Abstract
Background
Burnout is a psychological syndrome that is very common among medical residents. It consists of emotional exhaustion (EE), depersonalization (DP) and reduced personal accomplishment (PA).
Objective
To estimate burnout among different medical residency specialties.
Methods
A systematic review with meta-analysis was performed following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. A search of bibliographic databases and grey literature was conducted, from inception to March 2018. The following databases were accessed: Embase, PubMed, Web of Science, Google Scholar and Scopus, and 3,575 studies were found. Methodological quality was evaluated by Agency for Healthcare Research and Quality Methodology Checklist for Cross-Sectional/Prevalence Study. In the final analysis, 26 papers were included. Their references were checked for additional studies, but none were included.
Results
4,664 medical residents were included. High DP, EE and low PA proportions were compared. Specialties were distributed into three groups of different levels of burnout prevalence: general surgery, anesthesiology, obstetrics/gynecology and orthopedics (40.8%); internal medicine, plastic surgery and pediatrics (30.0%); and otolaryngology and neurology (15.4%). Overall burnout prevalence found for all specialties was 35.7%.
Conclusion
The prevalence of burnout syndrome was significantly higher among surgical/urgency residencies than in clinical specialties.
PROSPERO registration
Introduction
First described in 1974,[1] burnout syndrome is a psychological syndrome arising from a continued response to chronic interpersonal stressors while at work.[2] A generic description of burnout defines it as a state of physical and mental exhaustion related to caregiving activities or work.[1,3]
Work-related stress among healthcare professionals has become a serious health problem for workers and the world economy.[4] The syndrome among both doctors in practice and in training, has reached epidemic levels, with a prevalence near to or exceeding 50%.[5–8] Additionally, it has a notable economic impact, since the cost of replacing a physician in the workplace is up to 2–3 times his/her annual salary.[4]
Situations of emotional exhaustion and irritability in the work environment could lead to the development of psychiatric problems, with an emphasis on burnout, which is characterized by its subdimensions, being emotional exhaustion, depersonalization and diminished personal accomplishment.[9,10]
The consequences of burnout are potentially severe for caregivers, patients and health institutions, and include the risk of medical errors, depression, and adverse effects on patient safety.[3] A recent systematic review, including 20 articles, suggests that burnout affects primary healthcare providers (mainly nurses, but also physicians and pharmacists) and leads to high job stress, intense time pressure and workload as well as lack of organizational support.[11] The syndrome also affects patient satisfaction,[12] and along with personal distress, it has been related to self-reported suboptimal patient care practices among residents across numerous medical specialties.[8,13,14]
Focusing on its subdimensions, emotional exhaustion (EE), refers to feelings of overload and depletion of emotional resources; depersonalization (DP), is the negative response to other people, such as colleagues and patients, in a cynical and isolated way; and reduced personal accomplishment (PA), occurs when the subject feels less competent in his/her role.[9,10]
In this context, the Maslach Burnout Inventory (MBI)[15] is the most commonly used self-completion questionnaire for assessing burnout, as it presents greater validity and increased reliability concerning the multiple dimensions of the syndrome than other less common instruments.[9] It was designed to evaluate the three subdimensions, and consists of 22 items divided into three subscales. The EE subscale evaluates the complaints about feeling on edge and exhausted by work. The DP subscale measures impersonal responses and lack of empathy during professional activity, while the PA subscale evaluates the feelings of competence and achievement of success at work.
Resident physicians must develop specific skills in their chosen area during their medical residency in order to maintain quality of patient care.[16] During this period they are subjected to sleep deprivation, high workload and unsatisfactory salaries,[17] as well as taking on many responsibilities in their workplaces.[18,19] This combination of factors makes them vulnerable to the development of burnout,[18] leading to interference with the individual's ability to sort through diagnostic dilemmas, establish rapport, as well as work through complex treatment decision-making.[3] Studies have suggested that residents may experience adverse mental health and work performance, with a high prevalence of the syndrome.[20]
Published data in the scientific literature on burnout syndrome in residents are limited to one-specialty evaluation. Information that analyzes the prevalence of the syndrome in multiple specialties simultaneously would help indicate which residents are more susceptible to this syndrome. A comprehensive search was conducted in 2005, which included 19 studies, but it did not follow strict criteria and, what is more, it is more than ten years old.[21]
The goal of this systematic review with meta-analysis is to summarize the published studies and to estimate burnout syndrome prevalence among different medical resident specialties, as well as to point out the medical specialties most affected by the syndrome.
Methods
This systematic review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)[22] and was registered with the International Prospective Register of Systematic Reviews (PROSPERO reference CRD42018090270).
Data sources and search strategy
A search was conducted using a combination of free-text and medical subject heading (MeSH) search terms, text words and keywords based on each database characteristic focusing on synonyms of burnout syndrome and medical residents.
Accessing the MeSH Database, the following heading related to the burnout syndrome was found: Burnout, Professional–an excessive stress reaction to one’s occupational or professional environment. It is manifested by feelings of emotional and physical exhaustion coupled with a sense of frustration and failure. In regard to medical residents, the MeSH heading is Internship and Residency–Programs of training in MEDICINE and medical specialties offered by hospitals for graduates of MEDICINE to meet the requirements established by accrediting authorities.
Thus, the search strategy utilized was ((((((medical resident) OR resident) OR residency training) OR residency) OR (internship and residency))) AND (((burnout) OR burnout syndrome) OR professional burnout. The following databases were accessed: Embase, PubMed, Web of Science, Google Scholar and Scopus, which yielded 3,575 citations. The above search strategy was used in PubMed, but equivalent synonyms were utilized in each particular database. Electronic searches were made for articles published from January, 1974, when burnout was first described,[1] to March 2018. No language restriction was imposed. No medical librarian was recruited for the search.
Evaluation of the methodological quality of the primary studies
An evaluation of the methodological quality/risk of bias of the primary cross-sectional studies was performed with the instrument Agency for Research and Health Quality (AHRQ) Methodology Checklist for Cross-sectional Study/Prevalence.[23] The AHRQ checklist consists of 11 items, with classifications of ‘yes’, ‘no’, or “unclear’. In this study, the articles are classified as excellent (ten or more items with a ‘yes’ response); ‘good’ (seven to nine ‘yes’ answers); ‘weak’ (from four to six ‘yes’ responses) and ‘poor’ methodological quality (from one to three ‘yes’ answers).
Inclusion and exclusion criteria
The following inclusion criteria were defined: study design—cross-sectional/survey studies; population—medical residents during their specialization training programs; intervention—22 item-MBI version[15] was used as measurement instrument; controls—medical specialties were compared among themselves.; outcome—whether criteria for burnout syndrome, or any of its subdimensions, were present (positivity) according to the MBI; the subdimensions cutoff points adopted—low EE ≤ 18, high EE ≥ 27; low DP ≤ 5, high DP ≥ 10; and high PA ≥ 40, low PA ≤ 33.[24–27]; burnout risk defined as high DP and/or EE cutoffs (low PA was not an obligatory criterion); publication time after 1974, and; ‘excellent’ and ‘good’ quality studies according to Agency for Healthcare Research and Quality (AHRQ) Methodology Checklist for Cross-Sectional/Prevalence Study.[23]
There have been a significant number of studies that have applied shortened versions of the MBI, however, these have included confusing variables and thus have not allowed proper analysis of the subdimensions. Since the full version of the MBI is the most robust and complete burnout measurement tool, others versions were not accepted in this research.
