Abstract
PURPOSE
Access to a usual source of care (USC) is associated with better preventive health and chronic disease treatment. Although most older adults have a USC, loss of USC, and factors associated with loss of USC, have not previously been examined.
METHODS
We followed 7,609 participants of the National Health and Aging Trends Study annually for up to 6 years (2011–2016). Discrete time-to-event techniques and pooled logistic regression were used to identify demographic, clinical, and social factors associated with loss of USC.
RESULTS
Ninety-five percent of older adults reported having a USC in 2011, of whom 5% subsequently did not. Odds of losing a USC were higher among older adults with unmet transportation needs (adjusted odds ratio [aOR] 1.67), who moved to a new residence (aOR 2.08), and who reported depressive symptoms (aOR 1.40). Odds of losing a USC were lower for those who had ≥4 chronic conditions (vs 0–1; aOR 0.42) and with supplemental (aOR 0.52) or Medicaid (aOR 0.67) insurance coverage.
CONCLUSIONS
We identified factors associated with older adults’ loss of a USC. Potentially modifiable factors, such as access to transportation and supplemental insurance, deserve further investigation to potentially assist older adults with continuous access to care.
Key words: aging, continuity of care, access to care
INTRODUCTION
Older adults are a growing segment of the population.1 As older adults disproportionately experience chronic conditions2,3 and frequently utilize health care services, access to a usual source of medical care (USC), is particularly important in effective management of their care.4 A robust evidence base demonstrates that persons with a USC are more likely to receive appropriate chronic disease treatment5–8 and have better disease control.9–12 Having a USC has also been linked to increased receipt of preventive health services,13–16 fewer emergency department visits,17 and fewer unmet medical needs such as inability to renew needed medications.18
The overwhelming majority of Medicare beneficiaries (95.6%) report having a USC.19 Older adults without a USC tend to be younger (aged 65–74 years vs ≥75 years), male, nonwhite, Hispanic, have lower income, less educational attainment, and tend to be healthier such that they are less likely to have functional limitations or depressive symptoms.20,21 Medicare beneficiaries without supplemental insurance (17%) coverage are more than 3 times as likely to lack a USC compared with those having individually purchased (4.5%) or employee-sponsored supplemental plans (2.8%).19
Although the cross-sectional characteristics of those with and without a USC are well described, few studies have examined USC stability, especially among older adults. More than 1 in 20 older adults with a USC report having had it for less than a year,19 suggesting that instability may not be a rare occurrence. To our knowledge, the 2 studies which have examined the factors associated with loss or gain of USC have been conducted among working-age adults (aged 39–46 years)22 and children (aged <18 years).23 Both studies found that those who experienced a loss or gain of USC over the previous year were more likely to report unmet health needs. Adults with an unstable USC were more likely to be female, have lower self-rated health, and lower income.22 We are not aware of any prior studies that examined loss or gain of USC among older adults.
Older adults face circumstances that may make maintaining a relationship with a USC difficult such as declining functional status,24 transportation limitations,25 or fixed income. Therefore, we were particularly interested in factors associated with loss of a USC. The primary objective of this study is to describe the factors associated with a loss and failure to regain a USC in the previous 12 months among older adults.
METHODS
Data from interviews (rounds 1–6, 2011–2016) of the National Health and Aging Trends Study26 were used to construct a data set with individual person-period observations. The National Health and Aging Trends Study is a longitudinal nationally representative sample of Medicare beneficiaries aged 65 years and older living in the contiguous United States. The study uses a stratified 3-stage sample design with oversampling of older adults by age and Black non-Hispanic persons. In-person interviews are conducted annually with the participant or proxy if the participant is unable to respond. Detailed self-report data on chronic conditions, functional ability, health care utilization, and economic status are collected. The sample size of the original cohort in 2011 was 8,245 (70.9% response rate). Subsequent annual interviews resulted in a sample size of 7,075 (86.1% response rate) in 2012, 5,799 (88.3% response rate) in 2013, 4,737 (89.9% response rate) in 2014, 4,152 (76.8% response rate) in 2015, and 3,675 (90.6% response rate) in 2016.27 These data are publicly available, do not contain individual identifiers, and are therefore exempt from human subjects review.
