A study of practice effects found that just four trials of the (JHFT) significantly improved test performance.
Abstract
The Jebsen Hand Function Test (JHFT) is a standardized assessment that has been used as a clinical outcome measure. To appropriately interpret the effects of an intervention on hand function (as measured by the JHFT), the extent to which this instrument shows significant practice effects must be quantified. The purpose of this study was to determine whether the JHFT is susceptible to within-session practice effects. The results showed that the dominant and nondominant hands significantly improved on the JHFT and many of its subtests over six consecutive trials. Although practice effects might complicate the interpretation of change due to intervention, we briefly relate our findings to emerging neuropsychological evidence that practice effects may indicate a person’s motor learning potential or treatment responsiveness.
The Jebsen Hand Function Test (JHFT) is a clinical assessment of hand function. Its three main advantages include its ability to (1) provide objective measurement of standardized motor tasks relative to published normative data, (2) assess a wide range of hand functions commonly used in activities of daily living, and (3) be administered in a short amount of time (Jebsen et al., 1969). Because of these advantages, the JHFT has also been used as an outcome measure for documenting effects in rehabilitation interventions (e.g., Beekhuizen & Field-Fote, 2005; Charles & Gordon, 2007; Friel et al., 2016). Therefore, the JHFT is, by design, administered multiple times.
Much of the normative data for the JHFT, however, have been compiled according to the original standard JHFT protocol (Jebsen et al., 1969) by testing each hand only once. Although test–retest reliability was initially reported as acceptable, more recent studies have suggested that performance on the JHFT is not entirely stable over time, and therefore it may be subject to significant practice effects. Generally speaking, the term practice effects has been defined as improvements in test performance due to repeated exposure to the test (McCaffrey et al., 2000).
Some studies have accounted for potential JHFT practice effects by introducing a short familiarization phase (5–10 trials) to let participants achieve a stable baseline (Boggio et al., 2006; Hummel et al., 2005). This dose of practice has not, however, been formally established; neither have previous studies statistically compared trial-by-trial performance on the overall JHFT or its subtests. Although within-session practice effects may raise concerns about the stability or reliability of an assessment, they have clinical prognostic value (Duff et al., 2010). Thus, the purpose of this exploratory study was to test whether the JHFT and any of its subtests are susceptible to within-session practice effects.
Method
Participants
Twelve adults with no neurological impairment and a mean age of 26.3 yr (standard deviation = 3.1) participated. Participants were recruited from among students at the University of South Carolina. No compensation or academic credit was provided for participation. Given that an even smaller sample of healthy young adults had demonstrated (yet not statistically compared) within-session improvements on the JHFT in the nondominant hand (n = 8; Boggio et al., 2006), we expected that our sample size was sufficient for testing potential within-session practice effects. (Effect sizes, which indicate adequate power for detection of trial-by-trial differences, are described below.)
Exclusion criteria included (1) one or more self-reported neurological conditions (e.g., history of concussion); (2) acute or chronic musculoskeletal conditions that could affect upper extremity motor function; and (3) left-handedness or ambidexterity. Hand dominance was determined using a modified version of the Edinburgh Handedness Questionnaire (Oldfield, 1971). Only participants with a laterality quotient of ≥80% (“strongly right-handed”) were included. All procedures were carried out with prior approval by the affiliated institutional review board. Informed consent was obtained from all participants before they enrolled in the study.
Jebsen Hand Function Test
The JHFT is an assessment of hand function during simulated activities of daily living that includes a variety of timed motor activities (Jebsen et al., 1969). It involves seven subtests: (1) Card Turning; (2) picking up paper clips and placing them into a can (referred to as Picking Up Small Common Objects); (3) picking up small objects (raw kidney beans) with a teaspoon and placing them into a can (referred to as Simulated Feeding); (4) Stacking Checkers; (5) moving large, light cans (referred to as Moving Light Objects); and (6) moving heavy cans (referred to as Moving Heavy Objects). The seventh JHFT subtest involves writing a copied sentence that includes 24 letters and is written at a third-grade reading level. This writing subtest is often excluded in experimental studies because of its large differences between hands, dependence on education level, and low reliability (Beebe & Lang, 2009; Sears & Chung, 2010). Thus, our primary measure of JHFT performance was the total time to complete six of the seven subtests, excluding the writing test, which is consistent with previous studies that have used the JHFT in laboratory experiments (Boggio et al., 2006; Charles & Gordon, 2007; Convento et al., 2014; Hummel et al., 2005). We also used the six individual subtests as secondary measures of performance to identify which, if any, were also subject to any within-session practice effects.
