Abstract
Brazil’s Sistema Único de Saúde, or Unified Health System policy, has delivered major improvements in health coverage and outcomes, but challenges remain, including the rise of non-communicable diseases (NCDs) and variations in quality of care across the country. Some of these challenges may be met through the adaptation and implementation of a South African primary care strategy, the Practical Approach to Care Kit (PACK). Developed by the University of Cape Town’s Knowledge Translation Unit (KTU), PACK is intended for in-country adaptation by employing a mentorship model. Using this approach, the PACK Adult guide and training materials were localised for use in Florianópolis, Santa Catarina, Brazil, as part of an initiative to reform primary care, expand care for NCDs and make services more accessible and equitable. The value of the collaboration between the KTU and Florianópolis municipality is the transfer of skills and avoidance of duplication of effort involved in de-novo guide development, while ensuring that materials are locally acceptable and applicable. The collaboration has informed the development of the KTU’s PACK mentorship package and led to a relationship between the groups of developers, ensuring ongoing learning and research, with the potential of assisting the further scale-up of PACK in Brazil.
Keywords: public health, health policy, health systems
Summary box.
The Practical Approach to Care Kit (PACK) programme, which has been developed, tested and scaled up in South Africa provides locally applicable, evidence-informed guidance and training for clinicians working in primary healthcare facilities.
Health officials in Florianópolis, Brazil recognised that the PACK programme might strengthen primary care services through provision of integrated comprehensive guidance for health workers.
Through a process of mentorship between the Knowledge Translation Unit in Cape Town and health workers from Florianópolis, a localised version of the PACK Adult guide and training materials for use in Brazil were developed.
Lessons learnt from this collaboration have informed the development of a PACK localisation package to mentor adaptation of the PACK programme for other countries.
Introduction
The centrepiece of Brazil’s Sistema Único de Saúde or Unified Health System is the Family Health Strategy, which aims to provide comprehensive primary care delivered by multidisciplinary teams.1 The scale-up of these teams has been rapid; by June 2018, 43 384 teams covering over 134 million people, or almost 65% of Brazil’s population, had been established.2 Despite improved health outcomes like a decrease in under-five mortality3–6 and reduced hospital admissions,7–9 there are continuing challenges. These include a rise in non-communicable diseases (NCDs)3 and variations in the quality of primary care, with unequal distribution of health workers, high turnover and poor management.10 Integrated provision of clinical care by doctors and nurses has improved accessibility and efficiency of primary care.11 However, a restrictive legal framework has hampered clinical practice by nurses12 and may have contributed to diverting their role toward administrative rather than clinical responsibilities.13
Florianópolis, a city of 486 000 in Santa Catarina state,14 was the first municipality in Brazil to achieve universal health coverage and has received awards for healthcare innovations.15 16 However, the quality of care between its clinics remains variable and barriers to access persist.17 This prompted a primary care reform in 2010, which targeted timely access to quality comprehensive care. The Primary Care Services Portfolio,18 published in 2014, introduced changes in the organisation of primary care, including the redefinition of roles within the health team.18 In parallel, new nursing protocols were developed that provided for additional legal and technical support for the scope of practice for nurses.19 This reform prompted a search for tools suited to the practice of primary care, including integrated clinical guidance and South Africa’s Practical Approach to Care Kit (PACK) programme was identified as potentially suitable.
The PACK programme comprises four components: (1) a clinical decision support tool (the PACK Global Adult guide), which provides a comprehensive and integrated approach to common presenting symptoms and chronic conditions among adults attending primary care in low-income and middle-income countries (LMICs),20 21 (2) a training and implementation strategy, that employs a cascade model for scaling up and an onsite, team-based training approach informed by adult education principles,22 (3) a health system strengthening component and (4) monitoring and evaluation elements. Developed and tested by the University of Cape Town’s Knowledge Translation Unit (KTU) over almost two decades,23 the programme has been adopted by South Africa’s department of health as part of the Ideal Clinic initiative24 to improve and standardise primary healthcare. It has been introduced in primary care facilities throughout South Africa, reaching over 30 000 primary care health workers. Four randomised controlled trials have shown modest but consistent improvements across multiple health outcomes,25–28 and qualitative work has shown improved job satisfaction among health workers.29 30
This paper describes the localisation of the PACK programme to the Florianópolis primary healthcare context and highlights the learnings from this experience. This paper forms part of a Collection of reports in which the development and methods employed in PACK are described.