Persons living in a nursing home or residential care facility in round 1 were excluded as data were only collected about the facility and no interview was conducted with sample persons who were living in the facility (n = 636). Participants who completed a round 1 interview and subsequently transitioned to a facility were included if an interview was completed in subsequent rounds.
MEASURES
USC status was determined from round 1 (baseline) survey responses to the question, “Is there a doctor that you think of as your regular doctor, that is, a doctor you usually go to when you are sick and need advice about your health?” Loss of a USC was defined as the first transition from reporting having a USC in round 1 to reporting no USC in a subsequent round.
We examined older adults’ demographic factors, health status, function, and financial and social supports. Demographic factors included respondent type (proxy vs self), sex, age, race/ethnicity, marital status, type of residence, educational attainment, current census division, and whether the participant reported moving to a new residence since the last round. Health status indicators included self-rated health and hospitalization in the last 12 months. We categorized depressive symptoms using previously established cut points for responses to the PHQ-2.28 Presence of chronic conditions was determined using self-report of a physician’s diagnosis of heart attack, heart disease, high blood pressure, arthritis, osteoporosis, diabetes, lung disease, stroke, dementia or Alzheimer’s disease, or cancer. Functional status was determined by a report of help needed with self-care activities in the last 12 months. Report of any fall in the last 12 months was also recorded. Income quartiles were constructed using the first round assignment of income.29 A composite measure of supplemental insurance coverage was created based on report of either supplemental (Medi-gap) or drug coverage. Medicaid coverage was noted separately. Presence of a transportation barrier is a composite measure of participant’s response of yes to any of the following: “In the past month, did a transportation problem ever keep you from (visiting friends and family, attending religious services, participating in clubs, classes, or other organized activities, or going out for enjoyment).” As item nonresponse was limited, ranging from 0% to 5%, with most variables at <1%, we assigned missing values the modal value.
Statistical Analysis
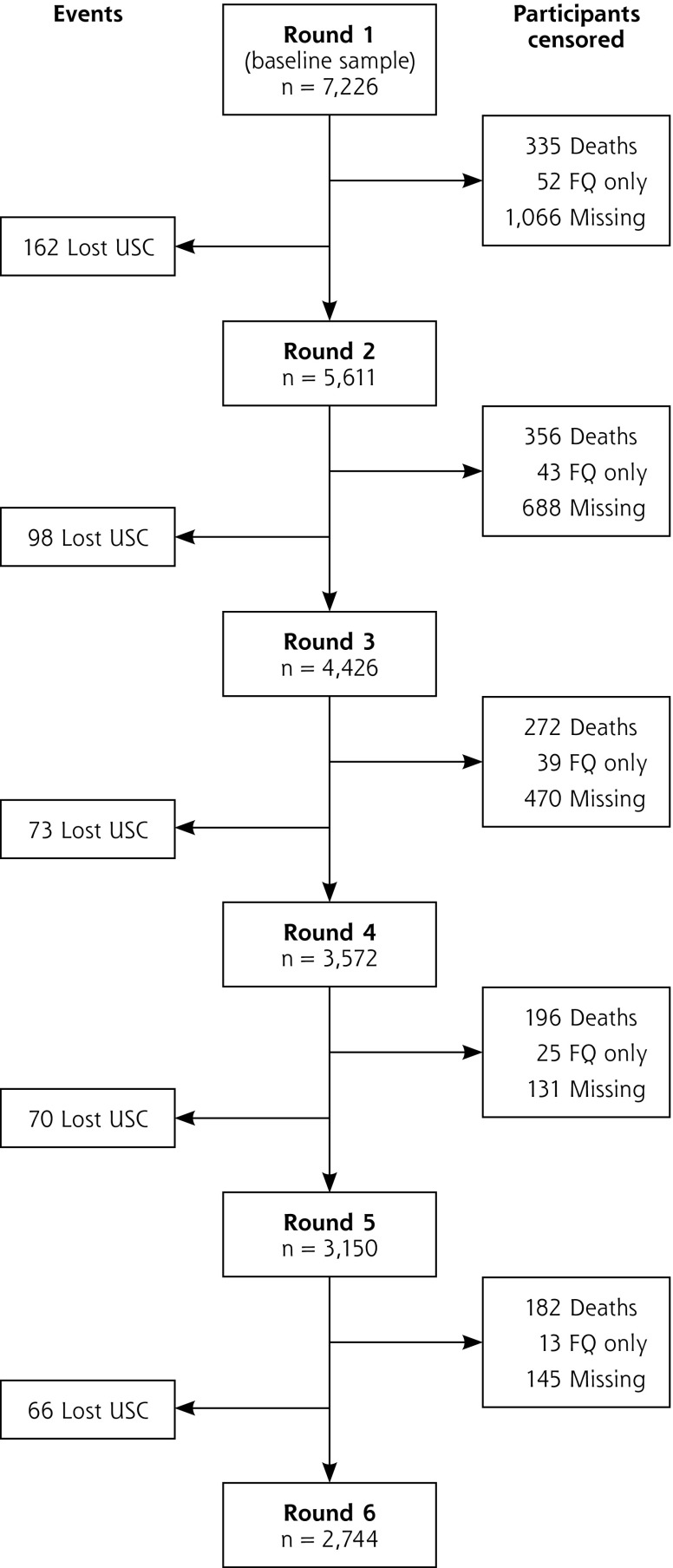
