Abstract
Histological characteristics and clinical behaviour define lung neuroendocrine tumors (NETs), which are classified into four groups: typical (TC) and atypical carcinoids (AC), large-cell neuroendocrine carcinomas (LCNCs) and small-cell lung cancers (SCLCs). Historically, outcome and treatment of these rare neoplasms have been based on small, usually mono-institutional clinical series. Furthermore, their rarity makes quite impossible to design randomised clinical trial to compare different treatments especially in unusual clinical presentations. In 2012, the European Society of Thoracic Surgeons (ESTS) launched a new working-group, specifically dedicated to lung NETs, with the aim to develop modern knowledge on biology and behaviour of these tumors, and to disseminate it within the scientific community. A dedicated retrospective database was at first developed and sent to all the ESTS centres interested to this project. More than 2,000 operated NETs cases have been rapidly collected, and they represented the clinical substrate of several published scientific studies. The retrospective data collection intrinsic limitations in term of patients’ selection and treatment, along with the problem of possible missing data, were the reasons why the ESTS NETs working-group decided in 2015 to design and promote a new prospective database, employing the official ESTS platform. The aim of this review paper is to report the ESTS Lung NETs working-group history and to explain the architecture and use of the lung NETs databases.
Keywords: Lung, neuroendocrine tumors (NETs), outcome, retrospective database, prospective database
Introduction: the reasons for a choice
Neuroendocrine tumors (NETs) of the lung represent approximately 25% of all the neuroendocrine neoplasms of the human body (1,2). The 2015 World Health Organization (WHO) classification, by combining architectural tumor characteristics (cell size, organoid palisading rosettes and different nuclear/cytoplasm ratio) and additional histological parameters (different mitotic and proliferation indexes and presence of necrosis) classifies lung NETs into four different groups, with different biological behaviour, ranging from low-grade typical carcinoid (TC), to intermediate-grade atypical carcinoid (AC) and high-grade large-cell neuroendocrine carcinoma (LCNC) and small-cell lung cancer (SCLC) (3). NETs’ incidence has increased in the last decades, due, probably, to an improvement in diagnostic tools (especially histology and immunohistochemistry) and awareness, as well as to the dramatic diffusion of lung cancer screening programs worldwide. Currently, NETs’ incidence is reported to be up to 1.57/1,000,000/year (4,5). SCLC is the most common lung NET, with a 15% of invasive primary lung cancers; LCNC accounts for approximately 8% of resected lung tumors; bronchial carcinoids (TC + AC) are about 1% to 2% of all the primary lung cancers. Figure 1 shows NETs’ incidence, according their different histologies.
Figure 1.
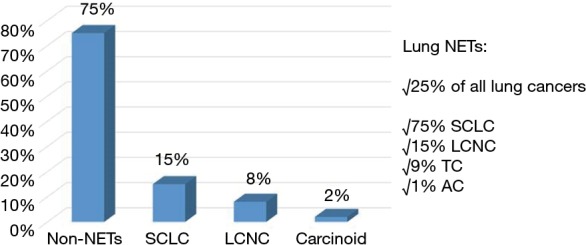
Lung NETs’ incidence according to their different histological subgroups. NETs, neuroendocrine tumors; TC, typical carcinoid; AC, atypical carcinoid; LCNC, large-cell neuroendocrine carcinoma; SCLC, small-cell lung cancer.
Several issues are currently matter of discussion concerning NETs biology: (I) the role of Ki-67 proliferation index to improve the prognostic tumor stratification; (II) the type of surgical resection, especially in early-stage tumors; (III) the role of endoscopic treatment in centrally located ones; (IV) the management of multicentric lesions; (V) the type and the length of postoperative follow-up; (VI) the management of advanced/metastatic NETs, according to their histologic subtype.
With the aim to give an answer to those questions, the European Society of Thoracic Surgeons (ESTS) Council approved and launched in 2012 a new working-group, specifically dedicated to the lung NETs, which was officially presented during the 20th European Conference on General Thoracic Surgery, held in Essen (Germany) between June 10th and 13th 2012, with the purpose of gathering a group of experts worldwide, developing knowledge on such rare neoplasms and disseminating it within the scientific community.
