Abstract
Background
Cystic fibrosis (CF) is a disease characterized by chronic airway infection with a high incidence and poor prognosis. Pseudomonas aeruginosa and Aspergillus fumigatus are pathogens commonly found in CF patients. Clinically, these two microorganisms often coexist in the airway of CF patients. Combined infection with P. aeruginosa and A. fumigatus results in worsening lung function and clinical condition.
Methods
In this review, we focus on the mutual inhibition and promotion mechanisms of P. aeruginosa and A. fumigatus in CF patients. We also summarized the mechanisms of the interaction between these pathogenic microorganisms.
Results
P. aeruginosa inhibits A. fumigatus growth through the effects of phenazines, the quorum sensing system, iron competition, bacteriophages, and small colony variants. P. aeruginosa induces A. fumigatus growth through volatile organic compounds and subbacteriostatic concentrations of phenazines. A. fumigatus interferes with P. aeruginosa, affecting its metabolic growth via phenazine metabolic transformation, gliotoxin production, and reduced antibiotic sensitivity.
Discussion
Coexistence of P. aeruginosa and A. fumigatus can lead to both mutual inhibition and promotion. In different stages of CF disease, the interaction between these two pathogenic microorganisms may shift between promotion and inhibition. A discussion of the mechanisms of P. aeruginosa and A. fumigatus interaction can be beneficial for further treatment of CF patients and for improving the prognosis of the disease.
Keywords: Pseudomonas aeruginosa, Infection, Aspergillus fumigatus, Intermicrobial interaction, Cystic fibrosis
Introduction
Cystic fibrosis (CF) is the most common inherited lung infection disease; it is estimated that more than 70,000 people worldwide suffer from CF (Cystic Fibrosis Foundation, 2017). As CF affects multiple organs, the morbidity and mortality of CF are caused by airway infection and the associated inflammation (Zhao et al., 2012). Mutations in the cystic fibrosis transmembrane conductance regulator (CFTR) gene result in dysfunction or a lack of CFTR protein and impaired mucociliary clearance in CF patients. CF-related lung disease begins early in life, with inflammation, impaired mucociliary clearance, and consequent chronic infection of the airways (Robinson & Bye, 2002).
The pathogens Pseudomonas aeruginosa and Aspergillus fumigatus are common in lung infections. The bacterium P. aeruginosa infects 70–80% of adult patients with CF (Al-Momani et al., 2016; Salsgiver et al., 2016) and A. fumigatus is the most common fungal pathogen isolated from the airways of CF patients. The reported prevalence of A. fumigatus colonization in CF patients is between 16% and 58% (Amin et al., 2010; Becker et al., 1996; Skov et al., 2005; Stevens et al., 2003; Valenza et al., 2008). Moreover, many studies have shown that the sputum of CF patients contains both P. aeruginosa and A. fumigatus. Previous studies have reported the isolation of A. fumigatus in up to 60% of CF patients with P. aeruginosa infection, and P. aeruginosa has been isolated in up to 64.2% of CF patients with A. fumigatus infection (Bakare et al., 2003; Paugam et al., 2010). The results from a systematic review and meta-analysis showed that the pooled co-colonization prevalence of P. aeruginosa and A. fumigatus in patients with CF was 15.8% (95% CI [9.9–21.8]) with variation ranging between 2.3% and 44.8% (Zhao et al., 2018).
Co-colonization by P. aeruginosa and A. fumigatus in CF patients correlates with a worsened condition (Amin et al., 2010; Shoseyov et al., 2006). For example, an Irish registry analysis showed that P. aeruginosa and A. fumigatus co-colonization was associated with reduced FEV1, more frequent hospitalization, greater respiratory exacerbation, and increased use of anti-microbials compared with patients without the co-existence of these pathogens (Reece et al., 2017). Another study reported increased levels of toxic products in supernatants from P. aeruginosa and A. fumigatus co-culture compared with those from P. aeruginosa monoculture. Indeed, the production of cytotoxic elastase by P. aeruginosa increases in the presence of the filamentous fungus A. fumigatus, damaging human lung epithelial cells, decreasing lung function and facilitating disease progression (Smith et al., 2015).
Pseudomonas aeruginosa and A. fumigatus interact in a complex manner in the airways of co-infected CF patients. In this review, we summarize in detail the mechanisms underlying the interaction between P. aeruginosa and A. fumigatus. We review the principles of mutual inhibition and growth promotion of P. aeruginosa and A. fumigatus as well as interaction between the two microorganisms in CF patients at different stages of the disease, emphasizing the impact of such interactions on the conditions of CF patients. In the presence of co-infection, P. aeruginosa and A. fumigatus do not exist in isolation; instead, they affect each other and combat the immune response together to collaboratively affect the development of the disease.
Survey methodology
The EmBase, PubMed, and Web of Science databases were searched (until January 2018) using the following free-text terms: P. aeruginosa, A. fumigatus, and CF.
Inhibitory effect of P. aeruginosa on A. fumigatus
Pseudomonas aeruginosa inhibits A. fumigatus growth by the effect of phenazines, the quorum sensing (QS) system, iron competition, bacteriophages, and small colony variants (SCVs).
Phenazines constitute a large proportion of the numerous molecules secreted by P. aeruginosa during growth and are considered important virulence factors against target organisms, including other bacteria, fungi, and mammalian cells (Gibson, Sood & Hogan, 2009; Lau et al., 2004; Price-Whelan, Dietrich & Newman, 2006; Whiteson et al., 2014). Phenazines are present in CF patient sputum at concentrations ranging from 1 to 100 μg ml−1 (Wilson et al., 1988), and their increasing concentrations can cause a concomitant decline in lung function (Hunter et al., 2012). In CF patients, overproduction of alginate in P. aeruginosa biofilms generates a hypoxic gradient and anaerobic environment that enhances phenazine toxicity (Wang, Kern & Newman, 2010). P. aeruginosa phenazines have an important impact on electron shuttling, redox chemistry, and biofilm development through the toxic superoxide signaling and generation (Pierson & Pierson, 2010; Price-Whelan, Dietrich & Newman, 2006). Phenazines are regarded as endogenous redox-active molecules that promote P. aeruginosa growth and survival under iron-limiting conditions in CF patients and include five secreted molecules: pyocyanin (5-N-methyl-1-hydroxyphenazine, PYO) (Blyth & Forey, 1971; Kerr et al., 1999; Mangan, 1969), 1-hydroxyphenazine (1-HP) (Kerr et al., 1999; Mangan, 1969), phenazine-1-carboxamide (PCN), phenazine-1-carboxylic acid (PCA) (Briard et al., 2015), and dirhamnolipids (diRhls) (Briard et al., 2017).
The QS system comprises a cell density-based intercellular communication system in which signals are transmitted within the same bacterial species and between different species. The QS system regulates a variety of biological characteristics, including the release of virulence factors. The QS system in P. aeruginosa is involved in the regulation of elastase, pyocyanin, proteolytic enzyme, and biofilm formation (Lee & Zhang, 2015). There are three known QS systems in P. aeruginosa, namely, las, rhl, and pqs.
Fe is a very important element for P. aeruginosa and A. fumigatus growth. In fact, the numerous iron acquisition systems underlie the ability of P. aeruginosa to survive in diverse environments, with a strong ability to compete with other organisms for this essential metallonutrient. There are three classes of pyoverdines, which are iron chelators, with similar iron-binding properties and levels of activity. Type II pyoverdine is the main type involved in P. aeruginosa strains associated with CF (De Vos et al., 2001).
Bacteriophages have an important impact on bacterial virulence and phenotypic variation. It has been shown that the formation of SCVs in biofilms can be mediated by the filamentous bacteriophage Pf4 of the P. aeruginosa strain PAO1 (Mooij et al., 2007), and this morphological type is related to parameters of poor lung function in CF patients.
As SCVs represent a CF P. aeruginosa phenotype, analysis of SCVs isolated during chronic P. aeruginosa colonization in CF patients is a worthy endeavor. For example, it has been reported that SCVs isolated from CF patients are resistant to antibiotics and are associated with poor lung function and a poor clinical condition (Evans, 2015; Hogardt & Heesemann, 2010; Häussler et al., 1999).
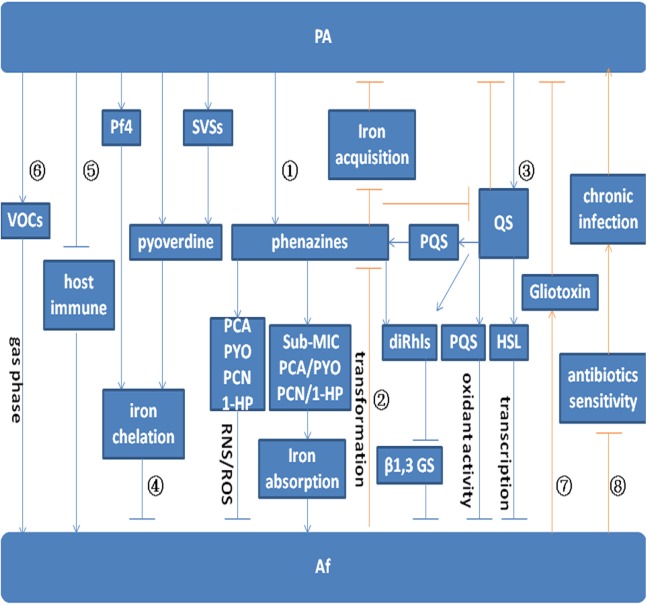
Inhibitory effect of phenazines on the growth of A. fumigatus
Pseudomonas aeruginosa-secreted phenazines prevent the growth of A. fumigatus. It is thought that the toxic effects of phenazines on prokaryotes and diverse eukaryotic hosts result from their redox activities or inactivation of oxidative stress response proteins (Hassett et al., 1992; Muller, 2002; O’Malley et al., 2003). In target cells, reduced phenazines are oxidized by NAD(P)H and oxygen to generate reactive oxygen species (ROS), specifically O2·− Moreover, generation of reactive nitrogen species (RNS) is induced by overproduction of O2·− (Martínez & Andriantsitohaina, 2009). Nitric oxide (NO·) is produced by mitochondrial processes, and highly toxic peroxynitrite radicals (ONOO−) are generated via reactions between NO· with O2·− radicals (Martínez & Andriantsitohaina, 2009). Overall, mitochondria are the main target of phenazine-produced ROS and RNS, and phenazines have a significant impact on the mitochondrial ultrastructure of A. fumigatus hyphae. All four phenazines (PYO, PCA, PCN, 1-HP) show A. fumigatus growth inhibitory effects by inducing the production of ROS, specifically O2·−, and the RNS ONOO− (pathway ① in Fig. 1) (Briard et al., 2015).