Exclusion criteria were: studies not submitted to and approved by Ethical Committees (or similar); longitudinal studies; results not specified by each individual specialty, and; study population as subgroups among medical residents themselves.
Intervention studies were also excluded, even though there was the possibility that they would provide additional data; it was considered that they would represent a source of heterogenous data and thus would be a conceptual error.
Selection of articles for review
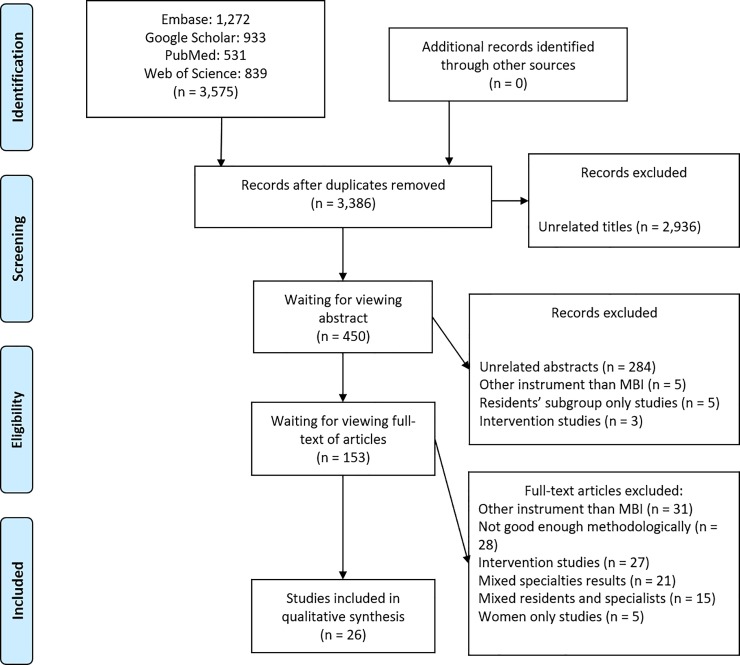
The initial review of the articles was based on analysis of the titles. From the total number of retrieved articles (n = 3,575), 189 were excluded because they were found in more than one database, leaving 3,386 studies. At the screening stage, 2,936 papers were excluded because their titles were too distant from the research theme. The total of approved titles was 450. A selection of these articles from the contents of their abstracts excluded 297 for one or more of the following reasons: (1) unrelated to the research theme; (2) a questionnaire other than the MBI was used; (3) not cross-sectional/survey studies or (4) the study population was restricted to specific subgroups among medical residents (for instance, only male, or only female). The remaining 153 articles were read entirely and 26 were selected to be included in the systematic review, after being considered ‘excellent’ and/or ‘good’ methodological studies. The other 127 papers were also excluded because they were intervention studies; did not present enough research data; had mixed specialty results or had mixed resident and specialist groups. (Fig 1)
Fig 1. Article selection.
Selection process in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses).[22].
The included papers also had their references researched for additional studies that could be included on the systematic review, but no others were found. Four researchers (LFM, HMR, JVSC, and AKG) conducted the process of selecting articles, independently. Disagreements were solved by consensus.
Data extraction
The data were carefully evaluated and extracted independently from all the eligible publications. Data retrieved from the studies included author, publication year, country, specialties evaluated, population size, scores on each MBI dimension and the overall burnout value as shown in Table1.
Statistical analysis
The data were analyzed with STATA 12.0 [28]. Prevalence standard errors were calculated using the standard formula for proportions: sqrt[p*(1 –p)/n]; Heterogeneity across studies in the proportion of medical residents presenting with burnout syndrome, high DP, high EE and low PA was tested with the chi-square and the proportion of total variation across studies attributable to heterogeneity was estimated by the I2 statistic. As there was evidence of significant heterogeneity across studies, the point estimates from each study were combined using a random effects meta-analysis model with the overall estimate obtained with the DerSimonian-Laird method. Sources of heterogeneity across studies were examined with meta-regression. Publication bias and small study effects were assessed with the Egger test.
Results
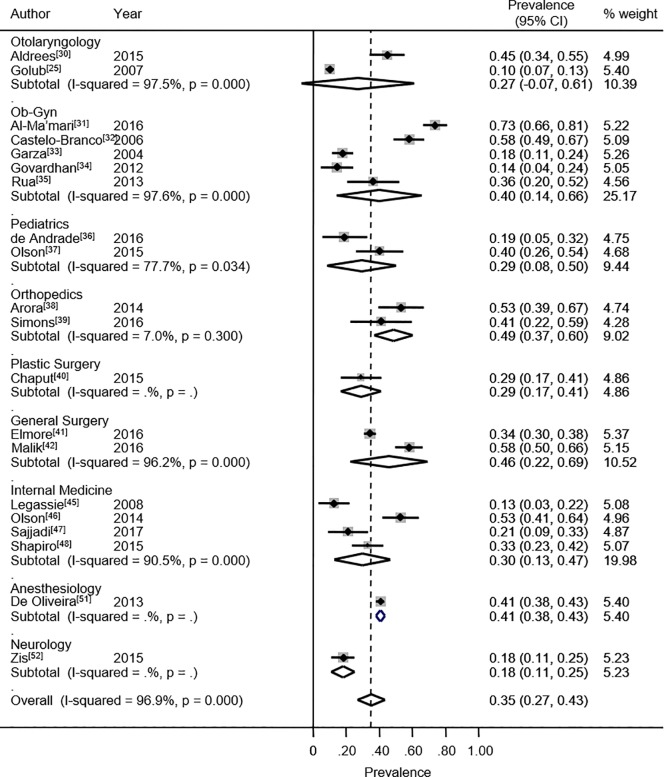
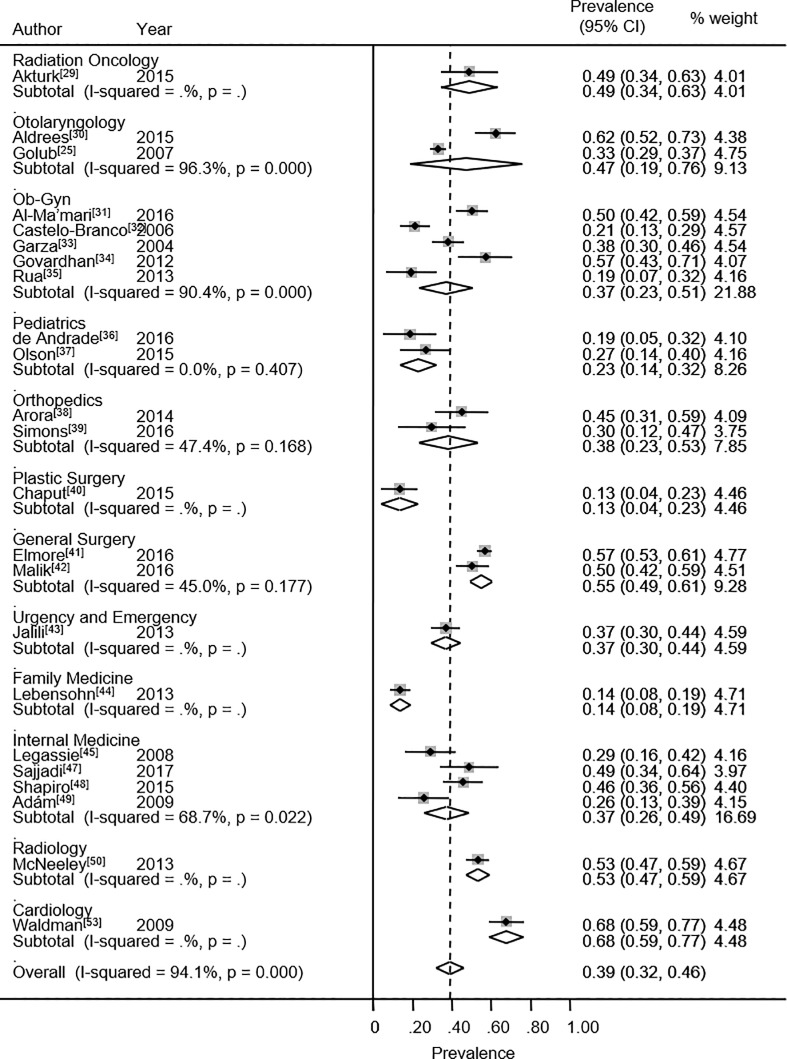
The 26 approved studies involved 4,664 medical residents. The design features of the selected studies are indicated in Table 1. The overall burnout prevalence found for all specialties was 35.1% (95% CI: 26.8% - 43.5%). This estimate was based on 20 studies. The heterogeneity chi-squared was 609.75 (p<0.001) with an I2 statistic of 96.9%. This comparison of the proportion of residents presenting burnout between all types of specialties suggests that the specialties are distributed into three groups with different levels of the syndrome: a group composed of general surgery,[41,42] anesthesiology,[51] obstetrics and gynecology,[31–35] and orthopedics[38,39] with a high prevalence of 42.5%; a group formed by internal medicine,[45–49] plastic surgery[40] and pediatrics,[36,37] with a moderate prevalence of 29.4%; and finally a group including otolaryngology[25,30] and neurology,[16] with a low burnout syndrome prevalence of 23.5% (Fig 2). However, no statistically significant difference was found by meta-regression (p = 0.17).