The group, chaired by Pier Luigi Filosso, designed a Steering Committee, composed by the following physicians: Pascal Alexandre Thomas, Federico Venuta, Mariano Garcia Yuste, Eric Lim, Alessandro Brunelli, Konstantinos Papagiannopoulos, Hisao Asamura and William Travis.
The first scientific initiative of the group was to design a survey on bronchial carcinoids’ management in rare and unusual clinical presentations, and to diffuse it amongst the ESTS members. A total of 172 centres worldwide replied to the questionnaire. There was a general agreement concerning the use of anatomic resections and parenchyma-sparing surgery, the importance of lymphadenectomy, the need for an adjuvant regimen in N+ ACs and the role of surgery for local recurrences. On the other hands, controversies emerged in the use of nuclear medicine imaging, the preoperative measurement of serum markers and the follow-up timing and characteristics (6).
A specific database was then designed, and sent to all the centres that showed interest to NETs management, in order to retrospectively collect as many cases as possible, in the shortest time possible. Up to 2014, more than 2,000 operated NETs cases were collected through 17 thoracic surgery institutions worldwide (Appendix 1 shows the list of participating centres), and the database was then used for several clinical studies.
The present review includes:
❖ A report of the history of the ESTS Neuroendocrine Tumours of the Lung Working Group and the ESTS neuroendocrine retrospective databases;
❖ An explanation of the architecture of the new ESTS neuroendocrine prospective database.
The ESTS lung NETs retrospective database
From June 2014, the ESTS lung NETs retrospective database project gathered many enthusiastic responses from the ESTS community. Data about more than 2,000 patients operated between 1994 and 2012 in 17 ESTS general thoracic surgery centres were collected. Mostly of the Institutions were from Europe, but also a renowned centre from the North America contributed to the data collection. So far, ESTS neuroendocrine retrospective database still represents one of the largest series of operated lung NETs ever collected. Overall survival (OS) and cumulative incidence of recurrence (CIR) were the first endpoints analysed (Figure 2A,B).
Figure 2.
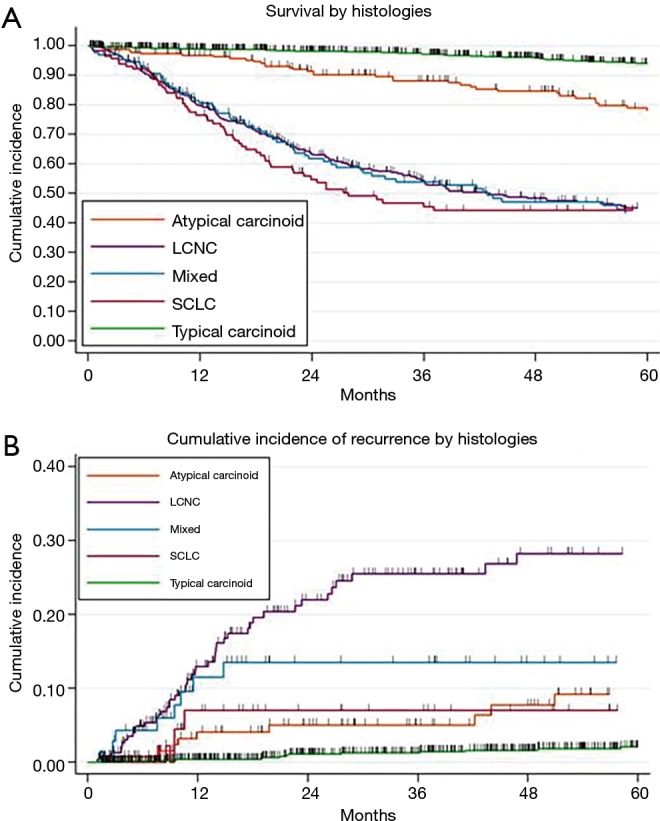
(A) Lung NETs OS curve and (B) CIR curve according to their different histologies. NETs, neuroendocrine tumors; OS, overall survival; CIR, cumulative incidence of recurrence; SCLC, small-cell lung cancer; LCNC, large-cell neuroendocrine carcinoma.