Participants who reported having a USC in round 1 (n = 7,226) were followed to identify whether they subsequently reported no USC (n = 469) (Figure 1). As we were interested in loss of USC status, the unit of analysis was the transition from one round to the next for each person-period. In this format, each participant could contribute up to 5 observations. Participants entered the study at round 1 and were followed until they experienced 1 of the following events: loss of USC, death, loss to follow-up, or study period completion (round 6), whichever occurred first.
Figure 1.
Participant flow diagram: loss of usual source of care.
FQ = Facility questionnaire only, no participant interview; USC = Usual source of care
We first examined the National Health and Aging Trends Study sample by baseline report of USC using descriptive statistics, comparing group differences using X2 analyses. We then used multivariable pooled logistic regression to examine which demographic, clinical, and social factors are associated with a loss of USC. Pooled logistic regression is considered equivalent to Cox proportional hazards models when the outcome is uncommon30 and is intended for data collected at discrete time intervals.31
We also conducted a sensitivity analyses in which we removed individuals who reported living in residential care or a nursing home to assess the sensitivity of results to differential loss to follow-up.
All analyses were conducted in Stata version 14 (StataCorp LLC) using the svy commands and weights to account for the complex sampling strategy and to produce population estimates.
RESULTS
A total of 7,609 participants at round 1 responded to the interview, of whom 383 (5%) reported no USC and were excluded. Those who did and did not report a USC were significantly different in several regards (Supplemental Table 1, available at http://www.annfammed.org/content/16/6/538/suppl/DC1/). Older adults without a USC were more likely to be male, younger, unmarried, and to have lower income. Those without a USC also reported better health, were less likely to have 1 or more chronic conditions, and tended to lack self-care help.
Loss of USC
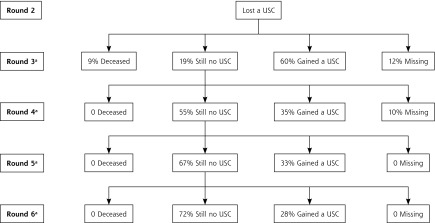
Among the 7,226 participants who reported a USC at baseline, a total of 469 reported loss of USC. Details by round are shown in Figure 1. Those who did and did not lose a USC during the study had different baseline characteristics (Table 1). Most of the individuals who reported loss of a USC in round 2 re-gained a USC by the next round (60%); however, with subsequent rounds individuals who remained without a USC were more likely to continue to report no USC (Figure 2).
