Abstract
Purpose
Childhood reactive airway diseases (RADs) are concerning problems in children’s airways and may be preceded by bronchiolitis and may progress to childhood asthma. The severity of the disease is indicated by deterioration in pulmonary functions, increased usage of rescue medications, and recurrent wheezing episodes. Macrolides have both antimicrobial and anti-inflammatory functions and have been used as adjunctive therapy in childhood RADs.
Patients and methods
We conducted a meta-analysis to evaluate the effect of macrolides in children with RAD. Literature searches were systematically conducted using an electronic database from inception to August 2018. The Cochrane review risk of bias assessment tool was used to assess the quality of each randomized controlled trial.
Results
Sixteen randomized controlled trials comprising 1,415 participants were investigated in this meta-analysis. Children treated with macrolide therapy showed significantly better pulmonary functions in both forced expiratory volume in one second (% predicted) (difference in means=−9.77, 95% CI=−14.18 to −5.35, P<0.001; I2=0%) and forced expiratory flow 25–75 (% predicted) (difference in means=−14.14, 95% CI=−26.11 to −2.18, P=0.02; I2=29.56%). In addition, the short-acting β-agonist usage days and recurrent wheezing risk were significantly lowered in children with macrolide treatment (standardized difference in means=−0.34, 95% CI=−0.59 to −0.09, P=0.007, I2=27.05% and standardized difference in means=−0.53, 95% CI=−0.81 to −0.26, P<0.001, I2=0%, respectively). Furthermore, the growth of Moraxella catarrhalis from nasal swabs was less in children treated with macrolides (odds ratio=0.19, 95% CI=0.11–0.35, P<0.001). Children who took macrolides had a lower risk of adverse events (risk ratio=0.83, 95% CI=0.70–0.98, P=0.024, I2=0%).
Conclusion
This current meta-analysis suggested that adjunctive therapy with macrolides is safe and effective for achieving better outcomes in childhood RAD.
Keywords: macrolides, childhood, asthma, recurrent wheezing, bronchiolitis, pulmonary function, efficacy, reactive airway disease
Introduction
Asthma remains a significant burden in both developing and developed countries and causes morbidity and mortality.1 Acute exacerbation in both partially and poorly controlled asthma is the major factor contributing to morbidity and the cost of insurance, particularly in children.2 Childhood asthma is often preceded by acute, severe, and recurrent episodes of severe lower respiratory tract infections in the initial years of life.3 Nearly one-third of preschool children present with recurrent wheezing during the first 5–6 years of life.4 Among children diagnosed with recurrent wheezing or asthma, ~20% of them visit emergency departments (EDs), and 7% of them are hospitalized each year, which are major stresses for both families and health care resources.5–7 Infants hospitalized with bronchiolitis are at significantly increased risk for both recurrent wheezing and childhood asthma.8 There are overlapping characteristics and similarities among childhood asthma, recurrent wheezing and bronchiolitis, and they may be considered to be one disease in different periods of time in some children. Therefore, the differentiation of specific reactive airway disease (RAD) entities in clinical practice is often not possible.
There has been little progress in the treatment of asthma exacerbations and long-term care over the past 20 years, as well as limited evidence for the management and prevention of preschool wheezing. High doses of inhaled steroids administered early have been proved to prevent severe asthma exacerbations in adolescents and adults while posing a risk of diminished linear growth in children with asthma.9,10 Furthermore, only hydration, oxygen, and the use of inhaled short-acting β2 agonists (SABAs) have shown evidence of being successful for the treatment of preschool childhood wheezing.11,12 Finally, there has been no effective treatment to change the long-term disease course in childhood asthma, recurrent wheezing, and bronchiolitis. Thus, identification of a better treatment to alleviate the severity of both asthma exacerbation and recurrent wheezing is of clinical importance.
There is emerging evidence that both viral and bacterial agents play important roles in the pathogenesis of both asthma exacerbations in children and recurrent wheezing in young infants.13–15 Viral agents such as rhinovirus are significant factors in disease progression from bronchiolitis to asthma and in triggering asthma exacerbations.16 Atypical infections are common in pediatric severe asthma and severe chronic bronchitis and likely are pathogenic across the broad spectrum of RAD syndromes.17–20 Of the causative pathogens, both Mycoplasma pneumoniae and Chlamydia pneumoniae are strongly associated with new-onset asthma, recurrent wheezing, refractory bronchitis, acute bronchiolitis, and asthma exacerbations in children.18,21–24 It has been reported that C. pneumoniae infection is common in school-age children and the immune response to chronic C. pneumoniae infection may intercommunicate with allergic inflammation to exacerbate asthma symptoms.15 In patients with asthma with M. pneumoniae infection, the use of macrolides may alleviate the symptoms of asthma. In addition, treatment with clarithromycin in patients with asthma who are colonized with mycoplasma and chlamydia species led to a reduction in pro-inflammatory and T-helper 2 cytokines, such as tumor necrosis factor-alpha, IL-5, and IL-12 mRNA, in bronchoalveolar lavage (BAL) and airway tissue.25,26 Recently, a toxin produced by M. pneumoniae, the community acquired respiratory distress syndrome (CARDS) toxin was identified.27 Although without statistical significance, Wood et al declared a strong correlation between poor asthma control and testing positive for CARDS toxin and concluded that CARDS toxin could deteriorate asthma symptoms.28 In addition, the upper airway colonization with capsular polysaccharide bacteria can predict subsequent recurrent wheezing and asthma diagnosis at the age of 5 years.29 These studies provide a foundation for the use of macrolides in children with asthma and recurrent wheezing.
In addition to the well-established antimicrobial activity of macrolides, they have also been characterized to have an anti-inflammatory effect.30,31 The immunomodulatory activity of macrolides has been hypothesized to have a role in the therapy of chronic inflammatory airway diseases, such as asthma and COPD.32,33 Previous serial studies34,35 in adult asthma patients have shown the benefits of 6–12 weeks of azithromycin treatment in the improvement of overall asthma symptoms. They discussed both the anti-inflammatory and antimicrobial mechanism of azithromycin, and finally proved that the anti-inflammatory effects wane after the treatment is completed, whereas the antimicrobial effects persist at 1 year of follow-up.35 Johnston et al reported that the early use of telithromycin in an acute asthma episode significantly improved symptom scores and lung function compared with a control group irrespective of the bacteriological status, implicating a non-antimicrobial mechanism.36 A recent report also showed that azithromycin treatment during respiratory syncytial virus (RSV) bronchiolitis not only reduced airway IL-8 levels and overall respiratory morbidity but also prolonged the time to a third wheezing episode.37
A previous meta-analysis published by the Cochrane library tried to elucidate the role of macrolides for chronic asthma and reported positive effects for both forced expiratory volume in one second (FEV1) and asthma symptoms;38 however, each results included almost adult studies with only one child study in each result and may be insufficient to represent the true condition in children. Another meta-analysis only included children under 2 years of age, and the limited number of studies provided insufficient data for final analysis due to the heterogeneous outcomes between the included studies.39 In addition, the analysis39 included antibiotics other than macrolides and also showed no benefits. Such results may be related to the variability of adult asthma and childhood asthma. Therefore, it may be the reason why there is currently no clear evidence that the use of macrolides in the treatment of childhood wheezing is of significant clinical benefit.
Since the two meta-analyses conducted in 2014, several new reports have been published within the past 4 years.37,40–43 To update the published data and focus this issue precisely on the specific age group and the extended effects of macrolides, we conducted this detailed meta-analysis of the effects of macrolides in children with RAD, such as bronchiolitis, recurrent wheezing, and asthma.
Methods
This systematic review and meta-analysis were conducted in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) guidelines (Table S1).44 We searched the following databases from inception to the end of August 2018: Embase, PubMed, and the Cochrane Library and the Cumulative Index to Nursing and Allied Health Literature (CINAHL). We used the keywords “Asthma” or “Chronic cough” or “infantile asthma” or “wheezing” or “wheez*” and “Erythromycin” or “Azithromycin” or “Zithromax” or “Clarithromycin” or “macrolide(s)” in our search. Our strategy is shown in Table S2. To ensure a comprehensive search, we did not limit the language, year or type of publication. Two authors (W-TL and S-JL) conducted the search independently, and disagreements were resolved through discussion with the third author (T-LY).
Study selection and methodological quality assessment
After the initial search, two independent reviewers (W-TL and T-LY) scanned each abstract from the search publications to identify trials that met the inclusion criteria for systematic review and meta-analysis. Two review authors (W-TL and T-LY) independently reviewed the full-text articles of the retrieved trials that met the inclusion criteria. The randomized controlled trials (RCTs) included met all of the following eligibility criteria: 1) focused on human children aged <18 years; 2) included a control group, including concurrent use of inhaled corticosteroid (ICS), Montelukast, long-acting and short-acting bronchodilators, in the study design; 3) included the use of a macrolide such as troleandomycin, erythromycin, azithromycin, or clarithromycin by the intervention group; 4) investigated the efficacy of macrolide treatment in children with asthma/recurrent wheezing/chronic bronchitis/acute bronchiolitis; and 5) provided data for clinical disease control and serological biomarkers change. We excluded the following: 1) articles irrelevant to the topic, 2) duplicate publications and populations, 3) trials of a crossover study design, and 4) studies without sufficient data for extracting or calculating the pooled analysis. Quality assessment of all included studies was conducted independently by four researchers (M-CT, H-HC, Y-JC, and HHL) using the Cochrane review risk of bias assessment tool.45 The adequacy of randomization, allocation concealment, blinding methods, implementation of the intention-to-treat analysis, dropout rate, complete outcome data, selective data reporting, and other biases was assessed. Each domain was categorized as low, high, or unclear.
Data extraction and analysis
Five authors (M-CT, H-HC, Y-JC, HHL, and CYL) independently extracted the data from all included studies, and the following data were collected: first author’s name, year of publication, country of publication, number of patients, age of patients, sex ratio of patients, number of patients in the intervention and control groups, type of intervention (including the length of treatment), concomitant treatment and baseline medications, clinical outcome measures (including the timing of the outcome in relation to the treatment and the outcome persistent after treatment), and severe adverse effects.
Meta-analysis
Because of the significant heterogeneity expected among the participants of all the included studies, a random-effect model was used rather than the fixed-effect model.46 Comprehensive Meta-Analysis software version 3 (Biostat, Englewood, NJ, USA) was used for all the analyses. Dichotomous data were calculated using an OR or risk ratio with 95% CI. Difference in means (MD) or standardized difference in means (SMD) with 95% CI was used for analysis of continuous outcomes. Heterogeneity was quantified with the Q test and I2 statistics to evaluate the dispersion of the true effect of the included trials.47 Publication bias was evaluated by visual inspection of the funnel plots and Egger’s tests.48 Subgroup analysis was performed to further analyze the effects of clinical variables as possible origins of heterogeneity, such as duration of macrolides, type of macrolides, and the different age group. Finally, meta-regression analyses were conducted only when data could be assessed throughout more than five trials.
Results
Description of studies and quality assessment
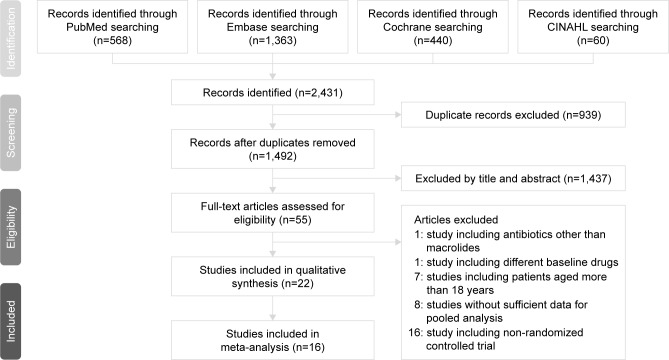
Initial database searching disclosed the following results: 568 studies in PubMed, 1,363 studies in Embase, 440 studies in Cochrane, and 60 studies in CINAHL. Of these 2,431 articles, we excluded 939 articles because of the duplications of studies. Of the remaining 1,492 articles, we excluded another 1,437 studies on the basis of title and abstract alone and retained 55 studies. Among the 55 studies, 16 studies were non-RCTs, 8 studies were without sufficient data for pooled analysis, 7 studies included participants over 18 years of age, 1 study used antibiotics other than macrolides as intervention medications, and the baseline controller medications between the intervention and control group in one study were different. Therefore, a total of 22 RCTs were included in our systemic review. Figure 1 shows the searching process. Most of the included studies showed low bias using the Cochrane assessment tool.
Figure 1.
The Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) flow diagram.
Demographics
Among the 22 RCTs, a total of 2,091 participants with ages ranging from 0 to 18 years were enrolled. These studies were held worldwide, with eight studies in the USA;32,37,42,49–51 three trials in Brazil;52–54 two trials each in Australia/New Zealand55,56 and Bangladesh;57,58 and one trial each in the Philippines,59 Taiwan,40 Turkey,60 Greece,61 Italy,62 Denmark,43 and Canada.41 Eight RCTs enrolled children with an underlying asthma diagnosis with or without hospitalization or an ED visit, mostly aged more than 5 years;32,40,49–51,59,61,62 11 studies enrolled toddlers hospitalized because of bronchiolitis aged less than 3 years 37,41,43,52–58,60,63,64 and 2 trials recruited children aged 12–71 months with recurrent wheezing with an ED visit.41,42 Three studies shared identical patient groups with different outcome assessments.37,56,63 Other characteristics of the included trials are listed in Table 1.