The retrospective database demonstrated to be a mine rich of information concerning the clinical management of such rare lung tumors. All those data were meticulously reported during the working-group annual business meetings, during the ESTS Annual Congresses, and proposals for future studies were also formally collected.
Several clinical studies were published, based on the lung NETs retrospective database.
One was an outcome comparison between intermediate and high-grade tumors (AC and LCNC) which, for the first time, were clinically compared (7). The results showed that age, tumor size and sublobar resections were independent negative prognostic factors influencing ACs’ OS. In LCNCs, advanced TNM stage negatively affected outcome. Furthermore, local recurrence or distant metastasis were significantly more common in LCNCs, as expected.
The second study was dedicated to elaborate a prognostic model of survival for TCs, by analysing the outcome of more than 1,100 operated cases (8). Backward selection resulted in a prediction model for mortality including age, gender, previous malignancies, peripheral tumour, TNM stage and ECOG PS. The final model showed a good discrimination ability with a C-statistic equal to 0.836 (bootstrap optimism-corrected 0.806) (Figure 3). This model was externally validated in 2016 by another International multicentre cohort study (9).
Figure 3.
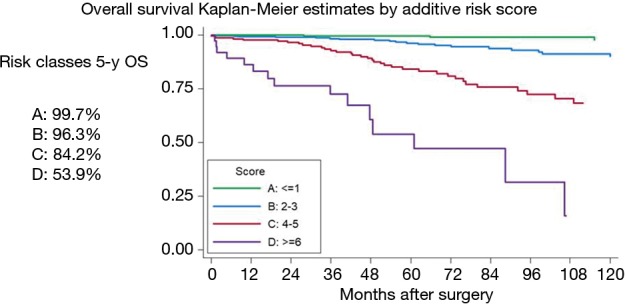
TCs OS curve by the risk scores. NETs, neuroendocrine tumors. TCs, typical carcinoids; NETs, neuroendocrine tumors; OS, overall survival.
The third publication was a review article about the management of advanced NETs (10), and it was the result of a satellite symposia on “Clinical Management of Lung NETs” organized by the ESTS Lung NETs working-group and held during the 21st European Conference on General Thoracic Surgery in Birmingham (UK), 2013.
Finally, the role and impact of adjuvant CT in LCNC was the object of an oral presentation at the 95th Annual Meeting of the American Association for Thoracic Surgery (AATS), in Seattle, on April, 2015. By analysing a series of 400 operated LCNCs, an evidence of a higher OS in patients receiving adjuvant CT (adjusted HR 0.73; 95% CI: 0.56–0.96, P=0.022) was observed. Therefore, although surgery remains the mainstay of curative options in LCNCs, a combination with other treatments (e.g., neoadjuvant or adjuvant CT ± RT) should be evaluated by future studies.
Nevertheless, a retrospective data collection presents intrinsic limitations related to patients’ selection and treatment bias, along with the problem of possible missing data. This was the reason why the ESTS NETs working-group decided to promote a new prospective database. In 2015 the ESTS Council accepted and launched the online lung NETs prospective database, employing the official ESTS platform.
One step beyond: the lung NETs prospective database
Stimulated by the encouraging scientific results of the retrospective dataset, in 2015 the ESTS Neuroendocrine Tumours of the Lung Working Group decided to promote a new prospective one, using the official ESTS platform; its represented one of the first satellite databases incorporated in the ESTS Core Registry.
The initial structure of the ESTS NETs prospective database has been replaced in 2016 with a brand-new platform.
This new format encompassed a new tool: the dashboard or Clinical Care Analysis (CCA). This resource, available for each contributor, produces a clear snapshot on the status of completeness rate of specific dataset fields, as well as the distribution of patients’ characteristics in the dataset.