Figure 1. Model for the interaction between P. aeruginosa and A. fumigatus.
Arrows indicate promotion. Arrows without heads indicate inhibition. Blue lines indicate the effect of P. aeruginosa on A. fumigatus. Red lines indicate the effect of A. fumigatus on P. aeruginosa. Pathway ① indicates the effect of P. aeruginosa on A. fumigatus by phenazine. PYO, PCA, PCN, and 1-HP inhibit A. fumigatus growth by inducing the production of ROS and RNS. Sub-MIC PYO, PCA, PCN, and 1-HP promote A. fumigatus growth by iron absorption. A. fumigatus growth can be inhibited by diRhls, which blocks β1,3 GS activity. Pathway ② shows the effect of A. fumigatus on P. aeruginosa by phenazine transformation. The metabolic conversion of phenazine by A. fumigatus inhibits the reduction of Fe3+ and affects QS system regulation in P. aeruginosa. Pathway ③ depicts the inhibition of toxic products and small molecules regulated by the QS system. The QS system in P. aeruginosa inhibits A. fumigatus growth via the effect of diRhls, PQS, and 3-oxo-C12 HSL. Pathway ④ shows that P. aeruginosa inhibits A. fumigatus growth via the effect of pyoverdine, Pf4, and SVSs on A. fumigatus iron deprivation. Pathway ⑤ and Pathway ⑥ illustrate P. aeruginosa promotion of A. fumigatus growth through the inhibition of host immune components and emission of VOCs. Pathway ⑦ shows that gliotoxin produced by A. fumigatus interferes with the metabolic growth of P. aeruginosa. Pathway ⑧ shows that A. fumigatus reduces the sensitivity of P. aeruginosa to antibiotics and promotes chronic infection.
Another related study reported that phenazine-derived metabolites acting as interspecies signals can affect filamentous fungal development through oxidative stress regulation (Zheng et al., 2015b). In P. aeruginosa–A. fumigatus co-culture biofilms, development of the latter is differentially modulated by phenazine-derived metabolites of the former. With a decreasing phenazine gradient, A. fumigatus shifts from weak vegetative growth to an asexual sporulation phase (conidiation), and this shift in morphology is correlated with the production of phenazine radicals and concomitant ROS generation by phenazine redox cycling.
DiRhls induce A. fumigatus to produce an extracellular matrix that facilitates P. aeruginosa binding. A. fumigatus growth can be inhibited by diRhls, which blocks the β1,3 glucan synthase (GS) activity (pathway ① in Fig. 1) (Briard et al., 2017).
A recent study reported that a double phenazine mutant was similar to the wild-type organism in terms of its inhibitory power against A. fumigatus (Sass et al., 2018), with little difference caused by the complete lack of phenazine molecules due to mutation. The results of this study are different from those of previous studies. Several previous studies have emphasized the inhibitory power of phenazines on A. fumigatus (Briard et al., 2015, 2017; Zheng et al., 2015b), but a deficiency of these molecules via mutation appeared to cause little difference in this study. This finding suggests that the concentrations of phenazines that have been previously studied in vitro may be irrelevant to those in vivo. In addition, compensation for the loss of phenazine-mediated inhibitory activity by upregulation of other factors in the mutants could not be excluded in this study. Further research is needed to explore the effect of phenazines on the growth of A. fumigatus.
Effects of the inhibition of the QS system on the growth of A. fumigatus
The P. aeruginosa QS network plays a role in inhibiting A. fumigatus growth and biofilm formation (pathway ③ in Fig. 1) (Mowat et al., 2010). The las QS system is essential for the production of the diffusible signaling molecule acyl homoserine lactone (AHL) N-(3-oxododecanoyl)-l-homoserine lactone (3-oxo-C12 HSL) (Smith & Iglewski, 2003), resulting in the expression of specific target genes in P. aeruginosa. In addition, 3-oxo-C12 HSL is one of the AHLs frequently identified in extracts of respiratory secretions from CF patients infected with P. aeruginosa (Smith & Iglewski, 2003). By utilizing two P. aeruginosa QS knockout strains, PAO1:ΔLasI and PAO1:ΔLasR, one study illustrated that 3-oxo-C12 HSL inhibits A. fumigatus biofilm formation (Mowat et al., 2010). The PAO1:ΔLasI strain was unable to synthesize 3-oxo-C12 HSL, whereas PAO1:ΔLasR synthesized 3-oxo-C12 HSL but could not respond to it. Furthermore, A. fumigatus growth was significantly greater when in direct co-culture with PAO1:ΔLasI and PAO1:ΔLasR than in co-culture with wild-type PAO1. The indirect effect of the P. aeruginosa QS knockout strains on A. fumigatus biofilm development was assessed using the Transwell system, which showed significantly less inhibition of A. fumigatus biofilm development when in indirect co-culture with PAO1:ΔLasI and PAO1:ΔLasR than with the wild-type strain. Additionally, the cellular viability of A. fumigatus conidia and the biomass of A. fumigatus biofilms were reduced by diffusible and heat-stable soluble molecules, such as decanol, decanoic acid and dodecanol (structurally similar to the QS molecules produced by P. aeruginosa) in a concentration-dependent manner. At the molecular level, it is likely that these molecules lead to hyphal repression by affecting key transcription factors (Mowat et al., 2010).
In CF patients, P. aeruginosa produces rhamnolipids (Rhls), which are controlled by the QS system. Rhls are largely composed of diRhls and monorhamnolipids, and the diRhls secreted by P. aeruginosa may affect A. fumigatus. For example, diRhls induce A. fumigatus to produce an extracellular matrix that facilitates binding by P. aeruginosa (Briard et al., 2017). As stated above, diRhls also inhibit A. fumigatus growth by blocking β1,3 GS activity and altering cell wall architecture. In the presence of diRhls, A. fumigatus displays multibranched hyphae and a thicker cell wall rich in chitin. This growth phenotype of A. fumigatus is similar to that following treatment with anti-fungal echinocandins. Although the two rhamnose moieties attached to fatty acyl chains are essential structures for the interaction of diRhl with β1,3 GS, the site of β1,3 GS action differs between diRhls and echinocandins. Overall, diRhls and azole anti-fungals exhibit a synergistic anti-fungal effect (Briard et al., 2017).
A recent study reported that alkylhydroxyquinolones (AHQs), autoinducers secreted by P. aeruginosa, could suppress biofilm formation in A. fumigatus. The AHQ interkingdom signaling molecules 2-heptyl-3-hydroxy-4-quinolone (PQS) and 2-heptyl-4-quinolone (HHQ), which are involved in QS in P. aeruginosa, were both able to alter A. fumigatus biofilm biomass and structure (Reen et al., 2016). Both pro- and anti-oxidant activities have been reported for PQS and HHQ. AHQ interkingdom signaling molecules can interact with lipopolysaccharides, cellular membranes, and membrane vesicles in several bacterial species (Häussler & Becker, 2008). Redox-active phenazines of P. aeruginosa, which exhibit inhibitory activity against A. fumigatus growth, are also controlled by AHQs (Moree et al., 2012). Overall, these small interkingdom signaling molecules of P. aeruginosa disrupt A. fumigatus biofilm formation and render A. fumigatus susceptible to clearance by drugs. As these bacterial molecules are selectively non-cytotoxic to host cell lines, they may be used as viable molecular therapeutics.
The anti-A. fumigatus capacity of P. aeruginosa pyoverdine mutants has been assessed in recent studies. Some residual inhibition of A. fumigatus can be detected in pyoverdine mutants, and in addition to the anti-Aspergillus effect of pyoverdine, other inhibitors may contribute to the total fungal inhibition by wild-type P. aeruginosa. Some of these residual inhibitors in pyoverdine mutants may be related to QS-regulated metabolites, such as Rhls. The anti-Aspergillus ability of QS mutants was also examined, with the results showing that QS-regulated metabolites have an important anti-Aspergillus function. Indeed, these metabolites are potential intermicrobial inhibitors. The decreased anti-A. fumigatus activity of QS mutants might be related to loss of the combined activity of many downstream products, and decreases in pyoverdine production in QS mutants may also lead to their reduced anti-Aspergillus capacity (Sass et al., 2018).
Inhibition of A. fumigatus growth by Fe metabolism
Pseudomonas aeruginosa inhibits A. fumigatus growth through Fe limitation, which can, in part, result from the modulation of siderophore production by the fungus due to metabolites from the bacterium (Phelan et al., 2014).
