Abstract
Background
This study examines the effects of the COPD-specific health promoting self-management intervention “Better living with COPD” on different self-management-related domains, self-efficacy, and sense of coherence (SOC).
Methods
In a randomized controlled design, 182 people with COPD were allocated to either an intervention group (offered Better living with COPD in addition to usual care) or a control group (usual care). Self-management-related domains were measured by the Health Education Impact Questionnaire (heiQ) before and after intervention. Self-efficacy was measured by the General Self-Efficacy Scale (GSE) and SOC was measured by the 13-item Sense of Coherence Scale (SOC-13). Effects were assessed by ANCOVA, using intention-to-treat (ITT) analysis and per-protocol analysis (PPA).
Results
The PPA and the ITT analysis showed significant positive changes on Constructive attitudes and approaches (heiQ) (ITT: P=0.0069; PPA: P=0.0021) and Skill and technique acquisition (heiQ) (ITT: P=0.0405; PPA: P=0.0356). Self-monitoring and insight (heiQ) showed significant positive change in the PPA (P=0.0494). No significant changes were found on the other self-management domains (heiQ), self-efficacy (GSE), or SOC (SOC-13).
Conclusion
Better living with COPD had a significant positive short-term effect on some self-management-related domains, and could be an intervention contributing to the support of self-management in people with COPD. However, further work is needed to establish the clinical relevance of the findings and to evaluate the long-term effects.
Keywords: constructive attitudes and approaches, Health Education Impact Questionnaire (heiQ), self-efficacy, self-monitoring and insight, sense of coherence, skill and technique acquisition
Introduction
COPD is characterized by persistent airflow limitation and respiratory symptoms, due to abnormalities in airways and/or the alveolus, and is a leading cause of mortality and morbidity worldwide.1,2 The disease is common, preventable, and treatable,2 and individuals living with COPD must make daily decisions regarding their own care; thus, self-management is an essential part of living with COPD3,4 and essential for the health care system’s efficiency and effectiveness.5 Still, previous studies suggest that individuals’ management of COPD is often far from optimal.6–8
Various self-management support interventions (SMIs) have been developed to facilitate adequate self-management of COPD.9,10 However, agreement on the definition of SMIs has previously been lacking,11 although their multifaceted nature and emphasis on enhancing people’s active roles and responsibilities have been highlighted.12 Recent guidelines state that SMIs for people with COPD are “structured but personalized and often multi-component interventions, with goals of motivating, engaging and supporting the participants to positively adapt their behavior(s) and develop skills to better manage their disease”.13,14 SMIs should provide information,12 elicit personalized goals, formulate appropriate strategies, and focus on intrinsic processes (eg, motivation, resource utilization, coping, and self-efficacy),11,13–15 and mental health.10 Furthermore, behavior change techniques are recommended to elicit participants’ motivation, confidence, and competence.14
Recent systematic reviews and meta-analyses of randomized controlled trials of COPD-specific multicomponent SMIs in primary care show positive effects of SMIs, such as a reduced number of unscheduled physician visits16 and COPD-related hospital admissions,9,12,17 reduced emotional distress,16,17 improved health-related quality of life (HRQoL),9 and increased self-efficacy.16 Two other systematic and integrative reviews18,19 reported less dyspnea,18 changed health care utilization,18,19 and improved HRQoL in people who have undergone SMIs.18,19 However, some studies included in the reviews12,16–19 contain supervised exercises. This exceeds support levels coherent with SMIs in COPD11 and makes it difficult to distinguish between the effects of the SMI and those of the exercise component. Furthermore, SMIs can have a specified salutogenic orientation and/or use motivational interviewing (MI) techniques. A study by Benzo et al20 concludes that the use of MI may increase a person’s commitment and engagement in self-management and be feasible for people living with COPD, and evidence from related health care settings indicates that the use of a salutogenic orientation may be feasible and effective.21
Few studies have examined the effects of COPD-specific SMIs on self-management-related abilities or behavior. One study’s effects include improved skill and technique acquisition, improved self-monitoring and insight, and more constructive attitudes and approaches.22 Studies have also found better adherence to inhalation treatment and techniques,23 increased smoking cessation,24 improved knowledge of COPD,23–25 improved identification and treatment of exacerbations,23 and improved activation for self-management22 in those who have undergone COPD-specific SMIs.
The importance of integrating SMIs in the primary care setting has been increasingly accentuated.3,26 In this study, we have developed a structured and salutogenic oriented health-promoting COPD-specific SMI, named Better living with COPD,27 for implementation in local municipal health services. Our hypothesis is that Better living with COPD would improve different self-management-related domains, general self-efficacy, and sense of coherence (SOC).
Material and methods
Design and participants
This randomized controlled trial (ClinicalTrials.gov identification: NCT02479841) examines the effects of Better living with COPD on eight self-management-related domains (primary outcomes), general self-efficacy and SOC (secondary outcomes) in a parallel design, with a baseline measure (before randomization) and a follow-up measure 1–2 weeks after the intervention period. We expected that different self-management-related domains would be improved, but general self-efficacy and SOC are rather stable personal characteristics,29–31 therefore it is possible that the time frame (a few weeks after the intervention period) might be too short to see changes in general self-efficacy and SOC.
Participants with COPD from eleven municipalities on the west coast of Norway were recruited from a hospital register with the following inclusion criteria: registered ICD-10 code J44.0, 1, 8, or 9 after January 1, 2010; age ≥18 years; confirmed COPD grade II–IV, according to the Global Initiative for Chronic Obstructive Lung Disease (GOLD);32 and the ability to read and speak Norwegian. Exclusion criteria were substantial cognitive impairment reported in a medical journal (eg, severe dementia, severe Alzheimer’s disease), substantial alcohol and/or drug abuse, or a life expectancy <12 months due to comorbidity. Evaluation of fulfillment of inclusion and exclusion criteria was conducted by a research nurse and a lung specialist in collaboration.
The Health Education Impact Questionnaire (heiQ) was considered the primary outcome, and a sample power for a two-sample t-test (individual randomization), with a suggested effect size of 0.50 (Cohen’s d), a significance level of 0.05, and 80% power, together with an allowed 20% attrition rate, resulted in the inclusion of a minimum of 154 participants.
Allocation, randomization, and procedures
The allocation ratio was 1:1. Included participants were given a running number (based on the alphabetical order of last names), and then the numbers were randomized by a statistician (using MATLAB33) with no access to the participant list. However, the geographically varying recruitment for a group intervention led to challenges with the allocation. Based on previous research,34 the minimum group size was set to five participants, and as an attrition of 20% was expected, this indicates that at a minimum of six participants were to be allocated to each group. In municipalities with fewer than 12 registered participants, it was therefore not possible to establish two groups, and we decided to allocate one group to either intervention or control. In the larger municipalities, participants were allocated individually to the groups. The participants were randomly assigned to groups of ten within the municipality, and then the groups were randomized to either intervention or control, whereas participants from municipalities with only one group were randomized to either intervention or control at the municipality level. In total, 61 participants from six municipalities were randomized at the municipality level, whereas 121 participants were individually randomized. Of the 182 study participants, 92 were randomized to an intervention group and 90 to a control group. Those randomized to an intervention group were offered Better living with COPD in addition to usual care, whereas those randomized to a control group received usual care, although they were informed that they would be offered the intervention ~6 months later.
Participants were recruited between February and June 2015. Questionnaires including demographic and clinical characteristics were measured at baseline (inclusion), whereas the self-management-related domains, general self-efficacy, and SOC were measured at baseline and follow-up. The questionnaires were sent by post, and one reminder was sent out after ~3 weeks in cases with no response.
All participants received an information letter about the study before agreeing to participate and were informed of their allocation in a separate letter after randomization. The study was approved by the Regional Committee of Medical Research Ethics (reference no 2013/1741), and all participants gave written informed consent.