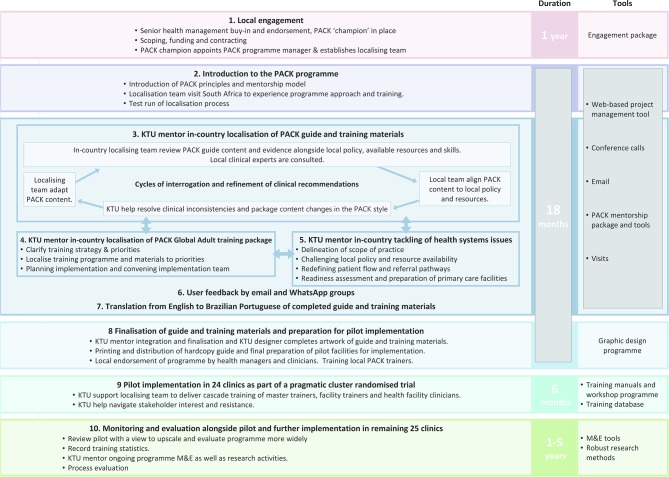
Localisation of PACK using a mentorship model
A goal of the PACK programme is to provide comprehensive, evidence-informed and policy-aligned clinical guidance at the point of care that addresses the needs of end-users and trains them to use it in their daily practice. To achieve this, the guide content and training programme needs to be localised to fit the context for which it is being developed. The PACK mentorship model is described more fully elsewhere31 but includes localisation of the PACK guide and training programme, addressing local health system issues, user testing and initial implementation and evaluation. Although an earlier version of PACK, known by a different name (PALSA—Practical Approach to Lung Health South Africa),32 33 had been localised for Minas Gerais state in Brazil (PAL GARD),34 Mexico (Programa AIRE),35 Malawi (PALM),36 the Gambia (PALSA PLUS Gambia)37 and PACK in Botswana (PACK Botswana),38 the Florianópolis version was the first time a mentorship model was used. Figure 1 provides details of this mentorship process, and figure 2 shows the timelines involved.
Figure 1.
Step-by-step mentorship of Practical Approach to Care Kit programme localisation and initial implementation in Brazil.
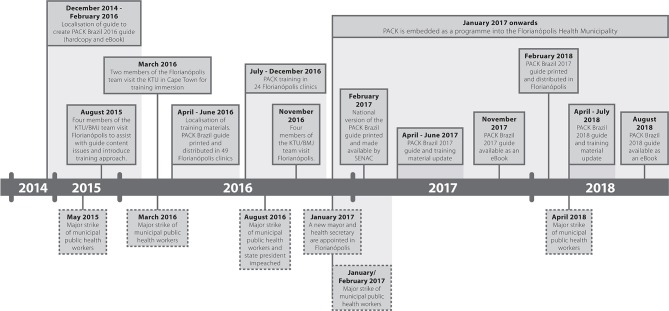
Figure 2.
Timeline of localisation, initial implementation and updating of Practical Approach to Care Kit in Brazil.
Mentorship was performed almost exclusively remotely, by email, an online project management tool (Trello) and teleconference calls, with only three face-to-face opportunities. Early in the process, KTU members visited Florianópolis to introduce the in-country mentees to the PACK principles and style of guide presentation, to discuss content issues and introduce the training approach. Following completion of the guide, the Florianópolis team members visited Cape Town for an immersion training course, in order to experience first-hand the PACK training principles in action. The third occasion was during the initial implementation stage, when a KTU team visited Florianópolis to review the successes and challenges of the programme, and plan further evaluation.
Localisation of the guide
A KTU content mentor (CW) worked closely with an in-country team led by a local family physician (RZ) over 14 months to complete the 103-page PACK guide for Florianópolis.
The generic PACK Global Adult guide content, was divided into 13 clinical sections, uploaded onto Trello, and each page of each section was reviewed and revised through an iterative process of consultation between the KTU mentor and mentees in Florianópolis. The localising team worked off editable localisation templates of the English guide provided by the KTU. The evidence underpinning each recommendation in the PACK Global Adult guide was provided in an Evidence and Decision Support document developed by the KTU in collaboration with the British Medical Journal (BMJ) Knowledge Centre.20 For the Florianópolis version, the team reviewed both this document and municipal and national guidelines and protocols listed in figure 3. The local team then engaged with local health workers and stakeholders to ensure that final decisions on content were applicable and acceptable for Florianópolis.
Figure 3.