Table 1.
Characteristics of randomized controlled trials using macrolides on children with asthma, recurrent wheezing and bronchiolitis
| Reference | Country | Population (M%:F%) | Age (range/mean±SD) | Intervention:control | Intervention | Concomitant/baseline medication (I:C) % | Outcome measure | Severe adverse events (%) |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Ball et al 199049 | USA | 15 children severe, steroid-requiring asthma | 8–18 years (13.1±3.0) 13.8±3.0 vs 12.4±3.2 | 5:5:5 | Troleandomycin 250 mg QD × 2 days the QOD × 7 times, totally 2 weeks | Methyl-prednisolone 40 mg/1.73 m2 | Steroid dose reduction, symptoms scores, morning plasma cortisol concentration, FEV1, FVC, TGV, methacholine PC20, eosinophil count after 2 weeks, methylprednisolone clearance | Nil |
| Kamada et al 199350 | USA | 18 children severe, steroid- requiring asthma (36%:64%) | 6–17 years 14.3±2.9 vs 11.3±2.7 | 6:7:5 | Troleandomycin 250 mg QD or QOD depending on steroid protocol for 12 weeks | Prednisolone ≥20 mg QOD, bronchodilator ≥4 times/day, theophylline, ICS 500–1,000 µg BID | Steroid dose reduction, symptoms scores, need for extra prednisolone, PEFR, pre-bronchodilator FEV1, FEF 25%–75%, methacholine PC20, morning plasma cortisol concentration, urinary cortisol excretion, bone density, hip flexor strength after 12 weeks | Abnormal liver function (7.6%) |
| Fonseca-Aten et al 200632 | USA | 43 children history of recurrent wheezing/asthma with an AE to ED (74%:26%) | 4–17 years 112.5 (62–187) vs 100 (50–181) months | 22:21 | Clarithromycin 15 mg/kg/day, BID for 5 days, orally | SABA (39 of 43), LABA (3 of 43), and/or ICS (12 of 43) | serum/nasopharyngeal aspirates: TNF-α, IFN-γ, IL-1β, IL-2, IL-4, IL-5, IL-6, IL-8, IL-10, GM-CSF, RANTES, eotaxin, MIP-1α, MIP-1β, MCP-1; Mycoplasma pneumoniae, Chlamydia pneumoniae detection in nasopharyngeal swabs/serologic test; dyspnea, wheeze, cough, asthma score | NR |
| Piacentini et al 200762 | Italy | 16 children hospitalized for asthma (75%:25%) | 13.9±2.4 vs 12.9±2.6 | 8:8 | Azithromycin 10 mg/kg QD for 3 consecutive days/week × 8 weeks | ICS (fluticasone, 100–200 µg/day; beclomethasone dipropionate, 200–400 µg/day), SABA as needed | FEV1, FVC, FEF 25%–75%, bronchial hyper-responsiveness (expressed as the dose– response slope of FEV1 fall after hypertonic saline inhalation, and induced sputum) | NR |
| Tahan et al 200760 | Turkey | 21 infants hospitalized for RSV bronchiolitis, first episode of wheezing (57%:43%) | ≥7 months 2 (1–6) vs 2 (1–7) | 12:9 | Clarithromycin (15 mg/kg) QD × 3 weeks | β2-agonist (when SpO <94%, 2 RR >60 breaths/min, wheezing on auscultation, respiratory distress) | Primary outcome: LOS; duration of need for O2, IVF and β2-agonist Secondary outcomes: changes in the IL-4, IL-8, eotaxin, IFN-γ levels, readmission rate 6 months after discharge | NR |
| Rasul et al 200857 | Bangladesh | 60 children hospitalized for bronchiolitis (72%:28%) | 0–2 years (80% below 6 months) | 15:22:23 | Erythromycin orally | O2(for those with SpO2, 95%) and nebulization | Progress of the symptoms after 72 hours, progress of the signs after 72 hours, outcomes of bronchiolitis (improved, deteriorated, hospital stay) | NR |
| Strunk et al 200851 | USA | 55 children moderate-to-severe persistent asthma (58%:42%) | 6–18 years (11.2±2.6) | 17:19:19 | Azithromycin 250 mg QD (for those 25–40 kg) or 500 mg QD (for those .40 kg) | Budesonide 400–800 µg BID; Serevent Diskus® 50 µg BID (run-in/post randomized) | Primary outcome: time to inadequate asthma control M. pneumoniae, C. pneumoniae detection in nasal washes: PCR assays | NR |
| Kabir et al 200958 | Bangladesh | 295 children hospitalized for breathing difficulty/chest indrawing (73%:27%) | ,24 months | 99:99:97 IV ampicillin: oral erythromycin: no antibiotics (P-Ab: O-Ab: N-Ab) | P-Ab (50 mg/kg/dose 6 hourly IV) O-Ab (10 mg/kg/dose 6 hourly) | Nebulized salbutamol at 0.15 mg/kg/6–8 hours, O2 inhalation (SpO2 <90%), IVF maintenance | 18 symptoms/signs which were graded on a two-point recovery scale of “rapid” and “gradual”, indicating improvement within “four days” and “beyond four days”, respectively | NR |
| Koutsoubari et al 201261 | Greece | 40 children intermittent/mild persistent asthma with an acute AE (45%:55%) | 6–14 years 9.1±2.7 vs 8.4±2.5 | 18:22 | Clarithromycin 15 mg/kg × 3 weeks | Prophylactic treatment according to asthma control level (GINA) ICS (61.1:59.1) | Primary outcome: days without symptoms within subsequent 12 weeks. Secondary outcome: symptom-free days after first AE, number/severity of periods with loss of control, time to first loss of control, PEFR variability, duration of the index episode, FEV1, mean daily morning PEFR; RT-PCR in nasal wash samples | NR |
| Pinto et al 201252 | Brazil | 184 infants hospitalized with AB (60%:40%) | ≥2 months 3.1±2.2 vs 3.1±2.3 | 88:96 | Azithromycin 10 mg/kg/day × 7 days | Antibiotics (4.5:6.3); Steroid (4.5:7.3); bronchodilator (20.5:21.8) | Primary outcomes: LOS, duration of O2 Other variables: antibiotic use, broncho-dilators use, admission to the PICU, immunofluorescence for adenovirus, parainfluenza, influenza, RSV | NR |
| Mccallum et al 201355 | Australia/New Zealand | 96 children hospitalized, O2-required bronchiolitis (68%:32%) | ≥18 months 5.3 (3–9.4) vs 5 (3–8.5) | 50:46 | Azithromycin (30 mg/kg), single large dose of oral liquid | Antibiotics (72.0:70.0); Supplemental IVF (38.0:41.0) | Primary endpoints: LOS, duration of O2 Other outcomes: any respiratory-related readmissions in 6 months of discharge, identification of respiratory viruses and bacterial pathogens (RT-PCR/culture) | Nil |
| Chiong-Manaysay and Andaya 201459,a | Philippines | 23 children with FEV1 <80% before treatment | Children | 13:10 | Clarithromycin 15 mg/kg/day bid × 3 weeks | NR | Asthma Control Test questionnaires and spirometry (FVC, FEV1, FEV1/FVC, FEF 25%–75% and PEFR) prior medication and after the study period | NR |
| Bacharier et al 2015 42 | USA | 443 children histories of recurrent, severe wheezing (62%:38%) | 12–71 months (41.5±16.5) 42.5±16.4 vs 40.2±16.6 | 223:220 RTIs 473:464 | Azithromycin 12 mg/kg/day × 5 days | Albuterol 4 times daily for the first 48 hours/whenever needed at any time during the RTI | Primary outcome: number of RTIs not progressing to a severe LRTI (prescription of oral corticosteroids) Secondary outcome: numbers of urgent care/ED visits, hospitalizations. Symptom scores, albuterol use, time to second RTI | Nil |
| Beigelman et al 2015 37 | USA | 39 infants hospitalized with RSV bronchiolitis (59%:41%) | 1–18 months (3.8±2.9) 3.7±3.7 vs 3.9±2.0 | 19:20 | Azithromycin 10 mg/kg/day × 7 days then 5 mg/kg/day × 7 days | Antibiotic treatment (0:2); hypertonic saline treatment (1:0) | Primary outcomes: serum and nasal lavage IL-8 levels, proportion of participants with ≥2 additional wheezing episodes after treatment Secondary outcomes: proportion of participants with ≥3 wheezing episodes, with diagnosed asthma, being-prescribed with ICS, the time to second and third episode, the number of, ED visits for respiratory symptoms, courses of OCS, days of rescue albuterol, days with respiratory symptoms | Nil |
| Beigelman et al 2015 63 | USA | 39 children hospitalized with RSV infection (59%:41%) | 1–18 months (3.8±2.9) 3.7±3.7 vs 3.9±2.0 | 19:20 | Azithromycin 10 mg/kg/day × 7 days then 5 mg/kg/day × 7 days | Antibiotic treatment (0:2); hypertonic saline treatment (1:0) | RSV load in nasal lavage samples obtained on randomization, day 8, and day 15 | Nil |
| Mccallum et al 2015 56 | Australia/New Zealand | 219 children hospitalized with bronchiolitis (62%:38%) | ≥24 months 5.7 (3–10) vs 5.6 (3–9) | 106:113 (LOS/6-month readmission) 59:74 (O2 duration) 100:110 (day 21 clinical review) | Azithromycin 30 mg/kg/dose weekly × 3 times | Nonmacrolide antibiotics prescribed prior to hospital (45.0:42.0); during hospital (61.0:60.0); IVF (23.0:20.0) | Primary endpoint: LOS, duration of O2, day 21 clinical review, 6 months readmission; microbiology: Nasopharyngeal swabs for virus/bacteria (RT-PCR/culture) | Nil |
| Silveira D’Azevedo V et al 201653,a | Brazil | 91 infants hospitalized with AB | <12 months | 51:40 | Azithromycin × 7 days | NR | Wheezing and hospitalization in a follow-up 1, 3, and 6 months after the AB | NR |
| Stokholm et al 2016 43 | Denmark | 72 children recurrent asthma- like symptoms, troublesome lung symptoms ≥3 days (65%:35%) | 1–3 years 2.0±0.6 | 74:74 episodes | Azithromycin 10 mg/kg/day × 3 days | ICS (84%:80%); Montelukast (64.0:57.0) | Primary outcome: duration of episodes of troublesome lung symptoms after initiation of treatment Secondary outcomes: time from treatment to the next episode of troublesome lung symptoms, episodes that turned into severe AE (need for oral steroids/hospitalization), and the duration of β2 agonist use after treatment | 1:1 Hospitalized for AGE: 4 days after randomized Hospitalized for pneumonia: 20 days after randomized |
| Wan et al 2016 40 | Taiwan | 56 children with mild persistent asthma (63%:37%) | 5–16 years 10.1±3.1 vs 10.2±3.1 | 36:20 | Clarithromycin 5 mg/kg/day × 4 weeks | Fluticasone propionate 50 µg/puff bid | Childhood asthma control test, FEV1, FEF 25%–75%, FeNO, total IgE, absolute eosinophil count, ECP level | NR |
| Zhou et al 2016 64 | USA | 39 infants hospitalized with first RSV bronchiolitis (59%:41%) | 1–18 months (3.8±2.9) 3.7±3.7 vs 3.9±2.0 | 19:20 | Azithromycin 10 mg/kg/day × 7 days then 5 mg/kg/day × 7 days | Antibiotic treatment (0:2); hypertonic saline treatment (1:0) | Recurrent wheezing: assessed monthly over a year following the initial episode Microbiome sequencing ≥ changes in nasal lavage microbial communities following the study treatments | Nil |
| Mandhane et al 2017 41 | Canada | 222 children presenting to ED with wheezing (72%:28%) | 12–60 months 34.8±13.6 vs 30.5±13.9 | 110:112 (primary analysis); 87:82 (secondary analysis) | Azithromycin 10 mg/kg/day at day 1 then 5 mg/kg/day × 4 days (day 2–5) | Prior ED: ICS (62.7:58.9) SABA (35.5:36.6); At ED discharge: SABA (79.1:73.2) OCS (59.1:62.5) ICS (57.3:50.9) | Primary outcome: time (days) to respiratory symptoms resolution Secondary outcomes: the number of days children used a SABA during the 21 day follow-up, time to disease exacerbation during the following 6 months | Nil |
| Pinto et al 2017 54,a | Brazil | 83 infants hospitalized with AB | <12 months | 46:37 | Azithromycin × 7 days | NR | LOS, identification of respiratory viruses, recurrent wheezing/hospital readmission post-AB | NR |
Note:
Studies have been only reported as abstracts.