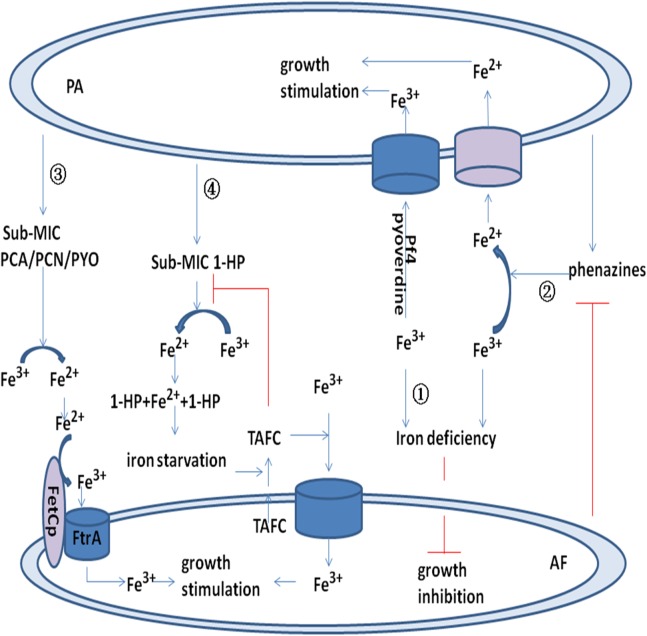
Recent research has shown that P. aeruginosa pyoverdine can suppress A. fumigatus growth and biofilm formation via the chelation of iron, reducing its availability to A. fumigatus (pathway ④ in Fig. 1) (Sass et al., 2018). In this study, pvdD pchE and pvdD mutants (loss of pyoverdine and siderophore), which are defective in inhibiting A. fumigatus growth and biofilm formation in various assays, were evaluated. The inhibitory effect of pyoverdine deletion mutants was restored with pure pyoverdine, and the A. fumigatus sidA mutant that is unable to produce siderophores was found to be hypersusceptible to P. aeruginosa metabolites and to pyoverdine. Thus, the siderophore-deficient A. fumigatus mutant was readily inhibited by P. aeruginosa. Clinical P. aeruginosa isolates derived from the lungs of CF patients have revealed a correlation between the amount of pyoverdine produced and the anti-fungal activity of clinical samples. The results suggest that the siderophore pyoverdine is an important inhibitory molecule (Sass et al., 2018).
As pyoverdine can capture iron from the environment, it can deprive A. fumigatus of the iron that is essential for its growth and metabolism. Iron sequestration by pyoverdine leads to iron starvation and increased siderophore secretion by A. fumigatus (Sass et al., 2018). In a shared microenvironment, P. aeruginosa and A. fumigatus compete for iron to promote their own survival, and high pyoverdine expression antagonizes A. fumigatus metabolism and growth, which might support anti-fungal treatment. Key aspects of the competition between P. aeruginosa and A. fumigatus include the relative amounts of siderophores produced, the speed of siderophore production, and the relative affinity for Fe.
Bacteriophage Pf4 inhibits the metabolic activity of A. fumigatus biofilms
In a recent study, it was reported that the Pf4 phagosome can inhibit A. fumigatus metabolism and growth by binding iron and causing iron deficiency (pathway ④ Fig. 1) (Penner et al., 2016). Pf4 inhibition of A. fumigatus is caused by iron binding and the sequestration of A. fumigatus iron resources (pathway ① Fig. 2), and inhibition of A. fumigatus metabolism by Pf4 can be overcomed with ferric iron supplementation. Moreover, inhibition of A. fumigatus biofilm formation by phages is reversed by low doses of iron, indicating that A. fumigatus is more sensitive to iron inhibition by the Pf4 phage than it is to other elements in P. aeruginosa supernatants (Penner et al., 2016). This Pf4 phage-mediated inhibition was found to be dose dependent and could be alleviated by phage denaturation. This inhibition of Pf4 was more significant in preformed A. fumigatus biofilms than during biofilm formation. In contrast, Pf4 had no effect on planktonic conidia (Penner et al., 2016). These findings suggest that the site of phage action is specific to the extracellular matrix or hyphae (Reichhardt et al., 2015). Another two phages, Pf1 and fd, showed no inhibitory action against A. fumigatus. Pf4 attaches to A. fumigatus hyphae, and fungal inhibition may occur at the biofilm surface. The shorter phage Pf1 did not bind as extensively to A. fumigatus biofilms as did Pf4 and exhibited less efficient inhibition (Penner et al., 2016).
Figure 2. Model for the interaction between P. aeruginosa and A. fumigatus by iron uptake and competition.
Pyoverdine and Pf4 phage bind to Fe3+ and promote uptake by P. aeruginosa. Pyoverdine and Pf4 phage deprive A. fumigatus of Fe3+ and inhibit its growth (pathway ①). Phenazine reduces Fe3+ to Fe2+ and promotes P. aeruginosa uptake of Fe2+. Phenazine is converted by A. fumigatus into metabolic products with potentially modified redox potentials. These products may inhibit the reduction of Fe3+ in P. aeruginosa (pathway ②). Sub-MIC PYO, PCN, and PCA reduce Fe3+ to Fe2+ and promote the FetCp/FtrA complex of A. fumigatus to take up Fe2+ (pathway ③). Sub-MIC 1-HP reduces Fe3+ to Fe2+, and two 1-HP molecules bind the newly formed Fe2+. This chelating activity induces iron starvation and activates triacetylfusarinine C (TAFC). TAFC promotes A. fumigatus uptake of Fe3+ and stimulates its growth (pathway ④).
Acute infection of P. aeruginosa by Pf bacteriophage can decrease the production of pyoverdine and the inhibitory capacity toward A. fumigatus biofilms. Thus, the reduced production of anti-microbials by P. aeruginosa infected by Pf bacteriophage may promote co-infection with A. fumigatus in CF airways (Secor et al., 2017).
SCVs in A. fumigatus intermicrobial competition
In a study of SCVs in intermicrobial competition with A. fumigatus (Anand et al., 2017b), the SCVs isolated from P. aeruginosa was shown to inhibit A. fumigatus biofilm formation, and this inhibitory capacity toward A. fumigatus biofilm was found to be related to pyoverdine (pathway ④ in Fig. 1) (Anand et al., 2017b). Indeed, isolated SCVs with high pyoverdine production had the highest inhibitory capacity in every co-culture method evaluated. Correspondingly, the two SCV isolates with the lowest inhibitory activities did not produce pyoverdine, suggesting that pyoverdine is the key P. aeruginosa inhibitor of A. fumigatus (Anand et al., 2017b).
Pseudomonas aeruginosa SCVs exhibit heterogeneity in inhibiting A. fumigatus biofilms. For instance, the inhibitory abilities of clinical SCVs isolates and reference CF non-mucoid isolates of P. aeruginosa or filtrates from P. aeruginosa planktonic or biofilm cultures were compared by coincubation with A. fumigatus during biofilm formation or in preformed biofilm. The metabolic activities of A. fumigatus biofilms were measured by different assays, with pyoverdine in filtrates being measured by spectrophotometry. The results showed that SCVs inhibited A. fumigatus biofilm formation, although the inhibitory effects of different SCVs were quite different. By adjusting planktonic culture filtrates, differences in SCV inhibition were related to SCV growth or deficient inhibitor production. Overall, the ability of SCVs to inhibit A. fumigatus biofilm was related to pyoverdine (Anand et al., 2017b). Thus, SCVs isolated from P. aeruginosa may be important in CF because they are capable of inhibiting A. fumigatus biofilm.
Inhibition of A. fumigatus by P. aeruginosa under conditions of hypoxia
Most studies examining the inhibition of A. fumigatus by P. aeruginosa have been performed under normoxic conditions. However, patients with acute exacerbation or progression of CF may exhibit hypoxia in focal lung sites (Cowley et al., 2015; Lambiase, Catania & Rossano, 2010; Worlitzsch et al., 2002). A. fumigatus inhibition by P. aeruginosa was recently evaluated under hypoxic conditions (Anand, Clemons & Stevens, 2017a), and the results showed that although the inhibitory activities of P. aeruginosa were effective under aerobic, hypoxic, or anaerobic conditions, P. aeruginosa growth was slow under hypoxic or anaerobic conditions, thus decreasing the ability of P. aeruginosa filtrates to inhibit A. fumigatus growth and biofilm formation. Regardless of the planktonic or biofilm state, the extracellular molecules produced by P. aeruginosa under anaerobic conditions were less inhibitory toward A. fumigatus growth and biofilm formation than were those under aerobic conditions. Therefore, the inhibitory power of P. aeruginosa against both A. fumigatus preformed biofilm and biofilm formation was decreased under hypoxic conditions (Anand, Clemons & Stevens, 2017a).
During the course of CF progression, P. aeruginosa mutants with a low level of pyoverdine production often appear, and the ratio of Fe3+ to Fe2+ decreases under hypoxic conditions. Intracellular iron acquisition by P. aeruginosa occurs mainly through the ingestion of low-activity Fe2+ via the production of phenazines and membrane permease (Cartron et al., 2006; Cornelis & Dingemans, 2013; Nguyen & Oglesby-Sherrouse, 2015). P. aeruginosa in the airway of CF patients typically shows low pyoverdine expression, and as mentioned above, pyoverdine can inhibit A. fumigatus growth by depriving A. fumigatus of iron. Under hypoxic conditions, the inhibitory effect of P. aeruginosa on A. fumigatus declines; thus, the growth of A. fumigatus is promoted (Sass et al., 2018). These findings explain why A. fumigatus is able to colonize CF airways following P. aeruginosa colonization and why A. fumigatus may persist during CF disease progression or chronic lung infection (Amin et al., 2010; Baxter et al., 2013a; Fillaux et al., 2012; Forsyth et al., 1988; Mirković et al., 2016; Nicolai et al., 1990; Speirs, Van Der Ent & Beekman, 2012).
After a long period of hypoxia, the interaction between P. aeruginosa and A. fumigatus appears to be similar to that under normoxic conditions (Anand, Clemons & Stevens, 2017a). Other factors may also affect P. aeruginosa and A. fumigatus interactions, such as prolonged use of antibiotics or inhaled corticosteroids (Noni et al., 2014).