Intervention
The SMI, Better living with COPD, aimed to increase the participants’ consciousness of their potential, their internal and external resources and their abilities to use them, and thus to improve their self-management capabilities in the context of everyday living. A salutogenic orientation was incorporated into the group conversations. This orientation included a focus on SOC; understanding, manageability, and meaningfulness, and on emphasizing health as a continuum, the person’s history, the understanding of tension and strain as potentially health promoting, resources for health, and active adaption,34,35 as described by Langeland et al.36,37 MI,38–40 congruent with improvement in self-efficacy,41,42 enhanced activation for self-management,42 and a salutogenic approach,43 was used as a communication technique.
The intervention consists of weekly 2-hour-long group conversations over 11 weeks.44 The face-to-face conversations took place in meeting locations in the participants’ home municipalities. The sessions started with participants discussing their everyday life experiences. The next part was related to topics initiated by conversations based on reflected notes (homework) related to those topics, voluntarily prepared by the participants. Themes such as problem solving, goal setting, symptoms, social challenges, physical activity, nutrition, medication, smoking cessation, exacerbations, and psychological issues were covered.27 A small booklet with information and advice about physical activity, nutrition, dyspnea, and health care resources was handed out during the SMI45 in addition to a general COPD action plan draft.46 Each session followed a similar structure,27,36 albeit customized according to group dynamics and participants’ needs. From this, the intervention was delivered as planned, but with some variation due to differences in group dynamics.
All group sessions were planned to be moderated by two moderators. The main moderator was a registered nurse (RN) with special competence in COPD care,47 salutogenesis, self-efficacy, and MI. In addition, the main moderator had initial training in the intervention and had previously co-moderated Better living with COPD with the first author. An RN and/or a physiotherapist from the participant’s home municipality participated as co-moderator.
Usual care
The Norwegian guidelines for care and treatment of people with COPD include specific criteria regarding frequency of visits to a general practitioner, smoking cessation, physiotherapy, nutritional advice, and pulmonary rehabilitation.48 Although it is possible that “usual care” varies between municipalities,49,50 the Norwegian health care system is mainly based on public funding and a principle of universal access regardless of residential area.51 Therefore, no precautions were taken in this study to ensure equality in usual care.
Measures
Demographic and clinical characteristics
Age and sex were obtained from the hospital register, whereas education, cohabitation, comorbidity, and years diagnosed with COPD were self-reported.
Lung function
For participants with spirometry conducted according to international standards52,53 less than 12 months prior to enrollment, data on post-bronchodilator FVC and FEV1 were obtained from medical records. For participants with the last spirometry registered more than 12 months prior to enrollment, a new spirometry was conducted according to international standards.52,53 To calculate FEV1 percentage predicted (FEV1% predicted), Norwegian reference values were used.54 COPD disease severity was classified using GOLD criteria2: moderate (II), severe (III), or very severe (IV), defined as FEV1/FVC <0.7 and FEV1% 50%–79% (II), FEV1% 30%–49% (III), or FEV1% <30% (IV).2
Modified Medical Research Council (mMRC) Dyspnoea Scale
The mMRC48,55 Dyspnoea Scale was used to measure dyspnea. This measure asks people to rate dyspnea by choosing the statement best describing when dyspnea occurs. Different statements describing decreasing levels of physical activity that may precipitate shortness of breath are presented on a five-point scale (range 0–4), with higher scores indicating more severe dyspnea.2,55 The mMRC Dyspnoea Scale has shown satisfactory reliability and validity.56–58
COPD Assessment Test (CAT)
To measure COPD symptom burden, the CAT59 was used. The CAT consists of eight items (cough, phlegm, chest tightness, breathlessness, activities, confidence, sleep, and energy) rated on a 0–5 scale. The total score range is 0–40, with a higher score indicating a higher symptom burden.59–61 The CAT has shown satisfactory reliability and validity.59,60,62,63
Self-management
HeiQ, version 2.0,28,64 was used to measure eight self-management-related domains: 1) Positive and active engagement in life; 2) Health directed activities; 3) Skill and technique acquisition; 4) Constructive attitudes and approaches; 5) Self-monitoring and insight; 6) Health service navigation; 7) Social integration and support; and 8) Emotional distress. HeiQ comprises 40 items, scored on a Likert scale ranging from 1 (strongly disagree) to 4 (strongly agree).28,64 Domain scores are calculated by adding the score of items within scales and dividing by the number of items; consequently, all domain scores range between 1 and 4. Higher scores indicate higher levels of self-management ability for all domains, except for the Emotional distress domain, where a higher score indicates more emotional distress. This generic questionnaire has shown satisfactory validity and reliability across diverse settings,28,64–67 and has been used in studies including people with COPD.22,68,69 Cronbach’s alpha ranged from 0.63 (Health service navigation) to 0.90 (Emotional distress).
General Self-Efficacy Scale (GSE)
The GSE was used to measure self-efficacy. The GSE is a ten-item scale designed to assess perceived general self-efficacy.70–72 Each item is scored on a Likert scale ranging from 1 (not at all true) to 4 (exactly true), generating a sum score ranging from 10 to 40. Higher scores indicate higher self-efficacy.70,71 Up to two responses (20%) were allowed to be missing and were replaced by the mean value of the person’s valid scores.73 The GSE has been used in studies including people with COPD,73,74 and has shown satisfactory reliability and validity.30,70,71,73,75
Sense of Coherence Scale-13 (SOC-13)
SOC was measured using the SOC-13.29 The SOC-13 is a 13-item short form of the original 29-item Orientation to Life Questionnaire.29 Each item is rated on a seven-point Likert scale, where the most common anchor points are “never” and “very often”.29 The items cover comprehensibility (five items), manageability (four items), and meaningfulness (four items), generating a total sum score ranging from 13 to 91. Higher scores indicate stronger SOC.70 The SOC-13 has satisfactory reliability and validity,76–80 and has been used in previous COPD studies.81,82 In this study, missing data were substituted separately for individuals who answered at least 75% of the items for each component.
Data handling and statistical analysis
Missing data were a problem in the collected data. We used the observed data for all descriptive analyses. For the inference, we used multiple imputation with 50 imputed data sets.83 The imputation was based on information about heiQ, age, sex, education, FEV1% predicted, GSE, and SOC-13. Data were blinded during the analyses, ie, the groups were labeled with non-identifying terms.
Descriptive statistics were used to characterize the sample. The SMI effect on each heiQ domain, GSE, and SOC-13 was assessed by an analysis of covariance (ANCOVA), ie, a linear model for the follow-up measurement of each outcome depending on intervention type and adjusted for its baseline measure. All models were estimated using intention-to-treat (ITT) analysis and per-protocol analysis (PPA). The ITT analysis was conducted for all available data, while inclusion in the PPA required participants to follow the protocol sufficiently; ie, we included in the PPA all participants who had participated in more than half of the group conversations. The general significance level was set to 0.05. All descriptive computations were conducted using SPSS 24 (IBM Corp., Armonk, NY, USA), whereas the imputation and inference (ANCOVA) were carried out using R 3.484 with the package mice 2.46.85
Results
Participants’ characteristics
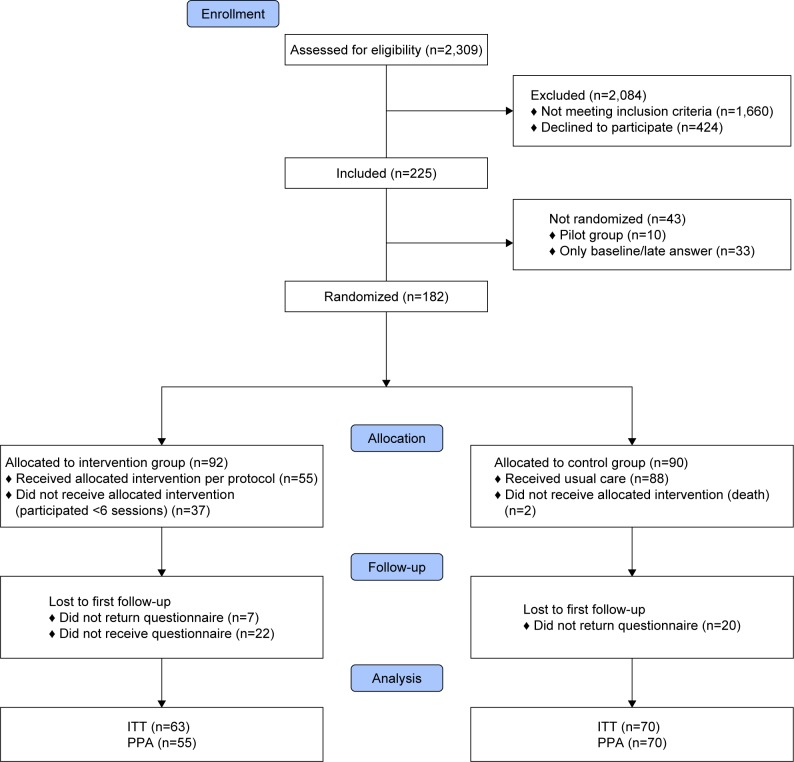
Of the 649 people invited to participate, 225 (34.7%) consented (baseline). Of these, 43 were excluded; ten were allocated to a pilot study and 33 either withdrew from further participation before randomization or responded post-randomization (Figure 1). Consequently, 182 participants were included in this study. The attrition rate was 22.2% in the control group and 31.5% in the intervention group (ITT).