Table 1. Characterization of systematic review included studies.
| Author | Publication year | Country | Specialties | Sample (n) | Depersonalization % (n) | Emotional Exhaustion % (n) | Personal Accomplishment % (n) | Burnout % (n) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| low | medium | high | Low | medium | High | low | medium | high | ||||||
| Akturk[29] | 2015 | Turkey | Radiation Oncology | 45 | 37.8 (17) | 35.6 (16) | 26.7 (12) | 15.6 (7) | 35.6 (16) | 48.9 (22) | 13.3 (6) | 17.8 (8) | 68.9 (31) | a |
| Aldrees[30] | 2015 | Saudi Arabia | Otolaryngology | 85 | 21.2 (18) | 23.6 (20) | 55.3 (47) | 14.1 (12) | 23.5 (20) | 62.3 (53) | 56.5 (48) | 27.1 (23) | 16.5 (14) | 44.7 (38) |
| Golub[25] | 2007 | U.S.A. | Otolaryngology | 514 | 25.1 (129) | 22.0 (113) | 52.9 (272) | 37.9 (195) | 29.0 (149) | 33.1 (170) | 21.6 (111) | 30.3 (156) | 48.0 (247) | 9.92 (51) |
| Subtotal | 599 | 25.6 (147) | 22.2 (133) | 53.3 (319) | 34.6 (207) | 28.2 (169) | 37.2 (223) | 26.5 (159) | 29.9 (179) | 43.6 (261) | 14.9 (89) | |||
| Al-Ma’mari[31] | 2016 | Canada | Obstetrics and Gynecology | 143 | a | a | 64.3 (92) | a | a | 50.3 (72) | 24.5 (35) | a | a | 73.4 (105) |
| Castelo-Branco[32] | 2006 | Spain | Obstetrics and Gynecology | 109 | a | a | 53.2 (58) | a | a | 21.1 (23) | a | a | a | 57.8 (63) |
| Garza[33] | 2004 | U.S.A. | Obstetrics and Gynecology | 136 | a | a | 47.1 (64) | a | a | 38.2 (52) | 19.1 (26) | a | a | 17.6 (24) |
| Govardhan[34] | 2012 | U.S.A. | Obstetrics and Gynecology | 49 | 18.4 (9) | 28.6 (14) | 53.1 (26) | 20.4 (10) | 22.4 (11) | 57.1 (28) | 38.8 (19) | 32.6 (16) | 28.6 (14) | 14.3 (7) |
| Rua[35] | 2013 | France | Obstetrics and Gynecology | 36 | 36.1 (13) | 33.3 (12) | 30.6 (11) | 47.2 (17) | 33.3 (12) | 19.4 (7) | 33.3 (12) | 55.6 (20) | 11.1 (4) | 36.1 (13) |
| Subtotal | 473 | 25.9 (22) | 30.6 (26) | 53.1 (251) | 31.8 (27) | 27.1 (23) | 38.5 (182) | 25.3 (92) | 42.3 (36) | 21.2 (18) | 44.9 (212) | |||
| de Andrade[36] | 2016 | Brazil | Pediatrics | 32 | 40.6 (13) | 34.4 (11) | 25.0 (8) | 46.9 (15) | 34.3 (11) | 18.7 (6) | 3.13 (1) | 59.4 (19) | 37.5 (12) | 18.7 (6) |
| Olson[37] | 2015 | U.S.A. | Pediatrics | 45 | a | a | 24.4 (11) | a | a | 26.7 (12) | 8.89 (4) | a | a | 40.0 (18) |
| Subtotal | 77 | 24.7 (19) | 18.0 (23.38) | 6.49 (5) | 31.2 (24) | |||||||||
| Arora[38] | 2014 | Australia | Orthopedics | 51 | 19.6 (10) | 45.1 (23) | 35.3 (18) | 19.6 (10) | 35.3 (18) | 45.1 (23) | 33.3 (17) | 33.3 (17) | 33.3 (17) | 52.9 (27) |
| Simons[39] | 2016 | U.S.A. | Orthopedics | 27 | 40.7 (11) | 22.2 (6) | 37.0 (10) | 26.0 (7) | 44.4 (12) | 29.6 (8) | 26.0 (7) | 33.3 (9) | 40.7 (11) | 40.7 (11) |
| Subtotal | 78 | 26.9 (21) | 37.2 (29) | 35.1 (28) | 21.8 (17) | 38.5 (30) | 39.7 (31) | 30.8 (24) | 33.3 (26) | 35.9 (28) | 48.7 (38) | |||
| Chaput[40] | 2015 | France | Plastic Surgery | 52 | 59.6 (31) | 15.4 (8) | 25.0 (13) | 63.5 (33) | 23.1 (12) | 13.5 (7) | 46.1 (24) | 21.1 (11) | 30.8 (16) | 28.8 (15) |
| Elmore[41] | 2016 | U.S.A. | General Surgery | 664 | 20.9 (139) | 29.2 (194) | 49.8 (331) | 19.7 (131) | 23.5 (156) | 56.8 (377) | 16.1 (107) | 37.5 (249) | 46.4 (308) | 34.0 (226) |
