Abstract
Hepatic artery aneurysms are rare and sometimes life-threating. Various treatments for hepatic artery aneurysms, including surgical and endovascular techniques are present. Here, we report the case of a 68-year-old woman who presented with an about 9 cm of common hepatic artery aneurysm detected during a routine medical checkup; she did not exhibit any symptoms. We successfully treated the aneurysm with transcatheter arterial embolization with isolation technique via pancreatic duodenal arcade.
Keywords: Common hepatic artery aneurysm, Transcatheter arterial embolization, Isolation technique via pancreaticoduodenal arcade
Introduction
Hepatic artery aneurysms are rare and account for 20% of visceral aneurysms [1]. They are often detected incidentally by imaging investigations for other conditions without symptoms [2]. Approximately 20%-30% of hepatic artery aneurysms may rupture and cause sudden abdominal pain and life-threating conditions [3]. Common treatment options for hepatic artery aneurysms include surgical and endovascular techniques. The treatment modalities for hepatic artery aneurysms depend on the clinical presentation, associated risk factors, and general status of the patient [4]. Additionally, the location and size of the aneurysm are commonly considered [5]. Herein, we report the case of giant common hepatic artery (CHA) aneurysm successfully treated by transcatheter arterial embolization (TAE) with isolation technique via pancreaticoduodenal arcade.
Case
A 68-year-old woman presented to our hospital due to a suspicion of pancreatic head tumor detected by ultrasonography during her medical checkup. She had received medications for schizophrenia. She had no previous history of abdominal surgery, trauma, or hypertension and had given birth twice. Her initial laboratory data appeared to be normal without anemia. Clinical examination revealed normal blood pressure and physical examination showed no significant problems.
To evaluate suspicious pancreatic head tumor, a contrast-enhanced computed tomography (CT) was performed that revealed an about 9 cm of CHA aneurysm with mural thrombosis and calcification (Fig. 1). Volume rendering 3D well displayed the aneurysm and no branch from the aneurysm (Fig. 2). Distal side of CHA showed to be intact. TAE was planned to prevent rupture. The aneurysm was too large and costly to treat with packing of its sack with coils, and there was no branch from the aneurysm. We believed that the isolation technique would be effective because the aneurysm was located in CHA, and there was sufficient collateral flow from the pancreaticoduodenal arcade.
Fig. 1.
A contrast-enhanced computed tomography showing a giant common hepatic artery aneurysm.
Fig. 2.
Volume rendering showing the aneurysm and the distal side of the common hepatic artery and no branch from the aneurysm.
The right common femoral artery was punctured under local anesthesia, and a 5-Fr cobra-shaped guiding catheter was inserted into the common trunk of the celiac artery and the superior mesenteric artery (SMA). Digital subtraction angiography (DSA) from the common trunk revealed CHA aneurysm. The guiding catheter was inserted into the aneurysm, and DSA from the aneurysm revealed the distal side of CHA and no other branches from the aneurysm (Fig. 3). We attempted to advance a 1.9-Fr micro catheter (Prograte λ19, Terumo Clinical Supply, Gifu, Japan) into the distal side of CHA through the aneurysm, with no success. Therefore, as an alternative, the left common femoral artery was punctured under local anesthesia, and a 5-Fr sheath introducer was inserted. A 4-Fr Shepherd hook-shaped catheter was inserted into the SMA. A 2.0-Fr micro balloon catheter (LOGOSSWITCH, Piolax Medical Devices Inc, Kanagawa, Japan) was advanced to the proximal side of the CHA and was inflated to occlude the artery. Subsequently, DSA from SMA was performed and it revealed the distal side of the CHA via very fine pancreaticoduodenal arcade (Fig. 4).