Figure 1.
Overview of recruitment, allocation, and randomization.
Abbreviations: ITT, intention to treat; PPA, per-protocol analysis.
Participants’ characteristics at baseline are shown in Table 1. Self-monitoring and insight (heiQ) had the highest mean ± SD score at 3.03±0.35, whereas Health directed activities (heiQ) had the lowest mean score at 2.63±0.63. The mean score for Emotional distress (heiQ) was 2.38±0.62, and the mean scores for self-efficacy (GSE) and SOC (SOC-13) were 25.97±6.42 and 64.59±9.64, respectively.
Table 1.
Characteristics of participants at baseline
| Randomized (N=182)j | Intervention (N=92)j | Control (N=90)j | |
|---|---|---|---|
|
| |||
| Value | Value | Value | |
|
| |||
| Age (years) | 68.93±8.58 | 68.53±8.16 | 69.34±9.02 |
| Sex, male | 111 (61.0) | 54 (58.7) | 57 (63.3) |
| Education | |||
| Primary school | 57 (32.2) | 29 (31.9) | 28 (32.6) |
| High school/university | 120 (67.8) | 62 (68.1) | 58 (67.4) |
| Cohabitation, living alonea | 54 (30.0) | 27 (29.3) | 27 (30.7) |
| Other chronic diseaseb | 170 (96.6) | 87 (95.6) | 83 (97.6) |
| Comorbidityc | 2.51±1.87 | 2.68±1.91 | 2.33±1.82 |
| FEV1% predicted | 45.03±15.31 | 45.22±14.44 | 44.84±16.23 |
| GOLDd grade | |||
| GOLD II | 73 (40.1) | 35 (38.0) | 38 (42.2) |
| GOLD III | 73 (40.1) | 42 (45.7) | 31 (34.4) |
| GOLD IV | 36 (19.8) | 15 (16.3) | 21 (23.3) |
| Years diagnosed with COPD | 8.83±5.87 | 9.20±6.25 | 8.47±5.49 |
| CATe score | 19.09±7.35 | 18.68±7.15 | 19.51±7.58 |
| mMRCf score | 1.82±1.09 | 1.88±1.06 | 1.76±1.12 |
| mMRC grade 0 | 20 (11.6) | 7 (7.9) | 13 (15.5) |
| mMRC grade 1 | 51 (29.5) | 29 (32.6) | 22 (26.2) |
| mMRC grade 2 | 51 (29.5) | 27 (30.3) | 24 (28.6) |
| mMRC grade 3 | 42 (24.3) | 20 (22.5) | 22 (26.2) |
| mMRC grade 4 | 9 (5.2) | 6 (6.7) | 3 (3.6) |
| Self-management domainsg | |||
| Positive and active engagement in life | 2.92±0.44 | 2.96±0.41 | 2.88±0.46 |
| Health directed activities | 2.63±0.63 | 2.63±0.68 | 2.64±0.58 |
| Skill and technique acquisition | 2.70±0.44 | 2.73±0.45 | 2.68±0.43 |
| Constructive attitudes and approaches | 2.89±0.44 | 2.90±0.40 | 2.88±0.48 |
| Self-monitoring and insight | 3.03±0.35 | 3.06±0.35 | 3.00±0.35 |
| Health service navigation | 2.87±0.38 | 2.93±0.38 | 2.82±0.38 |
| Social integration and support | 2.80±0.44 | 2.83±0.41 | 2.77±0.48 |
| Emotional distress | 2.38±0.62 | 2.41±0.62 | 2.34±0.63 |
| GSE,h total score | 25.97±6.42 | 26.92±6.16 | 24.96±6.57 |
| SOC-13,i total score | 64.59±9.64 | 65.10±9.64 | 64.06±9.66 |
Notes: Data are shown as mean ± SD or n (%).
Cohabitation: living alone; living with someone.
Other chronic disease: yes; no.
Comorbidity: rated between 0 (no comorbidities) and 16 based on a list of common comorbidities.
GOLD, grading of lung function; mild (I), moderate (II), severe (III), or very severe (IV), defined as FEV1/FVC <0.7 and FEV1% ≥80% (I), FEV1% 50%–79% (II), FEV1% 30%–49% (III), or FEV1% <30% (IV).
CAT: score range: 0–40.
mMRC: score range: 0–4.
Domains of the heiQ: score range: 1–4.
GSE: score range: 10–40.
SOC-13: score range: 13–91.
N=182, N=92, and N=90 are the largest N values; for some variables the N is lower.
Abbreviations: CAT, COPD Assessment Test; GOLD, Global Initiative for Chronic Obstructive Pulmonary Disease; GSE, General Self-Efficacy Scale; heiQ, Health Education Impact Questionnaire; mMRC, modified Medical Research Council Dyspnoea Scale; SOC-13, 13-item Sense of Coherence Scale.
Effects of Better living with COPD
As shown in Table 2, both PPA and ITT analysis showed significant positive changes on Constructive attitudes and approaches (heiQ) (PPA: P=0.0021, d=0.38; ITT: P=0.0069, d=0.32) and Skill and technique acquisition (heiQ) (PPA: P=0.0405, d=0.17; ITT: P=0.0356, d=0.17). While the estimated effect on Constructive attitudes and approaches (heiQ) was slightly higher using the PPA [mean change difference (95% CI) PPA: 0.16 (0.03 to 0.30) vs ITT: 0.14 (0.00 to 0.27)], the effect on Skill and technique acquisition (heiQ) [PPA: 0.06 (−0.07 to 0.19); ITT: 0.06 (−0.06 to 0.19)] was similar for both. In addition, the PPA indicated a significant positive change in self-monitoring and insight (heiQ) [P=0.0494, d=0.15, mean change difference (95% CI): 0.05 (−0.07 to 0.18)], although this was not significant in the ITT analysis (Table 2). The changes found in the other self-management domains were insignificant (P≥0.0944), as were the changes in general self-efficacy (GSE) and SOC (SOC-13) (P≥0.1814).
Table 2.