The different inhibitory capacities of P. aeruginosa on A. fumigatus between planktonic and biofilm states
Pseudomonas aeruginosa and A. fumigatus are commonly found in the airways of patients with CF in the form of biofilms, and their pathogenicity and resistance in the biofilm state differ from those in the planktonic state. The inhibitory capacity of P. aeruginosa toward A. fumigatus in the biofilm state is also different from that in the planktonic state (Mowat et al., 2010). As an example, the supernatant extracted from P. aeruginosa biofilm was more effective than that extracted from planktonic cells (Ferreira et al., 2015). Pyoverdine plays an important role in P. aeruginosa biofilm formation, and its production is higher in biofilm than in planktonic cells (Visaggio et al., 2015). Thus, the P. aeruginosa biofilm-mediated suppression of A. fumigatus growth and biofilm formation is greater than planktonic P. aeruginosa-mediated suppression. It is also possible that other inhibitors may play an important role in this process (Anand et al., 2017b).
As mentioned above, the inhibitory effects of P. aeruginosa on A. fumigatus biofilm formation and preformed biofilms are different; it has been reported that P. aeruginosa can inhibit A. fumigatus biofilm formation but has almost no effect on preformed biofilms. The mature filamentous biofilms of A. fumigatus clearly restricted the inhibitory capacity of P. aeruginosa (Mowat et al., 2010), and another study showed that preformed A. fumigatus biofilm was more resistant to P. aeruginosa (Ferreira et al., 2015). According to a recent study, preformed A. fumigatus biofilms are inhibited by biofilm filtrates of P. aeruginosa strains isolated from CF patients via apoptosis, an effect that is related to mitochondrial membrane damage caused by metacaspase activation (Shirazi et al., 2016). In contrast, the inhibitory capacity of P. aeruginosa Pf4 phage toward A. fumigatus preformed biofilm is higher than that during biofilm formation. The P. aeruginosa phage Pf4 had little effect on planktonic conidial growth (Penner et al., 2016), suggesting that hyphae or the extracellular matrix is the specific site of phage action (Reichhardt et al., 2015).
The different inhibitory abilities of P. aeruginosa on A. fumigatus conidia and hyphae
After A. fumigatus conidia colonization in the CF patient airway, A. fumigatus gradually forms a biofilm that is rich in hyphae, and P. aeruginosa exhibits different inhibitory capacities toward A. fumigatus conidia and hyphae. In simultaneous static co-cultures, P. aeruginosa cells can effectively kill A. fumigatus conidia cells, but P. aeruginosa cells show only a minor inhibitory effect on sporelings grown for 12 h or longer as well as hyphae (Manavathu, Vager & Vazquez, 2014). Indeed, during co-cultivation with P. aeruginosa, A. fumigatus sporelings grown for 12 h or longer and young hyphae were stronger than ungerminated conidia with respect to the formation of P. aeruginosa–A. fumigatus biofilm.
Aspergillus fumigatus hyphae can withstand the fungicidal effect of P. aeruginosa and can produce the cytotoxic compound gliotoxin, which has anti-bacterial activity. Production of mycotoxin increases during mycelial growth and biofilm formation in A. fumigatus (Manavathu, Vager & Vazquez, 2014), and P. aeruginosa growth and its ability to kill A. fumigatus are suppressed with increasing levels of gliotoxin. In addition, virulence factor production and the inhibitory action of P. aeruginosa are strengthened by this increased metabolic activity in cells. Overall, the metabolic activity of germinating conidia and young sporelings is strong, whereas that of mature hyphae is limited in the apical regions of filaments. The apex, which has high metabolic activity, is the site at which P. aeruginosa binds to A. fumigatus hyphae and acquires nutrients (Toljander et al., 2007); hyphae, which has low metabolic activity, are not sensitive to the toxic molecules of P. aeruginosa. In fact, the cell walls of mature hyphae are poorly permeable to the toxic molecules of P. aeruginosa. Hence, mature hyphae are not easily killed by P. aeruginosa (Manavathu, Vager & Vazquez, 2014).
Comparison of the inhibitory effect between different P. aeruginosa strains from CF patients and non-CF patients
In addition to CF patients, P. aeruginosa and A. fumigatus also co-exist in the airways of patients with conditions such as chronic obstructive pulmonary disease, bronchiectasis, and hospital-acquired pneumonia. P. aeruginosa in CF patient airways can be divided into two types: mucoid and non-mucoid. A recent survey showed that both non-CF and CF A. fumigatus strains are inhibited by P. aeruginosa metabolic products (Nazik et al., 2017), and another study reported that both P. aeruginosa cells and filtrates isolated from CF patients had greater inhibitory effects on A. fumigatus growth and biofilm formation in vitro than did materials isolated from non-CF patients (Ferreira et al., 2015). Furthermore, non-mucoid P. aeruginosa exerted greater inhibitory effects on A. fumigatus than did mucoid P. aeruginosa in CF patients (Shirazi et al., 2016).
Pseudomonas aeruginosa isolated from the airway of CF patients has a greater chance of contact and longer duration of co-existence with A. fumigatus than isolates from non-CF patients. In addition, P. aeruginosa isolated from CF patients produces more toxic products and inhibitors than that from non-CF patients. Thus, CF patient-derived P. aeruginosa has a greater inhibitory effect against A. fumigatus growth and biofilm formation than strains isolated from non-CF patients. Mucoid P. aeruginosa usually exists in the deep and hypoxic zone of the lung (Gaspar et al., 2013; Pressler et al., 2006; Tramper-Stranders et al., 2012), and the synthesis of toxic products and inhibitors of P. aeruginosa is reduced under hypoxic conditions. Overall, the inhibitory capacity of mucoid CF P. aeruginosa filtrates is less than that of non-mucoid CF filtrates.
Promotion of A. fumigatus growth by P. aeruginosa
Pseudomonas aeruginosa induces A. fumigatus growth through the action of sub-bacteriostatic concentrations of phenazines and volatile organic compounds (VOCs). Pathogen reproduction requires iron ions, and phenazines promote Fe3+ reduction in CF patients infected with P. aeruginosa (Hunter et al., 2013). In the early stages of infection, host immune cell molecules, such as lactoferrin or transferrin, actively chelate Fe3+ ions and inhibit the growth of P. aeruginosa and A. fumigatus. However, phenazines can promote P. aeruginosa and A. fumigatus growth by iron acquisition, and P. aeruginosa phenazines can reduce Fe3+ to Fe2+ and liberate Fe3+ from host immune cells (Banin, Vasil & Greenberg, 2005; Hernandez, Kappler & Newman, 2004; Wang et al., 2011). P. aeruginosa produces VOCs during the course of infection and reproduction, and these molecules can be detected in sputum samples of CF patients infected with P. aeruginosa (Goeminne et al., 2012).
Promotion effect of P. aeruginosa on A. fumigatus colonization and growth
Under certain conditions, P. aeruginosa promotes the growth of A. fumigatus. Therefore, many CF patients are susceptible to infection with A. fumigatus after infection with P. aeruginosa (Paugam et al., 2010). One study hypothesized that P. aeruginosa infection promotes the evolution of A. fumigatus sensitization (Kraemer et al., 2006).
Another study reported reduced colonization of A. fumigatus after anti-infective treatment of P. aeruginosa in patients with acute exacerbation of CF, potentially because the bacterium protects A. fumigatus via immune factors and growth conditions (Baxter et al., 2013b). During acute exacerbation in CF patients, the colonization and growth of A. fumigatus may be related to the negative effects of P. aeruginosa on host lung function and immune defense. Resistance of P. aeruginosa biofilms to host immune responses contributes to the growth and multiplication of A. fumigatus (pathway ⑤ in Fig. 1) (Baxter et al., 2013a). By analyzing pre- and post-antibiotic sputum samples from adult CF patients, a study showed that intravenous antibiotics targeting P. aeruginosa during CF pulmonary exacerbations had a negative impact on the colonization and growth of A. fumigatus (Baxter et al., 2013b). Because P. aeruginosa contributes to the colonization and growth of A. fumigatus in CF patients, it is also possible that both microbes work together to combat host immune factors, resulting in increased infection and decreased pulmonary function. Nonetheless, their relationship may become competitive with growth, and P. aeruginosa inhibits A. fumigatus in various ways, as described above. Further research is required to verify the interdependence between these two organisms for survival within the airways of CF patients.
Sub-bacteriostatic concentrations of phenazines induce A. fumigatus growth
Regarding P. aeruginosa and A. fumigatus competitive growth, the former produces phenazines to inhibit the growth of the latter (Zheng, Keller & Wang, 2015a), yet one study demonstrated that sub-bacteriostatic concentrations of phenazines can induce A. fumigatus growth in specific situations. For instance, it was reported that sub-bacteriostatic concentrations of PYO, PCA, and PCN can induce A. fumigatus growth by promoting iron uptake. The redox function of 1-HP, which is capable of chelating iron ions and inducing iron starvation in A. fumigatus, can also promote A. fumigatus growth (pathway ① in Fig. 1) (Briard et al., 2015).
Aspergillus fumigatus can obtain iron resources through low-affinity ferrous iron uptake, high-affinity reductive iron uptake and siderophore-mediated iron uptake (Schrettl et al., 2004). Three sub-bacteriostatic phenazines, PYO, PCA, and PCN, can induce the growth of an A. fumigatus mutant lacking SidAp and siderophore biosynthesis under iron starvation conditions, and it was suggested that phenazines reduce Fe3+ to Fe2+ and promote the ferroxidase FetCp/permease FtrAp complex of the A. fumigatus mutant to take up Fe2+ (pathway ③ in Fig. 2) (Briard et al., 2015). Fusarinine C (FsC) and triacetylfusarinine C (TAFC) are two extracellular siderophores of A. fumigatus, while ferricrocin and hydroxyferricrocin are two intracellular siderophores of A. fumigatus (Haas, 2012). Sub-bacteriostatic 1-HP produced by P. aeruginosa promotes A. fumigatus growth by iron chelation and stimulation of TAFC secretion (pathway ④ in Fig. 2) (Briard et al., 2015).