Participants completed six consecutive trials of the JHFT with each hand. Each trial was separated by 60 to 90 s to minimize any potential fatigue. The study was counterbalanced such that 6 participants completed the six consecutive trials of the JHFT with their nondominant (left) hand and then with their dominant (right) hand 24 hr later. The remaining 6 participants completed the test in the opposite order (right hand, then left hand). This practice amount was selected on the basis of previous studies showing that neurologically intact adults appear to require five to seven trials to achieve steady-state performance on the JHFT (Boggio et al., 2006; Figure 1), although this number of trials had not yet been tested statistically.
Figure 1.
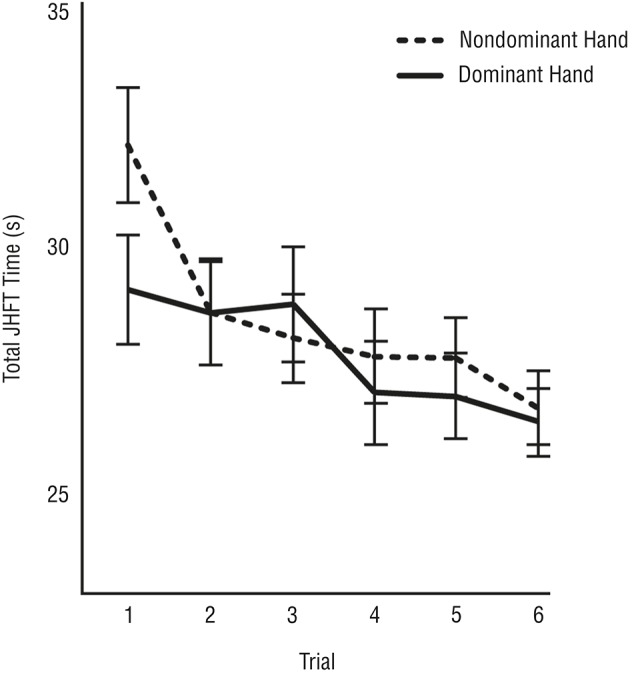
Mean ± SE total JHFT times are shown over six consecutive trials for the nondominant (dashed line) and dominant (solid lines) hands.
Note. Faster times indicate better performance. Each trial was separated by 60–90 s of rest. JHFT = Jebsen Hand Function Test; SE = standard error.
Statistical Analyses
JMP® software (Version 10; SAS Institute Inc., Cary, NC) was used for all statistical analyses (α = .05). Assumptions of normality were tested with Kolmogorov–Smirnov tests using the D statistic. We then used a 2 × 6 repeated-measures analysis of variance (ANOVA) to test for main effects of hand (left vs. right) and trial (1–6) and for any interaction between hand and trial on JHFT performance (measured in seconds). Both hand and trial were modeled as within-subject factors. Because of the participants’ right-hand proficiency on the JHFT relative to the left hand (Agnew & Maas, 1982; Jebsen et al., 1969), we were primarily concerned with any main effect of trial or a Hand × Trial interaction. The strength of any significant effect was reported using η2 values (.01–.059 = small, .06–.139 = medium, ≥.14 = large; Cohen, 1988). Post hoc analyses were conducted when warranted using Tukey’s honestly significant difference (HSD) tests.
We expected significant trial and Hand × Trial effects on total JHFT time. We also subjected data for each of the JHFT subtests (excluding writing) to the same 2 × 6 repeated-measures ANOVA to determine whether individual subtests were also susceptible to main or interaction effects with respect to trial number.
Results
Total Jebsen Hand Function Test Time
Assumptions of normality were confirmed for the total JHFT time (Kolmogorov’s D = 0.06, p = .15). Figure 1 shows the total JHFT time for the left and right hands over the course of the six trials, indicating improvements with practice for both hands. Although our ANOVA revealed no significant Hand × Trial interaction, F(5, 11) = 1.64, p = .15, there was a significant main effect of trial, as expected, F(5, 11) = 8.66, p < .0001, η2 = .13. Post hoc Tukey HSD tests indicated that by Trial 4, participants were significantly faster on the JHFT than they had been on Trial 1 (p < .001). Moreover, Trials 4–6 were not significantly different from each other (all ps > .83), thereby indicating steady-state performance across these trials. Figure 1 also illustrates the lack of any main effect of hand, F(1, 11) = 2.93, p = .09. Although participants’ left hands were slower than their right hands on the JHFT on Trial 1, any differences between hands were minimal on Trials 2–6 (see Figure 1).