Abbreviations: AB, acute bronchiolitis; AE, acute exacerbation; AGE, acute gastroenteritis; BHR, bronchial hyper-responsiveness; BID, twice per day; C, control; DRS, dose response slope; ECP, eosinophil cation protein; ED, emergency department; F, female; FEV1, forced expiratory volume in one second; FVC, forced vital capacity; FeNO, fractional exhaled nitric oxide; FEF 25%–75%, forced expiratory flow between 25% and 75% of vital capacity; GINA, Global Initiative For Asthma; GM-CSF, granulocyte-macrophage colony stimulating factor; I, intervention; ICS, inhaled corticosteroid; IL, interleukin; ICU, intensive care unit; IFN, interferon; IV, intravenous; IVF, intravenous fluid; LABA, long-acting inhaled β-agonist; LOS, length of stay; LRTI, lower respiratory tract infection; LTRA, leukotriene receptor antagonist; M, male; MCP, monocyte chemoattractant protein; MIP, macrophage inflammatory protein; methacholine PC20, concentration of methacholine required to induce a 20% decrease in FEV1; NR, not reported; PEFR, peak expiratory flow rate; QD, every day; QOD, every other day; RR, respiratory rate; RSV, respiratory syncytial virus; RTI, respiratory tract infection; RT-PCR, real-time polymerase chain reaction; SpO2, saturation of peripheral oxygen; SABA, short-acting β-agonist; TGV, thoracic gas volume.
Intervention
Among the 22 eligible studies using macrolides as adjunctive therapy, azithromycin was the most commonly used macrolide in the included studies, comprising 13 trials.37,41–43,51–56,62–64 Five studies used clarithromycin.32,40,59–61 Two studies used troleandomycin.49,50 Two studies used erythromycin.57,58 The dose and duration of supplemented macrolides were in the following ranges: 5–12 mg/kg/day for 3–14 days and 30 mg/kg/week for 8 weeks, 5–15 mg/kg/day for 5 days to 4 weeks and 250 mg/day or 250 mg on alternate days for 2 weeks or 12 weeks with azithromycin, clarithromycin, and troleandomycin, respectively. Systemic steroids were prescribed concomitantly in school-aged children with underlying asthma in two trials49,50 and in preschool children with hospitalizations/ED visits in two trials,41,52 respectively. ICSs were used in most studies (6/7) in school-aged children with an asthma diagnosis and all trials (3/3) in preschool children with recurrent wheezing. For studies that enrolled toddlers (all <2 years of age) hospitalized for acute bronchiolitis, an ICS was not used in any of the studies (0/9), and concomitant non-macrolide antibiotics were used in the minority (3/9).
Outcome measurement
Meta-analysis investigating the long-term effects of macrolides and placebo among children with asthma, recurrent wheezing and bronchiolitis
Is macrolide treatment beneficial to the pulmonary function of children with asthma and recurrent wheezing?
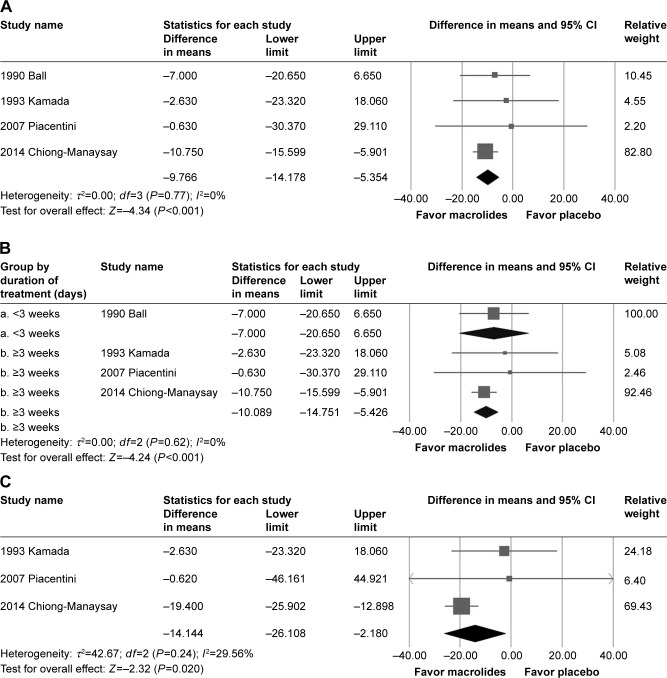
A total of four studies49,50,59,62 including 59 children and 3 studies50,59,62 including 49 children were enrolled for meta-analysis to determine the FEV1% and forced expiratory flow (FEF) 25%–75% after treatment. All the participants in the corresponding trials were children with asthma, and children in almost all (three of four) studies were aged more than 6 years. Two49,50 of the four studies enrolled children with severe, steroid-dependent asthma. The post-treatment FEV1% of children with asthma was significantly higher in the macrolide group than those in the placebo group (MD=−9.77, 95% CI=−14.18 to −5.35, P<0.001; I2=0%, τ=0.000) (Figure 2A). Although there was publication bias (t value=12.31, df=2, P=0.007), the results of the meta-analysis did not change (MD=−10.33, 95% CI=−14.60 to −6.06) after the trim and fill test (with two potentially missing studies to the left of the mean). The significance of the results became nonsignificant after deleting the study by Chiong et al59 who enrolled children with FEV1% <80% before treatment and used clarithromycin 15 mg/kg/day for 3 weeks (MD=−5.03, 95% CI=−15.67–5.61, P=0.354). In general, macrolides were seldom used for more than 2 weeks for the purpose of antimicrobial effects. In addition, we found that participants in the included studies (listed in Table 1) could be approximately grouped into two categories according to the duration of treatment: less than 3 weeks (12 articles) and more than 3 weeks (8 articles). Therefore, we tried to do subgroup analysis according to the duration of macrolides, although the heterogeneity was not significant. The results of subgroup meta-analysis of trials showed a significantly better treatment effect on FEV1% in children who took macrolides for more than 3 weeks (MD=−10.09, 95% CI=−14.75 to −5.43, P<0.001; I2=0%) (Figure 2B). Meanwhile, the post-treatment FEF 25%–75% of children with asthma in the macrolide group was also better than those in the placebo group (MD=−14.14, 95% CI=−26.11 to −2.18, P=0.02; I2=29.563%, τ=6.532) (Figure 2C). There was no significant publication bias (t value=0.086, df=1, P=0.945). The result became nonsignificant by removing the studies by Piacentini et al (MD=−14.01, 95% CI=−29.36 to 1.34, P=0.074)62 or Chiong et al (MD=−2.29, 95% CI=−21.12 to 16.55, P=0.812).59
Figure 2.
(A) Forest plot of the decreased forced expiratory volume percentage (FEV1%) between the macrolides group and the placebo group. (B) Forest plot of subgroup analysis of FEV1% by the duration of macrolides. (C) Forest plot of the decreased forced expiratory flow (FEF) 25%–75% between the macrolides group and the placebo group.
Does macrolide therapy decrease the need for rescue SABA usage?
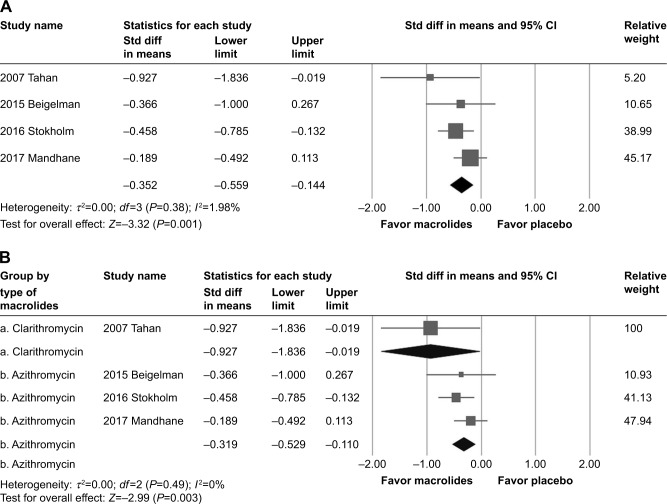
In the four RCTs37,41,43,60 including 430 participants, macrolides were associated with significantly fewer SABA usage days throughout the follow-up periods (SMD=−0.34, 95% CI=−0.59 to −0.09, P=0.007) (Figure 3A). There was neither significant heterogeneity (Q value=4.112, df=3, P=0.250, I2=27.047%, τ=0.133) nor publication bias (t value=1.526, df=2, P=0.266). However, after removing data from the study by Stokholm et al,43 which used azithromycin 10 mg/kg/day for 3 days in children aged 1–3 years, the results showed no significant difference between the macrolides and placebo group (SMD=−0.30, 95% CI=−0.66 to 0.06, P=0.098). The included studies were composed of preschool children hospitalized for bronchiolitis or who presented to the ED with wheezing.
Figure 3.
(A) Forest plot of the SABA usage days between the macrolides group and the placebo group. (B) Forest plot of subgroup analysis of SABA usage days by the type of macrolides.
Abbreviations: SABA, short-acting β2-agonist; std diff, standardized difference.
It was possible to perform subgroup analysis by dividing the four trials into two groups according to the type of macrolides. Azithromycin (n=356) was used in three RCTs. The results showed significantly less SABA usage days in children with bronchiolitis using macrolides (SMD=−0.32, 95% CI=−0.53 to −0.11, P=0.003, I2=0.000%) (Figure 3B). However, there were insufficient data for studies using non-azithromycin macrolides since only one study used clarithromycin.
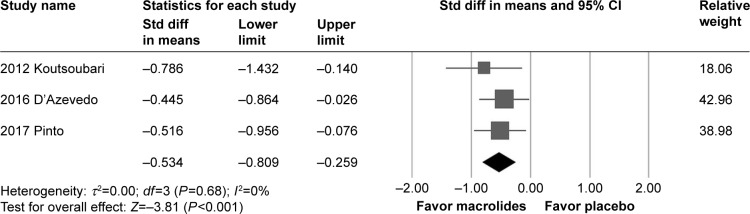
Does macrolide treatment lower the risk of recurrent wheezing?
For the risk of recurrent wheezing, 115 participants in the macrolides group showed significantly less recurrent wheezing (SMD=−0.53, 95% CI=−0.81 to −0.26, P<0.001, I2=0%, τ=0.000) (Figure 4) than the 99 patients in the placebo group among the selected three studies.53,54,61 There was no significant publication bias (t value=6.522, df=1, P=0.097). The enrolled children in the three studies were composed of school-aged children with intermittent mild to persistent asthma61 and toddlers less than 1-year-old hospitalized for acute bronchiolitis and the follow-up time were 3 months in two studies and 6 months in one study.53,54
Figure 4.
Forest plot of the recurrent wheezing risks between the macrolides group and the placebo group.
Abbreviation: Std diff, standardized difference.
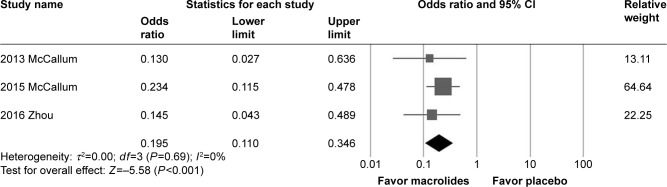
Does macrolide therapy alter the upper airway bacteria?
In three studies55,56,64 including 325 children less than 2 years of age hospitalized for bronchiolitis, patients in the macrolides group showed significantly less Moraxella catarrhalis by nasal swab (OR=0.19, 95% CI=0.11–0.35, P<0.001) (Figure 5). There was neither significant heterogeneity (Q value=0.731, I2=0%, P=0.694, τ=0.000) nor publication bias (t value=4.660, df=1, P=0.134). The significance was not changed after removing any single study.
Figure 5.
Forest plot of the nasal swab Moraxella catarrhalis between the macrolides group and the placebo group.