VOCs promote A. fumigatus growth
A recent study showed that VOCs released by P. aeruginosa can promote A. fumigatus growth (pathway ⑥ in Fig. 1) (Briard, Heddergott & Latgé, 2016), and dimethyl sulfide was found to be a VOC with an enhancement effect on A. fumigatus, which is mediated by the gas phase. During sulfur starvation, A. fumigatus utilizes exogenous VOCs to promote growth, and in patients with CF, it is possible that P. aeruginosa promotes the colonization and growth of A. fumigatus by releasing VOCs, causing a rapid decline in lung function (Briard, Heddergott & Latgé, 2016). This result is consistent with the results of past clinical studies showing that P. aeruginosa and A. fumigatus co-infection resulted in decreased lung function (Amin et al., 2010; Baxter et al., 2013b).
Without direct contact, P. aeruginosa and A. fumigatus interact through signaling molecules such as VOCs. With direct contact, P. aeruginosa can release the corresponding signaling molecules to promote A. fumigatus colonization and growth. However, when these pathogenic microorganisms grow and contact one another, they exert a mutual inhibitory effect with regard to nutrient competition (Briard, Heddergott & Latgé, 2016).
The effect of A. fumigatus on P. aeruginosa
Pseudomonas aeruginosa and A. fumigatus interact with each other under co-growth conditions in patients with CF and other chronic pulmonary infection diseases. A. fumigatus can also resist inhibition by P. aeruginosa and, to a certain extent, affect its growth and metabolism.
Metabolic transformation of phenazines produced by P. aeruginosa
Phenazines inhibit A. fumigatus by inducing the production of ROS and RNS. Sod2p of A. fumigatus can resist the injury caused by ROS and RNS and antagonize inhibition by P. aeruginosa (Briard et al., 2015). Another study demonstrated that the phenazines produced by P. aeruginosa can be metabolically converted by A. fumigatus to reduce their inhibitory effect. As an example, PCA can be converted to 1-HP,1-methoxyphenazine and phenazine-1-sulfate. Although 1-HP has an inhibitory effect on A. fumigatus, 1-HP was also able to induce the production of the A. fumigatus siderophores TAFC and FsC (Moree et al., 2012). Regardless, previous experiments have shown that 1-HP inhibits bacterial siderophore biosynthesis (Dietrich et al., 2008). PCA induces the reduction of Fe3+ to Fe2+ for P. aeruginosa biofilm formation (Wang et al., 2011), and conversion of PCA by A. fumigatus may also decrease P. aeruginosa iron acquisition for metabolism and biofilm formation. Phenazine is converted by A. fumigatus into metabolic products with potentially altered redox potentials, and these products may inhibit Fe3+ reduction in P. aeruginosa (pathway ② Fig. 2). The phenazines PYO and PCA produced by P. aeruginosa can be converted to phenazine dimers by A. fumigatus, which have a decreased inhibitory effect on A. fumigatus. The QS signaling molecule PYO of P. aeruginosa affects transcriptional regulation and induces biofilm formation. Metabolic conversion of PYO by A. fumigatus might have an effect on QS system regulation. Thus, A. fumigatus can transform P. aeruginosa metabolites and radically alter the effects on their interaction, including the degree of inhibition (pathway ② in Fig. 1) (Moree et al., 2012).
Gliotoxin produced by A. fumigatus interferes with the metabolic growth of P. aeruginosa
During co-culture, A. fumigatus can also invoke its own metabolism and signaling molecules to disrupt P. aeruginosa growth. Gliotoxin produced by A. fumigatus is also a major immunoevasive toxin that is important in mediating A. fumigatus-associated colonization within the context of CF (Chotirmall et al., 2014). Overall, the gliotoxin secreted by A. fumigatus suppresses the inhibitory ability and growth of P. aeruginosa (pathway ⑦ in Fig. 1) (Manavathu, Vager & Vazquez, 2014).
Reducing the sensitivity of P. aeruginosa to antibiotics and promoting chronic infection
Under specific conditions, A. fumigatus can maintain the growth of P. aeruginosa in a co-existence scenario. One case-control study showed that CF patients infected by A. fumigatus could easily develop chronic P. aeruginosa infections despite receiving anti-microbial therapy (pathway ⑧ in Fig. 1) (Pressler et al., 2006).
The sensitivity of P. aeruginosa to antibiotics also changes when it co-exists with A. fumigatus. One in vitro study showed that P. aeruginosa in a polymicrobial biofilm with A. fumigatus was less susceptible to cefepime than P. aeruginosa in a monomicrobial biofilm state (pathway ⑧ in Fig. 1) (Manavathu, Vager & Vazquez, 2014). The extracellular matrix of polymicrobial biofilms differs for P. aeruginosa monomicrobial biofilms, and the sensitivity of P. aeruginosa in polymicrobial biofilm to some antibiotics decreases as a result of the change in the biofilm extracellular matrix. Indeed, some antibiotics cannot kill P. aeruginosa in biofilm due to altered permeability of the polymicrobial biofilm extracellular matrix. In contrast, the change in extracellular matrix between polymicrobial biofilms and A. fumigatus monomicrobial biofilms is not obvious and may not be sufficient to cause changes in the sensitivity of A. fumigatus to anti-fungal agents. For example, the sensitivity of A. fumigatus to anti-fungal drugs, such as voriconazole and posaconazole, did not change in polymicrobial or monomicrobial biofilms (Manavathu, Vager & Vazquez, 2014).
At present, only a few studies have examined the effect of A. fumigatus on P. aeruginosa, and the underlying mechanism should be the focus of further research.
Conclusion
In the co-infection state, P. aeruginosa interacts with A. fumigatus in a number of ways. In the early stage of CF, P. aeruginosa first colonizes and then grows, providing favorable nutritional and immunological conditions for infection and colonization by A. fumigatus. P. aeruginosa and A. fumigatus in the CF patient airway then promote each other’s growth and grow together. As the disease progresses and resources become less abundant in the co-existence environment, the interaction between P. aeruginosa and A. fumigatus shifts to mutual inhibition. It is suggested that antibiotic treatment against P. aeruginosa can inhibit the progression of A. fumigatus infection early during co-infection. When the infection is exacerbated and the condition of the CF patients deteriorates, anti-infective treatment against one pathogen may lead to the growth and reproduction of the other pathogen. At present, combined anti-infective therapy against both pathogens should be used, as the above possibilities need to be further investigated by a large number of clinical studies. The interaction between the two pathogens is quite complicated in the process of CF disease development, and many mechanisms of action remain unclear. Further studies examining the influence of A. fumigatus on P. aeruginosa and the immunomodulatory mechanism between these pathogens and the human body must be carried out to facilitate the treatment of CF patients with polymicrobial infections.
Funding Statement
This work was supported by the Chinese Medicine Science and Technology Development Project Fund of Shandong Province under Grant No. 2017-200, the Postdoctoral Applications Research Project Fund of Qingdao under Grant No. 2016055, and The Affiliated Hospital of Qingdao University Youth Research Fund under Grant 2016. There was no additional external funding received for this study. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Contributor Information
Jingming Zhao, Email: wch7650@hotmail.com.
Wencheng Yu, Email: qdyuwencheng@hotmail.com.
Additional Information and Declarations
Competing Interests
The authors declare that they have no competing interests.
Author Contributions
Jingming Zhao conceived and designed the experiments, performed the experiments, analyzed the data, contributed reagents/materials/analysis tools, prepared figures and/or tables, authored or reviewed drafts of the paper, approved the final draft.
Wencheng Yu conceived and designed the experiments, performed the experiments, analyzed the data, contributed reagents/materials/analysis tools, prepared figures and/or tables, authored or reviewed drafts of the paper, approved the final draft.
Data Availability
The following information was supplied regarding data availability:
The research in this article did not generate any data or code. This is a literature review.