Patients ‘records are included in the following five different Electronic Medical Record data sections, further divided into different subsections:
❖ The demographic section, in common with the “core” dataset and the other satellite databases;
❖ The “Preoperative” section, which also includes three subcategories: (I) risk factors (comorbidities, smoking history and pulmonary function evaluation); (II) medical history—(initial clinical presentation, anamnesis, possible presence of paraneoplastic syndromes, serum markers levels); (III) diagnosis and staging (pre-operative diagnosis and radiology reports; invasive diagnostic procedures);
❖ The “Operation” section, with two subcategories: (I) group definition (data concerning type of surgery, pathological staging according to the 8th edition of the IASLC/UICC/AJCC TNM classification system, resection status and Ki67%, immunohistochemical staining) (II) treatment [complementary treatment (CT, RT and/or biological therapy) and its intent (induction, adjuvant or palliative treatment)];
❖ The post-operative section (early- and intermediate-term outcomes. In particular, complication, date and outcome of discharge, possible hospital readmission and 30–90-day mortality);
❖ The “Follow-up” section (data concerning: patient vital status and oncological outcome, presence of possible local and/or distant tumour recurrence, possible second malignancy development).
The database’s architecture allows to each contributor to enter the dataset in different time, as soon as patients’ data become available. Actually, not all the fields had the same importance, and the missing data research and compilation represents a huge time-consuming activity. Consequently, in order to maximize the essential data collection necessary for future statistical analyses, a “minimum dataset” has been developed, according to the experience of other specific databases.
The contribution to the ESTS prospective neuroendocrine prospective database is intensely encouraged among all the ESTS Institutions. In Appendix 2, instructions to how to get access to the database are provided. Finally, it is very important to highlight that contributors could use ESTS neuroendocrine database as its internal online database, for free.
Up to now, more than 150 new lung NETs operated cases have been collected, and this represents a very rich substrate for future scientific projects.
Conclusions
The ESTS Lung NETs working-group in the last years has demonstrated to be scientifically very active. In particular, the development of a retrospective database allowed the publication of several clinical studies which highlighted outcome and prognostic factors for such rare neoplasms. The new prospective dataset is now available and its contribution is strongly encouraged among all the ESTS Institutions. Its diffusion will improve the number of collected operated cases and, therefore, this will represent an extraordinary opportunity to definitively point out biological characteristics, outcome and optimal treatment for such rare lung neoplasms.
Acknowledgements
None.
Appendix 1. List of ESTS Lung Neuroendocrine Working-Group contributors
Caterina Casadio and Ottavio Rena (Unit of Thoracic Surgery, “Amedeo Avogadro” University of Eastern Piedmont, Novara, Italy); Paula Moreno Casado and Antonio Alvarez (Department of Thoracic Surgery, University Hospital “Reina Sofia”, Cordoba, Spain); Dariusz Sagan (Unit of Thoracic Surgery, Medical University of Lublin, Lublin, Poland); Paolo Carbognani and Luca Ampollini (Thoracic Surgery, University Hospital of Parma, Parma, Italy); Nizar Asadi and Federico Stella (Unit of Thoracic Surgery, University of Bologna, Bologna, Italy); Mario Nosotti and Luigi Santambrogio (Unit of Thoracic Surgery, Hospital Maggiore Policlinico, University of Milan, Milan, Italy); Pascal Alexandre Thomas and Lucile Gust (Department of Thoracic Surgery, Lung Transplantation & Diseases of the Esophagus, Aix-Marseille University & Hospitals System of Marseille (AP-HM), Marseille, France); Cecilia Pompili# and Alessandro Brunelli# (Department of Thoracic Surgery, St. James’s University Hospital, Leeds, UK); Stefano Margaritora and Marco Chiappetta (Catholic University “Sacred Heart” Rome, Rome, Italy); Christian Roesel (Rurhlandklinik, Westgerman Lung Center, University Hospital, University of Duisburg-Essen, Duisburg, Germany); Erino Angelo Rendina and Giulio Maurizi (Fondazione Eleonora Lorillard Spencer Cenci, S. Andrea Hospital Rome, Sapienza University of Rome, Rome, Italy), Valentina Larocca (Department of Thoracic Surgery, Spirito Santo Hospital, Pescara, Italy); Francesco Ardissone (San Luigi Gonzaga Hospital, University of Torino, Orbassano, Torino, Italy); William D. Travis and Inderpal SARKARIA (Memorial Sloan Kettering Cancer Center, New York, USA); Gaetano Rocco (Pascale Foundation, Naples, Italy).