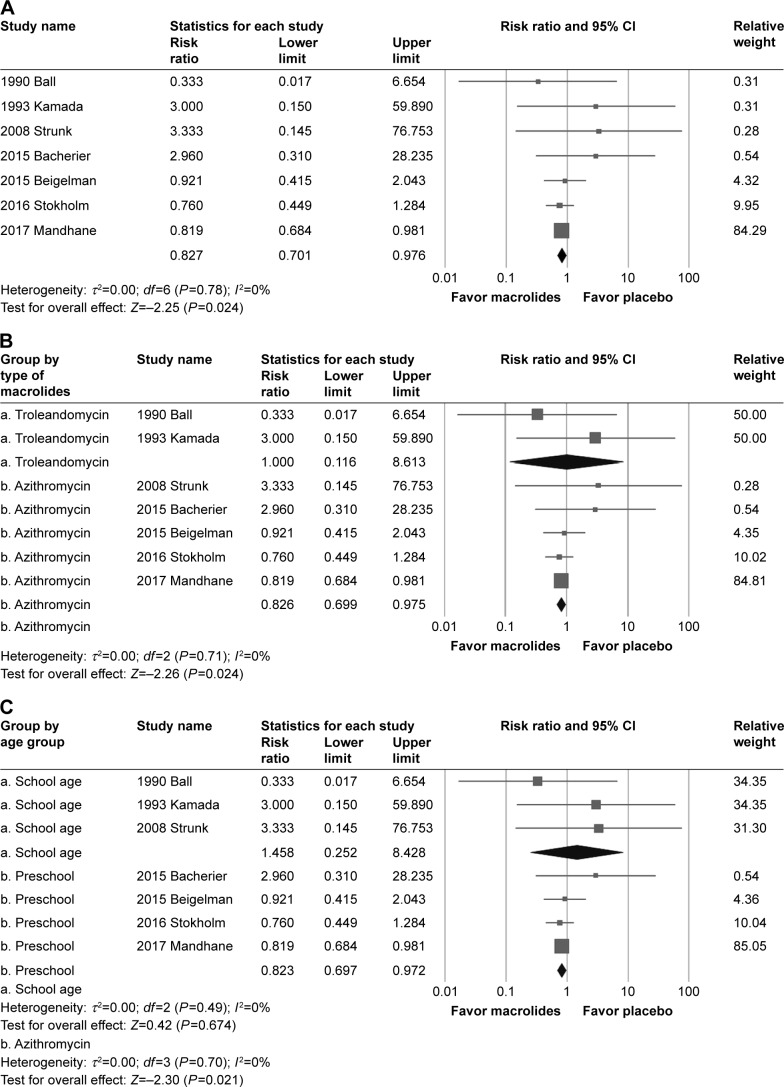
Adverse events
Compared with the placebo, participants in the macrolides group were associated with a lower risk to develop any adverse events (risk ratio=0.83, 95% CI=0.70–0.98, P=0.024, I 2=0%, τ=0.000, RCTs=7) (Figure 6A). There was no significant publication bias (t value=1.525, df=5, P=0.188). After removing the study by Mandhane et al,41 the results showed no significant difference between the macrolides and placebo groups (risk ratio=0.87, 95% CI=0.57–1.32, P=0.517). Most of the reported adverse events were related to gastrointestinal upset, such as nausea, vomiting, and abdominal pain. However, there were no enough data to do subgroup analysis according to the category of adverse events. It was possible to perform subgroup analysis according to the type of macrolides and the age of participants. The results showed that participants taking azithromycin (risk ratio=0.83, 95% CI=0.70–0.98, P=0.024, RCTs=5) but not troleandomycin (risk ratio=1.00, 95% CI=0.12–8.61, P=1.000) had lower risk of adverse effects (Figure 6B). Preschool children also had a lower risk of developing any adverse events (risk ratio=0.82, 95% CI=0.70–0.97, P=0.021, RCTs=4) but school-aged children did not (risk ratio=1.458, 95% CI=0.252–8.428, P=0.674) (Figure 6C).
Figure 6.
(A) Forest plot of the adverse events risks between the macrolides group and the placebo group. (B) Subgroup analysis of the adverse events risks by the type of macrolides. (C) Subgroup analysis of the adverse events risks by the age group.
Meta-regression
To examine the heterogeneity of the present analysis, we performed a meta-regression analysis using the male sex ratio and the duration of macrolides as moderators in the single meta-regression. We found that the effect of macrolides on the adverse events was not significantly confounded by the male sex ratio (slope=−0.549, P=0.183) (Figure S1) and the duration of macrolides (slope=0.021, P=0.326) (Figure S2).
Discussion
The current meta-analysis summarizes the effects of macrolides in children; six RCTs suggested that the supplementation with macrolides improves both the FEV1% and the FEF 25% with a mean difference of 10.43% and 19.41%, respectively. Moreover, pooled results from four trials showed that participants taking macrolides had fewer days of rescue SABA usage and three studies found that macrolides lowered the risks of recurrent wheezing. Furthermore, macrolides decreased the growth of M. catarrhalis in the upper airway. Finally, compared with participants who were taking placebos, those who were taking macrolide therapy had fewer adverse events.
To the best of our knowledge, this is the first meta-analysis to comprehensively investigate the efficacy of macrolides on childhood RAD including asthmatic and asthma-like diseases, such as recurrent wheezing and acute bronchiolitis. Our analysis included both school-aged children with more definitive asthma diagnoses and preschool children with concerning respiratory problems mimicking or preceding asthma. Compared with the two recent meta-analyses38,65 that enrolled studies on both adult and childhood asthma and focused on the effectiveness of macrolides on chronic asthma control and acute exacerbations, our study supplied more information on the analysis of treatment efficacy not only on the usefulness of pulmonary function tests, subsequent SABA usage, recurrent wheezing, but also the pathogenic bacteria status and the adverse drug reactions. The stricter inclusion criteria (only RCTs in the meta-analysis), the more recent search, and the concentrated age group (only children less than 18 years of age) ensured that the current meta-analysis is more up-to-date than the previous studies.
Our results are consistent with previous reports with regard to the effects of macrolides in the improvement of FEV1% in patients with asthma.38 Nevertheless, the analysis of FEV1% in Kew et al only enrolled one study recruiting adolescents in the pooled nine trials. In the current analysis, we pooled four trials and further found that macrolides improve pulmonary functions in both the large and small airways in school-aged children. However, the optimal dose and duration of macrolide treatment needed to offer a potential positive effect have not yet been established.37 Among the included studies in Kew et al, subgroup analysis according to the duration of macrolides was not done. In the current study, we found that those who use macrolides for more than 3 weeks had an increase in FEV1% from such treatment (Figure 2B). Although the evidence is limited considering the scanty numbers of included studies in current analysis, it is worth noted that the positive effects of macrolides in lung function in Kew et al may related to the prolonged duration (ranged from 4 to 52 weeks), which were far more than the general treatment. The effectiveness of prolonged macrolides treatment may be contributed to the antimicrobial effects rather than anti-inflammatory effects, which was shown in adult asthma studies.34,35 In addition, either incident M. pneumoniae or recurrent/chronic C. pneumoniae infection was thought to be related to newly-onset asthma and asthma exacerbation, even in non-atopic patients.15,66 Moreover, azithromycin taken daily for 1 year also benefit adult with COPD67 but had no benefits for adult with asthma who had only 3 days of treatment.68 Therefore, it seems that an extended treatment of macrolides could indeed lower the carrier status of C. pneumoniae/M. pneumoniae and help to improve the pulmonary functions. Even though macrolides are characterized by their broad spectrum of activity against common community-acquired respiratory pathogens and are widely used as first-line therapy, drug resistance has emerged with some common respiratory pathogens, such as Streptococcus pneumoniae.69 Moreover, previous studies70 determined that preschool wheezing is associated with pulmonary bacterial infection such as Haemophilus influenzae, S. pneumoniae, and M. catarrhalis, and patients received significant benefits from various classes of antibiotic therapy, including amoxicillin, amoxicillin/clavulanic acid, cefuroxime, and trimethoprim– sulfamethoxazole. The duration of these antibiotics varied, ranging from 2 to 16 weeks. Therefore, macrolides alone may not be enough to eradicate other respiratory pathogenic bacteria, which may also interfere the respiratory disease outcome. For those who take azithromycin, further studies are needed to make precise recommendations regarding the optimal duration, most appropriate, and safe macrolides to improve pulmonary functions in children with asthma.
As with the former meta-analysis65 that pooled two studies from children and adults for each and concluded that macrolide users had longer symptom-free days, our study demonstrated less SABA usage in the macrolides group. The subgroup analyses showed that children hospitalized for bronchiolitis received more benefits from macrolide therapy, especially in those who took azithromycin. Both participants infected by RSV and non-RSV showed better responses than those taking placebos (data not shown). In contrast to the previous meta-analysis that failed to demonstrate the advantage of macrolides for an exacerbation, current analysis revealed a lower risk of recurrent wheezing among children. Animal models71 had shown that azithromycin attenuated viral-dependent neutrophilic airway inflammation and was associated with decreased concentrations of BAL inflammatory mediators, such as IL-8 and granulocyte-macrophage colony-stimulating factor. In preschool children with recurrent wheezing, the cell profile from BAL also revealed neutrophil-mediated, but not eosinophil-mediated inflammation in the airway, which is often the situation in asthmatic adults.70,72 Therefore, the anti-neutrophilic properties of macrolides may serve as the mechanistic rationale for the prevention of recurrent wheezing. Furthermore, IL-8 is the main and potent neutrophilic activator and is characteristically elevated, especially during viral bronchiolitis, such as RSV infection.37 It may explain the better response to macrolides among those patients with bronchiolitis on the lower recurrent wheezing risk in our analysis. Moreover, Kloepfer et al73 had shown that co-detection of viruses with upper airway polysaccharide bacteria in children was associated with an increased risk of asthma exacerbation. The decreased carriage status of M. catarrhalis after macrolide treatment in our analysis (Figure 5) further strengthened this theory. Finally, the concentration of azithromycin in alveolar macrophage and BAL is 100-fold more than that in serum, and, together with their intracellular aggregated feature, results in a long half-life.74 The long-lasting effects may also be the reason for the improvement of long-term efficacy such as pulmonary function, less rescue medication usage, and lower risks of recurrent wheezing.
Nevertheless, there were insufficient data to be pooled to find the relationship between macrolides and residential bacteria other than M. catarrhalis in the airway. Further well-designed, placebo-controlled studies are required to clarify the influences of residential and pathogenic airway pathogens on the effect of macrolide therapy.
It is safe to take macrolides as the adjunctive therapy to treat childhood reactive disease in current analysis, especially for those who take azithromycin (Figure 6B). The safety of azithromycin had also been approved in adults who were treated with a longer duration for other disease ranged from 3 to 12 months in previous studies.75,76
Limitations
There are several limitations of this study. First, we could not perform the subgroup analysis because of the lack of studies, such as those regarding steroid dose reduction, time to respiratory symptoms relief, nasal IL-8, and concomitant medications, thereby limiting the strength of our analysis. Second, because of limited numbers of included trials, it was not possible to perform more meaningful meta-regressions to examine the impact of variables that may affect the heterogeneity of some constructed results in the current study. Third, some of the included trials had a small sample size and could not provide details on the randomization processes. Fourth, the following time in each study varied and may thus limit the usability in some results. Fifth, some reported results in current analysis were driven by one study41,59,62 within the analysis and may need more validation studies to make a stronger conclusion. Finally, we could not discover the precise pathophysiology behind our findings because of the basic limitation of the meta-analysis.
Conclusion
The present meta-analysis adds new evidence to the current knowledge about macrolides treating childhood RAD such as asthma, recurrent wheezing, and bronchiolitis. First, using macrolides as adjunctive therapy can improve pulmonary functions in both large and small airways in school-aged children. In addition, azithromycin treatment can decrease the need for rescue SABA usage among preschool children with recurrent wheezing or bronchiolitis. Furthermore, the recurrent wheezing risks and upper airway M. catarrhalis growth could be lowered by macrolide supplementation in children with a history of wheezing. Finally, macrolide therapy exhibits fewer risks of adverse events, especially for preschool children and those who use azithromycin. Additional large RCTs focusing on the optimal dose, biochemical features behind the wheezing phenotype, the role of the colonization airway pathogens, and head-to-head comparison of different macrolides’ efficacy and mechanism are required to validate these findings.
Supplementary materials
Meta-regression scatter plot showing there was no correlation between adverse events risk and male sex ratio.
Meta-regression scatter plot showing there was no correlation between adverse events risk and the duration of macrolides.
Table S1.
PRISMA-P checklist
| Section/topic | ≥ | Checklist item | Reported on page ≥ |
|---|---|---|---|
| Title | |||
| Title | 1 | Identify the report as a systematic review, meta-analysis, or both. | 1 |
| Abstract | |||
| Structured summary | 2 | Provide a structured summary including, as applicable: background; objectives; data sources; study eligibility criteria, participants, and interventions; study appraisal and synthesis methods; results; limitations; conclusions and implications of key findings; systematic review registration number. | 1 abstract |
| Introduction | |||
| Rationale | 3 | Describe the rationale for the review in the context of what is already known. | 2, 3 |
| Objectives | 4 | Provide an explicit statement of questions being addressed with reference to participants, interventions, comparisons, outcomes, and study design (PICOS). | 3 |
| Methods | |||
| Protocol and registration | 5 | Indicate if a review protocol exists, if and where it can be accessed (eg, web address), and, if available, provide registration information including registration number. | 3 |
| Eligibility criteria | 6 | Specify study characteristics (eg, PICOS, length of follow-up) and report characteristics (eg, years considered, language, publication status) used as criteria for eligibility, giving rationale. | 3 |
| Information sources | 7 | Describe all information sources (eg, databases with dates of coverage, contact with study authors to identify additional studies) in the search and date last searched. | 3 |
| Search | 8 | Present full electronic search strategy for at least one database, including any limits used, such that it could be repeated. | 3, Table S2 |
| Study selection | 9 | State the process for selecting studies (ie, screening, eligibility, included in systematic review, and, if applicable, included in the meta-analysis). | 3, 4 |
| Data collection process | 10 | Describe method of data extraction from reports (eg, piloted forms, independently, in duplicate) and any processes for obtaining and confirming data from investigators. | 3, 4 |
| Data items | 11 | List and define all variables for which data were sought (eg, PICOS, funding sources) and any assumptions and simplifications made. | 5–9 |
| Risk of bias in individual studies | 12 | Describe methods used for assessing risk of bias of individual studies (including specification of whether this was done at the study or outcome level), and how this information is to be used in any data synthesis. | 3, Table S3 |
| Summary measures | 13 | State the principal summary measures (eg, risk ratio, difference in means). | 3 |
| Synthesis of results | 14 | Describe the methods of handling data and combining results of studies, if done, including measures of consistency (eg, I2) for each meta-analysis. | 3 |
| Risk of bias across studies | 15 | Specify any assessment of risk of bias that may affect the cumulative evidence (eg, publication bias, selective reporting within studies). | 3, Table S3 |
| Additional analyses | 16 | Describe methods of additional analyses (eg, sensitivity or subgroup analyses, meta-regression), if done, indicating which were pre-specified. | 3 |
| Results | |||
| Study selection | 17 | Give numbers of studies screened, assessed for eligibility, and included in the review, with reasons for exclusions at each stage, ideally with a flow diagram. | 3, 4, Fig 1 |
| Study characteristics | 18 | For each study, present characteristics for which data were extracted (eg, study size, PICOS, follow-up period) and provide the citations. | 6–9, Table 1 |
| Risk of bias within studies | 19 | Present data on risk of bias of each study and, if available, any outcome level assessment (see Item 12). | 5, 8–10, Table S3 |
| Results of individual studies | 20 | For all outcomes considered (benefits or harms), present, for each study: (a) simple summary data for each intervention group (b) effect estimates and confidence intervals, ideally with a forest plot. | 6–11, Fig 2–6 |
| Synthesis of results | 21 | Present results of each meta-analysis done, including confidence intervals and measures of consistency. | 6–11, Fig 2–6 |
| Risk of bias across studies | 22 | Present results of any assessment of risk of bias across studies (see Item 15). | 6–11 |
| Additional analysis | 23 | Give results of additional analyses, if done (eg, sensitivity or subgroup analyses, meta-regression [see Item 16]). | 6–11, Fig 2, Fig 3, Fig 6 |
| Discussion | |||
| Summary of evidence | 24 | Summarize the main findings including the strength of evidence for each main outcome; consider their relevance to key groups (eg, healthcare providers, users, and policy makers). | 11–12 |
| Limitations | 25 | Discuss limitations at study and outcome level (eg, risk of bias), and at review-level (eg, incomplete retrieval of identified research, reporting bias). | 14 |
| Conclusions | 26 | Provide a general interpretation of the results in the context of other evidence, and implications for future research. | 14 |
| Funding | |||
| Funding | 27 | Describe sources of funding for the systematic review and other support (eg, supply of data); role of funders for the systematic review. | 15 |
Note: © 2009 Moher et al.23 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abbreviation: PRISMA-P, Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols.