| Malik[42] | 2016 | Pakistan | General Surgery | 133 | 24.8 (33) | 25.6 (34) | 49.6 (66) | 16.5 (22) | 33.1 (44) | 50.4 (67) | 53.4 (71) | 26.3 (35) | 20.3 (27) | 57.9 (77) |
| Subtotal | 797 | 21.6 (172) | 28.6 (228) | 49.1 (397) | 19.2 (153) | 25.1 (200) | 55.7 (444) | 22.3 (178) | 35.6 (284) | 42.0 (335) | 38.0 (303) | |||
| Jalili[43] | 2013 | Iran | Urgency and Emergency | 165 | a | a | 39.4 (65) | a | a | 37.0 (61) | 46.1 (76) | a | a | a |
| Lebensohn[44] | 2013 | U.S.A. | Family Medicine | 168 | 50.6 (85) | 25.6 (43) | 23.8 (40) | 58.3 (98) | 28.0 (47) | 13.7 (23) | a | a | a | a |
| Legassie[45] | 2008 | Canada | Internal Medicine | 48 | 29.2 (14) | 35.4 (17) | 35.4 (17) | 39.6 (19) | 31.2 (15) | 29.1 (14) | 27.1 (13) | 41.7 (20) | 31.2 (15) | 12.5 (6) |
| Olson[46] | 2014 | U.S.A. | Internal Medicine | 78 | a | a | a | a | a | a | a | a | a | 52.6 (41) |
| Sajjadi[47] | 2017 | Canada | Internal Medicine | 43 | 21.0 (9) | 32.6 (14) | 46.5 (21) | 11.6 (5) | 39.5 (17) | 48.8 (21) | 32.6 (14) | 34.9 (15) | 32.6 (14) | 20.9 (9) |
| Shapiro[48] | 2015 | U.S.A. | Internal Medicine | 94 | a | a | 50.0 (47) | a | a | 45.7 (43) | 77.7 (73) | a | a | 33.0 (31) |
| Adám[49] | 2009 | Hungary | Internal Medicine | 43 | a | a | 41.9 (18) | a | a | 25.6 (11) | 97.7 (42) | a | a | a |
| Subtotal | 306 | 25.3 (23) | 34.1 (31) | 47.7 (102) | 26.4 (24) | 35.2 (32) | 39.0 (89) | 62.3 (142) | 38.5 (35) | 31.9 (29) | 33.1 (87) | |||
| McNeeley[50] | 2013 | U.S.A. | Radiology | 266 | 50.7 (135) | a | 49.2 (131) | 47.0 (124) | a | 53.4 (142) | a | a | a | a |
| De Oliveira[51] | 2013 | U.S.A. | Anesthesiology | 1,417 | a | a | a | a | a | a | a | a | a | 40.6 (575) |
| Zis[52] | 2015 | Greece | Neurology | 116 | a | a | a | a | a | a | a | a | a | 18.1 (21) |
| Waldman[53] | 2009 | Argentina | Cardiology | 105 | a | a | 72.4 (76) | a | a | 67.6 (71) | 10.5 (11) | a | 51.4 (54) | a |
| Total | 4,664 | 34.6 (1051) | 27.0 (525) | 47.6 (1453) | 31.9 (706) | 27.7 (540) | 43.0 (1313) | 28.05 (704) | 35.6 (598) | 41.6 (784) | 35.7 (1364) | |||
Extracted data from approved studies.
aData not informed.
Fig 2. Burnout prevalence.
Forest plot of prevalence of burnout syndrome among medical and surgical residents.
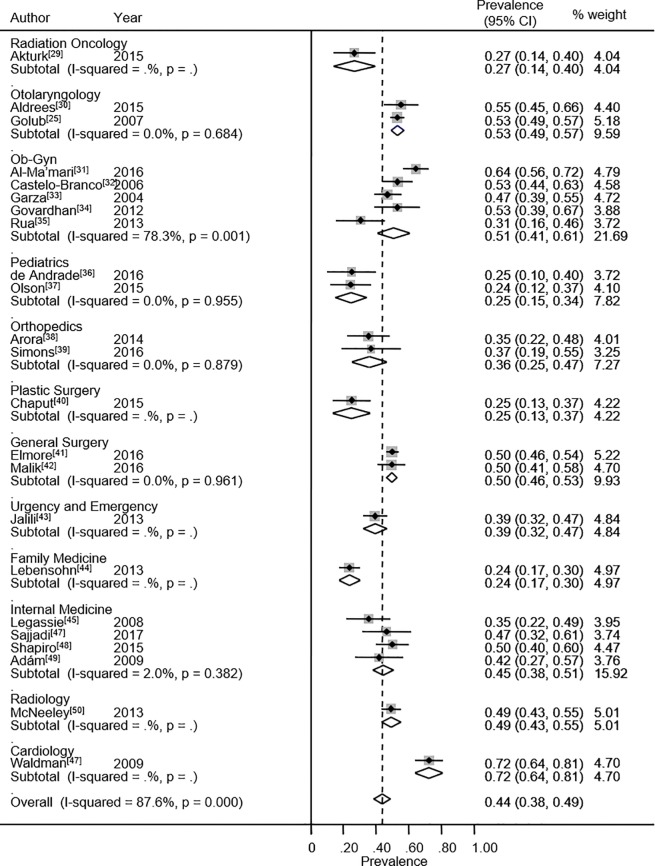
Concerning subdimensions, prevalence rates of high DP were reported in 23 studies. The heterogeneity chi-squared was 177.4 (p<0.001) with an I2 statistic of 87.6%. The meta-analytic prevalence estimate of high DP for all specialties was 43.6% (95% CI: 38.4% - 48.9%). The highest DP values were found in cardiology (defined as a medical residency for the purposes of the systematic review, although it is defined as a fellowship in the U.S.A),[53] otolaryngology with 53.3%[25,30] and obstetrics and gynecology with 50.6%.[31–35] (Fig 3). The specialties showing the highest percentages of low DP were plastic surgery (59.6%),[40] radiology (50.8%)[50] and family medicine (50.6%).[44]
Fig 3. Depersonalization.
Forest plot of prevalence of high depersonalization among medical and surgical residents.