References
- Al-Momani et al. (2016).Al-Momani H, Perry A, Stewart CJ, Jones R, Krishnan A, Robertson AG, Bourke S, Doe S, Cummings SP, Anderson A, Forrest T, Griffin SM, Brodlie M, Pearson J, Ward C. Microbiological profiles of sputum and gastric juice aspirates in cystic fibrosis patients. Scientific Reports. 2016;6(1):26985. doi: 10.1038/srep26985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amin et al. (2010).Amin R, Dupuis A, Aaron SD, Ratjen F. The effect of chronic infection with Aspergillus fumigatus on lung function and hospitalization in patients with cystic fibrosis. Chest. 2010;137(1):171–176. doi: 10.1378/chest.09-1103. [DOI] [PubMed] [Google Scholar]
- Anand, Clemons & Stevens (2017a).Anand R, Clemons KV, Stevens DA. Effect of anaerobiasis or hypoxia on Pseudomonas aeruginosa inhibition of Aspergillus fumigatus biofilm. Archives of Microbiology. 2017a;199(6):881–890. doi: 10.1007/s00203-017-1362-5. [DOI] [PubMed] [Google Scholar]
- Anand et al. (2017b).Anand R, Moss RB, Sass G, Banaei N, Clemons KV, Martinez M, Stevens DA. Small colony variants of Pseudomonas aeruginosa display heterogeneity in inhibiting Aspergillus fumigatus biofilm. Mycopathologia. 2017b;183(1):263–272. doi: 10.1007/s11046-017-0186-9. [DOI] [PubMed] [Google Scholar]
- Bakare et al. (2003).Bakare N, Rickerts V, Bargon J, Just-Nübling G. Prevalence of Aspergillus fumigatus and other fungal species in the sputum of adult patients with cystic fibrosis. Mycoses. 2003;46(1–2):19–23. doi: 10.1046/j.1439-0507.2003.00830.x. [DOI] [PubMed] [Google Scholar]
- Banin, Vasil & Greenberg (2005).Banin E, Vasil ML, Greenberg EP. Iron and Pseudomonas aeruginosa biofilm formation. Proceedings of the National Academy of Sciences of the United States of America. 2005;102:11076–11081. doi: 10.1073/pnas.0504266102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baxter et al. (2013a).Baxter CG, Moore CB, Jones AM, Webb AK, Denning DW. IgE-mediated immune responses and airway detection of Aspergillus and Candida in adult cystic fibrosis. Chest. 2013a;143(5):1351–1357. doi: 10.1378/chest.12-1363. [DOI] [PubMed] [Google Scholar]
- Baxter et al. (2013b).Baxter CG, Rautemaa R, Jones AM, Webb AK, Bull M, Mahenthiralingam E, Denning DW. Intravenous antibiotics reduce the presence of Aspergillus in adult cystic fibrosis sputum. Thorax. 2013b;68(7):652–657. doi: 10.1136/thoraxjnl-2012-202412. [DOI] [PubMed] [Google Scholar]
- Becker et al. (1996).Becker JW, Burke W, McDonald G, Greenberger PA, Henderson WR, Aitken ML. Prevalence of allergic bronchopulmonary aspergillosis and atopy in adult patients with cystic fibrosis. Chest. 1996;109(6):1536–1540. doi: 10.1378/chest.109.6.1536. [DOI] [PubMed] [Google Scholar]
- Blyth & Forey (1971).Blyth W, Forey A. The influence of respiratory bacteria and their biochemical fractions on Aspergillus fumigatus. Sabouraudia. 1971;9(3):273–282. doi: 10.1080/00362177185190531. [DOI] [PubMed] [Google Scholar]
- Briard et al. (2015).Briard B, Bomme P, Lechner BE, Mislin GL, Lair V, Prévost MC, Latgé JP, Haas H, Beauvais A. Pseudomonas aeruginosa manipulates redox and iron homeostasis of its microbiota partner Aspergillus fumigatus via phenazines. Scientific Reports. 2015;5(1):8220. doi: 10.1038/srep08220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briard, Heddergott & Latgé (2016).Briard B, Heddergott C, Latgé J-P. Volatile compounds emitted by Pseudomonas aeruginosa stimulate growth of the fungal pathogen Aspergillus fumigatus. MBio. 2016;7(2):e00219. doi: 10.1128/mBio.00219-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briard et al. (2017).Briard B, Rasoldier V, Bomme P, ElAouad N, Guerreiro C, Chassagne P, Muszkieta L, Latgé JP, Mulard L, Beauvais A. Dirhamnolipids secreted from Pseudomonas aeruginosa modify anjpegungal susceptibility of Aspergillus fumigatus by inhibiting β1,3 glucan synthase activity. ISME Journal. 2017;11(7):1578–1591. doi: 10.1038/ismej.2017.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cartron et al. (2006).Cartron ML, Maddocks S, Gillingham P, Craven CJ, Andrews SC. Feo—transport of ferrous iron into bacteria. BioMetals. 2006;19(2):143–157. doi: 10.1007/s10534-006-0003-2. [DOI] [PubMed] [Google Scholar]
- Chotirmall et al. (2014).Chotirmall SH, Mirkovic B, Lavelle GM, McElvaney NG. Immunoevasive Aspergillus virulence factors. Mycopathologia. 2014;178(5–6):363–370. doi: 10.1007/s11046-014-9768-y. [DOI] [PubMed] [Google Scholar]
- Cornelis & Dingemans (2013).Cornelis P, Dingemans J. Pseudomonas aeruginosa adapts its iron uptake strategies in function of the type of infections. Frontiers in Cellular and Infection Microbiology. 2013;3:75. doi: 10.3389/fcimb.2013.00075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cowley et al. (2015).Cowley ES, Kopf SH, LaRiviere A, Ziebis W, Newman DK. Pediatric cystic fibrosis sputum can be chemically dynamic, anoxic, and extremely reduced due to hydrogen sulfide formation. MBio. 2015;6(4):e00767. doi: 10.1128/mBio.00767-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cystic Fibrosis Foundation (2017).Cystic Fibrosis Foundation About cystic fibrosis. 2017. https://www.cff.org/What-is-CF/About-Cystic-Fibrosis/ https://www.cff.org/What-is-CF/About-Cystic-Fibrosis/
- De Vos et al. (2001).De Vos D, De Chial M, Cochez C, Jansen S, Tümmler B, Meyer J-M, Cornelis P. Study of pyoverdine type and production by Pseudomonas aeruginosa isolated from cystic fibrosis patients: prevalence of type II pyoverdine isolates and accumulation of pyoverdine-negative mutations. Archives of Microbiology. 2001;175(5):384–388. doi: 10.1007/s002030100278. [DOI] [PubMed] [Google Scholar]
- Dietrich et al. (2008).Dietrich LE, Teal TK, Price-Whelan A, Newman DK. Redox-active antibiotics control gene expression and community behavior in divergent bacteria. Science. 2008;321(5893):1203–1206. doi: 10.1126/science.1160619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans (2015).Evans TJ. Small colony variants of Pseudomonas aeruginosa in chronic bacterial infection of the lung in cystic fibrosis. Future Microbiology. 2015;10(2):231–239. doi: 10.2217/fmb.14.107. [DOI] [PubMed] [Google Scholar]
- Ferreira et al. (2015).Ferreira JA, Penner JC, Moss RB, Haagensen JA, Clemons KV, Spormann AM, Nazik H, Cohen K, Banaei N, Carolino E, Stevens DA. Inhibition of Aspergillus fumigatus and its biofilm by Pseudomonas aeruginosa is dependent on the source, phenotype and growth conditions of the bacterium. PLOS ONE. 2015;10(8):e0134692. doi: 10.1371/journal.pone.0134692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fillaux et al. (2012).Fillaux J, Brémont F, Murris M, Cassaing S, Rittié JL, Tétu L, Segonds C, Abbal M, Bieth E, Berry A, Pipy B, Magnaval JF. Assessment of Aspergillus sensitization or persistent carriage as a factor in lung function impairment in cystic fibrosis patients. Scandinavian Journal of Infectious Diseases. 2012;44(11):842–847. doi: 10.3109/00365548.2012.695454. [DOI] [PubMed] [Google Scholar]
- Forsyth et al. (1988).Forsyth KD, Hohmann AW, Martin AJ, Bradley J. IgG antibodies to Aspergillus fumigatus in cystic fibrosis: a laboratory correlate of disease activity. Archives of Disease in Childhood. 1988;63(8):953–957. doi: 10.1136/adc.63.8.953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaspar et al. (2013).Gaspar MC, Couet W, Olivier J-C, Pais AA, Sousa JJS. Pseudomonas aeruginosa infection in cystic fibrosis lung disease and new perspectives of treatment: a review. European Journal of Clinical Microbiology & Infectious Diseases. 2013;32(10):1231–1252. doi: 10.1007/s10096-013-1876-y. [DOI] [PubMed] [Google Scholar]
- Gibson, Sood & Hogan (2009).Gibson J, Sood A, Hogan DA. Pseudomonas aeruginosa-Candida albicans interactions: localization and fungal toxicity of a phenazine derivative. Applied and Environmental Microbiology. 2009;75(2):504–513. doi: 10.1128/AEM.01037-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goeminne et al. (2012).Goeminne PC, Vandendriessche T, Van Eldere J, Nicolai BM, Hertog ML, Dupont LJ. Detection of Pseudomonas aeruginosa in sputum headspace through volatile organic compound analysis. Respiratory Research. 2012;13(1):87. doi: 10.1186/1465-9921-13-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haas (2012).Haas H. Iron–a key nexus in the virulence of Aspergillus fumigatus. Frontiers in Microbiology. 2012;3:28. doi: 10.3389/fmicb.2012.00028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassett et al. (1992).Hassett DJ, Charniga L, Bean K, Ohman DE, Cohen MS. Response of Pseudomonas aeruginosa to pyocyanin: mechanisms of resistance, antioxidant defenses, and demonstration of a manganese-cofactored superoxide dismutase. Infection and Immunity. 1992;60:328–336. doi: 10.1128/iai.60.2.328-336.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernandez, Kappler & Newman (2004).Hernandez ME, Kappler A, Newman DK. Phenazines and other redox-active antibiotics promote microbial mineral reduction. Applied and Environmental Microbiology. 2004;70(2):921–928. doi: 10.1128/aem.70.2.921-928.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogardt & Heesemann (2010).Hogardt M, Heesemann J. Adaptation of Pseudomonas aeruginosa during persistence in the cystic fibrosis lung. International Journal of Medical Microbiology. 2010;300(8):557–562. doi: 10.1016/j.ijmm.2010.08.008. [DOI] [PubMed] [Google Scholar]