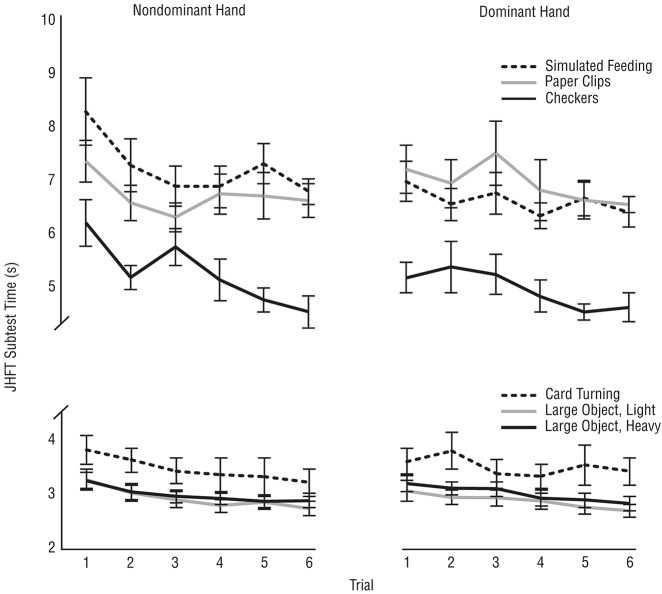
Individual Jebsen Hand Function Test Subtest Times
We also subjected the individual JHFT subtest times to our ANOVA, which further revealed no significant Hand × Trial interactions for any subtest (all Fs ≤ 1.53). There were, however, significant main effects of trial on the time to complete each subtest (Figure 2), which were small to medium in effect size: Card Turning, F(5, 11) = 2.66, p = .026, η2 = .029; Simulated Feeding, F(5, 11) = 3.00, p = .014, η2 = .064; Stacking Checkers, F(5, 11) = 4.55, p < .001, η2 = .12; Moving Light Objects, F(5, 11) = 8.55, p < .0001, η2 = .080; and Moving Heavy Objects, F(5, 11) = 7.09, p < .0001, η2 = .076.
Figure 2.
Mean ± SE times on the six JHFT subtests are shown over six consecutive trials for the nondominant and dominant hands.
Note. Faster times indicate better performance. The top panels show data for Simulated Feeding (dashed lines), Picking Up Small Common Objects (gray lines), and Stacking Checkers (black lines); the bottom panels show data for Card Turning (dashed lines), Lifting Light Objects (gray lines), and Lifting Heavy Objects (black lines). JHFT = Jebsen Hand Function Test; SE = standard error.
The only subtest that showed no significant effect of trial was Picking Up Small Common Objects, F(5, 11) = 1.42, p = .22 (see Figure 2, top panel, gray line). Although testing for main effects of hand on JHFT performance was not a primary goal of this study, we nevertheless observed no effect of hand on any of the subtests (all Fs ≤ 3.06) except for the Simulated Feeding subtest, F(1, 11) = 12.27, p < .001, η2 = .053. For that subtest, the left hand was consistently slower than the right hand, regardless of trial number (see Figure 2, top panel, dashed lines).
Discussion
The purpose of this study was to test whether the JHFT and any of its subtests are susceptible to within-session practice effects. Both the dominant (right) and nondominant (left) hands showed significant improvement across repeated administrations, as evidenced by main effects of trial on overall JHFT performance and five of the six subtests.
Note that our reported data for the first trial of the dominant (right) and nondominant (left) hands (see Figure 1, Trial 1 data) are consistent with normative data provided in previous datasets for age- and gender-matched participants (Agnew & Maas, 1982; Jebsen et al., 1969). Given that participants in this study repeated the JHFT six more times, however, their hands’ performances were no longer different and significantly improved with practice. Several other studies have already graphically displayed (but not statistically tested) within-session practice effects for only the nondominant hand on the JHFT over 10 or fewer trials (Boggio et al., 2006; Convento et al., 2014; Hummel et al., 2005), which our current data now further support statistically.
This study also supports why reports of the strength of the JHFT’s test–retest reliability have been equivocal. For example, within-session intrarater reliability for the JHFT tended to be lower than interrater reliability on a given trial in adults older than age 65 (Hackel et al., 1992), yet the test was originally reported as having no practice effect (Jebsen et al., 1969). Further work in characterizing such practice effects for the JHFT (or any other assessment) in clinical populations besides healthy young adults is therefore critical for determining its appropriateness as a postintervention outcome measure (e.g., Beekhuizen & Field-Fote, 2005; Colyer & Kappelman, 1981; Friel et al., 2016), given that the observed pre- versus posttest changes on the JHFT in these studies could be partially due to within- or between-session practice effects.