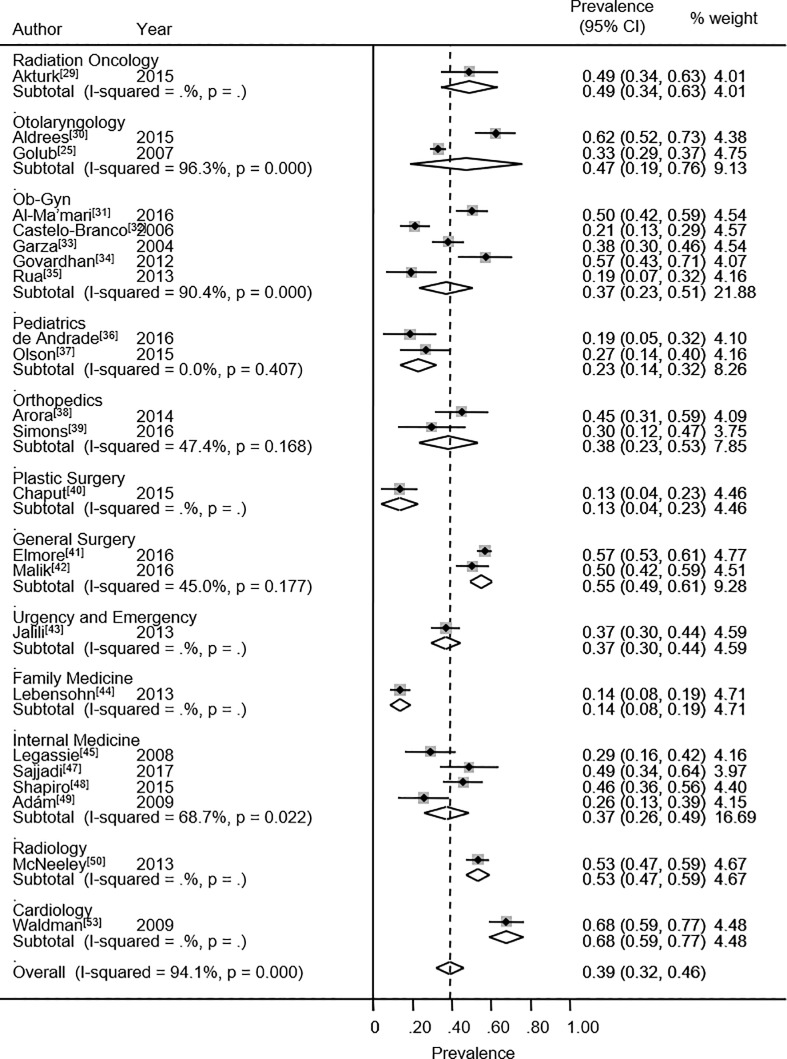
The overall prevalence rate of high EE was 38.9% (95% CI: 31.8% - 46.0%). Twenty-three studies reported high EE. The heterogeneity chi-squared was 369.8% (p<0.001) with an I2 statistic of 94.1%. The specialties presenting the highest percentage values for high EE are general surgery (54.8%), otolaryngology (47.3%) and radiation oncology (48.9%) (Fig 4). In contrast, plastic surgery (63.5%),[40] and family medicine (58.3%)[44] exhibited the highest percentage values for low EE.
Fig 4. Emotional exhaustion.
Forest plot of prevalence of high emotional exhaustion among medical and surgical residents.
The PA values demonstrated a different pattern. An overall value for low PA was equal to 34.3% (95% CI: 21.3% - 47.2%). Data was available from 20 studies. The heterogeneity chi-squared was 1348.6 (p<0.001) and I2 statistic was 98.6%. Internal medicine (59.2%);[45–49] plastic surgery (46.1%)[40] and urgency and emergency (46.1%)[43] had the residents with the lowest personal accomplishment values (Fig 5). However, radiation oncology (68.9%),[29] and cardiology (51.4%)[53] were the specialties with the highest personal accomplishment values.
Fig 5. Personal accomplishment.
Forest plot of prevalence of low personal accomplishment among medical and surgical residents.
Specialty, country and publication year were evaluated as sources of heterogeneity with meta-regression, but no statistically significant association was found. There was no evidence of publication bias or small study effects according to the Egger test. The estimated bias coefficient was 2.33 with a standard error of 2.18 (p = 0.30).
Discussion
This systematic review and meta-analysis suggests that residents/interns in surgical/urgency (SU) specialties (general surgery, anesthesiology, obstetrics and gynecology and orthopedics) are those with the highest prevalence of burnout syndrome, confirming previous studies conducted on physicians after specialization[4] Brazilian study, evaluating 250 residents, and in agreement with our study, identified that surgical residences are positively associated with the syndrome. Additionally, having suffered a stressful event in the last 6 months was independently associated with the syndrome (this event may have been in the same environment as the medical residency).[54]
Obstetrics and gynecology and general surgery were also specialties with a high prevalence, according to a comprehensive search performed previously, suggesting that these specialties are consolidated residencies with the highest burnout rates.[21] A possible explanation for this fact could be the emergency routine, given that the resident is dealing directly with life-threatening situations and that there is an overload of shifts, conditions that are common to these specialties. Both analyses cited above also had the following low burnout syndrome specialties in common: otolaryngology, plastic surgery and neurology. These are predominantly clinical residencies, with substantially less shifts and more elective and non-urgent situations.
In regard to the subdimensions, obstetrics and gynecology was the only one of the three specialties with the highest DP values that also had a high overall burnout prevalence. Such high prevalence was confirmed in a previous meta-analysis,[55] which included 12 obstetrics and gynecology studies. Cardiology was the specialty with the highest DP, but as the single study on cardiology did not show overall burnout ratio, this specialty could not be considered in the high prevalence group. However, among the highest percentages of low DP specialties, only plastic surgery also had a low burnout syndrome level. This discrepancy could also be seen in subdimension EE: cardiology had high EE, but there was no description of the overall burnout prevalence, as was with the other two high specialties in this category. Regarding low EE levels, plastic surgery was the only specialty having low overall burnout rate. Despite no residence review studies having been found on this specialty, a systematic review[56] showed very similar results (burnout syndrome and its subdimensions) when analyzing plastic surgeons after residence. Therefore, this partial heterogeneity shows burnout as a complex and multi-dimensional syndrome, as one dimension can prevail over another. Therefore, its final definition proves to be the real interaction of its subdimensions.
Current scientific literature suggests some individual risk factors for the onset of the syndrome in physicians. As previously mentioned, chronic exposure to stress is the main risk factor.[57] In this sense, Drummond[58] states that the practice of clinical medicine itself would be an important factor, since the medical professional is in constant contact with sick people, with pain, patients, and their families. Along with this, there is the combination of great responsibility for the health of other human beings and the lack of dedication to one’s personal life: during medical training in residences, the doctor is not taught to balance his dedication to work with his/her private life. Curiously, in physicians working in urgent departments, rather than the severity of the patients, organizational factors such as impaired working relationships showed a greater association with burnout syndrome. Finally, certain sociodemographic characteristics appear to be risk factors in the medical population: a young age, female gender, negative marital status and high workload.[57]
Burnout syndrome in medical personal, however, appears not to be a problem generated in the medical residence. A Chinese systematic review including 33 studies found substantial burnout levels in medical students, with over 40% of Chinese medical students having more than moderate levels of burnout.[59] The higher levels were found in more senior students.
An American cross-sectional study evaluating the syndrome in medical students, verified its presence already in the pre-clinical years, with 71% of the students receiving the diagnosis. These future doctors, in a 2018 study, had already exhibited high values since the first year of medical school. Among the main risk factors, a cross-sectional study found that lack of confidence in the acquisition of medical knowledge, not seeing the course as a source of pleasure and discomfort with academic activities were positively correlated with the syndrome.[60]
Another systematic review performed recently evaluated specialists themselves (after residency), assessing 24 specialties. It showed an elevation in burnout incidence from 2011 to 2014 in all specialties, the most affected being emergency medicine, urology, orthopedics, internal medicine and anesthesiology.[4]
As stated previously,[61] burnout occurring in medical students from SU specialties has the potential to negatively affect at the personal and institutional level, which could result in a negative attitude, absenteeism, poor performance, as well as inducing medical errors. For each increase of one point in the depersonalization score (based on the MBI) there is an 11% increase in the likelihood of reporting a medical error.[5] On the other hand, for a one-point increase in the emotional exhaustion score there is a 5% increase in the likelihood of reporting an error. Even in the absence of medical errors, burnout culminates in the decline in the quality of medical care because both residents and practicing physicians with syndrome symptoms report a reduction in compassion at work, succinct conversations with patients, and other suboptimal patient care experiences.[14,62]
This situation demonstrates how the problem of burnout should be addressed in the contexts of training, education and work. First, it is necessary to recognize that the problem exists and what its impacts are. To evaluate the prevalence and intensity of the syndrome, the best option is to use validated instruments (MBI) and apply these to students, interns, residents and the medical specialists themselves, periodically. This will not only allow a view of the status, it will also allow for the measurement of the effectiveness of the measures adopted.