- Hunter et al. (2012).Hunter RC, Klepac-Ceraj V, Lorenzi MM, Grotzinger H, Martin TR, Newman DK. Phenazine content in the cystic fibrosis respiratory tract negatively correlates with lung function and microbial complexity. American Journal of Respiratory Cell and Molecular Biology. 2012;47(6):738–745. doi: 10.1165/rcmb.2012-0088OC. [DOI] [PubMed] [Google Scholar]
- Hunter et al. (2013).Hunter RC, Asfour F, Dingemans J, Osuna BL, Samad T, Malfroot A, Cornelis P, Newman DK. Ferrous iron is a significant component of bioavailable iron in cystic fibrosis airways. MBio. 2013;4(4):e00557-13. doi: 10.1128/mBio.00557-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Häussler & Becker (2008).Häussler S, Becker T. The pseudomonas quinolone signal (PQS) balances life and death in Pseudomonas aeruginosa populations. PLOS Pathogens. 2008;4(9):e1000166. doi: 10.1371/journal.ppat.1000166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Häussler et al. (1999).Häussler S, Tümmler B, Weissbrodt H, Rohde M, Steinmetz I. Small-colony variants of Pseudomonas aeruginosa in cystic fibrosis. Clinical Infectious Diseases. 1999;29(3):621–625. doi: 10.1086/598644. [DOI] [PubMed] [Google Scholar]
- Kerr et al. (1999).Kerr JR, Taylor GW, Rutman A, Høiby N, Cole PJ, Wilson R. Pseudomonas aeruginosa pyocyanin and 1-hydroxyphenazine inhibit fungal growth. Journal of Clinical Pathology. 1999;52(5):385–387. doi: 10.1136/jcp.52.5.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraemer et al. (2006).Kraemer R, Deloséa N, Ballinari P, Gallati S, Crameri R. Effect of allergic bronchopulmonary aspergillosis on lung function in children with cystic fibrosis. American Journal of Respiratory and Critical Care Medicine. 2006;174(11):1211–1220. doi: 10.1164/rccm.200603-423OC. [DOI] [PubMed] [Google Scholar]
- Lambiase, Catania & Rossano (2010).Lambiase A, Catania MR, Rossano F. Anaerobic bacteria infection in cystic fibrosis airway disease. New Microbiologica. 2010;33:185–194. [PubMed] [Google Scholar]
- Lau et al. (2004).Lau GW, Hassett DJ, Ran H, Kong F. The role of pyocyanin in Pseudomonas aeruginosa infection. Trends in Molecular Medicine. 2004;10(12):599–606. doi: 10.1016/j.molmed.2004.10.002. [DOI] [PubMed] [Google Scholar]
- Lee & Zhang (2015).Lee J, Zhang L. The hierarchy quorum sensing network in Pseudomonas aeruginosa. Protein & Cell. 2015;6(1):26–41. doi: 10.1007/s13238-014-0100-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manavathu, Vager & Vazquez (2014).Manavathu EK, Vager DL, Vazquez JA. Development and antimicrobial susceptibility studies of in vitro monomicrobial and polymicrobial biofilm models with Aspergillus fumigatus and Pseudomonas aeruginosa. BMC Microbiology. 2014;14(1):53. doi: 10.1186/1471-2180-14-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mangan (1969).Mangan A. Interactions between some aural Aspergillus species and bacteria. Journal of General Microbiology. 1969;58(2):261–266. doi: 10.1099/00221287-58-2-261. [DOI] [PubMed] [Google Scholar]
- Martínez & Andriantsitohaina (2009).Martínez MC, Andriantsitohaina R. Reactive nitrogen species: molecular mechanisms and potential significance in health and disease. Antioxidants & Redox Signaling. 2009;11(3):669–702. doi: 10.1089/ars.2007.1993. [DOI] [PubMed] [Google Scholar]
- Mirković et al. (2016).Mirković B, Lavelle GM, Azim AA, Helma K, Gargoum FS, Molloy K, Gernez Y, Dunne K, Renwick J, Murphy P, Moss RB, Greene CM, Gunaratnam C, Chotirmall SH, McElvaney NG. The basophil surface marker CD203c identifies Aspergillus species sensitization in patients with cystic fibrosis. Journal of Allergy and Clinical Immunology. 2016;137(2):436–443.e439. doi: 10.1016/j.jaci.2015.07.045. [DOI] [PubMed] [Google Scholar]
- Mooij et al. (2007).Mooij MJ, Drenkard E, Llamas MA, Vandenbroucke-Grauls CM, Savelkoul PH, Ausubel FM, Bitter W. Characterization of the integrated filamentous phage Pf5 and its involvement in small-colony formation. Microbiology. 2007;153(6):1790–1798. doi: 10.1099/mic.0.2006/003533-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moree et al. (2012).Moree WJ, Phelan VV, Wu CH, Bandeira N, Cornett DS, Duggan BM, Dorrestein PC. Interkingdom metabolic transformations captured by microbial imaging mass spectrometry. Proceedings of the National Academy of Sciences of the United States of America. 2012;109(34):13811–13816. doi: 10.1073/pnas.1206855109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mowat et al. (2010).Mowat E, Rajendran R, Williams C, McCulloch E, Jones B, Lang S, Ramage G. Pseudomonas aeruginosa and their small diffusible extracellular molecules inhibit Aspergillus fumigatus biofilm formation. FEMS Microbiology Letters. 2010;313(2):96–102. doi: 10.1111/j.1574-6968.2010.02130.x. [DOI] [PubMed] [Google Scholar]
- Muller (2002).Muller M. Pyocyanin induces oxidative stress in human endothelial cells and modulates the glutathione redox cycle. Free Radical Biology and Medicine. 2002;33(11):1527–1533. doi: 10.1016/s0891-5849(02)01087-0. [DOI] [PubMed] [Google Scholar]
- Nazik et al. (2017).Nazik H, Moss RB, Karna V, Clemons KV, Banaei N, Cohen K, Choudhary V, Stevens DA. Are cystic fibrosis Aspergillus fumigatus isolates different? Intermicrobial interactions with Pseudomonas. Mycopathologia. 2017;182(3–4):315–318. doi: 10.1007/s11046-016-0087-3. [DOI] [PubMed] [Google Scholar]
- Nguyen & Oglesby-Sherrouse (2015).Nguyen AT, Oglesby-Sherrouse AG. Spoils of war: iron at the crux of clinical and ecological fitness of Pseudomonas aeruginosa. BioMetals. 2015;28:433–443. doi: 10.1007/s10534-015-9848-6. [DOI] [PubMed] [Google Scholar]
- Nicolai et al. (1990).Nicolai T, Arleth S, Spaeth A, Bertele-Harms RM, Harms HK. Correlation of IgE antibody titer to Aspergillus fumigatus with decreased lung function in cystic fibrosis. Pediatric Pulmonology. 1990;8(1):12–15. doi: 10.1002/ppul.1950080106. [DOI] [PubMed] [Google Scholar]
- Noni et al. (2014).Noni M, Katelari A, Dimopoulos G, Kourlaba G, Spoulou V, Alexandrou-Athanassoulis H, Doudounakis SE, Tzoumaka-Bakoula C. Inhaled corticosteroids and Aspergillus fumigatus isolation in cystic fibrosis. Medical Mycology. 2014;52(7):715–722. doi: 10.1093/mmy/myu038. [DOI] [PubMed] [Google Scholar]
- O’Malley et al. (2003).O’Malley YQ, Reszka KJ, Rasmussen GT, Abdalla MY, Denning GM, Britigan BE. The Pseudomonas secretory product pyocyanin inhibits catalase activity in human lung epithelial cells. American Journal of Physiology-Lung Cellular and Molecular Physiology. 2003;285(5):L1077–L1086. doi: 10.1152/ajplung.00198.2003. [DOI] [PubMed] [Google Scholar]
- Paugam et al. (2010).Paugam A, Baixench MT, Demazes-Dufeu N, Burgel PR, Sauter E, Kanaan R, Dusser D, Dupouy-Camet J, Hubert D. Characteristics and consequences of airway colonization by filamentous fungi in 201 adult patients with cystic fibrosis in France. Medical Mycology. 2010;48(Suppl 1):S32–S36. doi: 10.3109/13693786.2010.503665. [DOI] [PubMed] [Google Scholar]
- Penner et al. (2016).Penner JC, Ferreira JA, Secor PR, Sweere JM, Birukova MK, Joubert LM, Haagensen JA, Garcia O, Malkovskiy AV, Kaber G, Nazik H, Manasherob R, Spormann AM, Clemons KV, Stevens DA, Bollyky PL. Pf4 bacteriophage produced by Pseudomonas aeruginosa inhibits Aspergillus fumigatus metabolism via iron sequestration. Microbiology. 2016;162(9):1583–1594. doi: 10.1099/mic.0.000344. [DOI] [PubMed] [Google Scholar]
- Phelan et al. (2014).Phelan VV, Moree WJ, Aguilar J, Cornett DS, Koumoutsi A, Noble SM, Pogliano K, Guerrero CA, Dorrestein PC. Impact of a transposon insertion in phzF2 on the specialized metabolite production and interkingdom interactions of Pseudomonas aeruginosa. Journal of Bacteriology. 2014;196(9):1683–1693. doi: 10.1128/JB.01258-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierson & Pierson (2010).Pierson LS, Pierson EA. Metabolism and function of phenazines in bacteria: impacts on the behavior of bacteria in the environment and biotechnological processes. Applied Microbiology and Biotechnology. 2010;86(6):1659–1670. doi: 10.1007/s00253-010-2509-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pressler et al. (2006).Pressler T, Frederiksen B, Skov M, Garred P, Koch C, Høiby N. Early rise of anti-pseudomonas antibodies and a mucoid phenotype of pseudomonas aeruginosa are risk factors for development of chronic lung infection—a case control study. Journal of Cystic Fibrosis. 2006;5(1):9–15. doi: 10.1016/j.jcf.2005.11.002. [DOI] [PubMed] [Google Scholar]
- Price-Whelan, Dietrich & Newman (2006).Price-Whelan A, Dietrich LE, Newman DK. Rethinking ‘secondary’ metabolism: physiological roles for phenazine antibiotics. Nature Chemical Biology. 2006;2(2):71–78. doi: 10.1038/nchembio764. [DOI] [PubMed] [Google Scholar]