Table 1.
Round 1 Characteristics of Older Adults Who Did and Did Not Lose a USC Over 6 Yearsa,b,c
| Characteristic | Unweighted PopulationPercentages (n=7,226) | Weighted Population Estimates (n =35,305,631)d | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Lost USC, No. (%) | Retained USC, No. (%) | P Value | Lost USC, % | Retained USC, % | P Value | |
| Male | 186 (46) | 2,791 (41) | .04 | 48 | 43 | .14 |
| Age, y | ||||||
| 65–74 | 169 (42) | 2,640 (39) | .29 | 57 | 52 | .16 |
| 75–84 | 147 (37) | 2,750 (40) | 29 | 34 | ||
| ≥85 | 87 (21) | 1,433 (21) | 14 | 13 | ||
| Race/Ethnicityd | ||||||
| White, non-Hispanic | 249 (62) | 4,769 (70) | .001 | 77 | 82 | .05 |
| Nonwhite, non-Hispanic | 118 (29) | 1,658 (24) | 12 | 11 | ||
| Hispanic | 396 (6) | 36 (9) | 10 | 7 | ||
| Marital status | ||||||
| Married or with partner | 175 (43) | 3,463 (51) | .004 | 49 | 58 | .008 |
| Divorced, widowed, separated | 228 (57) | 3,360 (49) | 51 | 42 | ||
| Type of residence | ||||||
| Community | 374 (93) | 6,467 (95) | .09 | 90 | 95 | .005 |
| Residential care | 29 (7) | 356 (5) | 10 | 5 | ||
| Education | ||||||
| Less than high school diploma | 126 (31) | 1,799 (26) | .03 | 24 | 21 | .27 |
| More than high school diploma | 277 (69) | 5,024 (74) | 76 | 79 | ||
| Census division | ||||||
| Northeast | 73 (18) | 1,283 (19) | .82 | 17 | 20 | .56 |
| Midwest | 97 (24) | 1,587 (23) | 22 | 23 | ||
| South | 150 (37) | 2,652 (39) | 38 | 37 | ||
| West | 83 (21) | 1,301 (19) | 24 | 20 | ||
| Self-Rated health | ||||||
| Excellent/Very good | 160 (40) | 2,267 (39) | .83 | 43 | 44 | .93 |
| Good | 130 (32) | 2,197 (32) | 32 | 31 | ||
| Fair/Poor | 113 (28) | 2,002 (29) | 25 | 25 | ||
| Fallen in last year | 128 (32) | 2,146 (31) | .90 | 34 | 30 | .20 |
| Depressive symptoms | 74 (18) | 1,087 (16) | .20 | 17 | 14 | .17 |
| Number of chronic conditionsd | ||||||
| 0–1 | 127 (32) | 1,634 (24) | .001 | 32 | 27 | .09 |
| 2 | 103 (26) | 1,712 (25) | 26 | 25 | ||
| 3 | 93 (23) | 1,590 (23) | 22 | 22 | ||
| ≥4 | 80 (20) | 1,887 (28) | 20 | 25 | ||
| Admitted to hospital in last year | 98 (24) | 1,621 (24) | .80 | 23 | 21 | .48 |
| Needed self-care help in last year | 69 (17) | 1,307 (19) | .31 | 16 | 16 | .81 |
| Has a transportation barrier | 43 (11) | 518 (8) | .03 | 8 | 6 | .03 |
| Insurancee | ||||||
| Supplemental or drug | 380 (94) | 6,562 (96) | .06 | 94 | 96 | .11 |
| Medicaid | 74 (18) | 1,036 (15) | 12 | 12 | .93 | |
| Income quartile, $ | ||||||
| 1 (<13,000) | 118 (29) | 1,709 (25) | .001 | 24 | 20 | .003 |
| 2 (13,001–25,000) | 125 (31) | 1,701 (25) | 29 | 23 | ||
| 3 (25,001–50,000) | 87 (22) | 1,776 (26) | 24 | 28 | ||
| 4 (>50,000) | 73 (18) | 1,637 (24) | 23 | 30 | ||
USC = usual source of care.