Strategies against burnout can be divided into preventive and therapeutic. In prevention, the actions must be concentrated on the risk factors mentioned above and, thus, the modification of the organizational structure and work processes, improvements in the relationship between the professional and the organization and the promotion of healthy behaviors in physicians (mainly resilience).[57]
In regard to therapeutic strategies, a 2018 systematic review of 13 studies summarizes the results of the research in proposing training, starting from medical graduation, or coping strategies, interpersonal skills, management of negative emotions and relaxation techniques.[63]
Limitations of this review
Despite all the efforts deployed, this systematic review has certain limitations that should be considered when interpreting the results. Heterogeneity is a potential problem, since in the I2 statistic, there was a range from 87.6 to 98.6% in the summarized data. An explanation beyond meta-regression was attempted, but this analysis did not identify explanatory factors, probably due to the limited number of primary studies. Although, it is reasonable to consider that one possible explanation for this heterogeneity is that residents from different countries were included, and the different professional practices and cultures may have influenced the response to the MBI. Additionally, the study objective (including different medical specialties) may have concurred to increase this heterogeneity.
We minimized the likelihood of this issue by performing a careful search for published studies using explicit criteria for study inclusion, precise data extraction, and strict data analysis. In addition, as only cross-sectional studies were included, it is not possible to point out the main factors related to a higher prevalence of burnout syndrome in certain medical residences. Finally, it is an important fact that residency training differs from country to country and from program to program, and that program–or nation-specific data may not generalize well to a specialty-wide burnout rate.
Finally, this may lead to a critical interpretation of the meta-analysis and compromises any kind of generalization of the results, A larger number of standardized studies is needed, in order to reduce heterogeneity and, thus, allow for the application of future studies in another population of medical residents.
Conclusions
Burnout syndrome was identified as having a high prevalence among surgical/urgency (SU) residencies, but is not a single specialty problem, it affects all the medical residencies in different ways. Additionally, it is a health care organization problem, damaging mainly the patients’ well-being and likely has a financial impact. This systematic review and meta-analysis, by analyzing its prevalence among different specialties, makes it possible to prioritize certain areas (such as SU specialties) in the fight against burnout and its consequences. It cannot be denied that clinical specialties are affected, but since they are not explicitly harmed by this syndrome, public health efforts should concentrate on where the problem is explicit. Therefore, health interventions, such as reductions in duty-hours, mindfulness training, psychiatry guided self-development groups and mantra induced meditation (Respiratory One Method), which have already been established and proposed [64] can contribute to the reduction of burnout in medical residencies such as general surgery, anesthesiology, obstetrics and gynecology and orthopedics.
Supporting information
Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
(PDF)
Mesh terms combination entered in databases.
(PDF)
Graphic presentation of small study effects and publication bias.
(PDF)
Compilation of all data collected during the research.
(XLSX)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Freudenberger HJ. Staff Burn-Out. J Soc Issues. 1974;90(1):159–65. 10.1111/j.1540-4560.1974.tb00706.x [DOI] [Google Scholar]
- 2.Maslach C, Leiter MP. Understanding the burnout experience: Recent research and its implications for psychiatry. World Psychiatry. 2016;15(2):103–11. 10.1002/wps.20311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ishak WW, Lederer S, Mandili C, Nikravesh R, Seligman L, Vasa M, et al. Burnout During Residency Training: A Literature Review. J Grad Med Educ [Internet]. 2009;1(2):236–42. 10.4300/JGME-D-09-00054.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rothenberger DA. Physician Burnout and Well-Being: A Systematic Review and Framework for Action. Dis Colon Rectum. 2017;60(6):567–76. 10.1097/DCR.0000000000000844 [DOI] [PubMed] [Google Scholar]
- 5.Shanafelt TD, Balch CM, Bechamps GJ, Russell T, Dyrbye L, Satele D, et al. Burnout and Career Satisfaction Among American Surgeons. Trans. Meet Am Surg Assoc [Internet]. 2009;127(3):107–15. 10.1097/SLA.0b013e3181ac4dfd [DOI] [PubMed] [Google Scholar]
- 6.Shanafelt TD, Boone S, Tan L, Dyrbye LN, Sotile W, Satele D, et al. Burnout and Satisfaction With Work-Life Balance Among US Physicians Relative to the General US Population. Arch Intern Med [Internet]. 2012;172(18):1377 10.1001/archinternmed.2012.3199 [DOI] [PubMed] [Google Scholar]
- 7.Shanafelt TD, Hasan O, Dyrbye LN, Sinsky C, Satele D, Sloan J, et al. Changes in Burnout and Satisfaction with Work-Life Balance in Physicians and the General US Working Population between 2011 and 2014. Mayo Clin Proc [Internet]. Elsevier Inc; 2015;90(12):1600–13. 10.1016/j.mayocp.2015.08.023 [DOI] [PubMed] [Google Scholar]
- 8.West CP, Novotny PJ, Sloan JA, Kolars JC, Habermann TM, Shanafelt TD. Association of Perceived Medical Errors A Prospective Longitudinal Study. 2016;296(9):1071–8. 10.1001/jama.296.9.1071 [DOI] [PubMed] [Google Scholar]
- 9.Maslach C, Jackson S. The measurement of experienced Burnout. J Occup Behav [Internet]. 1981;2(2):99–113. 10.1002/job.4030020205/pdf [DOI] [Google Scholar]
- 10.Carlotto MS, Palazzo LDS. Síndrome de burnout e fatores associados: um estudo epidemiológico com professores. Cad Saude Publica [Internet]. 2006. May;22(5):1017–26. 10.1590/S0102-311X2006000500014 [DOI] [PubMed] [Google Scholar]
- 11.Dugani S, Afari H, Hirschhorn LR, Ratcliffe H, Veillard J, Martin G, et al. Prevalence and factors associated with burnout among frontline primary health care providers in low- and middle-income countries: A systematic review. Gates Open Res [Internet]. 2018;2(May):4 doi: 10.12688/gatesopenres.12779.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shanafelt TD, Balch CM, Bechamps G, Russell T, Dyrbye L, Satele D, et al. Burnout and Medical Errors Among American Surgeons. Ann Surg [Internet]. 2010;251(6):995–1000. 10.1097/SLA.0b013e3181bfdab3 [DOI] [PubMed] [Google Scholar]
