Abstract
Cementoblastomas are rare benign odontogenic tumors. Diagnosis of these lesions must be made by an association of clinical, radiographic, and histopathological findings. Cementoblastomas rarely occur in both primary and permanent dentitions. We describe the sixth case of cementoblastoma in the literature with the involvement of both deciduous and permanent teeth. The aim of this case report is to present the clinicoradiopathologic features of a cementoblastoma in a 4.5-year-old boy with an unusual recurrence. The first clinical and radiographic features appeared on the deciduous mandibular second molar. The second lesion occurred 1 year after treatment at 5.5 years old, involving the permanent mandibular first molar, and a subsequent lesion was seen at age 8 years in the edentulous region of the extracted mandibular first molar. After the last surgery, there was no recurrence of the lesion at 6 months’ follow-up. Follow-ups of patients with cementoblastomas are highly recommended for an early detection of recurrences.
Keywords: Cementoma , Dentition , Mandible , Odontogenic tumors
What’s Known
Although cementoblastomas are very rare, they should be considered a differential diagnosis in both dentitions
What’s New
Only a few cases of cementoblastomas involving both deciduous and permanent dentitions have been reported in the literature.
Introduction
Cementoblastomas constitute a relatively uncommon benign odontogenic neoplasm of the jaw. The incidence of this neoplasm is relatively rare, 1 to 6.2% of all odontogenic tumors.1 These lesions are considered the only true neoplasm of a cementum origin2 and are defined as neoplasms characterized by the formation of sheets of a cementum-like tissue containing a large number of reversal lines and a lack of mineralization at the periphery of the mass or in the more active growth area. Their etiology is unknown. Cementoblastomas usually occur in the second or third decade of human life. The lesions most frequently tend to be associated with a permanent erupted tooth such as the first molar tooth and the second mandibular premolar tooth and are very rarely associated with impacted and deciduous teeth. To our knowledge, 5 cases of cementoblastoma with the involvement of deciduous and permanent teeth have been reported so far3-7 (table 1). We report the sixth case of cementoblastoma involving both deciduous and permanent teeth of a child with an unusual recurrence.
Table 1.
Reported cases of cementoblastomas associated with primary and permanent teeth
Case Presentation
A 4.5-year-old boy was referred to the Oral and Maxillofacial Surgery Department of Tehran University of Medical Sciences with the chief complaint of swelling and mild pain in the posterior right mandibular area. An informed signed consent was obtained from the parent of the patient. The familial and medical histories were not contributory, and no evidence of facial trauma was reported.
On extra oral examination, there was mild swelling of the right lower jaw leading to mild facial asymmetry. The swelling was bony hard in consistency.
An intraoral examination revealed buccal and lingual cortical expansion. The overlying mucosa was normal. A vitality test with an electrical pulp tester yielded a positive reaction for the deciduous mandibular second molar. There was no functional difficulty with speech, swallowing, and breathing.
On panoramic radiography, there was a well-defined capsulated non-homogenized radiopaque mass related to the apical region of the right deciduous mandibular second molar (figure 1). Another considerable situation was that the roots of the right first unerupted molar were developed in comparison with the opposite side and had unusual radiolucency with them.
Figure1.

Panoramic view of the lesion shows a well-defined radiopaque mass at the apical region of the right deciduous mandibular second molar. Notice the radiolucent rim around the lesion and more developed roots of the right first unerupted molar.
On the basis of the clinical and radiographic features, the differential diagnosis of this lesion included odontoma, cementoblastoma, and osteoblastoma. Considering the radiographic features based on the attachment to the tooth root, we ruled out osteoblastoma. However, microscopic examination was necessary to differentiate between odontoma and cementoblastoma. Surgical enucleation of the lesion, including the removal of the involved teeth, was planned and executed under general anesthesia.
The tumor mass was embedded in the root of the deciduous mandibular second molar tooth and had an irregular surface with a maximum dimension of 1.6 cm.
Histopathologic examination revealed sheets of a cementum-like material entrapped within the vascular connective tissue stroma (figure 2a). The intervening connective tissue stroma was loose and vascular. Prominent reversal lines were seen within the sheets of the cementum-like material. Numerous large cementoblasts were evident around the calcified materials (figure 2b). Based on these finding and considering the attachment of the lesion to the tooth root, we confirmed the diagnosis of cementoblastoma.
Figure2.

Microscopic features of the tumor are depicted here, showing a) sheets and trabeculae of a cementum-like material with a loose vascular stroma (H & E staining, ×100) and b) prominent reversal lines (black arrow) and numerous large cementoblasts (red arrows) around the cementum-like material (H & E staining, ×400).