Table S2.
Searching strategy
| PubMed |
|---|
| ((((((((((Asthma OR asthma*))) OR infantile asthma) OR chronic cough) OR ((Bronchitis, Chronic OR chronic bronchitis))) OR ((Respiratory Sounds OR wheezing OR wheez*))) OR (Bronchiolitis OR Bronchiolitides OR acute bronchiolitis)) OR (Bronchiolitis, Viral OR Viral Bronchiolitides))) in All Fields |
| AND |
| ((((((Erythromycin OR T-Stat OR Erycette OR Erymax OR Ilotycin))) OR ((Clarithromycin OR TE-031 OR A-56268 OR Biaxin))) OR macrolide) OR ((Azithromycin OR Azythromycin OR Sumamed OR Toraseptol OR Vinzam OR CP-62993 OR CP 62993 OR CP62993 OR Zithromax OR Azitrocin OR Azadose OR Ultreon OR Zitromax OR Goxal OR Zentavion))) in All Fields |
| Filters: Child: birth-18 years |
| Embase |
| (‘asthma’ OR ‘asthma’/exp OR asthma OR asthma*) OR (‘chronic bronchitis’/exp) OR (‘abnormal respiratory sound’/exp) OR (infantile NEAR/3 asthma) OR (chronic NEAR/3 cough) OR (chronic NEAR/3 bronchitis) OR (‘wheezing’/exp OR wheezing OR wheez*) OR (‘bronchiolitis’/exp) OR (‘viral bronchiolitis’/exp) OR ((viral AND bronchiolitides OR bronchiolitis OR bronchiolitides OR acute) AND bronchiolitis) OR ((viral NEAR/3 bronchiolitides) OR bronchiolitis OR bronchiolitides OR (acute NEAR/3 bronchiolitis)) |
| AND |
| (‘erythromycin’/exp OR erythromycin OR ‘t stat’/exp OR ‘t stat’ OR ‘erycette’/exp OR erycette OR ‘erymax’/exp) OR ((‘azithromycin’/exp OR azithromycin OR ‘azythromycin’/exp OR azythromycin OR ‘sumamed’/exp OR sumamed OR toraseptol OR ‘vinzam’/exp OR vinzam OR ‘cp 62993′/exp OR ‘cp 62993′ OR cp) AND 62993 OR ‘cp62993′/exp OR cp62993 OR ‘zithromax’/exp OR zithromax OR ‘azitrocin’/exp OR azitrocin OR ‘azadose’/exp OR azadose OR ‘ultreon’/exp OR ultreon OR ‘zitromax’/exp OR zitromax OR goxal OR zentavion) OR (‘clarithromycin’/exp OR clarithromycin OR ‘te 031′/exp OR ‘te 031′ OR ‘a 56268′/exp OR ‘a 56268′ OR ‘biaxin’/exp OR biaxin) OR (‘macrolides’/exp OR macrolides OR ‘macrolide’/exp OR macrolide) |
| AND |
| ([adolescent]/lim OR [child]/lim OR [infant]/lim OR [newborn]/lim OR [preschool]/lim OR [school]/lim) |
| Cochrane |
| (MeSH descriptor: [Asthma] explode all trees) OR (MeSH descriptor: [Bronchitis, Chronic] explode all trees) OR (MeSH descriptor: [Respiratory Sounds] explode all trees) OR (MeSH descriptor: [Bronchiolitis] explode all trees) OR (MeSH descriptor: [Bronchiolitis, Viral] explode all trees) OR (Asthma or asthma* or infantile asthma or chronic cough or chronic bronchitis or Respiratory Sounds or wheezing or wheez*:ti,ab,kw (Word variations have been searched)) OR (Bronchiolitis or Bronchiolitides or acute bronchiolitis or Viral Bronchiolitides:ti,ab,kw (Word variations have been searched)) |
| AND |
| (MeSH descriptor: [Erythromycin] explode all trees) OR (MeSH descriptor: [Azithromycin] explode all trees) OR (MeSH descriptor: [Clarithromycin] explode all trees) OR (MeSH descriptor: [Macrolides] explode all trees) OR (Erythromycin or T-Stat or Erycette or Erymax or Ilotycin:ti,ab,kw (Word variations have been searched)) OR (Azithromycin or Azythromycin or Sumamed or Toraseptol or Vinzam or CP-62993 or CP 62993 or CP62993 or Zithromax or Azitrocin or Azadose or Ultreon or Zitromax or Goxal or Zentavion:ti,ab,kw (Word variations have been searched)) OR (Clarithromycin or TE-031 or A-56268 or Biaxin:ti,ab,kw (Word variations have been searched)) OR (macrolides or macrolide*:ti,ab,kw (Word variations have been searched)) |
| CINAHL |
| (MH “Asthma+”) OR (“chronic cough”) OR (infantile asthma) OR (MH “Bronchitis, Chronic”) OR (MH “Respiratory Sounds”) OR (MH “Bronchiolitis”) OR (asthma* OR infantile asthma OR chronic cough OR chronic bronchitis OR Respiratory Sounds OR wheezing OR wheez* OR Bronchiolitis OR Bronchiolitides OR acute bronchiolitis OR viral bronchiolitis OR Viral Bronchiolitides) |
| AND |
| ((MH “Erythromycin”) OR “Erythromycin”) OR (T-Stat OR Erycette OR Erymax OR Ilotycin) OR ((MH “Clarithromycin”) OR “Clarithromycin”) OR (TE-031 OR A-56268 OR Biaxin) OR ((MH “Antibiotics, Macrolide”) OR “macrolide”) OR ((MH “Azithromycin”) OR “Azithromycin”) OR (Sumamed OR Toraseptol OR Vinzam OR CP-62993 OR CP 62993 OR CP62993 OR Zithromax OR Azitrocin OR Azadose OR Ultreon OR Zitromax OR Goxal OR Zentavion) |
| Narrow by Subject Age: all child |
Abbreviation: CINAHL, Cumulative Index to Nursing and Allied Health.
Table S3.
Risk of bias assessment of each included studya
| Study validity domains | Sequence generation | Allocation concealment | Blinding of participants and personnel | Blinding of outcome assessment | Incomplete outcome data | Selective outcome reporting | Other sources of bias |
|---|---|---|---|---|---|---|---|
| Probiotics | |||||||
| Ball et al,1 1990 | Unclear | Unclear | Low | Low | Low | Unclear | Low |
| Kamada et al,2 1993 | Low | Low | Low | Low | Low | Unclear | Unclear |
| Fonseca-Aten et al,3 2006 | Unclear | Unclear | Unclear | Unclear | High | Low | Unclear |
| Piacentini et al,4 2007 | Low | Unclear | Low | Low | Unclear | Low | Unclear |
| Tahan et al,5 2007 | Low | Unclear | Low | Low | Low | Low | Unclear |
| Rasul et al,6 2008 | Low | Low | Low | Low | High | Low | Unclear |
| Strunk et al,7 2008 | Unclear | Unclear | Unclear | Unclear | Low | Low | Unclear |
| Kabir et al,8 2009 | Low | Unclear | Unclear | Unclear | Low | Low | Unclear |
| Koutsoubari et al,9 2012 | Low | High | High | High | Low | Low | Unclear |
| Pinto et al,10 2012 | Low | Unclear | Unclear | Unclear | Low | Low | Unclear |
| Mccallum et al,11 2013 | Low | Low | Low | Low | Low | Low | Unclear |
| Chiong-Manaysay and Andaya,12 2014 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear |
| Bacharier et al,13 2015 | Low | Low | Low | Low | Low | Low | Unclear |
| Beigelman et al, 14 2015 (letter) | Low | Low | Low | Low | Low | Low | Unclear |
| Beigelman et al,15 2015 | Low | Low | Low | Low | Low | Low | Low |
| Mccallum et al,16 2015 | Low | Low | Low | Low | Low | Low | Low |
| Silveira D’Azevedo et al,17 2016 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear |
| Stokholm et al,18 2016 | Low | Low | Low | Unclear | Low | Low | Low |
| Wan et al,19 2016 | Low | Low | Unclear | Unclear | Low | Low | Unclear |
| Zhou et al,20 2016 | Unclear | Unclear | Low | Low | Low | Low | Low |
| Mandhane et al,21 2017 | Low | Low | Low | Low | Unclear | Low | Low |
| Pinto et al,22 2017 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear |
Notes:
Each domain has been evaluated as being “High”, “Low”, or “Unclear” regarding the risk of bias following the guidelines of Cochrane. Collaboration’s tool for assessing risk of bias, the thorough and original evaluation form is attached in the following pages. “Low” in all Domains would place a study at “Low Risk of Bias”; “High” in any of the Domains would place a study at “High Risk of Bias”; “Unclear” in any of the domains would place the study at “Unclear Risk of Bias”.
References
- 1.Ball BD, Hill MR, Brennor M, Sanks R, Szefler SJ. Effect of low-dose troleandomycin on glucocorticoid pharmacokinetics and airway hyperresponsiveness in severely asthmatic children. Ann Allergy. 1990;65(1):37–45. [PubMed] [Google Scholar]
- 2.Kamada AK, Hill MR, Iklé DN, Brenner AM, Szefler SJ. Efficacy and safety of low-dose troleandomycin therapy in children with severe, steroid-requiring asthma. J Allergy Clin Immunol. 1993;91(4):873–882. doi: 10.1016/0091-6749(93)90345-g. [DOI] [PubMed] [Google Scholar]
- 3.Fonseca-Aten M, Okada PJ, Bowlware KL, et al. Effect of clarithromycin on cytokines and chemokines in children with an acute exacerbation of recurrent wheezing: a double-blind, randomized, placebo-controlled trial. Ann Allergy Asthma Immunol. 2006;97(4):457–463. doi: 10.1016/S1081-1206(10)60935-0. [DOI] [PubMed] [Google Scholar]
- 4.Piacentini GL, Peroni DG, Bodini A, et al. Azithromycin reduces bronchial hyperresponsiveness and neutrophilic airway inflammation in asthmatic children: a preliminary report. Allergy Asthma Proc. 2007;28(2):194–198. doi: 10.2500/aap.2007.28.2958. [DOI] [PubMed] [Google Scholar]
- 5.Tahan F, Ozcan A, Koc N. Clarithromycin in the treatment of RSV bronchiolitis: a double-blind, randomised, placebo-controlled trial. Eur Respir J. 2007;29(1):91–97. doi: 10.1183/09031936.00029206. [DOI] [PubMed] [Google Scholar]
- 6.Rasul CH, Kabir A, Rashid A, Mahboob AA, Hassan MA. Role of antibiotic in the outcome of bronchiolitis. Pakistan J Med Sci. 2008;24(5):707–711. [Google Scholar]
- 7.Strunk RC, Bacharier LB, Phillips BR, et al. Azithromycin or montelukast as inhaled corticosteroid-sparing agents in moderate-to-severe childhood asthma study. J Allergy Clin Immunol. 2008;122(6):e1134:1138–1144. doi: 10.1016/j.jaci.2008.09.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kabir A, Mollah AH, Anwar KS, Rahman A, Amin R, Rahman ME. Management of bronchiolitis without antibiotics: a multicentre randomized control trial in Bangladesh. Acta Paediatrica Int J Paediatr. 2009;98(10):1593–1599. doi: 10.1111/j.1651-2227.2009.01389.x. [DOI] [PubMed] [Google Scholar]
- 9.Koutsoubari I, Papaevangelou V, Konstantinou GN, et al. Effect of clarithromycin on acute asthma exacerbations in children: an open randomized study. Pediatr Allergy Immunol. 2012;23(4):385–390. doi: 10.1111/j.1399-3038.2012.01280.x. [DOI] [PubMed] [Google Scholar]
- 10.Pinto LA, Pitrez PM, Luisi F, et al. Azithromycin therapy in hospitalized infants with acute bronchiolitis is not associated with better clinical outcomes: a randomized, double-blinded, and placebo-controlled clinical trial. J Pediatr. 2012;161(6):1104–1108. doi: 10.1016/j.jpeds.2012.05.053. [DOI] [PubMed] [Google Scholar]
- 11.Mccallum GB, Morris PS, Chatfield MD, et al. A single dose of azithromycin does not improve clinical outcomes of children hospitalised with bronchiolitis: a randomised, placebo-controlled trial. PLoS One. 2013;8(9):e74316. doi: 10.1371/journal.pone.0074316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chiong-Manaysay K, Andaya A. Effectiveness of Macrolide (Clarithromycin) treatment on pediatric patients with mild-moderate persistent asthma: a randomised controlled study. Allergy Eur J Allergy Clin Immunol. 2014;69:291. [Google Scholar]
- 13.Bacharier LB, Guilbert TW, Mauger DT, et al. Early administration of azithromycin and prevention of severe lower respiratory tract illnesses in preschool children with a history of such illnesses a randomized clinical trial. J Am Med Assoc. 2015;314(19):2034–2044. doi: 10.1001/jama.2015.13896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Beigelman A, Isaacson-Schmid M, Sajol G, et al. Randomized trial to evaluate azithromycin’s effects on serum and upper airway IL-8 levels and recurrent wheezing in infants with respiratory syncytial virus bronchiolitis. J Allergy Clin Immunol. 2015;1351178(5):1171. doi: 10.1016/j.jaci.2014.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Beigelman A, Bacharier LB, Baty J, et al. Does azithromycin modify viral load during severe respiratory syncytial virus bronchiolitis? J Allergy Clin Immunol. 2015;136(4):1129–1131. doi: 10.1016/j.jaci.2015.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mccallum GB, Morris PS, Grimwood K, et al. Three-weekly doses of azithromycin for indigenous infants hospitalized with bronchiolitis: a multicentre, randomized, placebo-controlled trial. Front Pediatr. 2015;3:32. doi: 10.3389/fped.2015.00032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Silveira D’Azevedo V, Roza CA, Luisi F, Pitrez PM, Stein RT, Pinto LA. Azithromycin therapy in infants with bronchiolitis reduces recurrent wheezing 3 months after hospitalization: a randomized, placebo-controlled trial. Pediatric Pulmonol. 2016;51:S9. [Google Scholar]
- 18.Stokholm J, Chawes BL, Vissing NH, et al. Azithromycin for episodes with asthma-like symptoms in young children aged 1–3 years: a randomised, double-blind, placebo-controlled trial. Lancet Respir Med. 2016;4(1):19–26. doi: 10.1016/S2213-2600(15)00500-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wan KS, Liu YC, Huang CS, Su YM, Ym S. Effects of low-dose clarithromycin added to fluticasone on inflammatory markers and pulmonary function among children with asthma: a randomized clinical trial. Allergy Rhinol. 2016;7(3):131–134. doi: 10.2500/ar.2016.7.0168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhou Y, Bacharier LB, Isaacson-Schmid M, et al. Azithromycin therapy during respiratory syncytial virus bronchiolitis: upper airway microbiome alterations and subsequent recurrent wheeze. J Allergy Clin Immunol. 2016;138(4):e1215:1215–1219. doi: 10.1016/j.jaci.2016.03.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mandhane PJ, Paredes Zambrano De Silbernagel P, Nwe Aung Y, et al. Treatment of preschool children presenting to the emergency department with wheeze with azithromycin: a placebo-controlled randomized trial. PLoS One. 2017;12(8):e0182411. doi: 10.1371/journal.pone.0182411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pinto LA, Jones MH, Pitrez PM, Stein RT. Azithromycin administered at the time of severe bronchiolitis has a protective effect on subsequent wheezing in infants. Pediatr Pulmonol. 2017;52:S165–S166. [Google Scholar]
- 23.Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: The PRISMA Statement. PLoS Med. 2009;6(6):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
Acknowledgments
We gratefully acknowledge the kind help of Ping-Tao Tseng in providing suggestions for statistics. The manuscript has been edited for grammar, language, and proofreading by Enago, the editing brand of Crimson Interactive Pvt., Ltd.
Footnotes
Author contributions
All authors contributed equally to this study and have read and approved the final manuscript. S-JL and W-TL conducted the search. W-TL and T-LY designed and conducted the study and analyzed the data, performed the validation of the results. W-TL wrote the paper. M-CT, H-HC, Y-JC, HHL, CYL, T-LY, and W-TL extracted the data. All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Akinbami LJ, Moorman JE, Bailey C. Trends in asthma prevalence, health care use, and mortality in the United States, 2001–2010. NCHS Data Brief. 2012;94:1–8. [PubMed] [Google Scholar]
- 2.Chang CF, Herrod HG, Steinberg SS. Prevalence and costs of acute and chronic potentially avoidable pediatric hospitalizations in Tennessee. Tenn Med. 2009;102(11):35–39. [PubMed] [Google Scholar]
- 3.Papadopoulos NG, Christodoulou I, Rohde G, et al. Viruses and bacteria in acute asthma exacerbations-a GA(2) LEN-DARE systematic review. Allergy. 2011;66(4):458–468. doi: 10.1111/j.1398-9995.2010.02505.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Np L, Gold DR, Weiss ST, Celedon JC. Recurrent wheeze in early childhood and asthma among children at risk for atopy. Pediatrics. 2006;117(6):e1132–e1138. doi: 10.1542/peds.2005-2271. [DOI] [PubMed] [Google Scholar]
- 5.Nath JB, Hsia RY. Children’s emergency department use for asthma, 2001–2010. Acad Pediatr. 2015;15(2):225–230. doi: 10.1016/j.acap.2014.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bush A. Practice imperfect–treatment for wheezing in preschoolers. N Engl J Med. 2009;360(4):409–410. doi: 10.1056/NEJMe0808951. [DOI] [PubMed] [Google Scholar]
- 7.Bisgaard H, Szefler S. Prevalence of asthma-like symptoms in young children. Pediatr Pulmonol. 2007;42(8):723–728. doi: 10.1002/ppul.20644. [DOI] [PubMed] [Google Scholar]
- 8.Singh AM, Moore PE, Gern JE, Lemanske RF, Hartert TV. Bronchiolitis to asthma: a review and call for studies of gene-virus interactions in asthma causation. Am J Respir Crit Care Med. 2007;175(2):108–119. doi: 10.1164/rccm.200603-435PP. [DOI] [PubMed] [Google Scholar]
- 9.Mckeever T, Mortimer K, Wilson A, et al. Quadrupling inhaled glucocorticoid dose to abort asthma exacerbations. N Engl J Med. 2018;378(10):902–910. doi: 10.1056/NEJMoa1714257. [DOI] [PubMed] [Google Scholar]
- 10.Jackson DJ, Bacharier LB, Mauger DT, et al. Quintupling inhaled glucocorticoids to prevent childhood asthma exacerbations. N Engl J Med. 2018;378(10):891–901. doi: 10.1056/NEJMoa1710988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ducharme FM, Tse SM, Chauhan B. Diagnosis, management, and prognosis of preschool wheeze. Lancet. 2014;383(9928):1593–1604. doi: 10.1016/S0140-6736(14)60615-2. [DOI] [PubMed] [Google Scholar]
- 12.Ralston SL, Lieberthal AS, Meissner HC, et al. Clinical practice guideline: the diagnosis, management, and prevention of bronchiolitis. Pediatrics. 2014;134(5):e1474–e1502. doi: 10.1542/peds.2014-2742. [DOI] [PubMed] [Google Scholar]
- 13.Holgate ST. Rhinoviruses in the pathogenesis of asthma: the bronchial epithelium as a major disease target. J Allergy Clin Immunol. 2006;118(3):587–590. doi: 10.1016/j.jaci.2006.06.023. [DOI] [PubMed] [Google Scholar]
- 14.Medina JL, Coalson JJ, Brooks EG, et al. Mycoplasma pneumoniae CARDS toxin induces pulmonary eosinophilic and lymphocytic inflammation. Am J Respir Cell Mol Biol. 2012;46(6):815–822. doi: 10.1165/rcmb.2011-0135OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cunningham AF, Johnston SL, Julious SA, Lampe FC, Ward ME. Chronic Chlamydia pneumoniae infection and asthma exacerbations in children. Eur Respir J. 1998;11(2):345–349. doi: 10.1183/09031936.98.11020345. [DOI] [PubMed] [Google Scholar]
- 16.Lemanske RF, Jackson DJ, Gangnon RE, et al. Rhinovirus illnesses during infancy predict subsequent childhood wheezing. J Allergy Clin Immunol. 2005;116(3):571–577. doi: 10.1016/j.jaci.2005.06.024. [DOI] [PubMed] [Google Scholar]
- 17.Schmidt SM, Muller CE, Bruns R, Wiersbitzky SK. Bronchial Chlamydia pneumoniae infection, markers of allergic inflammation and lung function in children. Pediatr Allergy Immunol. 2001;12(5):257–265. doi: 10.1034/j.1399-3038.2001.00042.x. [DOI] [PubMed] [Google Scholar]
- 18.Schmidt SM, Muller CE, Gurtler L, et al. Chlamydia pneumoniae respiratory tract infection aggravates therapy refractory bronchitis or pneumonia in childhood. Klinische Padiatrie. 2005;217(1):9–14. doi: 10.1055/s-2004-818791. [DOI] [PubMed] [Google Scholar]
- 19.Webley WC, Salva PS, Andrzejewski C, et al. The bronchial lavage of pediatric patients with asthma contains infectious Chlamydia. Am J Respir Crit Care Med. 2005;171(10):1083–1088. doi: 10.1164/rccm.200407-917OC. [DOI] [PubMed] [Google Scholar]
- 20.Webley WC, Tilahun Y, Lay K, et al. Occurrence of Chlamydia trachomatis and Chlamydia pneumoniae in paediatric respiratory infections. Eur Respir J. 2009;33(2):360–367. doi: 10.1183/09031936.00019508. [DOI] [PubMed] [Google Scholar]
- 21.Esposito S, Blasi F, Arosio C, et al. Importance of acute Chlamydia pneumoniae and Chlamydia pneumoniae infections in children with wheezing. Eur Respir J. 2000;16(6):1142–1146. doi: 10.1034/j.1399-3003.2000.16f21.x. [DOI] [PubMed] [Google Scholar]
- 22.Nagy A, Kozma GT, Keszei M, Treszl A, Falus A, Szalai C. The development of asthma in children infected with Chlamydia pneumoniae is dependent on the modifying effect of mannose-binding lectin. J Allergy Clin Immunol. 2003;112(4):729–734. doi: 10.1016/s0091-6749(03)02010-4. [DOI] [PubMed] [Google Scholar]
- 23.Zirakishvili D, Chkhaidze I, Barnabishvili N. Mycoplasma pneumoniae and Chlamydia pneumoniae in hospitalized children with bronchiolitis. Georgian Med News. 2015;240(240):73–78. [PubMed] [Google Scholar]
- 24.Duenas Meza E, Jaramillo CA, Correa E, et al. Virus and Mycoplasma pneumoniae prevalence in a selected pediatric population with acute asthma exacerbation. J Asthma. 2016;53(3):253–260. doi: 10.3109/02770903.2015.1075548. [DOI] [PubMed] [Google Scholar]
- 25.Martin RJ, Kraft M, Chu HW, Berns EA, Cassell GH. A link between chronic asthma and chronic infection. J Allergy Clin Immunol. 2001;107(4):595–601. doi: 10.1067/mai.2001.113563. [DOI] [PubMed] [Google Scholar]
- 26.Kraft M, Cassell GH, Pak J, Martin RJ. Mycoplasma pneumoniae and Chlamydia pneumoniae in asthma: effect of clarithromycin. Chest. 2002;121(6):1782–1788. doi: 10.1378/chest.121.6.1782. [DOI] [PubMed] [Google Scholar]
- 27.Kannan TR, Baseman JB. ADP-ribosylating and vacuolating cytotoxin of Mycoplasma pneumoniae represents unique virulence determinant among bacterial pathogens. Proc Natl Acad Sci U S A. 2006;103(17):6724–6729. doi: 10.1073/pnas.0510644103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wood PR, Hill VL, Burks ML, et al. Mycoplasma pneumoniae in children with acute and refractory asthma. Ann Allergy Asthma Immunol. 2013;110(5):e321:328–334. doi: 10.1016/j.anai.2013.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bisgaard H, Hermansen MN, Buchvald F, et al. Childhood asthma after bacterial colonization of the airway in neonates. N Engl J Med. 2007;357(15):1487–1495. doi: 10.1056/NEJMoa052632. [DOI] [PubMed] [Google Scholar]
- 30.Rubin BK, Henke MO. Immunomodulatory activity and effectiveness of macrolides in chronic airway disease. Chest. 2004;125(2 Suppl):70s–78s. doi: 10.1378/chest.125.2_suppl.70s. [DOI] [PubMed] [Google Scholar]
- 31.Amsden GW. Anti-inflammatory effects of macrolides – an underappreciated benefit in the treatment of community-acquired respiratory tract infections and chronic inflammatory pulmonary conditions? J Antimicrob Chemother. 2005;55(1):10–21. doi: 10.1093/jac/dkh519. [DOI] [PubMed] [Google Scholar]
- 32.Fonseca-Aten M, Okada PJ, Bowlware KL, et al. Effect of clarithromycin on cytokines and chemokines in children with an acute exacerbation of recurrent wheezing: a double-blind, randomized, placebo-controlled trial. Ann Allergy Asthma Immunol. 2006;97(4):457–463. doi: 10.1016/S1081-1206(10)60935-0. [DOI] [PubMed] [Google Scholar]
- 33.Gotfried MH. Macrolides for the treatment of chronic sinusitis, asthma, and COPD. Chest. 2004;125(2 Suppl):52S–60S. doi: 10.1378/chest.125.2_suppl.52s. [DOI] [PubMed] [Google Scholar]
- 34.Hahn DL, Plane MB, Mahdi OS, Byrne GI. Secondary outcomes of a pilot randomized trial of azithromycin treatment for asthma. PLoS Clin Trials. 2006;1(2):e11. doi: 10.1371/journal.pctr.0010011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hahn DL, Grasmick M, Hetzel S, Yale S, AZMATICS (AZithroMycin-Asthma Trial In Community Settings) Study Group Azithromycin for bronchial asthma in adults: an effectiveness trial. J Am Board Fam Med. 2012;25(4):442–459. doi: 10.3122/jabfm.2012.04.110309. [DOI] [PubMed] [Google Scholar]
- 36.Johnston SL, Blasi F, Black PN, et al. The effect of telithromycin in acute exacerbations of asthma. N Engl J Med. 2006;354(15):1589–1600. doi: 10.1056/NEJMoa044080. [DOI] [PubMed] [Google Scholar]
- 37.Beigelman A, Isaacson-Schmid M, Sajol G, et al. Randomized trial to evaluate azithromycin’s effects on serum and upper airway IL-8 levels and recurrent wheezing in infants with respiratory syncytial virus bronchiolitis. J Allergy Clin Immunol. 2015;1351178(5):1171. doi: 10.1016/j.jaci.2014.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kew KM, Undela K, Kotortsi I, Ferrara G. Macrolides for chronic asthma. Cochrane Database Syst Rev. 2015;9(9):Cd002997. doi: 10.1002/14651858.CD002997.pub4. [DOI] [PubMed] [Google Scholar]
- 39.Farley R, Spurling GK, Eriksson L, Del Mar CB. Antibiotics for bronchiolitis in children under two years of age. Cochrane Database Syst Rev. 2014;10:Cd005189. doi: 10.1002/14651858.CD005189.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wan KS, Liu YC, Huang CS, Su YM, Ym S. Effects of low-dose clarithromycin added to fluticasone on inflammatory markers and pulmonary function among children with asthma: a randomized clinical trial. Allergy Rhinol. 2016;7(3):131–134. doi: 10.2500/ar.2016.7.0168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mandhane PJ, Paredes Zambrano De Silbernagel P, Nwe Aung Y, et al. Treatment of preschool children presenting to the emergency department with wheeze with azithromycin: a placebo-controlled randomized trial. PLoS One. 2017;12(8):e0182411. doi: 10.1371/journal.pone.0182411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bacharier LB, Guilbert TW, Mauger DT, et al. Early administration of azithromycin and prevention of severe lower respiratory tract illnesses in preschool children with a history of such illnesses a randomized clinical trial. J Am Med Assoc. 2015;314(19):2034–2044. doi: 10.1001/jama.2015.13896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Stokholm J, Chawes BL, Vissing NH, et al. Azithromycin for episodes with asthma-like symptoms in young children aged 1–3 years: a randomised, double-blind, placebo-controlled trial. Lancet Respir Med. 2016;4(1):19–26. doi: 10.1016/S2213-2600(15)00500-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhang P, Bai J, He J, Liang Y, Chen P, Wang J. A systematic review of tranexamic acid usage in patients undergoing femoral fracture surgery. Clin Interv Aging. 2018;13:1579–1591. doi: 10.2147/CIA.S163950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Higgins JP, Altman DG, Gotzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ (Clinical research ed) 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Borenstein M, Hedges LV, Higgins JP, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. 2010;1(2):97–111. doi: 10.1002/jrsm.12. [DOI] [PubMed] [Google Scholar]
- 47.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 48.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ (Clinical research ed) 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ball BD, Hill MR, Brennor M, Sanks R, Szefler SJ. Effect of low-dose troleandomycin on glucocorticoid pharmacokinetics and airway hyperresponsiveness in severely asthmatic children. Annals of Allergy. 1990;65(1):37–45. [PubMed] [Google Scholar]
- 50.Kamada AK, Hill MR, Iklé DN, Brenner AM, Szefler SJ. Efficacy and safety of low-dose troleandomycin therapy in children with severe, steroid-requiring asthma. J Allergy Clin Immunol. 1993;91(4):873–882. doi: 10.1016/0091-6749(93)90345-g. [DOI] [PubMed] [Google Scholar]
- 51.Strunk RC, Bacharier LB, Phillips BR, et al. Azithromycin or montelukast as inhaled corticosteroid-sparing agents in moderate-to-severe childhood asthma study. J Allergy Clin Immunol. 2008;122(6):e1134:1138–1144. doi: 10.1016/j.jaci.2008.09.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Pinto LA, Pitrez PM, Luisi F, et al. Azithromycin therapy in hospitalized infants with acute bronchiolitis is not associated with better clinical outcomes: a randomized, double-blinded, and placebo-controlled clinical trial. J Pediatr. 2012;161(6):1104–1108. doi: 10.1016/j.jpeds.2012.05.053. [DOI] [PubMed] [Google Scholar]
- 53.Silveira D’Azevedo V, Roza CA, Luisi F, Pitrez PM, Stein RT, Pinto LA. Azithromycin therapy in infants with bronchiolitis reduces recurrent wheezing 3 months after hospitalization: A randomized, placebo-controlled trial. Pediatric Pulmonology. 2016;51:S9. [Google Scholar]
- 54.Pinto LA, Jones MH, Pitrez PM, Stein RT. Azithromycin administered at the time of severe bronchiolitis has a protective effect on subsequent wheezing in infants. Pediatric Pulmonology. 2017;52:S165–S166. [Google Scholar]
- 55.Mccallum GB, Morris PS, Chatfield MD, et al. A single dose of azithromycin does not improve clinical outcomes of children hospitalised with bronchiolitis: a randomised, placebo-controlled trial. PLoS One. 2013;8(9):e74316. doi: 10.1371/journal.pone.0074316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mccallum GB, Morris PS, Grimwood K, et al. Three-weekly doses of azithromycin for indigenous infants hospitalized with bronchiolitis: a multicentre, randomized, placebo-controlled trial. Front Pediatr. 2015;3:32. doi: 10.3389/fped.2015.00032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rasul CH, Kabir A, Rashid A, Mahboob AA, Hassan MA. Role of antibiotic in the outcome of bronchiolitis. Pakistan J Med Sci. 2008;24(5):707–711. [Google Scholar]
- 58.Kabir A, Mollah AH, Anwar KS, Rahman A, Amin R, Rahman ME. Management of bronchiolitis without antibiotics: a multicentre randomized control trial in Bangladesh. Acta Paediatrica Int J Paediatr. 2009;98(10):1593–1599. doi: 10.1111/j.1651-2227.2009.01389.x. [DOI] [PubMed] [Google Scholar]
- 59.Chiong-Manaysay K, Andaya A. Effectiveness of Macrolide (Clarithromycin) treatment on pediatric patients with mild-moderate persistent asthma: a randomised controlled study. Allergy Eur J Allergy Clin Immunol. 2014;69:291. [Google Scholar]
- 60.Tahan F, Ozcan A, Koc N. Clarithromycin in the treatment of RSV bronchiolitis: a double-blind, randomised, placebo-controlled trial. Eur Respir J. 2007;29(1):91–97. doi: 10.1183/09031936.00029206. [DOI] [PubMed] [Google Scholar]
- 61.Koutsoubari I, Papaevangelou V, Konstantinou GN, et al. Effect of clarithromycin on acute asthma exacerbations in children: an open randomized study. Pediatr Allergy Immunol. 2012;23(4):385–390. doi: 10.1111/j.1399-3038.2012.01280.x. [DOI] [PubMed] [Google Scholar]
- 62.Piacentini GL, Peroni DG, Bodini A, et al. Azithromycin reduces bronchial hyperresponsiveness and neutrophilic airway inflammation in asthmatic children: a preliminary report. Allergy Asthma Proc. 2007;28(2):194–198. doi: 10.2500/aap.2007.28.2958. [DOI] [PubMed] [Google Scholar]
- 63.Beigelman A, Bacharier LB, Baty J, et al. Does azithromycin modify viral load during severe respiratory syncytial virus bronchiolitis? J Allergy Clin Immunol. 2015;136(4):1129–1131. doi: 10.1016/j.jaci.2015.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zhou Y, Bacharier LB, Isaacson-Schmid M, et al. Azithromycin therapy during respiratory syncytial virus bronchiolitis: Upper airway microbiome alterations and subsequent recurrent wheeze. J Allergy Clin Immunol. 2016;138(4):1215–1219.e5. doi: 10.1016/j.jaci.2016.03.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Normansell R, Sayer B, Waterson S, Dennett EJ, del Forno M, Dunleavy A. Antibiotics for exacerbations of asthma. Cochrane Database Syst Rev. 2018;6:Cd002741. doi: 10.1002/14651858.CD002741.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Yeh JJ, Wang YC, Hsu WH, Kao CH. Incident asthma and Mycoplasma pneumoniae: a nationwide cohort study. J Allergy Clin Immunol. 2016;137(4):e1016:1017–1023. doi: 10.1016/j.jaci.2015.09.032. [DOI] [PubMed] [Google Scholar]
- 67.Albert RK, Connett J, Bailey WC, et al. Azithromycin for prevention of exacerbations of COPD. N Engl J Med. 2011;365(8):689–698. doi: 10.1056/NEJMoa1104623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Johnston SL, Szigeti M, Cross M, et al. Azithromycin for acute exacerbations of asthma: The AZALEA Randomized Clinical Trial. JAMA Intern Med. 2016;176(11):1630–1637. doi: 10.1001/jamainternmed.2016.5664. [DOI] [PubMed] [Google Scholar]
- 69.Nuermberger E, Bishai WR. The clinical significance of macrolide-resistant Streptococcus pneumoniae: it’s all relative. Clin Infect Dis. 2004;38(1):99–103. doi: 10.1086/380126. [DOI] [PubMed] [Google Scholar]
- 70.Schwerk N, Brinkmann F, Soudah B, Kabesch M, Hansen G. Wheeze in preschool age is associated with pulmonary bacterial infection and resolves after antibiotic therapy. PLoS One. 2011;6(11):e27913. doi: 10.1371/journal.pone.0027913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Beigelman A, Mikols CL, Gunsten SP, Cannon CL, Brody SL, Walter MJ. Azithromycin attenuates airway inflammation in a mouse model of viral bronchiolitis. Respir Res. 2010;11:90. doi: 10.1186/1465-9921-11-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Le Bourgeois M, Goncalves M, Le Clainche L. Bronchoalveolar cells in children. Chest. 2002;122(3):791–797. doi: 10.1378/chest.122.3.791. [DOI] [PubMed] [Google Scholar]
- 73.Kloepfer KM, Lee WM, Pappas TE, et al. Detection of pathogenic bacteria during rhinovirus infection is associated with increased respiratory symptoms and asthma exacerbations. J Allergy Clin Immunol. 2014;133(5):1301–1307. doi: 10.1016/j.jaci.2014.02.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Olsen KM, San Pedro G, Gann LP, Gubbins PO, Halinski DM, Campbell GD. Intrapulmonary pharmacokinetics of azithromycin in healthy volunteers given five oral doses. Antimicrob Agents Chemother. 1996;40(11):2582–2585. doi: 10.1128/aac.40.11.2582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.O’Connor CM, Dunne MW, Pfeffer MA, et al. Azithromycin for the secondary prevention of coronary heart disease events: the WIZARD study: a randomized controlled trial. JAMA. 2003;290(11):1459–1466. doi: 10.1001/jama.290.11.1459. [DOI] [PubMed] [Google Scholar]
- 76.Grayston JT, Kronmal RA, Jackson LA, et al. Azithromycin for the secondary prevention of coronary events. N Engl J Med. 2005;352(16):1637–1645. doi: 10.1056/NEJMoa043526. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Meta-regression scatter plot showing there was no correlation between adverse events risk and male sex ratio.
Meta-regression scatter plot showing there was no correlation between adverse events risk and the duration of macrolides.
Table S1.