- Reece et al. (2017).Reece E, Segurado R, Jackson A, McClean S, Renwick J, Greally P. Co-colonisation with Aspergillus fumigatus and Pseudomonas aeruginosa is associated with poorer health in cystic fibrosis patients: an Irish registry analysis. BMC Pulmonary Medicine. 2017;17(1):70. doi: 10.1186/s12890-017-0416-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reen et al. (2016).Reen FJ, Phelan JP, Woods DF, Shanahan R, Cano R, Clarke S, McGlacken GP, O’Gara F. Harnessing bacterial signals for suppression of biofilm formation in the nosocomial fungal pathogen Aspergillus fumigatus. Frontiers in Microbiology. 2016;7:2074. doi: 10.3389/fmicb.2016.02074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reichhardt et al. (2015).Reichhardt C, Ferreira JA, Joubert LM, Clemons KV, Stevens DA, Cegelski L. Analysis of the Aspergillus fumigatus biofilm extracellular matrix by solid-state nuclear magnetic resonance spectroscopy. Eukaryotic Cell. 2015;14(11):1064–1072. doi: 10.1128/EC.00050-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson & Bye (2002).Robinson M, Bye PT. Mucociliary clearance in cystic fibrosis. Pediatric Pulmonology. 2002;33(4):293–306. doi: 10.1002/ppul.10079. [DOI] [PubMed] [Google Scholar]
- Salsgiver et al. (2016).Salsgiver EL, Fink AK, Knapp EA, LiPuma JJ, Olivier KN, Marshall BC, Saiman L. Changing epidemiology of the respiratory bacteriology of patients with cystic fibrosis. Chest. 2016;149(2):390–400. doi: 10.1378/chest.15-0676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sass et al. (2018).Sass G, Nazik H, Penner J, Shah H, Ansari SR, Clemons KV, Groleau MC, Dietl AM, Visca P, Haas H, Déziel E, Stevens DA. Studies of Pseudomonas aeruginosa mutants indicate pyoverdine as the central factor in inhibition of Aspergillus fumigatus biofilm. Journal of Bacteriology. 2018;200(1):e00345-17. doi: 10.1128/JB.00345-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schrettl et al. (2004).Schrettl M, Bignell E, Kragl C, Joechl C, Rogers T, Arst HN, Haynes K, Haas H. Siderophore biosynthesis but not reductive iron assimilation is essential for Aspergillus fumigatus virulence. Journal of Experimental Medicine. 2004;200(9):1213–1219. doi: 10.1084/jem.20041242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Secor et al. (2017).Secor PR, Sass G, Nazik H, Stevens DA. Effect of acute predation with bacteriophage on intermicrobial aggression by Pseudomonas aeruginosa. PLOS ONE. 2017;12(6):e0179659. doi: 10.1371/journal.pone.0179659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shirazi et al. (2016).Shirazi F, Ferreira JA, Stevens DA, Clemons KV, Kontoyiannis DP. Biofilm filtrates of Pseudomonas aeruginosa strains isolated from cystic fibrosis patients inhibit preformed Aspergillus fumigatus biofilms via apoptosis. PLOS ONE. 2016;11(3):e0150155. doi: 10.1371/journal.pone.0150155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shoseyov et al. (2006).Shoseyov D, Brownlee KG, Conway SP, Kerem E. Aspergillus bronchitis in cystic fibrosis. Chest. 2006;130(1):222–226. doi: 10.1378/chest.130.1.222. [DOI] [PubMed] [Google Scholar]
- Skov et al. (2005).Skov M, McKay K, Koch C, Cooper PJ. Prevalence of allergic bronchopulmonary aspergillosis in cystic fibrosis in an area with a high frequency of atopy. Respiratory Medicine. 2005;99(7):887–893. doi: 10.1016/j.rmed.2004.11.018. [DOI] [PubMed] [Google Scholar]
- Smith et al. (2015).Smith K, Rajendran R, Kerr S, Lappin DF, Mackay WG, Williams C, Ramage G. Aspergillus fumigatus enhances elastase production in Pseudomonas aeruginosa co-cultures. Medical Mycology. 2015;53(7):645–655. doi: 10.1093/mmy/myv048. [DOI] [PubMed] [Google Scholar]
- Smith & Iglewski (2003).Smith RS, Iglewski BH. Pseudomonas aeruginosa quorum sensing as a potential antimicrobial target. Journal of Clinical Investigation. 2003;112:1460–1465. doi: 10.1172/JCI20364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Speirs, Van Der Ent & Beekman (2012).Speirs JJ, Van Der Ent CK, Beekman JM. Effects of Aspergillus fumigatus colonization on lung function in cystic fibrosis. Current Opinion in Pulmonary Medicine. 2012;18(6):632–638. doi: 10.1097/MCP.0b013e328358d50b. [DOI] [PubMed] [Google Scholar]
- Stevens et al. (2003).Stevens DA, Moss RB, Kurup VP, Knutsen AP, Greenberger P, Judson MA, Denning DW, Crameri R, Brody AS, Light M, Skov M, Maish W, Mastella G, Conference PitCFFC Allergic bronchopulmonary aspergillosis in cystic fibrosis—state of the art: cystic fibrosis foundation consensus conference. Clinical Infectious Diseases. 2003;37(Suppl 3):S225–S264. doi: 10.1086/376525. [DOI] [PubMed] [Google Scholar]
- Toljander et al. (2007).Toljander JF, Lindahl BD, Paul LR, Elfstrand M, Finlay RD. Influence of arbuscular mycorrhizal mycelial exudates on soil bacterial growth and community structure. FEMS Microbiology Ecology. 2007;61(2):295–304. doi: 10.1111/j.1574-6941.2007.00337.x. [DOI] [PubMed] [Google Scholar]
- Tramper-Stranders et al. (2012).Tramper-Stranders GA, Van Der Ent CK, Molin S, Yang L, Hansen SK, Rau MH, Ciofu O, Johansen HK, Wolfs TF. Initial Pseudomonas aeruginosa infection in patients with cystic fibrosis: characteristics of eradicated and persistent isolates. Clinical Microbiology and Infection. 2012;18(6):567–574. doi: 10.1111/j.1469-0691.2011.03627.x. [DOI] [PubMed] [Google Scholar]
- Valenza et al. (2008).Valenza G, Tappe D, Turnwald D, Frosch M, Konig C, Hebestreit H, Abele-Horn M. Prevalence and antimicrobial susceptibility of microorganisms isolated from sputa of patients with cystic fibrosis. Journal of Cystic Fibrosis. 2008;7(2):123–127. doi: 10.1016/j.jcf.2007.06.006. [DOI] [PubMed] [Google Scholar]
- Visaggio et al. (2015).Visaggio D, Pasqua M, Bonchi C, Kaever V, Visca P, Imperi F. Cell aggregation promotes pyoverdine-dependent iron uptake and virulence in Pseudomonas aeruginosa. Frontiers in Microbiology. 2015;6:902. doi: 10.3389/fmicb.2015.00902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, Kern & Newman (2010).Wang Y, Kern SE, Newman DK. Endogenous phenazine antibiotics promote anaerobic survival of Pseudomonas aeruginosa via extracellular electron transfer. Journal of Bacteriology. 2010;192(1):365–369. doi: 10.1128/JB.01188-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang et al. (2011).Wang Y, Wilks JC, Danhorn T, Ramos I, Croal L, Newman DK. Phenazine-1-carboxylic acid promotes bacterial biofilm development via ferrous iron acquisition. Journal of Bacteriology. 2011;193:3606–3617. doi: 10.1128/JB.00396-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whiteson et al. (2014).Whiteson KL, Meinardi S, Lim YW, Schmieder R, Maughan H, Quinn R, Blake DR, Conrad D, Rohwer F. Breath gas metabolites and bacterial metagenomes from cystic fibrosis airways indicate active pH neutral 2,3-butanedione fermentation. ISME Journal. 2014;8(6):1247–1258. doi: 10.1038/ismej.2013.229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson et al. (1988).Wilson R, Sykes DA, Watson D, Rutman A, Taylor GW, Cole PJ. Measurement of Pseudomonas aeruginosa phenazine pigments in sputum and assessment of their contribution to sputum sol toxicity for respiratory epithelium. Infection and Immunity. 1988;56:2515–2517. doi: 10.1128/iai.56.9.2515-2517.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Worlitzsch et al. (2002).Worlitzsch D, Tarran R, Ulrich M, Schwab U, Cekici A, Meyer KC, Birrer P, Bellon G, Berger J, Weiss T, Botzenhart K, Yankaskas JR, Randell S, Boucher RC, Döring G. Effects of reduced mucus oxygen concentration in airway Pseudomonas infections of cystic fibrosis patients. Journal of Clinical Investigation. 2002;109(3):317–325. doi: 10.1172/JCI13870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao et al. (2018).Zhao J, Cheng W, He X, Liu Y. The co-colonization prevalence of Pseudomonas aeruginosa and Aspergillus fumigatus in cystic fibrosis: a systematic review and meta-analysis. Microbial Pathogenesis. 2018;125:122–128. doi: 10.1016/j.micpath.2018.09.010. [DOI] [PubMed] [Google Scholar]
- Zhao et al. (2012).Zhao J, Schloss PD, Kalikin LM, Carmody LA, Foster BK, Petrosino JF, Cavalcoli JD, VanDevanter DR, Murray S, Li JZ, Young VB, LiPuma JJ. Decade-long bacterial community dynamics in cystic fibrosis airways. Proceedings of the National Academy of Sciences of the United States of America. 2012;109(15):5809–5814. doi: 10.1073/pnas.1120577109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng, Keller & Wang (2015a).Zheng H, Keller NP, Wang Y. Establishing a biofilm co-culture of Pseudomonas and Aspergillus for Metabolite Extraction. Bio-Protocol. 2015a;5(23):e1667. doi: 10.21769/BioProtoc.1667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng et al. (2015b).Zheng H, Kim J, Liew M, Yan JK, Herrera O, Bok JW, Kelleher NL, Keller NP, Wang Y. Redox metabolites signal polymicrobial biofilm development via the NapA oxidative stress cascade in Aspergillus. Current Biology. 2015b;25(1):29–37. doi: 10.1016/j.cub.2014.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The following information was supplied regarding data availability:
The research in this article did not generate any data or code. This is a literature review.