Regular post-surgical follow-ups revealed a new lesion at age 5.5 with mild swelling. On panoramic evaluation, there were 2 circular homogenized well-defined and capsulated radiopaque masses related to both roots of the erupted first mandibular molar (figure 3a). Further surgery was done to remove the lesion and the associated tooth. The lesion presented the previous diagnosis and cementoblastoma was reported.
Figure3.
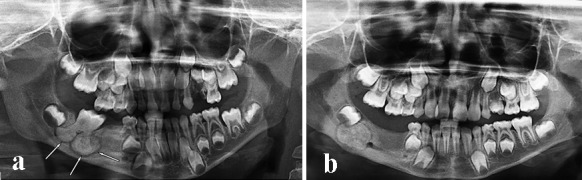
a) Panoramic view shows 2 radiopaque masses related to both roots of the mandibular first erupted molar. Notice the radiolucent rim around the lesion. b) Panoramic view shows the unusual recurrence of the lesion, a circular radiopaque mass in the edentulous region of the extracted mandibular first molar. Notice the radiolucent rim around the lesion.
At age 8 years, the patient was referred to the abovementioned department with a complaint of swelling at the previously mentioned location.
In the panoramic view, there was a circular capsulated homogenized radiopaque mass in the edentulous region of the extracted mandibular first molar (figure 3b). Local wide excision was performed under general anesthesia, and the recurrent lesion was harvested. Similar to the previous diagnosis, the lesion presented a benign cementoblastoma.
Given the unusual recurrences of the lesion after local wide lesion excision, we recommended a close follow-up of the patient. At 3 follow-ups of the patient at 3, 6, and 9 months after the last surgery, there was no evidence of recurrence fortunately.
Discussion
Cementoblastomas constitute a benign neoplasm of cementoblasts and represent the only true neoplasm of the cementum. They can be seen with the involvement of deciduous teeth, impacted molars, and multiple teeth as well.7 Ohki et al.5 reported a rare case of cementoblastoma involving multiple deciduous and permanent teeth including the second deciduous molar, first premolar, and the first and second permanent molars embedded in the crown and root of the right maxillary second premolar. Solomon et al.6 reported the youngest case of cementoblastoma involving both dentitions in 2012. Nonetheless, to the best of our knowledge, our presented case is younger than the other 5 cases having been reported thus far (table 1).
Pain, tenderness, and swelling can be seen obviously in most patients with cementoblastomas, although the lesion can be asymptomatic. The associated tooth is vital and often exhibits pain. Our case presented with a swelling with a mild pain in the posterior right mandibular area.
Some authors have determined 3 developmental stages for cementoblastomas. The first stage is that of a noncalcified matrix, which can be characterized by the formation of a circular radiolucent area in the region of the apex of a vital tooth. The second or cementoblastic stage is a stage in which a radiopaque material develops from the center to the peripheral region of the lesion. The third or maturation stage is the stage where the whole lesion is radiopaque while surrounded by a radiolucent rim.
In a review of 36 diagnosed cases of cementoblastoma by Brannon et al.,8 24 (66.7%) cases were radiopaque, 10 (27.7%) had mixed densities, and the remaining 2 (5.5%) were radiolucent. In our case, the lesion could be categorized into the maturation or third stage.
As the lesion matures, the differential diagnosis should include osteoblastoma, odontoma, hypercementosis, cemental dysplasia, and condensing osteitis as is discussed below:
1. Osteoblastomas have very similar clinical and radiographic findings, but tooth-mass continuity does not exist. Generally, the radiopacity of osteoblastomas is more irregular than that of cementoblastomas. However, the majority of osteoblastomas have persistent pain due to osteolytic borders.
2. Odontomes are usually not continuous to the root and also have heterogeneous radiopacity showing the presence of multiple dental tissues.
3. Hypercementoses are small lesions and are not followed by pain or jaw swelling.
4. A radiolucent band around a benign cementoblastoma is usually better defined and more uniform than that with cemental dysplasia.
5. Condensing osteitis is a well-defined radiopaque lesion that typically appears around the apex of a necrotic tooth root. Condensing osteitis does not have the peripheral radiolucent rim which is typical of cementoblastomas. It is an important feature insofar as it helps distinguish condensing osteitis from cementoblastomas.
Histologically, cementoblastomas reveal sheets of a cementum-like tissue demonstrating numerous reversal lines and active cementoblasts. The trabeculae of the cementum are attached to the root of the tooth. In addition to cementoblasts, cementoclasts are enclosed within the hard tissue or around the periphery of trabeculae.9 A capsule-like band of fibrous connective tissue at the periphery may be present.