PRISMA-P checklist
| Section/topic | ≥ | Checklist item | Reported on page ≥ |
|---|---|---|---|
| Title | |||
| Title | 1 | Identify the report as a systematic review, meta-analysis, or both. | 1 |
| Abstract | |||
| Structured summary | 2 | Provide a structured summary including, as applicable: background; objectives; data sources; study eligibility criteria, participants, and interventions; study appraisal and synthesis methods; results; limitations; conclusions and implications of key findings; systematic review registration number. | 1 abstract |
| Introduction | |||
| Rationale | 3 | Describe the rationale for the review in the context of what is already known. | 2, 3 |
| Objectives | 4 | Provide an explicit statement of questions being addressed with reference to participants, interventions, comparisons, outcomes, and study design (PICOS). | 3 |
| Methods | |||
| Protocol and registration | 5 | Indicate if a review protocol exists, if and where it can be accessed (eg, web address), and, if available, provide registration information including registration number. | 3 |
| Eligibility criteria | 6 | Specify study characteristics (eg, PICOS, length of follow-up) and report characteristics (eg, years considered, language, publication status) used as criteria for eligibility, giving rationale. | 3 |
| Information sources | 7 | Describe all information sources (eg, databases with dates of coverage, contact with study authors to identify additional studies) in the search and date last searched. | 3 |
| Search | 8 | Present full electronic search strategy for at least one database, including any limits used, such that it could be repeated. | 3, Table S2 |
| Study selection | 9 | State the process for selecting studies (ie, screening, eligibility, included in systematic review, and, if applicable, included in the meta-analysis). | 3, 4 |
| Data collection process | 10 | Describe method of data extraction from reports (eg, piloted forms, independently, in duplicate) and any processes for obtaining and confirming data from investigators. | 3, 4 |
| Data items | 11 | List and define all variables for which data were sought (eg, PICOS, funding sources) and any assumptions and simplifications made. | 5–9 |
| Risk of bias in individual studies | 12 | Describe methods used for assessing risk of bias of individual studies (including specification of whether this was done at the study or outcome level), and how this information is to be used in any data synthesis. | 3, Table S3 |
| Summary measures | 13 | State the principal summary measures (eg, risk ratio, difference in means). | 3 |
| Synthesis of results | 14 | Describe the methods of handling data and combining results of studies, if done, including measures of consistency (eg, I2) for each meta-analysis. | 3 |
| Risk of bias across studies | 15 | Specify any assessment of risk of bias that may affect the cumulative evidence (eg, publication bias, selective reporting within studies). | 3, Table S3 |
| Additional analyses | 16 | Describe methods of additional analyses (eg, sensitivity or subgroup analyses, meta-regression), if done, indicating which were pre-specified. | 3 |
| Results | |||
| Study selection | 17 | Give numbers of studies screened, assessed for eligibility, and included in the review, with reasons for exclusions at each stage, ideally with a flow diagram. | 3, 4, Fig 1 |
| Study characteristics | 18 | For each study, present characteristics for which data were extracted (eg, study size, PICOS, follow-up period) and provide the citations. | 6–9, Table 1 |
| Risk of bias within studies | 19 | Present data on risk of bias of each study and, if available, any outcome level assessment (see Item 12). | 5, 8–10, Table S3 |
| Results of individual studies | 20 | For all outcomes considered (benefits or harms), present, for each study: (a) simple summary data for each intervention group (b) effect estimates and confidence intervals, ideally with a forest plot. | 6–11, Fig 2–6 |
| Synthesis of results | 21 | Present results of each meta-analysis done, including confidence intervals and measures of consistency. | 6–11, Fig 2–6 |
| Risk of bias across studies | 22 | Present results of any assessment of risk of bias across studies (see Item 15). | 6–11 |
| Additional analysis | 23 | Give results of additional analyses, if done (eg, sensitivity or subgroup analyses, meta-regression [see Item 16]). | 6–11, Fig 2, Fig 3, Fig 6 |
| Discussion | |||
| Summary of evidence | 24 | Summarize the main findings including the strength of evidence for each main outcome; consider their relevance to key groups (eg, healthcare providers, users, and policy makers). | 11–12 |
| Limitations | 25 | Discuss limitations at study and outcome level (eg, risk of bias), and at review-level (eg, incomplete retrieval of identified research, reporting bias). | 14 |
| Conclusions | 26 | Provide a general interpretation of the results in the context of other evidence, and implications for future research. | 14 |
| Funding | |||
| Funding | 27 | Describe sources of funding for the systematic review and other support (eg, supply of data); role of funders for the systematic review. | 15 |
Note: © 2009 Moher et al.23 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abbreviation: PRISMA-P, Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols.
Table S2.
Searching strategy
| PubMed |
|---|
| ((((((((((Asthma OR asthma*))) OR infantile asthma) OR chronic cough) OR ((Bronchitis, Chronic OR chronic bronchitis))) OR ((Respiratory Sounds OR wheezing OR wheez*))) OR (Bronchiolitis OR Bronchiolitides OR acute bronchiolitis)) OR (Bronchiolitis, Viral OR Viral Bronchiolitides))) in All Fields |
| AND |
| ((((((Erythromycin OR T-Stat OR Erycette OR Erymax OR Ilotycin))) OR ((Clarithromycin OR TE-031 OR A-56268 OR Biaxin))) OR macrolide) OR ((Azithromycin OR Azythromycin OR Sumamed OR Toraseptol OR Vinzam OR CP-62993 OR CP 62993 OR CP62993 OR Zithromax OR Azitrocin OR Azadose OR Ultreon OR Zitromax OR Goxal OR Zentavion))) in All Fields |
| Filters: Child: birth-18 years |
| Embase |
| (‘asthma’ OR ‘asthma’/exp OR asthma OR asthma*) OR (‘chronic bronchitis’/exp) OR (‘abnormal respiratory sound’/exp) OR (infantile NEAR/3 asthma) OR (chronic NEAR/3 cough) OR (chronic NEAR/3 bronchitis) OR (‘wheezing’/exp OR wheezing OR wheez*) OR (‘bronchiolitis’/exp) OR (‘viral bronchiolitis’/exp) OR ((viral AND bronchiolitides OR bronchiolitis OR bronchiolitides OR acute) AND bronchiolitis) OR ((viral NEAR/3 bronchiolitides) OR bronchiolitis OR bronchiolitides OR (acute NEAR/3 bronchiolitis)) |
| AND |
| (‘erythromycin’/exp OR erythromycin OR ‘t stat’/exp OR ‘t stat’ OR ‘erycette’/exp OR erycette OR ‘erymax’/exp) OR ((‘azithromycin’/exp OR azithromycin OR ‘azythromycin’/exp OR azythromycin OR ‘sumamed’/exp OR sumamed OR toraseptol OR ‘vinzam’/exp OR vinzam OR ‘cp 62993′/exp OR ‘cp 62993′ OR cp) AND 62993 OR ‘cp62993′/exp OR cp62993 OR ‘zithromax’/exp OR zithromax OR ‘azitrocin’/exp OR azitrocin OR ‘azadose’/exp OR azadose OR ‘ultreon’/exp OR ultreon OR ‘zitromax’/exp OR zitromax OR goxal OR zentavion) OR (‘clarithromycin’/exp OR clarithromycin OR ‘te 031′/exp OR ‘te 031′ OR ‘a 56268′/exp OR ‘a 56268′ OR ‘biaxin’/exp OR biaxin) OR (‘macrolides’/exp OR macrolides OR ‘macrolide’/exp OR macrolide) |
| AND |
| ([adolescent]/lim OR [child]/lim OR [infant]/lim OR [newborn]/lim OR [preschool]/lim OR [school]/lim) |
| Cochrane |
| (MeSH descriptor: [Asthma] explode all trees) OR (MeSH descriptor: [Bronchitis, Chronic] explode all trees) OR (MeSH descriptor: [Respiratory Sounds] explode all trees) OR (MeSH descriptor: [Bronchiolitis] explode all trees) OR (MeSH descriptor: [Bronchiolitis, Viral] explode all trees) OR (Asthma or asthma* or infantile asthma or chronic cough or chronic bronchitis or Respiratory Sounds or wheezing or wheez*:ti,ab,kw (Word variations have been searched)) OR (Bronchiolitis or Bronchiolitides or acute bronchiolitis or Viral Bronchiolitides:ti,ab,kw (Word variations have been searched)) |
| AND |
| (MeSH descriptor: [Erythromycin] explode all trees) OR (MeSH descriptor: [Azithromycin] explode all trees) OR (MeSH descriptor: [Clarithromycin] explode all trees) OR (MeSH descriptor: [Macrolides] explode all trees) OR (Erythromycin or T-Stat or Erycette or Erymax or Ilotycin:ti,ab,kw (Word variations have been searched)) OR (Azithromycin or Azythromycin or Sumamed or Toraseptol or Vinzam or CP-62993 or CP 62993 or CP62993 or Zithromax or Azitrocin or Azadose or Ultreon or Zitromax or Goxal or Zentavion:ti,ab,kw (Word variations have been searched)) OR (Clarithromycin or TE-031 or A-56268 or Biaxin:ti,ab,kw (Word variations have been searched)) OR (macrolides or macrolide*:ti,ab,kw (Word variations have been searched)) |
| CINAHL |
| (MH “Asthma+”) OR (“chronic cough”) OR (infantile asthma) OR (MH “Bronchitis, Chronic”) OR (MH “Respiratory Sounds”) OR (MH “Bronchiolitis”) OR (asthma* OR infantile asthma OR chronic cough OR chronic bronchitis OR Respiratory Sounds OR wheezing OR wheez* OR Bronchiolitis OR Bronchiolitides OR acute bronchiolitis OR viral bronchiolitis OR Viral Bronchiolitides) |
| AND |
| ((MH “Erythromycin”) OR “Erythromycin”) OR (T-Stat OR Erycette OR Erymax OR Ilotycin) OR ((MH “Clarithromycin”) OR “Clarithromycin”) OR (TE-031 OR A-56268 OR Biaxin) OR ((MH “Antibiotics, Macrolide”) OR “macrolide”) OR ((MH “Azithromycin”) OR “Azithromycin”) OR (Sumamed OR Toraseptol OR Vinzam OR CP-62993 OR CP 62993 OR CP62993 OR Zithromax OR Azitrocin OR Azadose OR Ultreon OR Zitromax OR Goxal OR Zentavion) |
| Narrow by Subject Age: all child |
Abbreviation: CINAHL, Cumulative Index to Nursing and Allied Health.
Table S3.
Risk of bias assessment of each included studya
| Study validity domains | Sequence generation | Allocation concealment | Blinding of participants and personnel | Blinding of outcome assessment | Incomplete outcome data | Selective outcome reporting | Other sources of bias |
|---|---|---|---|---|---|---|---|
| Probiotics | |||||||
| Ball et al,1 1990 | Unclear | Unclear | Low | Low | Low | Unclear | Low |
| Kamada et al,2 1993 | Low | Low | Low | Low | Low | Unclear | Unclear |
| Fonseca-Aten et al,3 2006 | Unclear | Unclear | Unclear | Unclear | High | Low | Unclear |
| Piacentini et al,4 2007 | Low | Unclear | Low | Low | Unclear | Low | Unclear |
| Tahan et al,5 2007 | Low | Unclear | Low | Low | Low | Low | Unclear |
| Rasul et al,6 2008 | Low | Low | Low | Low | High | Low | Unclear |
| Strunk et al,7 2008 | Unclear | Unclear | Unclear | Unclear | Low | Low | Unclear |
| Kabir et al,8 2009 | Low | Unclear | Unclear | Unclear | Low | Low | Unclear |
| Koutsoubari et al,9 2012 | Low | High | High | High | Low | Low | Unclear |
| Pinto et al,10 2012 | Low | Unclear | Unclear | Unclear | Low | Low | Unclear |
| Mccallum et al,11 2013 | Low | Low | Low | Low | Low | Low | Unclear |
| Chiong-Manaysay and Andaya,12 2014 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear |
| Bacharier et al,13 2015 | Low | Low | Low | Low | Low | Low | Unclear |
| Beigelman et al, 14 2015 (letter) | Low | Low | Low | Low | Low | Low | Unclear |
| Beigelman et al,15 2015 | Low | Low | Low | Low | Low | Low | Low |
| Mccallum et al,16 2015 | Low | Low | Low | Low | Low | Low | Low |
| Silveira D’Azevedo et al,17 2016 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear |
| Stokholm et al,18 2016 | Low | Low | Low | Unclear | Low | Low | Low |
| Wan et al,19 2016 | Low | Low | Unclear | Unclear | Low | Low | Unclear |
| Zhou et al,20 2016 | Unclear | Unclear | Low | Low | Low | Low | Low |
| Mandhane et al,21 2017 | Low | Low | Low | Low | Unclear | Low | Low |
| Pinto et al,22 2017 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear |
Notes:
Each domain has been evaluated as being “High”, “Low”, or “Unclear” regarding the risk of bias following the guidelines of Cochrane. Collaboration’s tool for assessing risk of bias, the thorough and original evaluation form is attached in the following pages. “Low” in all Domains would place a study at “Low Risk of Bias”; “High” in any of the Domains would place a study at “High Risk of Bias”; “Unclear” in any of the domains would place the study at “Unclear Risk of Bias”.