Effects of better living with COPD (primary outcomes) evaluated by PPA and ITT analysis, ANCOVA: means from baseline and follow-up, mean change difference and effect size
| Self- management domains | PPAc | ITT | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||||||||
| Control | Intervention | Mean change differenceb | Control | Intervention | Mean change differenceb | ||||||||||||
|
| |||||||||||||||||
| N | Mean ± SDa | N | Mean ± SDa | Mean | 95% CI | d | P-valued | N | Mean ± SDa | N | Mean ± SDa | Mean | 95% CI | d | P-valued | ||
|
| |||||||||||||||||
| Positive and active engagement in life | Baseline | 68 | 2.87±0.47 | 54 | 2.94±0.40 | 86 | 2.88±0.46 | 91 | 2.96±0.41 | ||||||||
| Follow-up | 68 | 2.91±0.49 | 54 | 3.00±0.32 | 0.02 | −0.13 to 0.17 | 0.04 | 0.3634 | 68 | 2.91±0.47 | 60 | 2.97±0.33 | 0.00 | −0.14 to 0.14 | 0.00 | 0.5543 | |
| Health directed activities | Baseline | 67 | 2.60±0.54 | 54 | 2.53±0.71 | 85 | 2.64±0.58 | 91 | 2.63±0.68 | ||||||||
| Follow-up | 69 | 2.67±0.53 | 54 | 2.68±0.59 | 0.13 | −0.04 to 0.30 | 0.27 | 0.3154 | 69 | 2.67±0.53 | 60 | 2.70±0.59 | 0.11 | −0.05 to 0.28 | 0.25 | 0.3225 | |
| Skill and technique acquisition | Baseline | 68 | 2.68±0.45 | 54 | 2.78±0.44 | 86 | 2.68±0.43 | 90 | 2.73±0.45 | ||||||||
| Follow-up | 67 | 2.70±0.35 | 55 | 2.85±0.40 | 0.06 | −0.07 to 0.19 | 0.17 | 0.0405 | 67 | 2.70±0.35 | 61 | 2.85±0.38 | 0.06 | −0.06 to 0.19 | 0.17 | 0.0356 | |
| Constructive attitudes and approaches | Baseline | 68 | 2.88±0.46 | 54 | 2.93±0.43 | 86 | 2.88±0.48 | 90 | 2.90±0.40 | ||||||||
| Follow-up | 67 | 2.87±0.41 | 54 | 3.09±0.39 | 0.16 | 0.03 to 0.30 | 0.38 | 0.0021 | 67 | 2.87±0.41 | 61 | 3.07±0.41 | 0.14 | 0.00 to 0.27 | 0.32 | 0.0069 | |
| Self-monitoring and insight | Baseline | 69 | 2.97±0.34 | 54 | 3.05±0.33 | 87 | 3.00±0.35 | 91 | 3.06±0.35 | ||||||||
| Follow-up | 69 | 2.98±0.32 | 55 | 3.11±0.27 | 0.05 | −0.07 to 0.18 | 0.15 | 0.0494 | 69 | 2.98±0.32 | 61 | 3.09±0.27 | 0.02 | −0.10 to 0.15 | 0.07 | 0.0944 | |
| Health service navigation | Baseline | 68 | 2.79±0.37 | 54 | 2.92±0.35 | 86 | 2.82±0.38 | 91 | 2.93±0.38 | ||||||||
| Follow-up | 67 | 2.86±0.39 | 55 | 3.00±0.37 | −0.00 | −0.14 to 0.13 | −0.01 | 0.3606 | 67 | 2.86±0.39 | 62 | 3.00±0.38 | 0.00 | −0.13 to 0.13 | 0.00 | 0.3635 | |
| Social integration and support | Baseline | 69 | 2.79±0.48 | 53 | 2.80±0.42 | 87 | 2.77±0.48 | 89 | 2.83±0.41 | ||||||||
| Follow-up | 67 | 2.78±0.46 | 55 | 2.82±0.46 | 0.02 | −0.11 to 0.16 | 0.06 | 0.5623 | 67 | 2.78±0.46 | 61 | 2.82±0.45 | 0.02 | −0.11 to 0.14 | 0.05 | 0.5840 | |
| Emotional distress | Baseline | 68 | 2.32±0.60 | 54 | 2.30±0.61 | 86 | 2.34±0.63 | 90 | 2.41±0.62 | ||||||||
| Follow-up | 67 | 2.29±0.56 | 55 | 2.31±0.70 | −0.04 | −0.22 to 0.14 | −0.08 | 0.8809 | 67 | 2.29±0.56 | 61 | 2.32±0.71 | −0.03 | −0.20 to 0.14 | −0.06 | 0.8914 | |
Notes:
Means are presented from the data, therefore all participants (the total intervention and control groups) who provided data are included in the ITT description of means, including those with responses at only baseline or follow-up.
Mean change difference in both PPA and ITT is from the data; therefore, for both PPA and ITT only those with responses at both baseline and follow-up are represented.
Included in PPA were those who participated in more than half of the sessions on Better living with COPD.
P-value is from the ANCOVA based on multiple imputation (50 imputed data sets based on information on heiQ, education, FEV1%, GSE, and SOC). A P-value <0.05 was considered statistically significant and is marked in bold.
Abbreviations: ANCOVA, analysis of covariance; d, Cohen’s d; GSE, general self-efficacy; heiQ, Health Education Impact Questionnaire; ITT, intention-to-treat; PPA, per-protocol analysis; SOC, sense of coherence.
Discussion
Better living with COPD had a significant positive effect on Constructive attitudes and approaches in both PPA and ITT analysis. Constructive attitudes and approaches covers the important shift in how people view the impact of their condition on their lives, positive attitude, and sense of control and empowerment.28,64 Our finding is supported by a longitudinal study that found improvement in Constructive attitudes and approaches after a similar group-based SMI.22 Together, these findings suggest that participation in SMIs could improve Constructive attitudes and approaches for people with COPD. Although the effect size is larger in the PPA (d=0.38), the ITT analysis (d=0.32) better reflects the clinical effect.86,87 An effect size of 0.32 is considered small, according to Cohen,88 but is higher than the estimated benchmark effect sizes for change in Constructive attitudes and approaches, varying from 0.19 to 0.21.67 The salutogenic orientation of Better Living with COPD could be one explanation for the positive effect on Constructive attitudes and approaches. A salutogenic orientation focuses on health as a continuum, the person’s history, active adaption, and salutary factors, and stressors are seen as possibly salutary,29,36,37,89 and may have contributed to a shift in participants’ attitudes and approaches.
Better living with COPD also had a positive effect on Skill and technique acquisition, significant in both PPA and ITT analysis. The Skill and technique acquisition scale captures knowledge-based skills and techniques related to managing disease-related symptoms and health problems, including the use of particular aids,28 and our finding is supported by Turner et al.22 Inhalation techniques are important skills and techniques related to medication adherence in COPD.13,90 However, incorrect inhalation techniques are common,13,91,92 and inhalation techniques were therefore specifically addressed as a topic in one group session. As a result of this, a surprising finding was the small effect size (d=0.17) in Skill and technique acquisitions. One possible explanation may be related to the group-based intervention. Previous research suggests that repeating education and teach-back approaches are recommended,93–95 but in Better living with COPD, inhalation techniques were specifically addressed at one group session, and a teach-back approach was not mandatory for participants. Another possible explanation could be that inhalation techniques were not what participants had in mind when responding to the generic items in the Skill and technique acquisition scale.28
Furthermore, a significant positive effect of Better living with COPD was also found in the PPA for Self-monitoring and insight (P=0.0494). This is in accordance with the findings in the longitudinal study by Turner et al.22 Still, the effect size in this study (d=0.15) was smaller than the estimated benchmark effect sizes for change in this domain in chronic diseases in general.67 Also, the benchmark sizes presented for changes in heiQ scores are not benchmark sized for clinical relevance.67 Therefore, the clinical relevance of the improvements found on Self-monitoring and insight, as well as on the Constructive attitudes and approaches and Skill and technique acquisition domains, is uncertain.