Although the presence of practice effects in a clinical test may complicate the interpretation of true change due to an intervention, these effects may also have high clinical prognostic utility as a simple, convenient, and noninvasive way to test one’s learning capacity or treatment responsiveness (Duff et al., 2007, 2012). Data have shown that persons who have larger short-term practice effects are more responsive to rehabilitation (Duff et al., 2010). We acknowledge that this brief report does not correlate the magnitude of participants’ within-session practice effect on the JHFT with any other variable, outcome, or process; however, it does provide the necessary foundational evidence that the JHFT may in fact be an easy and viable candidate for evaluating motor learning capacity. On the basis of the data presented in this study, practice effects on the full JHFT (excluding the writing subtest) can be expected in either the left or the right hand and in as few as two to five trials in healthy young adults. Our data also suggest that some JHFT subtests may be more susceptible to practice effects (Simulated Feeding) than others (Picking Up Small Common Objects).
We also acknowledge that because in this study we tested only a sample of young adults with no impairment, the generalizability of our findings may be limited; similar trends for the JHFT in older and clinical populations have, however, been reported previously. The relative homogeneity and absence of motor dysfunction presented here may in fact have been ideal for testing the JHFT’s susceptibility to practice effects. One might expect participants in this study to be highly proficient, in particular with the dominant (right) hand, and may have been subject to ceiling effects that would be resistant to the benefits of practice (Suchy et al., 2011). We nevertheless observed significant improvements with repeated practice even in this sample.
Implications for Occupational Therapy Practice
The findings of this study have the following implications for occupational therapy practice:
Repeated exposure to the JHFT significantly improves test performance in as few as four trials.
Such improvements may be considered within-session practice effects.
When used as part of an outcome measure, such effects may complicate occupational therapists’ ability to interpret whether improvements on the JHFT over time are due to the intervention or repeated testing.
Such effects may, however, also have prognostic value in quantifying one’s motor learning ability, treatment responsiveness, or both.
Acknowledgments
This work was funded in part by the National Institutes of Health (Award K01 AG047926) and the American Heart Association (Award 15SDG24970011).
Contributor Information
Sydney Y. Schaefer, Sydney Y. Schaefer, PhD, is Assistant Professor, School of Biological and Health Systems Engineering, Arizona State University, Tempe, and Adjunct Assistant Professor, Department of Physical Therapy and Athletic Training, University of Utah, Salt Lake City; sydney.schaefer@asu.edu
Ashley Saba, Ashley Saba, DPT, was Doctoral Candidate, Physical Therapy Program, Department of Exercise Science, University of South Carolina, Columbia, at the time of the study.
Jessica F. Baird, Jessica F. Baird, PhD, is Postdoctoral Fellow, Physical Therapy Program, Department of Exercise Science, University of South Carolina, Columbia, and Department of Physical Therapy, University of Alabama, Birmingham. She collaborated on this research while she was at the University of South Carolina, Columbia
Melissa B. Kolar, Melissa B. Kolar, PhD, was Doctoral Candidate, Physical Therapy Program, Department of Exercise Science, University of South Carolina, Columbia, at the time of the study
Kevin Duff, Kevin Duff, PhD, is Professor, Department of Neurology and Center for Alzheimer’s Care, Imaging, and Research, University of Utah, Salt Lake City.