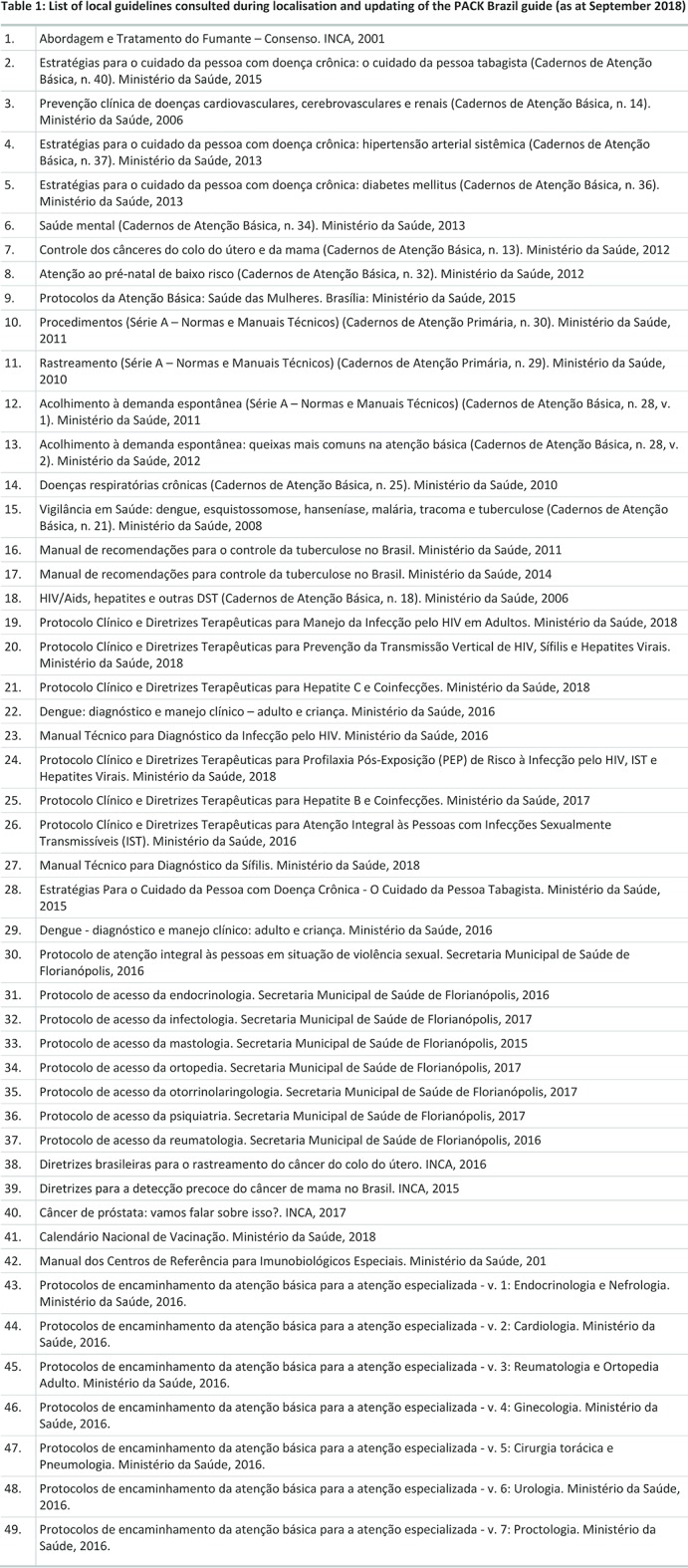
List of local guidelines consulted during localisation and updating of the PACK Brazil guide (as at September 2018).
For the Florianópolis version, additional pages were developed to address health issues that were not already covered in the PACK Global Adult guide. These were for the promotion of preventive care and screening (“General health assessment”) and for support for tobacco cessation (“Tobacco use”). These topics were prompted by patient requests for “a general check-up” and the fact that medications for tobacco cessation were available to patients attending primary care facilities in Florianópolis. A recent Zika virus outbreak in Brazil necessitated the inclusion of reference to this infection on relevant symptom pages (for example “Eye symptoms” and “Skin symptoms”) and in the maternity care section. Throughout the guide, along with clarifying referral pathways, a page detailing referral protocols was added to standardise patient referrals from primary to secondary care, a particular challenge faced in Florianópolis. Many of these content additions have since been integrated into the Global and subsequent localisations of the PACK Adult guide.39 40 An example of recommendations that were omitted in the Florianópolis version was the use of GeneXpert testing for suspected tuberculosis, as this is not part of local practice.
An important aspect of PACK is an emphasis on a team approach to care and task sharing. This is achieved by clear identification in the guide of the roles of each cadre of health worker. The standard approach is to colour code each medication in the text according to local prescribing authority for each cadre; for example, nurse, doctor or both. In the Florianópolis guide, this was extended to identify the authority to request investigations, perform procedures and refer patients.
The first PACK Brazil Adult guide (called PACK Brasil Adulto - Versão Florianópolis) was completed and published as an A4 hardcopy booklet in April 2016. Following its release, a national version was developed and made available later in 2016 through Serviço Nacional de Aprendizagem Comercial (Senac),41 a Brazilian government publication and professional education institution. This version, created to better reflect national protocols, was developed by the Florianópolis team, in collaboration with the KTU and Senac clinical editors.
Since the first guide in 2016, annual updates of both the PACK Brazil Adult Florianópolis and national versions for 2017 and 2018 have been developed by the team in Florianópolis, assisted by the KTU, to reflect updated evidence, revised local policies and needs and modifications prompted by user feedback. Electronic versions of each edition have also been made.