No significant effects were found on Positive and active engagement in life, Health directed activities, Health service navigation, Social integration and support, or Emotional distress. Previous randomized controlled studies including participants with chronic conditions have reported effects of various SMIs on one or more of these domains.96–98 However, differences between the SMIs, the context, and the participants make direct comparisons difficult, and possible explanations for our findings are multiple. For example, in accordance with models clarifying COPD-specific SMIs,11 Better living with COPD did not include supervised physical training. However, previous studies on pulmonary rehabilitation programs found the frequency and duration of supervised training to be crucial to increasing physical activity levels,99 and items related to physical activity are included in the Health directed activities domain of heiQ.28 Our findings could therefore suggest that support of some self-management-related domains could be better met by means additional to the ones included in Better living with COPD (eg, supervised physical training and individual teach-back methods).
In addition, the changes found in general self-efficacy and SOC were insignificant. The self-management-related domains are described as proximal outcomes of SMIs,28 but because self-efficacy and SOC are relatively stable personal characteristics,29–31 change may need time to develop. This is in line with descriptions of general self-efficacy and SOC as more distal outcomes of SMIs.28 The post-intervention scores were measured shortly after the intervention period, and it is possible that the time frame was too short to detect developing changes in these characteristics. Further work including long-term evaluations is warranted.
Some methodological remarks should be mentioned. Three different nurses were the main group moderators and participants were actively involved in the conversations, leading to possible differences in group dynamics. Although group moderators had education before the SMI, their experience with a specific salutogenic orientation varied, and none had previous experience using MI in group contexts. This may have introduced additional variance, possibly reflecting variance in a real-life clinical implementation, but the effects may have been weaker than with experienced group moderators. The response rate was low, although similar to another study of self-management (cross-sectional),100 but slightly lower than the response rate in another comparable study with inclusion criteria from a hospital register using postal mail.101 A low response rate may increase the risk of volunteer bias. The baseline measurement was performed before randomization, but since participants could not be further blinded, desirability bias could account for some changes in the intervention group. Knowledge of group assignment may affect participants’ responses to outcome measures and their behavior in the trial.102 Yet, this bias may have been reduced by the control group’s expectation of being offered the intervention after the study and possible activation following their knowledge of future SMI participation. Being informed that they would be offered the intervention after ~6 months could have had an impact on participants’ experience of the usual care provided.103 In addition, this study only explored short-term effects possibly affected by positive experiences in the group conversations. Long-term effects as well as prognostic or predictive factors are yet to be investigated. It is also possible that we had easier access to participants through hospital registers, and inclusion may differ in clinical practice. Previous studies suggest that SMIs may be hampered by challenges faced in real-world clinical settings, such as referrers’ lack of enthusiasm.104
One study limitation is that the follow-up measurements were limited because of a clerical error, where 22 intervention group participants did not receive follow-up questionnaires (Figure 1) after leaving the groups. This introduced unnecessary missing data in the ITT analysis. Unfortunately, we lack sufficient information to determine whether this affected the results, although there were no significant differences between these 22 and other participants at baseline on any of the self-management-related domains. This error also made it difficult to evaluate the attrition rate for those allocated to an intervention group, but the attrition rate was slightly higher (22.2%) than the estimated 20% for those allocated to a control group. In addition, we had to adapt the randomization procedure because of unexpectedly few participants in smaller municipalities, leading to a lower power than planned and a potential for introducing confounding variables owing to possible differences in services between the municipalities. The first author’s participation in the SMIs could also raise methodological issues.
Conclusion
No randomized controlled studies have previously evaluated the effects of a salutogenic oriented SMI for people with COPD on the eight self-management-related domains, self-efficacy, and SOC specified in this study, and this study significantly adds to the knowledge of effects of disease-specific and health-promoting SMIs in COPD. Better living with COPD had significant positive effects on some self-management-related domains (Constructive attitudes and approaches, Skills and technique acquisition, and Self-monitoring and insight), whereas no significant effects were found on the other domains, general self-efficacy, and SOC. Therefore, Better living with COPD may serve as one of several means of self-management support, but further work is necessary to establish possible long-term effects of Better living with COPD on the specified domains and to evaluate possible long-term effects on SOC and self-efficacy.
Data sharing statement
Participant data (sociodemographic variables [age, sex, and GOLD grade] and the eight heiQ domains) used in the analysis in this study, together with a complementary specification of the intervention, “Better living with COPD” (in Norwegian), can be obtained on direct request to the corresponding author.
Acknowledgments
The authors thank Mr Gunnar Egge for his contribution in planning and feasibility testing the intervention, and the municipalities for providing meeting locations and staff. This work was supported by the Western Norway Regional Health Authority [grant number 2013/911836] and the Norwegian Extra Foundation for Health and Rehabilitation [grant number 2015/RB13639].
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.López-Campos JL, Tan W, Soriano JB. Global burden of COPD. Respirology. 2016;21(1):14–23. doi: 10.1111/resp.12660. [DOI] [PubMed] [Google Scholar]
- 2.GOLD Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease. 2018. [Accessed March 26, 2018]. Available from: http://goldcopd.org/gold-reports/
- 3.Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary care. JAMA. 2002;288(19):2469–2475. doi: 10.1001/jama.288.19.2469. [DOI] [PubMed] [Google Scholar]
- 4.Lorig KR, Holman H. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med. 2003;26(1):1–7. doi: 10.1207/S15324796ABM2601_01. [DOI] [PubMed] [Google Scholar]
- 5.Holman H, Lorig K. Patient self-management: a key to effectiveness and efficiency in care of chronic disease. Public Health Rep. 2004;119(3):239–243. doi: 10.1016/j.phr.2004.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rogliani P, Ora J, Puxeddu E, Matera MG, Cazzola M. Adherence to COPD treatment: Myth and reality. Respir Med. 2017;129:117–123. doi: 10.1016/j.rmed.2017.06.007. [DOI] [PubMed] [Google Scholar]
- 7.Bryant J, McDonald VM, Boyes A, Sanson-Fisher R, Paul C, Melville J. Improving medication adherence in chronic obstructive pulmonary disease: a systematic review. Respir Res. 2013;14(1):109. doi: 10.1186/1465-9921-14-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sriram KB, Percival M. Suboptimal inhaler medication adherence and incorrect technique are common among chronic obstructive pulmonary disease patients. Chron Respir Dis. 2016;13(1):13–22. doi: 10.1177/1479972315606313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lenferink A, Brusse-Keizer M, van der Valk PD, et al. Self-management interventions including action plans for exacerbations versus usual care in patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2017;8:CD011682. doi: 10.1002/14651858.CD011682.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Newham JJ, Presseau J, Heslop-Marshall K, et al. Features of self-management interventions for people with COPD associated with improved health-related quality of life and reduced emergency department visits: a systematic review and meta-analysis. Int J Chron Obstruct Pulmon Dis. 2017;12:1705–1720. doi: 10.2147/COPD.S133317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wagg K. Unravelling self-management for COPD: what next? Chron Respir Dis. 2012;9(1):5–7. doi: 10.1177/1479972311435910. [DOI] [PubMed] [Google Scholar]
- 12.Jonkman NH, Westland H, Trappenburg JC, et al. Do self-management interventions in COPD patients work and which patients benefit most? An individual patient data meta-analysis. Int J Chron Obstruct Pulmon Dis. 2016;11:2063–2074. doi: 10.2147/COPD.S107884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.GOLD Global Strategy for the Diagnosis, Management and Prevention of COPD, Global Initiative for Chronic Obstructive Lung Disease. 2017. [Accessed September 3, 2017]. Available from: http://goldcopd.org.