Note: Source: the 2011–2016 National Health and Aging Trends Study.26 Estimates have been weighted to reflect survey design.
Includes community dwelling (n = 7,197) and residential care participants (n = 412) who completed a sample person interview. Excludes participants in residential care (n = 168) and participants in nursing home (n = 468) who did not complete a sample person interview.
Only 583 participants (8%) required a proxy to complete the interview. There was no significant difference in respondent type (P=.61) between those who did and did not lose a usual source of care.
For time-varying covariates, characteristics are reflective of baseline, round 1 (2011) responses rather than responses at the time of loss of USC.
Percentages may not sum to 100% due to rounding.
Insurance categories are not mutually exclusive, percentages will not sum to 100%.
Figure 2.
Population estimates for longitudinal follow-up of individuals who lost a USC in round 2.
USC = usual source of care.
aPercentages at each round represent the number of people in each category (deceased, still no USC, gained a USC, missing) in that round divided by the number of people who reported a loss of USC in the previous round.
The odds of loosing a USC (in adjusted analyses) (Table 2) during the study period were significantly greater for older adults of Hispanic ethnicity (adjusted odds ratio [aOR] 1.96), who were male (aOR 1.45), reported living in a residential care facility (aOR 1.94) or nursing home (aOR 6.41), had moved to a new residence since the previous interview (aOR 2.08), reported having depressive symptoms (aOR 1.40) or a transportation barrier (aOR 1.67). The likelihood of losing a USC was significantly lower for older adults who had 4 or more chronic conditions (vs 0–1; aOR 0.42) or reported a fall (aOR 0.77). Odds of losing a USC were also lower for those in the highest income quartile (vs quartile 1; aOR 0.66), who had supplemental (aOR 0.52) or Medicaid (aOR 0.67) coverage in addition to Medicare. Results were largely unchanged in our sensitivity analysis, which excluded participants who were residents of a nursing home or residential care facility at any point in the study (n = 819) (Supplemental Table 2, available at http://www.annfammed.org/content/16/6/538/suppl/DC1/).
Table 2.
Weighted aOR of Factors Associated With Loss of USC
| Adjusted OR (95% CI) | P Value | |
|---|---|---|
| Male | 1.45 (1.08–1.93) | .01 |
| Age, y | ||
| 65–74 | ref | – |
| 75–84 | 0.82 (0.64–1.03) | .09 |
| >85 | 0.77 (0.56–1.08) | .13 |
| Race/Ethnicity | ||
| White, non-Hispanic | ref | – |
| Nonwhite, non-Hispanic | 1.15 (0.91–1.45) | .24 |
| Hispanic | 1.96 (1.30–2.97) | .002 |
| Married or with a partner | 0.75 (0.56–1.01) | .06 |
| Residence | ||
| Community | ref | – |
| Residential care | 1.94 (1.24–3.05) | .005 |
| Nursing home | 6.41 (3.20–12.83) | <.001 |
| Proxy respondent | 1.48 (0.97–2.25) | .07 |
| More than high school diploma | 0.99 (0.78–1.27) | .94 |
| Census division | ||
| Northeast | ref | – |
| Midwest | 1.11 (0.73–1.70) | .62 |
| South | 1.22 (0.91–1.62) | .17 |
| West | 1.26 (0.89–1.79) | .19 |
| Self-Rated health | ||
| Excellent/Very Good | ref | – |
| Good | 0.83 (0.63–1.09) | .01 |
| Fair/Poor | 1.22 (0.80–1.85) | .34 |
| Fallen in last year | 0.77 (0.60–0.99) | .05 |
| Depressive symptoms | 1.40 (1.04–1.89) | .03 |
| Number of chronic conditions | ||
| 0–1 | ref | – |
| 2 | 0.82 (0.64–1.05) | .12 |
| 3 | 0.75 (0.57–0.98) | .04 |
| ≥4 | 0.42 (0.31–0.59) | <.001 |
| Admitted to hospital in last year | 1.08 (0.86–1.35) | .50 |
| Moved to a new residence | 2.08 (1.35–3.21) | .001 |
| Needs self-care help | 0.93 (0.71–1.22) | .60 |