Localisation of the training and implementation materials
The PACK training approach has been successfully used to scale-up PACK and its predecessors in South Africa and is detailed in another paper in this Collection.22 Localisation of the PACK training and implementation materials took place over a 3-month period, beginning in April 2016. These included training manuals and activities, case scenarios and key messages.
The localising team were already familiar with adult educational principles and outreach training strategies used by PACK, however, they had limited experience of applying them in practice, instead relying on traditional didactic-style lectures. As recommended by the KTU, the PACK model of continuous on-site, in-service training in regular 1 to 2- hour sessions, employing interactive small group learning techniques guided by facilitators, was adopted. This prompted the KTU to develop additional PACK training materials, including a training video,42 to better communicate this approach.
An important step in PACK training localisation was to prioritise the content of training, as it is not possible to cover all the contents of the guide in the initial 12 session PACK training course. In Florianópolis, this decision was informed by research on the demand for clinical services in Florianópolis,43 and a review of ICD-9 codes recorded for clinic visits. The topics selected included tuberculosis, which was being decentralised from hospital to primary care, and back pain, which accounted for a large proportion of primary care visits among adults. A decision to use interprofessional pairs of doctors and nurses to support training predated the introduction of PACK. However, PACK’s clarity around roles and PACK training helped to translate this into practice.
After delivering an initial 12 on-site training sessions, training pairs visited clinics monthly. Content queries were addressed during these sessions and sometimes new content requested; for example, a new training case scenario on dengue fever. Engagement between the localising team and primary care health workers using PACK in Florianópolis is ongoing via email and through a mobile app group (WhatsApp Messenger). Health workers are encouraged to question guide recommendations and provide feedback on training and systems issues.
Evaluation and research
Within 22 months of the start of the PACK programme, 26 training sessions had been delivered to 160 health workers in 24 clinics in Florianópolis between August 2016 and June 2018. Training in some clinics was delayed by municipal strike action, but despite interruptions, training coverage is high with 100% of eligible health workers exposed to at least one training session, and 70% having completed all 12 initial training sessions.
The effectiveness of the PACK training approach on patient care and outcomes (specifically diabetes, cardiovascular and respiratory endpoints) is being compared with passive dissemination of the PACK guide in a randomised evaluation.44 Electronic medical record data for more than 350 000 medical and nursing primary care consultations per year are being used, rarely available in LMIC settings. Outcomes are currently being analysed.
Our previous research has suggested that local professional rules, work conditions, support with implementation of guidelines and local health system issues have a significant impact on the implementation and outcomes of the PACK programme.29 45 Currently, a process evaluation in Florianópolis involving PACK trainers, trained health workers and local PACK programme leads, is assessing the acceptability, feasibility and uptake of the programme among primary care practitioners.46 Preliminary findings suggest a positive response to the PACK programme.
Challenges and learnings
Tackling the language difference
Localisation of guide content was performed in English using the English PACK Global Adult guide as a template. This enabled KTU mentorship of the process, which was highly valued by the localising team, and made possible by their bilingualism. Following content finalisation, local health workers performed translation of the English version of the PACK Brazil guide into Brazilian Portuguese. Owing to limitations of time and funding, professional translators could not be employed, and back translation to check the validity of the translation was not performed. Subsequent updates to the guide and training materials have been based on the Brazilian Portuguese versions with correspondence in English for any content-related queries. New content has been co-developed by the localising team and KTU mentor in English and then translated. In future non-English localisations, it will be important to consider the localising team’s ability to engage in English and the need for professional and bilateral translation processes to ensure complete fidelity of the content.
Local ownership
Our experience with Florianópolis confirms that intense engagement between mentors and the in-country localising team is essential during initial stages of adaptation and implementation but then diminishes with each annual update, as the local team gains skill and experience and the PACK guide becomes locally owned. However, mentors emphasise and local teams accept the importance of both clinical feedback from local end-users, particularly for updates, and support from the global PACK community to assist with queries and share updates and improvements to the programme.
Overcoming interprofessional challenges
New local clinical protocols to expand nurses’ roles to include NCD care evoked resistance from some nurses to the increased scope of practice and additional duties, and from some doctors who perceived it as a threat to their role. These attitudes were identified as potential challenges to PACK uptake at the clinic level, but the delineation of prescriber levels and clinical roles provided both clarity and confidence and general acceptance of the new nursing protocols. In addition, the joint learning and clinical discussion created by the PACK doctor–nurse training pairs helped to reduce doctor resistance to task sharing with nurses. Along with management commitment to address existing legal and policy barriers to teamwork, this was important to achieving task sharing and uptake of the programme.
Prompting health systems change
Engagement with local stakeholders throughout the development process provided the means for identifying and addressing health system barriers, and for facilitating rapid implementation and embedding of PACK into the local health system. It also provided the opportunity to make changes in clinical management practices, question the availability of certain medications and equipment and change the scope of practice at the primary care level—issues that are directly relevant to individual clinical practice. Examples include reducing the frequency of blood pressure checks in well-controlled hypertensives, access to urine dipsticks, optimising the duration of antibiotics for bacterial sinusitis and deciding when to refer newly diagnosed diabetic patients (Box 1). Ongoing discourse between programme leads, local health workers and managers has resulted in an engaged community of practice empowered to debate clinical recommendations within a context of co-learning and development.
Box 1. Adapting diabetes care recommendations for Practice Approach to Care Kit (PACK) Brazil.
During the adaptation of the pages on diabetes care, two issues that could be addressed in PACK were identified. First, the development of clinical protocols for care delivered by nurses, and second, the need to review referral pathways to specialised care. The introduction of PACK was identified by local health authorities as an opportunity to address these processes. For example, a discussion arose about nurses’ authority to initiate intravenous saline solution without a medical order. This led to the decision to colour-code not only medications, but examinations, procedures and tests as well. Thus, PACK came to serve as the comprehensive reference source for defining the roles of doctors and nurses in primary care, placing pressure on the nursing protocols to adopt task sharing and a greater role of nurses. A further example of this process was prompted by discussion on the feasibility and need to refer all diabetic patients younger than 35 years of age to specialist care. This led to the decision to create a page about appropriate reasons for referral, describing criteria for referral and referral pathways (for example, urgent/non-urgent specialist consultation, teleconsultation and emergency referral). In this way, small changes in the PACK diabetes pages served as a prototype of bottom-up, clinically driven health system change.
In addition, the PACK experience in Florianópolis led to the embedding of PACK in the management structures of the Florianópolis municipal Clinical Management Department, to lead the development of evidence-based technical documents, protocols and guidelines. Although creation of a specific post may not be viable for all LMIC settings, dedicated units (such as NCD units in local health ministries as laid out by the WHO Global NCD Action Plan 2013–202047), may prove suitable for embedding PACK within health systems.
Political instability
Localisation and implementation of the PACK programme in Brazil was, and continues to be, affected by an unpredictable period in Brazil, marked by austerity measures and political instability with frequent changes to health leadership and policies.48 Figure 2 depicts episodes of upheaval during the localisation and initial implementation of PACK Brazil. The localising team’s full engagement with the PACK programme resulted in better than expected uptake despite these issues. However, they continue to present a challenge to the rollout of PACK more broadly across Brazil.
Funding and upscale
Since 2016, the KTU in partnership with the BMJ and the Florianópolis team, have continued to invest effort in producing an annual update of the PACK Brazil guide and training materials. In the absence of designated funds, this work is driven by the high level of commitment from both teams to see the PACK programme used to support quality primary care throughout Brazil. Although PACK is a low-cost intervention, this situation is not sustainable, and the sourcing of funds for the PACK Global programme, particularly for LMICs, remains a critical objective.
Next steps
The PACK programme continues to form part of primary care in Florianópolis and results from the process evaluation and trial will provide a greater understanding of its effectiveness. Following the release of the national version of the guide, there are ongoing discussions at federal, state and municipal levels as well as with various non-governmental organisations and private healthcare providers in the hope of actualising broader scale up of the PACK programme across Brazil. In addition, there is potential for expansion of the localised PACK programme in Brazil to include other components of the PACK “suite”; for example, a guide for children and adolescents,49 and for lay health workers.
Conclusion
The localisation and implementation of PACK Adult for Florianópolis is an example of skills transfer and “south–south” collaboration, resulting in the production of a programme that is evidence-informed and locally acceptable, applicable and scaleable. The importance of adapting guidelines to each local context is recognised as a critical step in the development and implementation of best practice guidelines in LMICs, yet these countries often lack the skills and resources to perform this activity and are reliant on outside support. Consequently, such programmes often fail or become outdated. In contrast, PACK originates in such a country and has been effectively implemented and progressively improved in South Africa for almost two decades. The PACK Florianópolis experience illustrates that the programme is capable of export to other continents and across language barriers using a mentorship model. While it remains to be seen whether the PACK programme will be more widely adopted in Brazil, and be sustainable, its initial uptake and the new skills and enthusiasm of those that are supporting its updating and further development, suggest a positive future.
The PACK Florianópolis experience has also provided valuable insights and improvements that will be used in collaborations with other countries wishing to adopt this approach.
bmjgh-2018-001016supp001.docx (36KB, docx)
Acknowledgments
We would like to acknowledge all the health workers in Florianópolis who have contributed to and helped to keep the PACK programme in Florianópolis alive, and the former Health Secretary of Florianópolis, Daniel Moutinho, for his support of the programme. We would like to thank Ricardo Cypreste and the GARD Alliance for profiling the work of PACK more broadly within Brazil.
Footnotes
Handling editor: Seye Abimbola
Contributors: LF, JZ: established the partnership between the KTU and the Florianópolis Health Department, with support from EB, AC, RS, TE. LF: raised funding to cover the KTU contribution through a grant provided by the Peter Sowerby Foundation. JZ: obtained approval from the relevant Health Department officials to cover the Florianópolis Health Department contribution. CW, RZ: led the localisation of the guide with support from RC, JZ, MA. RZ, MA: led on localisation of the training materials and training implementation, with support from the KTU training team, including DG-P, LA. MB, EB, RS, AC: are leading the randomised trial evaluation. SN: the process evaluation. CW: wrote the first draft of the paper. All authors contributed intellectual content, edited the manuscript and approved the final version for submission.
Funding: Florianópolis Health Municipality for in-kind support, The Peter Sowerby Foundation for funding to support the evidence linkage and PACK Global Localisation Toolkit development in partnership with Brazil, and BMJ for overall project management support.
Competing interests: We have read and understood BMJ policy on declaration of interests and declare that CW, LF, TE, DGP, LA, RC and EB are employees of the KTU. TE reports grants from Peter Sowerby Foundation and personal fees from BMJ, during the conduct of the study. TD is an employee of the South African Medical Research Council. RZ and MA are employees of the City Health Department, Florianópolis, Brazil. JZ is an ex-employee of the City Health Department, Florianópolis, Brazil and a current holder of full-time PhD studentship from the Brazilian research agency CNPq. AC reports grants, personal fees and non-financial support from GSK, personal fees and non-financial support from AstraZeneca, personal fees and non-financial support from Boehringer Ingelheim, personal fees and non-financial support from MEDA, personal fees and non-financial support from Novartis, personal fees and non-financial support from EUROFARMA, personal fees and non-financial support from CHIESI, personal fees and non-financial support from Boston Scientific, outside the submitted work. EB reports grants to institution for clinical trials from Novartis, Boehringer Ingelheim, Merck, Takeda, GlaxoSmithKline, Hoffmann le Roche, Actelion, Chiesi, Sanofi-Aventis, Cephalon, TEVA, and AstraZeneca and personal fees from ICON, Novartis, Cipla, Vectura, Cipla, Menarini, ALK, ICON, Sanofi Regeneron, Boehringer Ingelheim and AstraZeneca, outside the submitted work, and is a Member of Global Initiative for Asthma Board and Science Committee. Since August 2015, the KTU and BMJ have been engaged in a non-profit strategic partnership to provide continuous evidence updates for PACK, expand PACK-related supported services to countries and organisations as requested, and where appropriate license PACK content. The KTU and BMJ co-fund core positions, including a PACK Global Development Director, and receive no profits from the partnership. PACK receives no funding from the pharmaceutical industry. This paper forms part of a Collection on PACK sponsored by the BMJ to profile the contribution of PACK across several countries towards the realisation of comprehensive primary health care as envisaged in the Declaration of Alma Ata, during its 40th anniversary.
Patient consent: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1. Macinko J, Harris MJ. Brazil's family health strategy–delivering community–based primary care in a universal health system. N Engl J Med 2015;372:2177–81. 10.1056/NEJMp1501140 [DOI] [PubMed] [Google Scholar]
- 2. Cobertura da Atenção Básica. Available from: https://egestorab.saude.gov.br/paginas/acessoPublico/relatorios/relHistoricoCoberturaAB.xhtml [accessed Sep 2018].
- 3. França EB, Passos VMA, Malta DC, et al. Cause-specific mortality for 249 causes in Brazil and states during 1990-2015: a systematic analysis for the global burden of disease study 2015. Popul Health Metr 2017;15:39 10.1186/s12963-017-0156-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Paim J, Travassos C, Almeida C, et al. The Brazilian health system: history, advances, and challenges. The Lancet 2011;377:1778–97. 10.1016/S0140-6736(11)60054-8 [DOI] [PubMed] [Google Scholar]
- 5. Rocha R, Soares RR. Evaluating the impact of community-based health interventions: evidence from Brazil's Family Health Program. Health Econ 2010;19(S1):126–58. 10.1002/hec.1607 [DOI] [PubMed] [Google Scholar]
- 6. Aquino R, de Oliveira NF, Barreto ML. Impact of the family health program on infant mortality in Brazilian municipalities. Am J Public Health 2009;99:87–93. 10.2105/AJPH.2007.127480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Macinko J, Dourado I, Aquino R, et al. Major expansion of primary care in Brazil linked to decline in unnecessary hospitalization. Health Aff 2010;29:2149–60. 10.1377/hlthaff.2010.0251 [DOI] [PubMed] [Google Scholar]
- 8. Rasella D, Harhay MO, Pamponet ML, et al. Impact of primary health care on mortality from heart and cerebrovascular diseases in Brazil: a nationwide analysis of longitudinal data. BMJ 2014;349:g4014 10.1136/bmj.g4014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the global burden of disease study 2010. Lancet 2012;380:2095–128. 10.1016/S0140-6736(12)61728-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Victora CG, Barreto ML, do Carmo Leal M, et al. Health conditions and health-policy innovations in Brazil: the way forward. Lancet 2011;377:2042–53. 10.1016/S0140-6736(11)60055-X [DOI] [PubMed] [Google Scholar]
- 11. Miclos PV, Calvo MCM, Colussi CF. Avaliação do desempenho das ações e resultados em saúde da atenção básica. Revista de Saúde Pública 2017;51:1–10.28099550 [Google Scholar]
- 12. Martiniano CS, Andrade PSde, Magalhães FC, et al. Legalization of nurse prescribing of medication in brazil: history, trends and challenges. Texto & Contexto - Enfermagem 2015;24:809–17. 10.1590/0104-07072015001720014 [DOI] [Google Scholar]
- 13. Feliciano KV, Kovacs MH, Sarinho SW. Overlapping of duties and technical autonomy among nurses of the Family Health Strategy. Rev Saude Publica 2010;44:520–7. [DOI] [PubMed] [Google Scholar]
- 14. Estimativas da população residente no Brasil e unidades da federação com data de referência em 1° de julho de. Available from: ftp://ftp.ibge.gov.br/Estimativas_de_Populacao/Estimativas_2017/estimativa_dou_2017.pdf [accessed Sep 2018].