- 14.Effing TW, Vercoulen JH, Bourbeau J, et al. Definition of a COPD self-management intervention: International Expert Group consensus. Eur Respir J. 2016;48(1):46–54. doi: 10.1183/13993003.00025-2016. [DOI] [PubMed] [Google Scholar]
- 15.van Hooft SM, Been-Dahmen JMJ, Ista E, van Staa A, Boeije HR. A realist review: what do nurse-led self-management interventions achieve for outpatients with a chronic condition? J Adv Nurs. 2017;73(6):1255–1271. doi: 10.1111/jan.13189. [DOI] [PubMed] [Google Scholar]
- 16.Baker E, Fatoye F. Clinical and cost effectiveness of nurse-led self-management interventions for patients with copd in primary care: A systematic review. Int J Nurs Stud. 2017;71:125–138. doi: 10.1016/j.ijnurstu.2017.03.010. [DOI] [PubMed] [Google Scholar]
- 17.Wang T, Tan JY, Xiao LD, Deng R. Effectiveness of disease-specific self-management education on health outcomes in patients with chronic obstructive pulmonary disease: An updated systematic review and meta-analysis. Patient Educ Couns. 2017;100(8):1432–1446. doi: 10.1016/j.pec.2017.02.026. [DOI] [PubMed] [Google Scholar]
- 18.Zwerink M, Brusse-Keizer M, van der Valk PD, et al. Self management for patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2014;3:CD002990. doi: 10.1002/14651858.CD002990.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jonsdottir H. Self-management programmes for people living with chronic obstructive pulmonary disease: a call for a reconceptualisation. J Clin Nurs. 2013;22(5–6):621–637. doi: 10.1111/jocn.12100. [DOI] [PubMed] [Google Scholar]
- 20.Benzo R, Vickers K, Ernst D, Tucker S, McEvoy C, Lorig K. Development and feasibility of a self-management intervention for chronic obstructive pulmonary disease delivered with motivational interviewing strategies. J Cardiopulm Rehabil Prev. 2013;33(2):113–123. doi: 10.1097/HCR.0b013e318284ec67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pelikan JM. The Application of Salutogenesis in Healthcare Settings. In: Mittelmark MB, Sagy S, Eriksson M, editors. The Handbook of Salutogenesis. Cham: Springer International Publishing; 2017. pp. 261–266. [PubMed] [Google Scholar]
- 22.Turner A, Anderson J, Wallace L, Kennedy-Williams P. Evaluation of a self-management programme for patients with chronic obstructive pulmonary disease. Chron Respir Dis. 2014;11(3):163–172. doi: 10.1177/1479972314539979. [DOI] [PubMed] [Google Scholar]
- 23.Garcia-Aymerich J, Hernandez C, Alonso A, et al. Effects of an integrated care intervention on risk factors of COPD readmission. Respir Med. 2007;101(7):1462–1469. doi: 10.1016/j.rmed.2007.01.012. [DOI] [PubMed] [Google Scholar]
- 24.Efraimsson EO, Hillervik C, Ehrenberg A. Effects of COPD self-care management education at a nurse-led primary health care clinic. Scand J Caring Sci. 2008;22(2):178–185. doi: 10.1111/j.1471-6712.2007.00510.x. [DOI] [PubMed] [Google Scholar]
- 25.Walters J, Cameron-Tucker H, Wills K, et al. Effects of telephone health mentoring in community-recruited chronic obstructive pulmonary disease on self-management capacity, quality of life and psychological morbidity: a randomised controlled trial. BMJ Open. 2013;3(9):e003097. doi: 10.1136/bmjopen-2013-003097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Helse-og omsorgsdepartementet . St meld 47 (2008–2009) Sam-handlingsreformen. Rett behandling – på rett sted – til rett tid. Norwegian; 2009. [Accessed June 1, 2018]. Available from: https://www.regjeringen.no/no/doku-menter/stmeld-nr-47-2008-2009-/id567201/ [Google Scholar]
- 27.Bentsen SB, Bringsvor HB, Kallekodt J, Iversen ES. Extrastiftelsen. Norwegian; 2016. [Accessed June 18, 2018]. Bedre liv med kols; utprøving av et helsefremmende egenomsorgsprogram for pasienter med kols i nærmiljøet der de bor. Available from: https://www.extrastiftelsen.no/prosjekter/bedre-liv-med-kols/ [Google Scholar]
- 28.Osborne RH, Elsworth GR, Whitfield K. The Health Education Impact Questionnaire (heiQ): an outcomes and evaluation measure for patient education and self-management interventions for people with chronic conditions. Patient Educ Couns. 2007;66(2):192–201. doi: 10.1016/j.pec.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 29.Antonovsky A. Unraveling the Mystery of Health: How People Manage Stress and Stay Well. San Francisco: Jossey-Bass; 1987. [Google Scholar]
- 30.Scholz U, Doña BG, Sud S, Schwarzer R. Is general self-efficacy a universal construct? Psychometric findings from 25 countries. Eur J Psychol Assess. 2002;18(3):242–251. [Google Scholar]
- 31.Schwarzer R. Self-efficacy: Thought Control of Action. Washington DC: Hemisphere; 1992. [Google Scholar]
- 32.GOLD Global Initiative for Chronic Obstructive Lung Disease: Global Strategy for the Diagnosis, Management and Prevention of COPD. 2014. [Accessed December 12, 2014]. Available from: https://goldcopd.org/
- 33.MATLAB 9.0. Natick, MA: The MathWorks, Inc; [Google Scholar]
- 34.Antonovsky A. Health, Stress, and Coping. San Francisco: Jossey-Bass; 1979. [Google Scholar]
- 35.Antonovsky A. Unravelling the Mystery of Health. San Francisco: Jossey-Bass; 1987. [Google Scholar]
- 36.Langeland E, Wahl AK, Kristoffersen K, Hanestad BR. Promoting coping: salutogenesis among people with mental health problems. Issues Ment Health Nurs. 2007;28(3):275–295. doi: 10.1080/01612840601172627. [DOI] [PubMed] [Google Scholar]
- 37.Langeland E, Riise T, Hanestad BR, Nortvedt MW, Kristoffersen K, Wahl AK. The effect of salutogenic treatment principles on coping with mental health problems: A randomised controlled trial. Patient Educ Couns. 2006;62(2):212–219. doi: 10.1016/j.pec.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 38.Rollnick S, Miller WR. What is Motivational Interviewing? Behav Cogn Psychother. 1995;23(04):325–334. doi: 10.1017/S1352465809005128. [DOI] [PubMed] [Google Scholar]
- 39.Wagner CC, Ingersoll KS. Motivational Interviewing in Groups. New York: Guilford Press; 2013. [Google Scholar]
- 40.Rollnick S, Miller WR, Butler C. Motivational Interviewing in Health Care: Helping Patients Change Behavior. New York: Guilford Press; 2008. [Google Scholar]
- 41.Lane C, Butterworth S, Speck L. Motivational interviewing groups for people with chronic health conditions. In: Wagner CC, Ingersoll KS, editors. Motivational Interviewing in Groups. New York: Guilford Press; 2013. pp. 314–331. [Google Scholar]
- 42.Linden A, Butterworth SW, Prochaska JO. Motivational interviewing-based health coaching as a chronic care intervention. J Eval Clin Pract. 2010;16(1):166–174. doi: 10.1111/j.1365-2753.2009.01300.x. [DOI] [PubMed] [Google Scholar]
- 43.Højdahl T, Magnus JH, Hagen R, Langeland E. “VINN”- An accredited motivational program promoting convicted women’s sense of coherence and coping. Euro Vista. 2013;2(3):177–190. [Google Scholar]
- 44.Bentsen SB, Langeland E, Holm AL. Evaluation of self-management interventions for chronic obstructive pulmonary disease. J Nurs Manag. 2012;20(6):802–813. doi: 10.1111/j.1365-2834.2012.01469.x. [DOI] [PubMed] [Google Scholar]
- 45.Alsaker T, Egge G, Knutsen BF. Livet med kols – egeninnsats. Helse Fonna, Tysvær kommune, Landsforeningen for hjerte-og lungesyke & FOUSAM. Norwegian; 2014. [Accessed June 12, 2018]. Available from: http://www.helsetorg-modellen.net/wp-content/uploads/2015/01/kols_brosjyre.pdf. [Google Scholar]
- 46.Alsaker T, Egge G, Knutsen BF. Livet med kols – Egenbehandling-splan. Helse Fonna, Tysvær kommune, Landsforeningen for hjerte-og lungesyke & FOUSAM. Norwegian; 2014. [Accessed June 12, 2018]. https://helse-fonna.no/seksjon-behandling/documents/livet-med-kols-behandlingsplan.pdf. [Google Scholar]
- 47.Berland A, Bentsen SB. Patients with chronic obstructive pulmonary disease in safe hands: An education programme for nurses in primary care in Norway. Nurse Educ Pract. 2015;15(4):271–276. doi: 10.1016/j.nepr.2015.03.003. [DOI] [PubMed] [Google Scholar]
- 48.Helsedirektoratet . Kols Nasjonal faglig retningslinje og veileder for forebygging, diagnostisering og oppfølging. Oslo: Helsedirektoratet; 2012. Norwegian. [Google Scholar]
- 49.Riksrevisjonen . The Office of the Auditor General’s investigation of resource utilisation and quality in the health service following the introduction of the Coordination Reform. Document 3:5. Oslo: Office of the Auditor General of Norway; 2015–2016. 2016. Norwegian. [Google Scholar]
- 50.Riksrevisjonen . The Office of the Auditor General’s investigation of public health work. Document 3:11. Oslo: Office of the Auditor General of Norway; 2014–2015. 2015. Norwegian. [Google Scholar]
- 51.Lindahl AK. The Norwegian Health Care System. 2015. [Accessed January 24, 2018]. Available from: https://www.commonwealthfund.org/sites/default/files/documents/___media_files_publications_fund_report_2016_jan_1857_mos-sialos_intl_profiles_2015_v7.pdf.