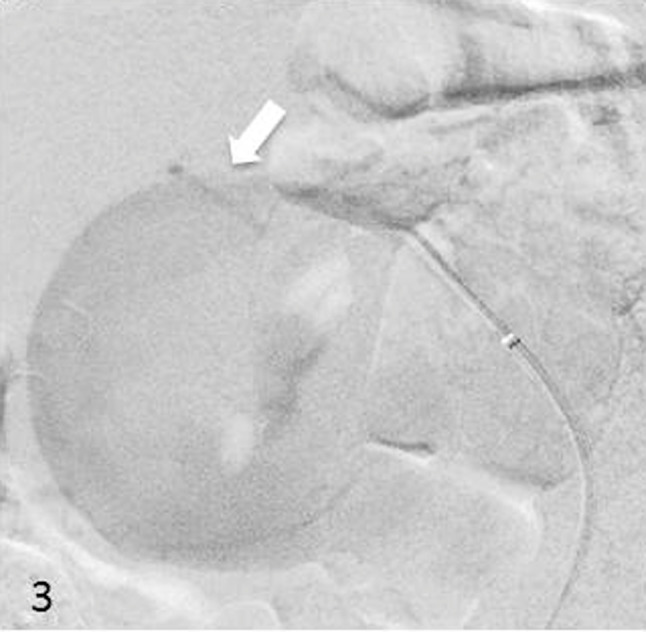
Fig. 3.
Digital subtraction angiography from the aneurysm revealing the distal side of the common hepatic artery (arrow).
Fig. 4.
Digital subtraction angiography from the superior mesenteric artery showing the distal side of the common hepatic artery via very fine pancreaticoduodenal arcade (arrow head) with the common hepatic artery balloon occluded (arrow).
After deflating the balloon, a 1.9-Fr micro catheter was advanced to the distal side of CHA via very fine pancreaticoduodenal arcade. To embolize the distal side of CHA, we used 1-fibered pushable coil (Tornade; Cook Medical, Bloomington, Indiana) and 3 bare puchable coils (C-stopper coil; Piolax Medical Devices Inc, Kanagawa, Japan).
Finally, we used a 6 mm Amplazer Vascular Plug Ⅳ (AVP; St. Jude Medical, St. Paul, MN) to embolize the proximal side of CHA, which resulted in complete embolization of the giant hepatic aneurysm with this isolation technique (Fig. 5). After the procedure, she had no complications and was subsequently discharged 10 days after TAE. A follow-up contrast-enhanced CT after 8 months after the treatment showed complete occlusion and reduction of the CHA without complications (Fig. 6).
Fig. 5.
Using 4 platinum coils to embolize the distal side of the aneurysm (arrow) and a 6 mm Amplazer Vascular Plug Ⅳ to embolize the proximal side of the aneurysm (arrowhead) resulted in complete embolization of the giant hepatic aneurysm with isolation technique.
Fig. 6.
Follow-up noncontrast computed tomography (A) and contrast-enhanced computed tomography (B) after 8 months revealed complete occlusion and downsizing of the common hepatic aneurysm (arrow).
Discussion
Hepatic artery aneurysms are rare and accounts for about 0.002% [6]. They are the second most common visceral aneurysms after splenic artery aneurysms, and they occur more in males than in females. The aneurysms are often located in the extrahepatic artery with the most common location being CHA demonstrated in 63% of cases. There are various etiologies and atherosclerosis accounts for about 30%. Trauma, iatrogenic injury, vasculitis, and fibromuscular dysplasia are known as other causes [7].
Almost all hepatic artery aneurysms are asymptomatic and they are often detected incidentally. The risk of rupture of hepatic artery aneurysms is reported to be 20%-30% and causes life-threating conditions when ruptured [3]. Because of this risk, the indication for treatment includes on symptomatic aneurysm, nonatherosclerotic aneurysms, pseudoaneurysm, and atherosclerotic aneurysm >2 cm [6], [8]. Abdominal contrast-enhanced CT and magnetic resonance imaging can diagnose hepatic artery aneurysms in most cases, however selective catheter angiography is the gold standard for diagnosis and for therapeutic intervention [9].
