ogden CL. Trends in obesity among adults in the united states, 2005 to 2014. JAMA. 2016;315(21):2284–2291. doi: 10.1001/jama.2016.6458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity among adults: United States, 2011–2012. NCHS Data Brief. 2013;(131):1–8. [PubMed] [Google Scholar]
- 21.Andreyeva T, Sturm R, Ringel JS. Moderate and Severe Obesity Have Large Differences in Health Care Costs. Obes Res 2004;12(12):1936–1943. doi: 10.1038/oby.2004.243. [DOI] [PubMed] [Google Scholar]
- 22.Galinsky T, Hudock S, Streit J. Addressing the Need for Research on Bariatric Patient Handling. Rehabil Nurs 2010;35(6):242–247. doi: 10.1002/j.2048-7940.2010.tb00054.x. [DOI] [PubMed] [Google Scholar]