Appendix 2. Instructions for access to the online ESTS neuroendocrine prospective database
Eligibility criteria: ESTS active member (ESTS membership status is checked before providing database credentials)
Log in at http://www.ests.org;
Click on “Collaboration” → European Database;
Click on “Database Registration Form” → Registration Form;
Download the Registration form;
Complete the form with the required information and send it to the addresses provided (KData Clinical Administrators);
You will receive the credentials for your Institutions for logging into the Database;
Direct access to the ESTS Registry: log in at https://ests.kdataclinical.it.
Once logged into the database:
Click on “Search/Add” → “Add new patient”;
You need to complete the fields with the demographics data;
Then you will see a menu with the neuroendocrine sections (Preop Netts, Op Netts, Postop Netts, F.up Netts);
Start completing the fields.
# Dr. Pompili and Dr. Brunelli conducted this study while they were at the Unit of Thoracic Surgery Ospedali Riuniti, Ancona, Italy.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Rekhtman N. Neuroendocrine tumors of the lung: an update. Arch Pathol Lab Med 2010;134:1628-38. [DOI] [PubMed] [Google Scholar]
- 2.Korse CM, Taal BG, van Velthuysen ML, et al. Incidence and survival of neuroendocrine tumours in the Netherlands according to histological grade: experience of two decades of cancer registry. Eur J Cancer 2013;49:1975-83. 10.1016/j.ejca.2012.12.022 [DOI] [PubMed] [Google Scholar]
- 3.Travis WD, Brambilla E, Burke AP, et al. WHO Classification of Tumours of the Lung, Pleura, Thymus and Heart. Fourth edition. Lyon: International Agency for Research on Cancer, 2015. [DOI] [PubMed] [Google Scholar]
- 4.Modlin IM, Lye KD, Kidd M. A 5-decade analysis of 13,715 carcinoid tumors. Cancer 2003;97:934-59. 10.1002/cncr.11105 [DOI] [PubMed] [Google Scholar]
- 5.Yao JC, Hassan M, Phan A, et al. One hundred years after "carcinoid": epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol 2008;26:3063-72. 10.1200/JCO.2007.15.4377 [DOI] [PubMed] [Google Scholar]
- 6.Filosso PL, Guerrera F, Thomas P, et al. Management of bronchial carcinoids: international practice survey among the European Society of Thoracic Surgeons. Future Oncol 2016;12:1985-99. 10.2217/fon-2016-0092 [DOI] [PubMed] [Google Scholar]
- 7.Filosso PL, Rena O, Guerrera F, et al. Clinical management of atypical carcinoid and large-cell neuroendocrine carcinoma: a multicentre study on behalf of the European Association of Thoracic Surgeons (ESTS) Neuroendocrine Tumours of the Lung Working Group†. Eur J Cardiothorac Surg 2015;48:55-64. 10.1093/ejcts/ezu404 [DOI] [PubMed] [Google Scholar]
- 8.Filosso PL, Guerrera F, Evangelista A, et al. Prognostic model of survival for typical bronchial carcinoid tumours: analysis of 1109 patients on behalf of the European Association of Thoracic Surgeons (ESTS) Neuroendocrine Tumours Working Group. Eur J Cardiothorac Surg 2015;48:441-7; discussion 447. 10.1093/ejcts/ezu495 [DOI] [PubMed] [Google Scholar]
- 9.Cattoni M, Vallières E, Brown LM, et al. External Validation of a Prognostic Model of Survival for Resected Typical Bronchial Carcinoids. Ann Thorac Surg 2017;104:1215-20. 10.1016/j.athoracsur.2017.05.019 [DOI] [PubMed] [Google Scholar]
- 10.Filosso PL, Ferolla P, Guerrera F, et al. Multidisciplinary management of advanced lung neuroendocrine tumors. J Thorac Dis 2015;7:S163-71. [DOI] [PMC free article] [PubMed] [Google Scholar]