Treatment options for hepatic artery aneurysms include surgical and endovascular techniques. Selection of the most appropriate treatment depends on its location of the aneurysm, clinical presentation, risk factors of rupture, and general condition of the patient [3]. The use of endovascular techniques for the treatment of hepatic artery aneurysms is gradually becoming more frequent because they are less invasive and reduce hospital stay and pain.
Endovascular techniques include isolation, packing, and stent placement technique. Visceral aneurysms are commonly treated with coil embolization using isolation or packing techniques.
Balderi et al reported that coil embolization was the preferred technique in 84% of the patients [10]. Isolation technique occludes arteries that flow into and out of an aneurysm. It is used to treat aneurysms of relatively large size, multiple aneurysms, and aneurysms of false wall. If branch vessels arise from the aneurysm sac, this technique is not effective because of possibility of the feeding by retrograde flow. A complication linked to this technique is organ infarction at the distal side in cases with insufficient collateral flow.
Packing technique is commonly used to embolize an aneurysm. This technique preserves blood flow at the distal side and prevents organ infarction. Complications associated with this technique include coil compaction and difficulty in treating an aneurysm of false wall due to the risk of rupture [11]. Moreover, this technique is not cost-effective when treating large aneurysms.
Multilayer stents and stent graft are also used for the treatments of the hepatic artery aneurysms [2], [10], [12]. Placement of a stent may preserve the flow of the affected artery; however, they cannot be placed in tortuous lesions and require a normal-caliber artery on either side of the aneurysm to seal the stent graft [13]. Complications associated with the use of stent placement technique include stent fracture, fragment migration, endleak, stent thrombosis, and risk of stent occlusion as a result of intimal hyperplasia [14], [15], [16].
In the present case, we considered that isolation technique would be an effective strategy because of location of the aneurysm (CHA), large size of the aneurysm, absence of branching, and sufficient collateral flow from the pancreaticoduodenal arcade. We attempted to advance the catheter into the distal side of CHA through the aneurysm; however, we encountered difficulty due to the large size of the aneurysm. Therefore, we opted to treat the aneurysm through the very fine pancreaticoduodenal arcade with isolation technique using coils and the Amplatzer plug. The procedure was successful, without any complications.
Conclusion
We successfully treated giant CHA aneurysm by TAE. In patients with difficulty of packing technique and antegrade isolation technique, TAE using retrograde isolation technique via pancreaticoduodenal arcade can be effective treatment option for CHA aneurysm.
Footnotes
Conflict of Interest/Disclosure Statement: All authors declare that they have no conflicts of interest.
References
- 1.Kantarci M., Karakaya A., Aydinli B., Yalcin Polat K., Ceviz M. Giant hepatic artery aneurysm causing portal hypertension. Dig Liver Dis. 2009;41(12):913. doi: 10.1016/j.dld.2008.09.004. [DOI] [PubMed] [Google Scholar]
- 2.Hashim A., Allaqaband S., Bajwa T. Leaking hepatic artery aneurysm successfully treated with covered stent. Catheter Cardiovasc Interv. 2009;74(3):500–505. doi: 10.1002/ccd.22012. [DOI] [PubMed] [Google Scholar]