- 52.Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319–338. doi: 10.1183/09031936.05.00034805. [DOI] [PubMed] [Google Scholar]
- 53.GOLD Global Institute for Chronic Obstructive Lung Disease, GOLD Spirometry Guide. 2010. [Accessed April 27, 2016]. Available from: https://goldcopd.org/gold-spirometry-guide/
- 54.Johannessen A, Lehmann S, Omenaas ER, Eide GE, Bakke PS, Gulsvik A. Post-bronchodilator spirometry reference values in adults and implications for disease management. Am J Respir Crit Care Med. 2006;173(12):1316–1325. doi: 10.1164/rccm.200601-023OC. [DOI] [PubMed] [Google Scholar]
- 55.Fletcher CM. Standardised questionnaire on respiratory symptoms: a statement prepeared and approved by the MRC Committee on the Aetiology of Chronic Bronchitis. Br Med J. 1960;2:1665. [Google Scholar]
- 56.Bestall JC, Paul EA, Garrod R, Garnham R, Jones PW, Wedzicha JA. Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax. 1999;54(7):581–586. doi: 10.1136/thx.54.7.581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Stenton C. The MRC breathlessness scale. Occup Med. 2008;58(3):226–227. doi: 10.1093/occmed/kqm162. [DOI] [PubMed] [Google Scholar]
- 58.Mahler DA, Wells CK. Evaluation of clinical methods for rating dyspnea. Chest. 1988;93(3):580–586. doi: 10.1378/chest.93.3.580. [DOI] [PubMed] [Google Scholar]
- 59.Jones PW, Harding G, Berry P, Wiklund I, Chen WH, Kline Leidy N. Development and first validation of the COPD Assessment Test. Eur Respir J. 2009;34(3):648–654. doi: 10.1183/09031936.00102509. [DOI] [PubMed] [Google Scholar]
- 60.Jones PW, Brusselle G, Dal Negro RW, et al. Properties of the COPD assessment test in a cross-sectional European study. Eur Respir J. 2011;38(1):29–35. doi: 10.1183/09031936.00177210. [DOI] [PubMed] [Google Scholar]
- 61.Karloh M, Fleig Mayer A, Maurici R, Pizzichini MMM, Jones PW, Pizzichini E. The COPD Assessment Test: What do we know so far?: A systematic review and meta-analysis about clinical outcomes prediction and classification of patients into GOLD stages. Chest. 2016;149(2):413–425. doi: 10.1378/chest.15-1752. [DOI] [PubMed] [Google Scholar]
- 62.Dodd JW, Hogg L, Nolan J, et al. The COPD assessment test (CAT): response to pulmonary rehabilitation. A multicentre, prospective study. Thorax. 2011;66(5):425–429. doi: 10.1136/thx.2010.156372. [DOI] [PubMed] [Google Scholar]
- 63.Jones PW, Harding G, Wiklund I, et al. Tests of the responsiveness of the COPD assessment test following acute exacerbation and pulmonary rehabilitation. Chest. 2012;142(1):134–140. doi: 10.1378/chest.11-0309. [DOI] [PubMed] [Google Scholar]
- 64.Wahl AK, Osborne RH, Langeland E, et al. Making robust decisions about the impact of health education programs: Psychometric evaluation of the Health Education Impact Questionnaire (heiQ) in diverse patient groups in Norway. Patient Educ Couns. 2016;99(10):1733–1738. doi: 10.1016/j.pec.2016.05.001. [DOI] [PubMed] [Google Scholar]
- 65.Elsworth GR, Nolte S, Osborne RH. Factor structure and measurement invariance of the Health Education Impact Questionnaire: Does the subjectivity of the response perspective threaten the contextual validity of inferences? SAGE Open Med. 2015. May, [Accessed April 2, 2018]. http://journals.sagepub.com/doi/abs/10.1177/2050312115585041. [DOI] [PMC free article] [PubMed]
- 66.Nolte S, Elsworth GR, Osborne RH. Absence of social desirability bias in the evaluation of chronic disease self-management interventions. Health Qual Life Outcomes. 2013;11(1):114. doi: 10.1186/1477-7525-11-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Elsworth GR, Osborne RH. Percentile ranks and benchmark estimates of change for the Health Education Impact Questionnaire: Normative data from an Australian sample. [Accessed June 1, 2018];SAGE Open Med. 2017 Mar;23:5. doi: 10.1177/2050312117695716. https://www.ncbi.nlm.nih.gov/pubmed/28560039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Schuler M, Musekamp G, Bengel J, Nolte S, Osborne RH, Faller H. Measurement invariance across chronic conditions: a systematic review and an empirical investigation of the Health Education Impact Questionnaire (heiQ™) Health Qual Life Outcomes. 2014;12:56. doi: 10.1186/1477-7525-12-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bélanger A, Hudon C, Fortin M, Amirall J, Bouhali T, Chouinard M-C. Validation of a French-language version of the health education impact Questionnaire (heiQ) among chronic disease patients seen in primary care: a cross-sectional study. Health Qual Life Outcomes. 2015;13(1):1–9. doi: 10.1186/s12955-015-0254-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Schwarzer R. General Self-Efficacy Scale (GSE). [homepage on the Internet] [Accessed March 20, 2017]. [updated 2012, February 12]. Available from: http://userpage.fu-berlin.de/~health/selfscal.htm.
- 71.Schwarzer R. Everything you want to know about the General Self-Efficacy Scale but were afraid to ask. 2014. [Accessed March 20, 2017]. Available from: http://userpage.fu-berlin.de/~health/faq_gse.pdf.