- 13.Firth-Cozens J, Greenhalgh J. Doctors’ perceptions of the links between stress and lowered clinical care. Soc Sci Med. 1997;44(7):1017–22. 10.1016/S0277-9536(96)00227-4 [DOI] [PubMed] [Google Scholar]
- 14.Shanafelt T et al. Burnout and Self-Reported Patient Care in an Internal Medicine Residency Program. Ann Intern Med. 2002;136(5):358–67. 10.7326/0003-4819-136-5-200203050-00008 [DOI] [PubMed] [Google Scholar]
- 15.Maslach C, Jackson S, Leiter M. The Maslach Burnout Inventory: Manual CPP Inc; 1996;(January):191–218. Available from: https://www.researchgate.net/profile/Christina_Maslach/publication/277816643_The_Maslach_Burnout_Inventory_Manual/links/5574dbd708aeb6d8c01946d7/The-Maslach-Burnout-Inventory-Manual.pdf [Google Scholar]
- 16.Zis P, Anagnostopoulos F, Sykioti P. Burnout in medical residents: a study based on the job demands-resources model. Sci World J [Internet]. 2014;2014:1–10. 10.1155/2014/673279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lockley SW, Cronin JW, Evans EE, Cade BE, Lee CJ, Landrigan CP, et al. Effect of Reducing Interns’ Weekly Work Hours on Sleep and Attentional Failures. N Engl J Med [Internet]. 2004. October 28;351(18):1829–37. 10.1056/NEJMoa041404 [DOI] [PubMed] [Google Scholar]
- 18.Thomas NK. Resident Burnout. JAMA [Internet]. 2004. December 15;292(23):2880 10.1001/jama.292.23.2880 [DOI] [PubMed] [Google Scholar]
- 19.Geurts S, Rutte C, Peeters M. Antecedents and consequences of work-home interference among medical residents. Soc Sci Med. 1999;48(9):1135–48. 10.1016/S0277-9536(98)00425-0 [DOI] [PubMed] [Google Scholar]
- 20.Levey RE. Sources of Stress for Residents and Recommendations for Programs to Assist Them. Acad Med [Internet]. 2001;76(2):142–50. 10.1097/00001888-200102000-00010 [DOI] [PubMed] [Google Scholar]
- 21.Prins JT, Gazendam-Donofrio SM, Tubben BJ, Van Der Heijden FMMA, Van De Wiel HBM, Hoekstra-Weebers JEHM. Burnout in medical residents: A review. Med Educ [Internet]. 2007. August;41(8):788–800. http://wiley.com/10.1111/j.1365-2923.2007.02797.x [DOI] [PubMed] [Google Scholar]
- 22.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev [Internet]. 2015;4(1):1 10.1186/2046-4053-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.AHQR. Methods Guide for Effectiveness and Comparative Effectiveness Reviews. In: Methods Guide for Effectiveness and Comparative Effectiveness Reviews [Internet]. 2008. Available from: https://effectivehealthcare.ahrq.gov/sites/default/files/pdf/cer-methods-guide_overview.pdf [Google Scholar]
- 24.Maslach C. A multidimensional theory of burnout In: Cooper CL, editor. Theories of Organizational Stress. 1st ed Manchester: Oxford University Press; 1998. Available from: https://www.researchgate.net/profile/Christina_Maslach/publication/280939428_A_Multidimensional_Theory_of_Burnout/links/55cd2b0708aebebb8 f577ea5/A-Multidimensional-Theory-of-Burnout.pdf [Google Scholar]
- 25.Golub JS, Weiss PS, Ramesh AK, Ossoff RH, Johns MM. Burnout in residents of otolaryngology-head and neck surgery: a national inquiry into the health of residency training. Acad Med [Internet]. 2007. June;82(6):596–601. 10.1097/ACM.0b013e3180556825 [DOI] [PubMed] [Google Scholar]
- 26.Fletcher AM, Pagedar N, Smith RJH. Factors correlating with nurnout in practicing otolaryngologists. Otolaryngol—Head Neck Surg. 2012;146(2):234–9. 10.1177/0194599811428585 [DOI] [PubMed] [Google Scholar]
- 27.Johns MM, Ossoff RH. Burnout in academic chairs of otolaryngology: head and neck surgery. Laryngoscope [Internet]. 2005;115(11):2056–61. 10.1097/01.MLG.0000181492.36179.8B [DOI] [PubMed] [Google Scholar]
- 28.StataCorp LLCataCorp LLC. Stata Statistical Software: Release 12. StataCorp.; 2011.
- 29.Akturk N. Burnout syndrome and depression levels and related factors in Turkish radiation oncology residents. Turkish J Oncol [Internet]. 2015;30(3):109–17. 10.5505/tjoncol.2015.1256 [DOI] [Google Scholar]
- 30.Aldrees T, Badri M, Islam T, Alqahtani K. Burnout among otolaryngology residents in Saudi Arabia: A multicenter study. J Surg Educ [Internet]. Elsevier; 2015. September;72(5):844–8. 10.1016/j.jsurg.2015.02.006 [DOI] [PubMed] [Google Scholar]
- 31.Al-Ma’mari NO, Naimi AI, Tulandi T. Prevalence and predictors of burnout among obstetrics and gynecology residents in Canada. Gynecol Surg [Internet]. Gynecological Surgery; 2016. November 20;13(4):323–7. 10.1007/s10397-016-0955-3 [DOI] [Google Scholar]
- 32.Castelo-Branco C, Figueras F, Eixarch E, Quereda F, Cancelo MJ, González S, et al. Stress symptoms and burnout in obstetric and gynaecology residents. BJOG An Int J Obstet Gynaecol [Internet]. 2007. January 4;114(1):94–8. doi: wiley.com/10.1111/j.1471-0528.2006.01155.x [DOI] [PubMed] [Google Scholar]
- 33.Garza JA, Schneider KM, Promecene P, Monga M. Burnout in Residency: A Statewide Study. South Med J [Internet]. 2004. December;97(12):1171–3. 10.1097/01.SMJ.0000129926.66568.10 [DOI] [PubMed] [Google Scholar]
- 34.Govardhan LM, Pinelli V, Schnatz PF. Burnout, depression and job satisfaction in obstetrics and gynecology residents. Conn Med [Internet]. 2012. August;76(7):389–95. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23248861 [PubMed] [Google Scholar]
- 35.Rua C, Body G, Marret H, Ouldamer L. Prévalence du syndrome d’épuisement professionnel parmi les internes de gynécologie-obstétrique et facteurs associés. J Gynécologie Obs Biol la Reprod [Internet]. Elsevier Masson SAS; 2015. January;44(1):83–7. doi: org/10.1016/j.jgyn.2013.12.001 [DOI] [PubMed] [Google Scholar]
- 36.de Andrade APM, Amaro E, Farhat SCL, Schvartsman C. Higher burnout scores in paediatric residents are associated with increased brain activity during attentional functional magnetic resonance imaging task. Acta Paediatr [Internet]. 2016. June;105(6):705–13. wiley.com/10.1111/apa.13371 [DOI] [PubMed] [Google Scholar]
- 37.Olson K, Kemper KJ, Mahan JD. What Factors Promote Resilience and Protect Against Burnout in First-Year Pediatric and Medicine-Pediatric Residents? J Evid Based Complementary Altern Med [Internet]. 2015;20(3):192–8. 10.1177/2156587214568894 [DOI] [PubMed] [Google Scholar]
- 38.Arora M, Diwan AD, Harris IA. Prevalence and factors of burnout among Australian orthopaedic trainees: a cross-sectional study. J Orthop Surg (Hong Kong) [Internet]. 2014. December;22(3):374–7. 10.1177/230949901402200322 [DOI] [PubMed] [Google Scholar]
- 39.Simons BS, Foltz PA, Chalupa RL, Hylden CM, Dowd TC, Johnson AE. Burnout in U.S. Military Orthopaedic Residents and Staff Physicians. Mil Med [Internet]. 2016. August;181(8):835–9. 10.7205/MILMED-D-15-00325 [DOI] [PubMed] [Google Scholar]