- 15. da Cruz AM, Oliveira MIR. Estudo para Redimensionamento de Auxiliares Administrativos nas Unidades Básicas de Saúde da Secretaria Municipal. Prêmio INOVASUS 2013;81. [Google Scholar]
- 16. Saraiva S, Cremonese E. Implantação do modelo de apoio matricial em saúde mental no município de Florianópolis, SC III Concursonacional de experiências em saúde da família: trabalhos premiadosBrasília. Brasil Ministério da Saúde, 2008. [Google Scholar]
- 17. Giovanella L, de Mendonça MH, de Almeida PF, et al. Family health: limits and possibilities for an integral primary care approach to health care in Brazil. Cien Saude Colet 2009;14:783–94. [DOI] [PubMed] [Google Scholar]
- 18. Prefeitura municipal de florianópolis secretaria municipal de saúde gabinete do secretário. Available from: http://www.pmf.sc.gov.br/arquivos/arquivos/pdf/29_11_2016_16.17.33.73c009e15b1538cd39469d1b7ec80eb2.pdf [accessed Sep 2018].
- 19. Protocolos de enfermagem. Available from: http://www.pmf.sc.gov.br/entidades/saude/index.php?cms=protocolos+de+enfermagem&menu=10&submenuid=1478 [accessed Sep 2018].
- 20. Cornick R, Picken S, Wattrus C, et al. The Practical Approach to Care Kit (PACK) guide: developing a clinical decision support tool to simplify, standardise and strengthen primary healthcare delivery. BMJ Glob Health 2018;3(Suppl 5):e000962 10.1136/bmjgh-2018-000962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Mash B, Fairall L, Adejayan O, et al. A morbidity survey of South African primary care. PLoS One 2012;7:e32358 10.1371/journal.pone.0032358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Simelane ML, Georgeu-Pepper D, Ras CJ. The Practical Approach to Care Kit (PACK) training programme—scaling up and sustaining support for health workers to improve primary care. BMJ Global Health 2018;In press. doi: 10.1136/bmjgh-2018-001124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Fairall L, Bateman E, Cornick R, et al. Innovating to improve primary care in less developed countries: towards a global model. BMJ Innov 2015;1:196–203. 10.1136/bmjinnov-2015-000045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ideal clinic South Africa. Available from: https://www.idealclinic.org.za/ [accessed Sep 2018].
- 25. Fairall LR, Zwarenstein M, Bateman ED, et al. Effect of educational outreach to nurses on tuberculosis case detection and primary care of respiratory illness: pragmatic cluster randomised controlled trial. BMJ 2005;331:750–4. 10.1136/bmj.331.7519.750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Zwarenstein M, Fairall LR, Lombard C, et al. Outreach education for integration of HIV/AIDS care, antiretroviral treatment, and tuberculosis care in primary care clinics in South Africa: PALSA PLUS pragmatic cluster randomised trial. BMJ 2011;342:d2022 10.1136/bmj.d2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Fairall L, Bachmann MO, Lombard C, et al. Task shifting of antiretroviral treatment from doctors to primary-care nurses in South Africa (STRETCH): a pragmatic, parallel, cluster-randomised trial. Lancet 2012;380:889–98. 10.1016/S0140-6736(12)60730-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Fairall LR, Folb N, Timmerman V, et al. Educational outreach with an integrated clinical tool for nurse-Led non-communicable chronic disease management in primary care in South Africa: a pragmatic cluster randomised controlled trial. PLoS Med 2016;13:e1002178 10.1371/journal.pmed.1002178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Georgeu D, Colvin CJ, Lewin S, et al. Implementing nurse-initiated and managed antiretroviral treatment (NIMART) in South Africa: a qualitative process evaluation of the STRETCH trial. Implement Sci 2012;7:66 10.1186/1748-5908-7-66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Stein J, Lewin S, Fairall L, et al. Building capacity for antiretroviral delivery in South Africa: a qualitative evaluation of the PALSA PLUS nurse training programme. BMC Health Serv Res 2008;8:240 10.1186/1472-6963-8-240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Cornick R, Eastman T, Wattrus C. Crossing borders: the PACK experience of spreading a complex health system intervention across low and middle-income countries. BMJ Global Health 2018. In press: doi: 10.1136/bmjgh-2018-001088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Bheekie A, Buskens I, Allen S, et al. The Practical Approach to Lung Health in South Africa (PALSA) intervention: respiratory guideline implementation for nurse trainers. Int Nurs Rev 2006;53:261–8. 10.1111/j.1466-7657.2006.00520.x [DOI] [PubMed] [Google Scholar]
- 33. Demonstration project - South Africa. Available from: http://www.who.int/gard/countries/demonstration_project_south_africa/en/ [accessed Sep 2018].
- 34. Cruz AA, Camargos PA, Urrutia-Pereira M, et al. Global Alliance against Chronic Respiratory Diseases (GARD) Brazil success case: overcoming barriers. J Thorac Dis 2018;10:534–8. doi:10.21037/jtd.2018.01.40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Pérez-Padilla R. Hacia un programa de prevención y atención primaria de enfermedades respiratorias, AIREa (Acción Integrada por la Respiración). Neumología y Cirugía de Tórax 2012;71:244–9. [Google Scholar]
- 36. Schull MJ, Cornick R, Thompson S, et al. From PALSA PLUS to PALM PLUS: adapting and developing a South African guideline and training intervention to better integrate HIV/AIDS care with primary care in rural health centers in Malawi. Implement Sci 2011;6:82 10.1186/1748-5908-6-82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Analytical summary - Tuberculosis. Available from: http://www.aho.afro.who.int/profiles_information/index.php/Gambia:Analytical_summary_-_Tuberculosis [accessed Sep 2018].
- 38. Tsima BM, Setlhare V, Nkomazana O. Developing the Botswana primary care guideline: an integrated, symptom-based primary care guideline for the adult patient in a resource-limited setting. J Multidiscip Healthc 2016;9:347–54. 10.2147/JMDH.S112466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Awotiwon A, Sword C, Eastman T. Using a mentorship model to localise the Practical Approach to Care Kit (PACK): from South Africa to Nigeria. BMJ Global Health 2018;In press: doi: 10.1136/bmjgh-2018-001079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Mekonnen Y, Hanlon CFS, Cornick R. Using a mentorship model to localise the Practical Approach to Care Kit (PACK): from South Africa to Ethiopia. BMJ Global Health 2018; In press: doi: 10.1136/bmjgh-2018-001108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. PACK Brasil Adulto: kit de cuidados em atenção primária. Available from: http://www.editorasenacsp.com.br/portal/produto.do?appAction=vwProdutoDetalhe&idProduto=22689 [accessed Sep 2018].
- 42. PACK Training video. Available from: https://youtu.be/b1fgr7pCYJA (accessed Sep 2018)
- 43. Gusso GDF. Diagnóstico de demanda em Florianópolis utilizando a Classificação Internacional de Atenção Primária: 2° edição (CIAP-2). Universidade de São Paulo, 2009. [Google Scholar]
- 44. Bachmann MO, Bateman ED, Stelmach R, et al. Integrating primary care of chronic respiratory disease, cardiovascular disease and diabetes in Brazil: Practical Approach to Care Kit (PACK Brazil): study protocol for randomised controlled trials. J Thorac Dis 2018;10:4667–77. doi:10.21037/jtd.2018.07.34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Uebel K, Guise A, Georgeu D, et al. Integrating HIV care into nurse-led primary health care services in South Africa: a synthesis of three linked qualitative studies. BMC Health Serv Res 2013;13:171 10.1186/1472-6963-13-171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Davies VF. Formative study of the implementation of the Practical Approach to Care Kit in Brazil (PACK BRAZIL). Manuscript submitted for publication2018.
- 47. World Health Organization Global Action Plan for the Prevention and Control of NCDs 2013-2020. Geneva, Switzerland: WHO Press, 2013. [Google Scholar]
- 48. Massuda A, Hone T, Leles FAG, et al. The Brazilian health system at crossroads: progress, crisis and resilience. BMJ Glob Health 2018;3:e000829 10.1136/bmjgh-2018-000829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Picken S, Hannington J, Fairall L. PACK Child: the development of a practical guide to extend the scope of integrated primary care for children and young adolescents. BMJ Global Health 2018. In press: doi: 10.1136/bmjgh-2018-000957. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2018-001016supp001.docx (36KB, docx)