Due to the lesion’s benign but locally aggressive nature, the first-choice treatment plan is complete removal of the lesion with the involved tooth. As a more conservative approach, maintenance of the associated tooth and removal of the lesion through a surgical endodontic technique has been reported. The approach of lesion excision without injuring the adjacent teeth can be used when the lesion is small in size, when a strategic tooth is involved, and when there is a sufficient crown-to-root ratio after apicoectomy.
We reported a case of cementoblastoma with the involvement of both deciduous and permanent teeth with an unusual recurrence 3 years after the last treatment, which was not seen in the previous reported cases with the involvement of both dentition systems.3-7
Cementoblastomas are regarded as benign neoplasms with a limitless growth potential but with little tendency to recur. However, evaluation of follow-up data in a case series reported by Brannon et al.8 and Nagvekar et al.10 showed a recurrence rate of about 37%, which in comparison with the recurrence rate of 5.9% from the other reported cases is considerably high.
In our case, regular post-surgical follow-ups revealed a new lesion at age 5.5 and a recurrence at age 8, three years after the last excision: an event not observed in the 5 previously reported cases in the literature.
Prognosis after the complete surgical excision of the tumor is excellent, but it is mandatory to follow up patients because of the wide range of recurrence in reported cases, especially the unusual recurrence in our presented case.
Conclusion
It is clear that the recurrence rate of cementoblastomas is much lower than that of more aggressive odontogenic tumors; nevertheless, many factors including some clinical features such as bone expansion may affect this phenomenon. Therefore, long-term follow-up must be performed due to the possibility of recurrence in these lesions.
Footnotes
Conflict of Interest: None declared.
References
- 1.Sumer M, Gunduz K, Sumer AP, Gunhan O. Benign cementoblastoma: a case report. Med Oral Patol Oral Cir Bucal. 2006;11:E483–5. [PubMed] [Google Scholar]
- 2.Neelakandan RS, Deshpande A, Krithika C, Bhargava D. Maxillary cementoblastoma--a rarity. Oral Maxillofac Surg. 2012;16:119–21. doi: 10.1007/s10006-011-0267-8. [DOI] [PubMed] [Google Scholar]
- 3.Chaput A, Marc A. A Case of Cementoma Localized on a Temporary Molar. SSO Schweiz Monatsschr Zahnheilkd. 1965;75:48–52. [PubMed] [Google Scholar]
- 4.Zachariades N, Skordalaki A, Papanicolaou S, Androulakakis E, Bournias M. Cementoblastoma: review of the literature and report of a case in a 7 year-old girl. Br J Oral Maxillofac Surg. 1985;23:456–61. doi: 10.1016/0266-4356(85)90031-2. [DOI] [PubMed] [Google Scholar]
- 5.Ohki K, Kumamoto H, Nitta Y, Nagasaka H, Kawamura H, Ooya K. Benign cementoblastoma involving multiple maxillary teeth: report of a case with a review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;97:53–8. doi: 10.1016/S1079210403005080. [DOI] [PubMed] [Google Scholar]
- 6.Solomon MC, Rehani Sh, Valiathan M, Rao L, Raghu AR, Rao NN, et al. Benign cementoblastoma involving multiple deciduous and permanent teeth of maxilla-a case report. Oral & Maxillofacial Pathology Journal. 2012;3(2):258–263. [Google Scholar]
- 7.Javed A, Hussain Shah SM. Giant Cementoblastoma Of Left Maxilla Involving A Deciduous Molar. J Ayub Med Coll Abbottabad. 2017;29:145–6. [PubMed] [Google Scholar]
- 8.Brannon RB, Fowler CB, Carpenter WM, Corio RL. Cementoblastoma: an innocuous neoplasm? A clinicopathologic study of 44 cases and review of the literature with special emphasis on recurrence. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93:311–20. doi: 10.1067/moe.2002.121993. [DOI] [PubMed] [Google Scholar]
- 9.Zaitoun H, Kujan O, Sloan P. An unusual recurrent cementoblastoma associated with a developing lower second molar tooth: a case report. J Oral Maxillofac Surg. 2007;65:2080. doi: 10.1016/j.joms.2006.06.288. [DOI] [PubMed] [Google Scholar]
- 10.Nagvekar S, Syed S, Spadigam A, Dhupar A. Rare presentation of cementoblastoma associated with the deciduous maxillary second molar. BMJ Case Rep. 2017;2017 doi: 10.1136/bcr-2017-221977. [DOI] [PMC free article] [PubMed] [Google Scholar]