| Has a transportation barrier | 1.67 (1.16–2.39) | .006 |
| Insurance | ||
| Supplemental or drug | 0.52 (0.34–0.80) | .004 |
| Medicaid | 0.67 (0.47–0.94) | .02 |
| Income quartile, $ | ||
| 1 (<13,000) | ref | – |
| 2 (13,001–25,000) | 1.12 (0.80–1.57) | .49 |
| 3 (25,001–50,000) | 0.82 (0.58–1.17) | .27 |
| 4 (>50,000) | 0.66 (0.44–0.99) | .05 |
USC = usual source of care; aOR = adjusted odds ratio.
Note: Source: the 2011–2016 National Health and Aging Trends Study.26 Estimates have been weighted to reflect survey design.
DISCUSSION
This is the first national study to examine factors associated with loss of USC among older adults, a fast-growing segment of the population.1 Our results suggest that clinical as well as social factors are important in an older adult’s ability to maintain a stable relationship with a provider over time.
Previous studies on loss of USC created composite outcomes which include both gaining and losing a USC.22,23 It seems plausible, however, that the factors associated with losing a USC might differ from those associated with gaining a USC. As most older adults in the United States have a USC, more individuals are at risk of loss than gain of USC in this population. Thus, we sought to examine factors involved in the pathway associated with losses of USC.
Some of the factors which were found to be significantly associated with losing a USC such as male sex, Hispanic ethnicity,19 and depressive symptoms20 have been associated with lack of a USC in cross-sectional studies. Similarly, lack of transportation has been identified as a barrier to accessing care among older32,33 and younger adults in cross sectional studies.34 Our findings extend this work by indicating that demographic and health factors are longitudinally associated with USC loss. This contribution is valuable because we examined individuals who were engaged in care but then lose a USC, while cross-sectional studies also capture those who continuously have no USC. The latter group may have chosen to not engage in care, rather than encountering an obstacle that made maintaining this relationship difficult.
Lack of insurance coverage has been repeatedly associated with decreased report of USC,5,18,22,35,36 including changes in USC due to changes in insurance coverage.22,36 The association between moving to a new address and increased odds of losing a USC makes intuitive sense; it may take some time after moving to a new area to find a new source of primary care. There is relatively little data on this topic, however, outside of the pediatric literature.37 The association between a higher number of chronic conditions or having fallen and lower odds of losing a USC are consistent with the notion that persons with multiple chronic conditions and functional impairment are more likely to utilize health care, potentially spurred by the symptoms associated with these conditions.38,39 In contrast, presence of depressive symptoms may decrease motivation to access care, potentially explaining the increased odds of losing a USC observed for those with depressive symptoms.
Many of the factors that were significantly associated with loss of a USC in the adjusted model, including number of chronic conditions, falls, depressive symptoms, and insurance status, were not significant in the unadjusted analysis of baseline characteristics (Tables 1 and 2). The response to interview questions associated with these variables may have changed with time and thus, a characteristic like falls or insurance status at the baseline interview may not be reflective of the response associated with losing a USC years later.