- 40.Chaput B, Bertheuil N, Jacques J, Smilevitch D, Bekara F, Soler P, et al. Professional Burnout Among Plastic Surgery Residents. Ann Plast Surg [Internet]. 2015. July;75(1):2–8. 10.1097/SAP.0000000000000530 [DOI] [PubMed] [Google Scholar]
- 41.Elmore LC, Jeffe DB, Jin L, Awad MM, Turnbull IR. National Survey of Burnout among US General Surgery Residents [Internet]. Vol. 223, Journal of the American College of Surgeons. Elsevier Ltd; 2016. 440–451 p. doi: org/10.1016/j.jamcollsurg.2016.05.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Malik AA, Bhatti S, Shafiq A, Khan RS, Butt UI, Bilal SM, et al. Burnout among surgical residents in a lower-middle income country—Are we any different? Ann Med Surg [Internet]. 2016. August;9:28–32. 10.1016/j.amsu.2016.05.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jalili M, Sadeghipour Roodsari G, Bassir Nia A. Burnout and associated factors among iranian emergency medicine practitioners. Iran J Public Health [Internet]. 2013. September 15;42(9):1034–42. 10.1038/ijos.2012.26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lebensohn P, Dodds S, Benn R, Brooks AJ, Birch M, Cook P, et al. Resident wellness behaviors: relationship to stress, depression, and burnout. Fam Med [Internet]. 2013. September;45(8):541–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24129866 [PubMed] [Google Scholar]
- 45.Legassie J, Zibrowski EM, Goldszmidt MA. Measuring resident well-being: Impostorism and burnout syndrome in residency. J Gen Intern Med [Internet]. 2008. July 10;23(7):1090–4. 10.1007/s11606-008-0536-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Olson SM. Burnout and Physical Activity in Minnesota Internal Medicine Resident Physicians. J Grad Med Educ. 2014;(December):669–74. 10.4300/JGME-D-13-00396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sajjadi S, Norena M, Wong H, Dodek P. Moral distress and burnout in internal medicine residents. Can Med Educ J [Internet]. 2017. February;8(1):e36–43. 10.1016/j.jcrc.2015.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Shapiro J, Zhang B, Warm EJ. Residency as a Social Network: Burnout, Loneliness, and Social Network Centrality. J Grad Med Educ [Internet]. 2015. December;7(4):617–23. 10.4300/JGME-D-15-00038.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Adám S, Torzsa P, Gyorffy Z, Vörös K, Kalabay L. Frequent high-level burnout among general practitioners and residents. Orv Hetil. 2009;150(7):317–23. 10.1556/OH.2009.28544 [DOI] [PubMed] [Google Scholar]
- 50.McNeeley MF, Perez FA, Chew FS. The emotional wellness of radiology trainees: Prevalence and predictors of burnout. Acad Radiol [Internet]. Elsevier Ltd; 2013;20(5):647–55. 10.1016/j.acra.2012.12.018 [DOI] [PubMed] [Google Scholar]
- 51.De Oliveira GS, Chang R, Fitzgerald PC, Almeida MD, Castro-Alves LS, Ahmad S, et al. The prevalence of burnout and depression and their association with adherence to safety and practice standards: A survey of united states anesthesiology trainees. Anesth Analg. 2013;117(1):182–93. 10.1213/ANE.0b013e3182917da9 [DOI] [PubMed] [Google Scholar]
- 52.Zis P, Artemiadis AK, Lykouri M, Xirou S, Roussopoulou A, Papageorgiou E, et al. Residency Training: Determinants of burnout of neurology trainees in Attica, Greece. Neurology [Internet]. 2015. September 15;85(11):e81–4. 10.1212/WNL.0000000000001924 [DOI] [PubMed] [Google Scholar]
- 53.Waldman S V., Diez JCL, Arazi HC, Linetzky B, Guinjoan S, Grancelli H Burnout, Perceived Stress, and Depression Among Cardiology Residents in Argentina. Acad Psychiatry [Internet]. 2009. July 1;33(4):296–301. 10.1176/appi.ap.33.4.296 [DOI] [PubMed] [Google Scholar]
- 54.Gouveia PA da C, Ribeiro MHC, Aschoff CA de M, Gomes DP, Silva NAF da, Cavalcanti HAF. Factors associated with burnout syndrome in medical residents of a university hospital. Rev Assoc Med Bras [Internet]. 2017. June;63(6):504–11. 10.1590/1806-9282.63.06.504 [DOI] [PubMed] [Google Scholar]
- 55.Chunming WM, Harrison R, MacIntyre R, Travaglia J, Balasooriya C. Burnout in medical students: A systematic review of experiences in Chinese medical schools. BMC Med Educ. BMC Medical Education; 2017;17(1):1–11. 10.1186/s12909-016-0842-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Campbell DA, Sonnad SS, Eckhauser FE, Campbell KK, Greenfield LJ. Burnout among American surgeons. Surgery. 2001;130(4):696–705. 10.1067/msy.2001.116676 [DOI] [PubMed] [Google Scholar]
- 57.Burnout Kumar S. and Doctors: Prevalence, Prevention and Intervention. Healthcare [Internet]. 2016. June 30;4(3):37 10.3390/healthcare4030037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Drummond D. Physician Burnout: Its Origin, Symptoms, and Five Main Causes. Fam Pract Manag [Internet]. 2015;22(5):42–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26554564 [PubMed] [Google Scholar]
- 59.Daniels AH, DePasse JM, Kamal RN. Orthopaedic Surgeon Burnout: Diagnosis, Treatment, and Prevention. J Am Acad Orthop Surg [Internet]. 2016. April;24(4):213–9. 10.5435/JAAOS-D-15-00148 [DOI] [PubMed] [Google Scholar]
- 60.Boni RA dos S, Paiva CE, de Oliveira MA, Lucchetti G, Fregnani JHTG, Paiva BSR. Burnout among medical students during the first years of undergraduate school: Prevalence and associated factors. Bianchi C editor. PLoS One [Internet]. 2018. March 7;13(3):e0191746 10.1371/journal.pone.0191746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Moradi Y, Baradaran HR, Yazdandoost M, Atrak S, Kashanian M. Prevalence of Burnout in residents of obstetrics and gynecology: A systematic review and meta-analysis. Med J Islam Repub Iran [Internet]. 2015;29(4):235 Available from: http://www.ncbi.nlm.nih.gov/pubmed/26793673 [PMC free article] [PubMed] [Google Scholar]
- 62.Dimou FM, Eckelbarger D, Riall TS. Surgeon burnout: A systematic review. J Am Coll Surg [Internet]. Elsevier Ltd; 2016;222(6):1230–9. 10.1016/j.jamcollsurg.2016.03.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wiederhold BK, Cipresso P, Pizzioli D, Wiederhold M, Riva G. Intervention for physician burnout: A systematic review. Open Med [Internet]. 2018. July 4;13(1):253–63. 10.1515/med-2018-0039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Williams D, Tricomi G, Gupta J, Janise A. Efficacy of Burnout Interventions in the Medical Education Pipeline. Acad Psychiatry [Internet]. 2015. February 18;39(1):47–54. 10.1007/s40596-014-0197-5 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
(PDF)
Mesh terms combination entered in databases.
(PDF)
Graphic presentation of small study effects and publication bias.
(PDF)
Compilation of all data collected during the research.
(XLSX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.