- 72.Schwarzer R, Jerusalem M. Causal and control beliefs. In: Weinman J, Wright S, Johnston M, editors. Measures in Health Psychology: A User’s Portfolio. Windsor: NFER-NELSON; 1995. pp. 35–37. [Google Scholar]
- 73.Andenæs R, Bentsen SB, Hvinden K, Fagermoen MS, Lerdal A. The relationships of self-efficacy, physical activity, and paid work to health-related quality of life among patients with chronic obstructive pulmonary disease (COPD) J Multidiscip Healthc. 2014;7:239–247. doi: 10.2147/JMDH.S62476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Bonsaksen T, Lerdal A, Fagermoen MS. Factors associated with self-efficacy in persons with chronic illness. Scand J Psychol. 2012;53(4):333–339. doi: 10.1111/j.1467-9450.2012.00959.x. [DOI] [PubMed] [Google Scholar]
- 75.Leganger A, Kraft P, Røysamb E, Røysamb E. Perceived self-efficacy in health behaviour research: Conceptualisation, measurement and correlates. Psychol Health. 2000;15(1):51–69. [Google Scholar]
- 76.Eriksson M, Lindström B. Validity of Antonovsky’s sense of coherence scale: a systematic review. J Epidemiol Community Health. 2005;59(6):460–466. doi: 10.1136/jech.2003.018085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Pallant JF, Lae L. Sense of coherence, well-being, coping and personality factors: further evaluation of the sense of coherence scale. Pers Individ Dif. 2002;33(1):39–48. [Google Scholar]
- 78.Schnyder U, Büchi S, Sensky T, Klaghofer R. Antonovsky’s sense of coherence: trait or state? Psychother Psychosom. 2000;69(6):296–302. doi: 10.1159/000012411. [DOI] [PubMed] [Google Scholar]
- 79.Feldt T, Lintula H, Suominen S, Koskenvuo M, Vahtera J, Kivimäki M. Structural validity and temporal stability of the 13-item sense of coherence scale: prospective evidence from the population-based HeSSup study. Qual Life Res. 2007;16(3):483–493. doi: 10.1007/s11136-006-9130-z. [DOI] [PubMed] [Google Scholar]
- 80.Antonovsky A. The structure and properties of the sense of coherence scale. Soc Sci Med. 1993;36(6):725–733. doi: 10.1016/0277-9536(93)90033-z. [DOI] [PubMed] [Google Scholar]
- 81.Delgado C. Sense of coherence, spirituality, stress and quality of life in chronic illness. J Nurs Scholarsh. 2007;39(3):229–234. doi: 10.1111/j.1547-5069.2007.00173.x. [DOI] [PubMed] [Google Scholar]
- 82.Lundman B, Forsberg KA, Jonsén E, et al. Sense of coherence (SOC) related to health and mortality among the very old: the Umeå 85+ study. Arch Gerontol Geriatr. 2010;51(3):329–332. doi: 10.1016/j.archger.2010.01.013. [DOI] [PubMed] [Google Scholar]
- 83.van Buuren S. Flexible Imputation of Missing Data. New York: Taylor and Francis; 2012. [Google Scholar]
- 84.R Core Team A language for statistical computing. 2017. [Accessed April 17, 2018]. Available from: https://www.r-project.org/
- 85.van Buuren S, Groothuis-Oudshoorn K. Mice: Multivariate Imputation by Chained Equations in R. J Stat Softw. 2011;45(3):1–67. [Google Scholar]
- 86.Ranganathan P, Pramesh CS, Aggarwal R. Common pitfalls in statistical analysis: Intention-to-treat versus per-protocol analysis. Perspect Clin Res. 2016;7(3):144–146. doi: 10.4103/2229-3485.184823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Gupta SK. Intention-to-treat concept: A review. Perspect Clin Res. 2011;2(3):109–112. doi: 10.4103/2229-3485.83221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Cohen J. Statistical Power Analysis for the Behavioural Sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum; 1988. [Google Scholar]
- 89.Langeland E, Vinje HF. The application of salutogenesis in mental healthcare settings. In: Mittelmark MB, Sagy S, Eriksson M, editors. The Handbook of Salutogenesis. Cham: Springer International Publishing; 2017. pp. 299–305. [PubMed] [Google Scholar]
- 90.Bonini M, Usmani OS. The importance of inhaler devices in the treatment of COPD. COPD Res and Practice. 2015. [Accessed June 18, 2018]. Available from: https://copdrp.biomedcentral.com/articles/10.1186/s40749-015-0011-0.
- 91.Crompton GK, Barnes PJ, Broeders M, et al. The need to improve inhalation technique in Europe: a report from the Aerosol Drug Management Improvement Team. Respir Med. 2006;100(9):1479–1494. doi: 10.1016/j.rmed.2006.01.008. [DOI] [PubMed] [Google Scholar]
- 92.Melani AS, Bonavia M, Cilenti V, et al. Inhaler mishandling remains common in real life and is associated with reduced disease control. Respir Med. 2011;105(6):930–938. doi: 10.1016/j.rmed.2011.01.005. [DOI] [PubMed] [Google Scholar]
- 93.Klijn SL, Hiligsmann M, Evers S, Román-Rodríguez M, van der Molen T, van Boven JFM. Effectiveness and success factors of educational inhaler technique interventions in asthma & COPD patients: a systematic review. NPJ Prim Care Respir Med. 2017;27(1):24. doi: 10.1038/s41533-017-0022-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Pothirat C, Chaiwong W, Phetsuk N, Pisalthanapuna S, Chetsadaphan N, Choomuang W. Evaluating inhaler use technique in COPD patients. Int J Chron Obstruct Pulmon Dis. 2015;10:1291–1298. doi: 10.2147/COPD.S85681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Sanchis J, Corrigan C, Levy ML, Viejo JL, ADMIT Group Inhaler devices – from theory to practice. Respir Med. 2013;107(4):495–502. doi: 10.1016/j.rmed.2012.12.007. [DOI] [PubMed] [Google Scholar]
- 96.Francis KL, Matthews BL, Van Mechelen W, Bennell KL, Osborne RH. Effectiveness of a community-based osteoporosis education and self-management course: a wait list controlled trial. Osteoporos Int. 2009;20(9):1563–1570. doi: 10.1007/s00198-009-0834-0. [DOI] [PubMed] [Google Scholar]
- 97.Fortin M, Chouinard MC, Dubois MF, et al. Integration of chronic disease prevention and management services into primary care: a pragmatic randomized controlled trial (PR1MaC) CMAJ Open. 2016;4(4):E588–E598. doi: 10.9778/cmajo.20160031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Crotty M, Prendergast J, Battersby MW, et al. Self-management and peer support among people with arthritis on a hospital joint replacement waiting list: a randomised controlled trial. Osteoarthritis Cartilage. 2009;17(11):1428–1433. doi: 10.1016/j.joca.2009.05.010. [DOI] [PubMed] [Google Scholar]
- 99.Corhay JL, Dang DN, Van Cauwenberge H, Louis R. Pulmonary rehabilitation and COPD: providing patients a good environment for optimizing therapy. Int J Chron Obstruct Pulmon Dis. 2014;9:27–39. doi: 10.2147/COPD.S52012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Bos-Touwen I, Schuurmans M, Monninkhof EM, et al. Patient and disease characteristics associated with activation for self-management in patients with diabetes, chronic obstructive pulmonary disease, chronic heart failure and chronic renal disease: a cross-sectional survey study. PLoS One. 2015;10(5):e0126400–e0126415. doi: 10.1371/journal.pone.0126400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Sridhar M, Taylor R, Dawson S, Roberts NJ, Partridge MR. A nurse led intermediate care package in patients who have been hospitalised with an acute exacerbation of chronic obstructive pulmonary disease. Thorax. 2008;63(3):194–200. doi: 10.1136/thx.2007.077578. [DOI] [PubMed] [Google Scholar]
- 102.Karanicolas PJ, Farrokhyar F, Bhandari M. Blinding: Who, what, when, why, how? Can J Surg. 2010;53(5):345–348. [PMC free article] [PubMed] [Google Scholar]
- 103.Cunningham JA, Kypri K, Mccambridge J. Exploratory randomized controlled trial evaluating the impact of a waiting list control design. BMC Med Res Methodol. 2013;13:150. doi: 10.1186/1471-2288-13-150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Ackerman IN, Buchbinder R, Osborne RH. Challenges in evaluating an Arthritis Self-Management Program for people with hip and knee osteoarthritis in real-world clinical settings. J Rheumatol. 2012;39(5):1047–1055. doi: 10.3899/jrheum.111358. [DOI] [PubMed] [Google Scholar]