The association between living in a residential care or nursing facility and losing a USC warrants further investigation. Participants in the nursing facility who were previously in the community may have responded that they do not have a USC as the question asks about a doctor the participant “goes to” while nursing facilities usually provide on-site physician visits. Residential facilities, however, unlike nursing facilities, do not face federal requirements regarding routine visits from a physician,40 so continuing primary care for those in a residential facility largely resembles that of community dwelling older adults.41 The majority of those who report losing a USC and reside in a residential care facility were living in a residential facility in the prior round (data not shown), suggesting that perhaps with time, it has become difficult to travel to office visits or their primary clinician no longer follows patients in such facilities.41
Some participants who transitioned to a nursing or residential facility were excluded from the analysis due to failure to complete a participant interview (n = 172) (Figure 1). The aOR associated with nursing home residence had a particularly high point estimate (aOR 6.47) and was associated with a wide CI (4.46–10.85) reflective of the fact that such a transition is a relatively rare event. Removing this population from our analysis did not significantly change our findings (Supplemental Table 2, available at http://www.annfammed.org/content/16/6/538/suppl/DC1/).
Several limitations of this study should be considered. First, self-report of USC is a proxy for, rather than true measurement of, an individual’s actual access to primary care. USC is a widely used and important surrogate for access to care, however, and has been tied to a number of important outcomes. There was notable attrition of participants over the 5 years of follow-up (n = 2,500) (Figure 1). We conducted analyses of baseline characteristics of those who were and were not lost to follow-up during the study. Characteristics associated with loss to follow-up were largely similar to characteristics associated with loss of USC, meaning our results may underestimate the frequency of loss of USC and the strength of the association between some variables and loss of USC, such as race and ethnicity (Supplemental Table 3, available at http://www.annfammed.org/content/16/6/538/suppl/DC1/). Additionally, although we used multiple rounds of data, participants were interviewed yearly which limited our ability to capture the fluidity of loss in USC status; meaning our results may be better described as loss and failure to regain a USC in a timely manner than as loss of a USC. However, the annual interview construct does allow for plausible shifts in response to changes in enrollment in health insurance. Finally, our study is limited to assessing factors associated with an initial loss of USC rather than transitions between USC statuses.
Our study illustrates the importance of considering how changes in access to health insurance, transportation, or residence can have important implications for older adults’ ability to maintain a USC. Future work is needed to assess how changes in these factors affect older adults’ ability to experience a continuous source of care and the impact of that continuity on functional decline and hospital admissions.
Footnotes
Conflicts of interest: authors report none.
To read or post commentaries in response to this article, see it online at http://www.AnnFamMed.org/content/16/6/538.
Previous presentations: A previous version of the analysis in this manuscript was presented at the American Geriatrics Society Annual Meeting; May 18-20, 2017; San Antonio, Texas.
Supplemental Materials: Available at http://www.AnnFamMed.org/content/16/6/538/suppl/DC1/.
Funding support: This study was supported by the Health Services and Research Association grants T32HP10025B0 & U1QHP2870 (SN) and NIA 1K24AG056578-01 (CB).
References
- 1.Ortman JM, Velkoff VA, Hogan H. An aging nation: the older population in the United States. US Department of Commerce web site; https://www.census.gov/prod/2014pubs/p25-1140.pdf. Published May 2014. [Google Scholar]
- 2.Wolff JL, Starfield B, Anderson G. Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Arch Intern Med. 2002; 162(20): 2269–2276. [DOI] [PubMed] [Google Scholar]
- 3.Vogeli C, Shields AE, Lee TA, et al. Multiple chronic conditions: prevalence, health consequences, and implications for quality, care management, and costs. J Gen Intern Med. 2007; 22 Suppl 3(Suppl 3): 391–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005; 83(3): 457–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Spatz ES, Ross JS, Desai MM, Canavan ME, Krumholz HM. Beyond insurance coverage: usual source of care in the treatment of hypertension and hypercholesterolemia. Data from the 2003–2006 National Health and Nutrition Examination Survey. Am Heart J. 2010; 160(1): 115–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moy E, Bartman BA, Weir MR. