Abstract
The standard therapy for thyroid cancer is total or near total thyroidectomy, followed by the administration of radioactive iodine for remnant ablation or residual disease. Patients with radioiodine therapy are predisposed to second malignant neoplasms in organs such as central nervous system (CNS), breast, prostate, kidney, bone marrow, salivary gland, and digestive tract. Exposure to carcinogen including occupational and therapy related hazard, aging and genetic susceptibility are other causes of second primary cancers. The second primary malignancies are not uncommon and, nowadays, the prevalence of it is mildly increasing due to the increasing survival of cancer patients and advances in early diagnosis and therapeutic modalities. Here, we present a fifty-one-year-old man with papillary thyroid carcinoma (PTC), who developed chronic lymphocytic leukemia (CLL), renal cell carcinoma (RCC), and basal cell carcinoma (BCC) in 15-20 years after radioactive iodine therapy. Second primary tumors are increasing and environmental, genetic susceptibility and increase in survival of cancer patients are the major risk factors.
Keywords: Second primary cancer , Thyroid cancer , Renal cell carcinoma , Chronic lymphocytic leukemia , Basal cell carcinoma
What’s Known
The behavior of low-grade tumor and early detection of malignancy, and radioactive iodine in this case, causes four primary cancer with long-term survival.
What’s New
We present a rare case with metachronous quadruple multiple primary cancers of thyroid, kidney, skin, and blood with long-term survival
Introduction
Quadruple primary synchronous and metachronous neoplasms are very rare and the incidence of them has been reported as below 0.1%; however, a few cases have reported to date. The second primary malignancies are not uncommon and, nowadays, the prevalence of it is mildly increasing due to the increasing survival of cancer patients and advances in early diagnosis and therapeutic modalities.1
Thyroid cancer is one of the most common endocrine malignancies and the standard therapy for it is total or near total thyroidectomy, followed by the administration of radioactive iodine for remnant ablation or residual disease. Radiation exposure is a risk factor for developing second malignant neoplasm, but, in addition, many factors such as genetic abnormality and smoking may make the individual susceptible to develop a second cancer. Multiple factors including age, radio-sensitivity of organ, gender, and radiation dosage predict second malignant neoplasm at the time of radiation exposure. Most common organs predisposed to second malignant neoplasm after radioactive iodine ablation are nervoussystem, breast, prostate, Kidney, bone marrow, salivary gland, urinary, and digestive tract.2,3
Differentiating second primary malignancy from the metastatic recurrence of primary cancer is very important and has prognostic and therapeutic values. Comprehensive genomic profiling and histologic analysis have helped physicians in distinguishing metastatic recurrence from second Primary Cancer.1
We describe here an extremely rare case of metachronous quadruple primary cancer with papillary thyroid carcinoma (PTC) that developed chronic lymphocytic leukemia, basal cell carcinoma, and renal cell carcinoma, respectively, over a fifteen years period after radioiodine therapy.
Case Presentation
A fifty-one-year-old male patient was referred to Hematology department by an endocrinologist because of abnormal complete blood count. The patient had leukocytosis with dominant lymphocyte series and mild thrombocytopenia, also lymph node biopsy consistent with small lymphocytic lymphoma (Figures 1, 2). He had a positive history of papillary thyroid cancer, and thyroidectomy and radioiodine ablation with 175 mci was done for him fifteen years ago (Figure 3). Flow cytometry of peripheral blood revealed chronic lymphocytic leukemia. Because of an early stage of chronic lymphocytic leukemia (stage 1 Rai), the patient did not receive any medication and was followed only with complete blood count monitoring.
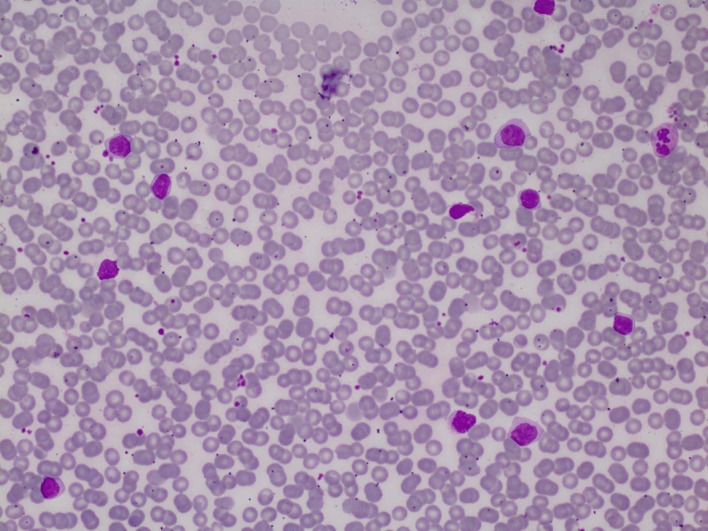
Figure1.
The figure shows Lymphocytosis caused by the proliferation of mature lymphocytes and few smudge cells. Other blood cells are unremarkable. Wright stain ×200
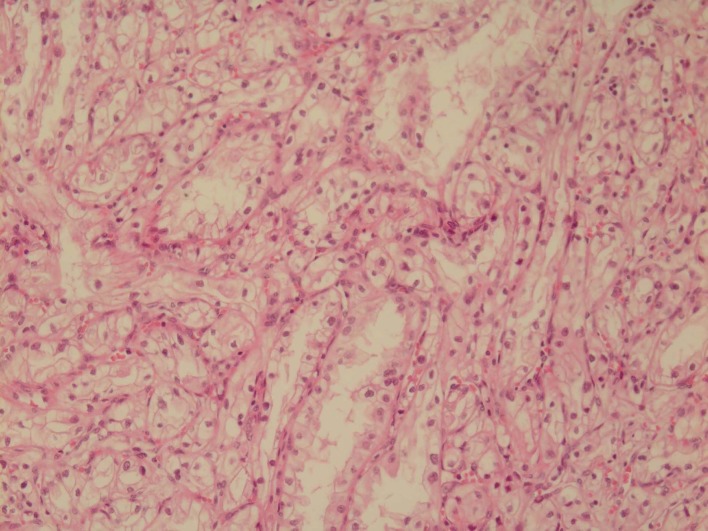
Figure2.
The figure shows a high view of lymph node shows diffuse proliferation of small lymphocytes, occasional prolymphocytes, and scanty mitotic figures. H&E ×400
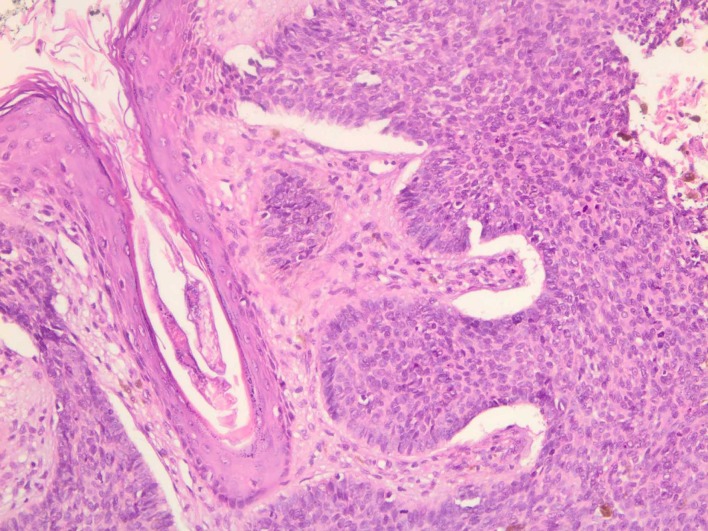
Figure3.
The figure shows a high view of papillary carcinoma metastatic to the lymph node. Surrounding lymphocytes are monotonous. H&E ×200
He had not had any problem for about 3.5 years until presented with right flank pain. Imaging study showed 2.5×2 cm tumoral lesion with different solid and cystic component in right lower pole of the right kidney without lymphadenopathy. The tumor was limited to mid pole of the right kidney without renal capsule or perirenal fat, so right radical nephrectomy with regional lymphadenectomy was done for him (Figure 4). Pathology revealed Renal Cell Carcinoma clear cell type.
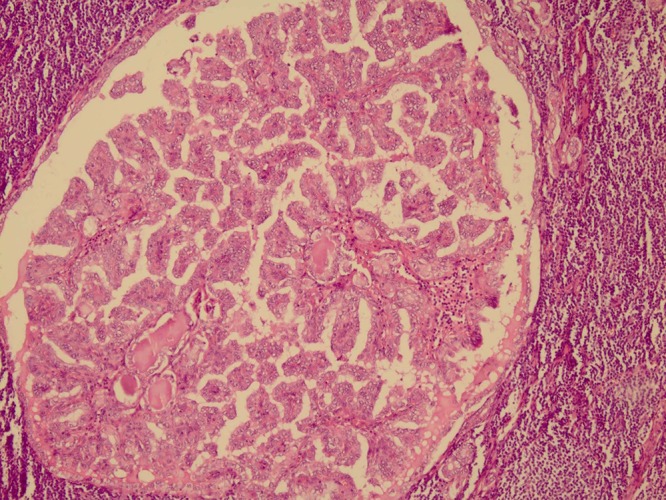
Figure4.
The figure shows Renal cell carcinoma, clear cell type. Tubules, nests, and sheets of clear cells with low-grade morphology could be seen. H&E ×200
3 months after nephrectomy, because of multiple pigmented lesions on the left and right side of the occiput, left posterior auricular, and neck area, excision with free margin was done for him and pathology was consistent with basal cell carcinoma (Figure 5). The patient fulfilled the written informed consent and we reported this case with the permission of the patient.
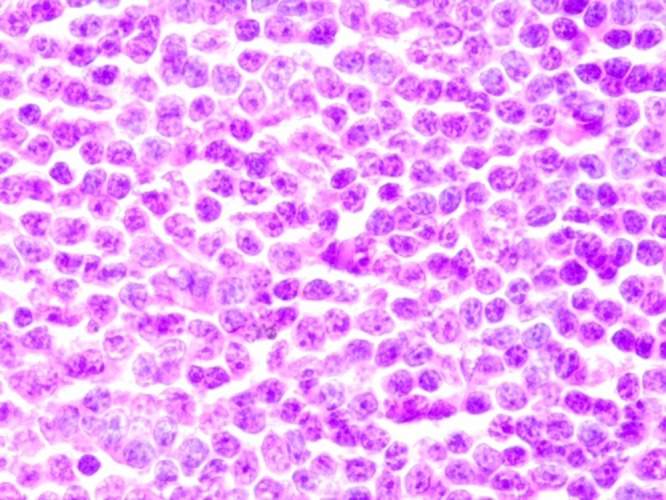
Figure5.
The figure shows a high power view of the basal cell carcinoma with nests of basaloid cells showing high nuclear to cytoplasmic ratio, high mitotic count, and peripheral palisading of nuclei. H&E ×200
Discussion
The occurrence of second and multiple primary cancers is increasing. Because of new diagnostic and therapeutic strategies, patients with underlying malignancy have long-term survival.
Median interval between the first and second malignancy was 3.41 (range 0.24-18.30) years. In children, overall cumulative incidence of second malignant neoplasm is 4.4% to 5.3% during twenty years’ surveillance. It is important that the overall five-year survival for second primary malignancy was lower than that of primary malignancies.5
Quadruple synchronous primary neoplasms are very rare with only four cases reported to date, though metachronous multiple primary malignancies are not extremely rare as multiple synchronous primary cancers. Exposure to carcinogen, including occupational and therapy-related hazards such as topoisomerase II inhibitor, lenalidomide, ionizing radiation that is a potent carcinogen by inducing DNA damage, is a cause of multiple primary tumors. One of the most important factors that predisposes patients to new cancer is aging. It is insinuated that DNA methylation and a number of stem-cell divisions in different tissue during aging may contribute to tumor formation.2Radioactive iodine ablation is the standard treatment for papillary thyroid cancer after surgery in high-risk patients and selected patients in low-risk group with high risk of recurrence or death. For successful remnant ablation in low-risk and high-risk patients, a minimum activity of 30-100 mci and 100-200 mci is recommended, respectively. Second primary malignancies are a concern related to radioiodine treatment. Several reports have suggested a possible relationship between I-131 administration and occurrence of some types of second primary malignancies; however, the findings are not consistent across studies.3
In a systematic review by Clement and colleagues, the incidence of second primary malignancies after radioiodine therapy was reported 2.7% to 8.7% during 7-13 years surveillance.3-5 This study confirms that the incidence of second primary malignancies after treatment with I-131 for thyroid cancer increased significantly. The most common second primary malignancies reported are breast and digestive tract cancers. Some organs concentrate radioiodine including breast, digestive tract, and urinary system whereas others express sodium iodine symporter, making them susceptible to malignant transformation.6 The study by Kuan-Yin Ko and colleagues revealed that the incidence of second primary malignancy was marginally higher in iodine-treated patients compared to those without iodine treatment. Urinary system, head, and neck cancer were the most reported cancers in this study. 7
Khang and colleagues showed a significantly increased risk of developing second primary malignancies in patients who had been treated with I-131 activity more than1000 mci/37 GBq19. When the cumulative dose of radioiodine exceeded 40 GBq (1.08 Ci), the odds of occurring second primary malignancies was radically increased.8
Although chemotherapy and radiotherapy cause second malignancy in a dose-dependent manner, genetic susceptibility causes different effects. Patients who harbor genetic mutations in highly penetrant genes such as RB (associated with retinoblastoma) or TP53 (associated with Li-Fraumeni syndrome) have high rate of SMNs in irradiated tissues. Low-penetrance genes are likely to be associated with a greater number of therapy-related SMNs. Family history, aging, race, and exposure to electromagnetic fields are risk factors for chronic lymphocytic leukemia. The other risk factors are exposure to petroleum, metals, pesticides/chemical fertilizers, detergents, and medical radiation.9
The latent period for the development of leukemia is reported to be in the range of 5-10 years and about 10-60 years for solid tumors. In renal cell carcinoma, the most important risk factors are older age, obesity, smoking, hypertension, and certain inherited syndromes.10
In our case, the patient developed CLL, BCC, and RCC in a duration between 15-20 years after radioiodine therapy. There are reports pointing to a relationship between BCC and RCC and radioiodine therapy but not CLL. In addition, patients with CLL are predisposed to second malignancy with the highest rate including melanoma, non-melanoma skin cancer, lung, other respiratory tract, oral cavity, pharynx, prostate, kidney, and lymphoma. The development of three cancers after radioactive iodine for PTC in this patient made him a choice for our case report.
One of the most important aspects of this case for the occurrence of multiple metachronous primary cancers is the presence of cancer with an indolent course and lesser aggression and also the presence of cancer in the early stage of the disease. It provides the opportunity to develop a new cancer in the propitious patient in long-term duration. One of the other reasons for this problem is the close follow-up in the patient with confirmed malignancy that can help us in the detection of cancer in the early stage of the disease.
Conclusion
Second primary tumors are increasing and environmental, genetic susceptibility, and an increase in the survival of cancer patients are the major risk factors. The indolent and less aggressive tumors can be present in a patient simultaneously or in separate time lapses in patients that are predisposed to developed cancer. So, they need long-term surveillance, including regular visits, history taking and physical exam, urinalysis, complete blood counts, CXR, and abdominopelvic sonography.
Footnotes
Conflict of Interest: None declared.
References
- 1.Weinberg BA, Gowen K, Lee TK, Ou SI, Bristow R, Krill L, et al. Comprehensive Genomic Profiling Aids in Distinguishing Metastatic Recurrence from Second Primary Cancers. Oncologist. 2017;22:152–7. doi: 10.1634/theoncologist.2015-0511. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Meeks MW, Grace S, Chen Y, Petterchak J, Bolesta E, Zhou Y, et al. Synchronous Quadruple Primary Neoplasms: Colon Adenocarcinoma, Collision Tumor of Neuroendocrine Tumor and Schwann Cell Hamartoma and Sessile Serrated Adenoma of the Appendix. Anticancer Res. 2016;36:4307–11. [PubMed] [Google Scholar]
- 3.Lim JW, Yeap FS, Chan YH, Yeoh AE, Quah TC, Tan PL. Second Malignant Neoplasms in Childhood Cancer Survivors Treated in a Tertiary Paediatric Oncology Centre. Ann Acad Med Singapore. 2017;46:11–9. [PubMed] [Google Scholar]
- 4.Behjati S, Gundem G, Wedge DC, Roberts ND, Tarpey PS, Cooke SL, et al. Mutational signatures of ionizing radiation in second malignancies. Nat Commun. 2016;7:12605. doi: 10.1038/ncomms12605. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rubino C, De Vathaire F, Dottorini M, Hall P, Schvartz C, Couette J, et al. Second primary malignancies in thyroid cancer patients. Br J Cancer. 2003;89:1638. doi: 10.1038/sj.bjc.6601319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gandhi S, Abhyankar A, Basu S. Dual malignancies in the setting of differentiated thyroid carcinoma: their synchronous or metachronous nature, impact of radioiodine treatment on occurrence of second malignancy and other associated variables. Nucl Med Commun. 2014;35:205–9. doi: 10.1097/MNM.0000000000000033. [DOI] [PubMed] [Google Scholar]
- 7.Ko KY, Kao CH, Lin CL, Huang WS, Yen RF. 131)I treatment for thyroid cancer and the risk of developing salivary and lacrimal gland dysfunction and a second primary malignancy: a nationwide population-based cohort study. Eur J Nucl Med Mol Imaging. 2015;42:1172–8. doi: 10.1007/s00259-015-3055-0. [DOI] [PubMed] [Google Scholar]
- 8.Fallahi B, Adabi K, Majidi M, Fard-Esfahani A, Heshmat R, Larijani B, et al. Incidence of second primary malignancies during a long-term surveillance of patients with differentiated thyroid carcinoma in relation to radioiodine treatment. Clin Nucl Med. 2011;36:277–82. doi: 10.1097/RLU.0b013e31820a9fe3. [DOI] [PubMed] [Google Scholar]
- 9.Wood ME, Vogel V, Ng A, Foxhall L, Goodwin P, Travis LB. Second malignant neoplasms: assessment and strategies for risk reduction. J Clin Oncol. 2012;30:3734–45. doi: 10.1200/JCO.2012.41.8681. [DOI] [PubMed] [Google Scholar]
- 10.Chow WH, Dong LM, Devesa SS. Epidemiology and risk factors for kidney cancer. Nat Rev Urol. 2010;7:245–57. doi: 10.1038/nrurol.2010.46. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]