Jill C. Stewart, Jill C. Stewart, PhD, PT, is Assistant Professor, Physical Therapy Program, Department of Exercise Science, University of South Carolina, Columbia
References
- Agnew P. J., & Maas F. (1982). Hand function related to age and sex. Archives of Physical Medicine and Rehabilitation, 63, 269–271. [PubMed] [Google Scholar]
- Beebe J. A., & Lang C. E. (2009). Relationships and responsiveness of six upper extremity function tests during the first six months of recovery after stroke. Journal of Neurologic Physical Therapy, 33, 96–103. https://doi.org10.1097/NPT.0b013e3181a33638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beekhuizen K. S., & Field-Fote E. C. (2005). Massed practice versus massed practice with stimulation: Effects on upper extremity function and cortical plasticity in individuals with incomplete cervical spinal cord injury. Neurorehabilitation and Neural Repair, 19, 33–45. 10.1177/1545968305274517 [DOI] [PubMed] [Google Scholar]
- Boggio P. S., Castro L. O., Savagim E. A., Braite R., Cruz V. C., Rocha R. R., … Fregni F. (2006). Enhancement of non-dominant hand motor function by anodal transcranial direct current stimulation. Neuroscience Letters, 404, 232–236. 10.1016/j.neulet.2006.05.051 [DOI] [PubMed] [Google Scholar]
- Charles J. R., & Gordon A. M. (2007). A repeated course of constraint-induced movement therapy results in further improvement. Developmental Medicine and Child Neurology, 49, 770–773. 10.1111/j.1469-8749.2007.00770.x [DOI] [PubMed] [Google Scholar]
- Cohen J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale, NJ: Erlbaum. [Google Scholar]
- Colyer R. A., & Kappelman B. (1981). Flexor pollicis longus tenodesis in tetraplegia at the sixth cervical level: A prospective evaluation of functional gain. Journal of Bone and Joint Surgery, 63, 376–379. 10.2106/00004623-198163030-00008 [DOI] [PubMed] [Google Scholar]
- Convento S., Bolognini N., Fusaro M., Lollo F., & Vallar G. (2014). Neuromodulation of parietal and motor activity affects motor planning and execution. Cortex, 57, 51–59. 10.1016/j.cortex.2014.03.006 [DOI] [PubMed] [Google Scholar]
- Duff K., Beglinger L. J., Moser D. J., Schultz S. K., & Paulsen J. S. (2010). Practice effects and outcome of cognitive training: Preliminary evidence from a memory training course. American Journal of Geriatric Psychiatry, 18, 91 10.1097/JGP.0b013e3181b7ef58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duff K., Beglinger L. J., Schultz S. K., Moser D. J., McCaffrey R. J., Haase R. F., … Paulsen J. S. (2007). Practice effects in the prediction of long-term cognitive outcome in three patient samples: A novel prognostic index. Archives of Clinical Neuropsychology, 22, 15–24. 10.1016/j.acn.2006.08.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duff K., Callister C., Dennett K., & Tometich D. (2012). Practice effects: A unique cognitive variable. Clinical Neuropsychologist, 26, 1117–1127. 10.1080/13854046.2012.722685 [DOI] [PubMed] [Google Scholar]
- Friel K. M., Kuo H. C., Fuller J., Ferre C. L., Brandao M., Carmel J. B., . . . Gordon A. M. (2016). Skilled bimanual training drives motor cortex plasticity in children with unilateral cerebral palsy. Neurorehabilitation and Neural Repair. Advance online publication. 10.1177/1545968315625838 [DOI] [PMC free article] [PubMed]
- Hackel M. E., Wolfe G. A., Bang S. M., & Canfield J. S. (1992). Changes in hand function in the aging adult as determined by the Jebsen Test of Hand Function. Physical Therapy, 72, 373–377. 10.1093/ptj/72.5.373 [DOI] [PubMed] [Google Scholar]
- Hummel F., Celnik P., Giraux P., Floel A., Wu W. H., Gerloff C., & Cohen L. G. (2005). Effects of non-invasive cortical stimulation on skilled motor function in chronic stroke. Brain, 128, 490–499. 10.1093/brain/awh369 [DOI] [PubMed] [Google Scholar]
- Jebsen R. H., Taylor N., Trieschmann R. B., Trotter M. J., & Howard L. A. (1969). An objective and standardized test of hand function. Archives of Physical Medicine and Rehabilitation, 50, 311–319. [PubMed] [Google Scholar]
- McCaffrey R. J., Duff K., & Westervelt H. J. (2000). Practitioner’s guide to evaluating change with neuropsychological assessment instruments. New York: Plenum/Kluwer. [Google Scholar]
- Oldfield R. C. (1971). The assessment and analysis of handedness: The Edinburgh Inventory. Neuropsychologia, 9, 97–113. 10.1016/0028-3932(71)90067-4 [DOI] [PubMed] [Google Scholar]
- Sears E. D., & Chung K. C. (2010). Validity and responsiveness of the Jebsen–Taylor Hand Function Test. Journal of Hand Surgery, 35, 30–37. 10.1016/j.jhsa.2009.09.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suchy Y., Kraybill M. L., & Franchow E. (2011). Practice effect and beyond: Reaction to novelty as an independent predictor of cognitive decline among older adults. Journal of the International Neuropsychological Society, 17, 101–111. 10.1017/S135561771000130X [DOI] [PubMed] [Google Scholar]