- 3.Kim J.H., Rha S.E., Chun H.J., Kim Y.S., Oh S.N., Lee Y.J. Giant aneurysm of the common hepatic artery: US and CT imaging findings. Abdom Imaging. 2010;35(2):212–214. doi: 10.1007/s00261-009-9501-3. [DOI] [PubMed] [Google Scholar]
- 4.Sessa C., Tinelli G., Porcu P., Aubert A., Thony F., Magne J.L. Treatment of visceral artery aneurysms: description of a retrospective series of 42 aneurysms in 34 patients. Ann Vasc Surg. 2004;18(6):695–703. doi: 10.1007/s10016-004-0112-8. [DOI] [PubMed] [Google Scholar]
- 5.Cavalcante R.N., Couto V.A., da Fonseca A.V., de Miranda R.B., Costa A.J., Correa J.A. Endovascular treatment of a giant hepatic artery aneurysm with Amplatzer vascular plug. J Vasc Surg. 2014;60(2):500–502. doi: 10.1016/j.jvs.2013.06.077. [DOI] [PubMed] [Google Scholar]
- 6.Abbas M.A., Fowl R.J., Stone W.M., Panneton J.M., Oldenburg W.A., Bower T.C. Hepatic artery aneurysm: factors that predict complications. J Vasc Surg. 2003;38(1):41–45. doi: 10.1016/s0741-5214(03)00090-9. [DOI] [PubMed] [Google Scholar]
- 7.Erben Y., De Martino R.R., Bjarnason H., Duncan A.A., Kalra M., Oderich G.S. Operative management of hepatic artery aneurysms. J Vasc Surg. 2015;62(3):610–615. doi: 10.1016/j.jvs.2015.03.077. [DOI] [PubMed] [Google Scholar]
- 8.Riesenman P.J., Bower T.C., Oderich G.S., Bjarnason H. Multiple hepatic artery aneurysms: use of transcatheter embolization for rupture. Ann Vasc Surg. 2006;20(3):399–404. doi: 10.1007/s10016-006-9025-z. [DOI] [PubMed] [Google Scholar]
- 9.Ferrara D., Giribono A.M., Viviani E., Padricelli A., Santagata A., Del Guercio L. Endovascular management of a large hepatic artery aneurysm. La Clinica terapeutica. 2017;168(3):e178–e180. doi: 10.7417/T.2017.2001. [DOI] [PubMed] [Google Scholar]
- 10.Balderi A., Antonietti A., Ferro L., Peano E., Pedrazzini F., Fonio P. Endovascular treatment of visceral artery aneurysms and pseudoaneurysms: our experience. La Radiologia medica. 2012;117(5):815–830. doi: 10.1007/s11547-011-0776-4. [DOI] [PubMed] [Google Scholar]
- 11.Yamamoto S., Hirota S., Maeda H., Achiwa S., Arai K., Kobayashi K. Transcatheter coil embolization of splenic artery aneurysm. Cardiovasc Intervent Radiol. 2008;31(3):527–534. doi: 10.1007/s00270-007-9237-9. [DOI] [PubMed] [Google Scholar]
- 12.Aburano H., Morinaga K., Shigenari N., Inoue D., Okuda M., Minami T. Common hepatic artery aneurysm treated with an endovascular stent-graft: a case report. Abdom Imaging. 2010;35(2):215–217. doi: 10.1007/s00261-008-9498-z. [DOI] [PubMed] [Google Scholar]
- 13.Larson R.A., Solomon J., Carpenter J.P. Stent graft repair of visceral artery aneurysms. J Vasc Surg. 2002;36(6):1260–1263. doi: 10.1067/mva.2002.129645. [DOI] [PubMed] [Google Scholar]
- 14.Bosiers M., Torsello G., Gissler H.M., Ruef J., Muller-Hulsbeck S., Jahnke T. Nitinol stent implantation in long superficial femoral artery lesions: 12-month results of the DURABILITY I study. J Endovasc Ther. 2009;16(3):261–269. doi: 10.1583/08-2676.1. [DOI] [PubMed] [Google Scholar]
- 15.Schoenefeld E., Donas K.P., Schonefeld T., Osada N., Austermann M., Torsello G. Mid-term outcome after endovascular therapy in the superficial femoral and popliteal artery using long stents. VASA. Zeitschrift fur Gefasskrankheiten. 2012;41(1):49–56. doi: 10.1024/0301-1526/a000163. [DOI] [PubMed] [Google Scholar]
- 16.Wilms G.E., Peene P.T., Baert A.L., Nevelsteen A.A., Suy R.M., Verhaeghe R.H. Renal artery stent placement with use of the Wallstent endoprosthesis. Radiology. 1991;179(2):457–462. doi: 10.1148/radiology.179.2.2014292. [DOI] [PubMed] [Google Scholar]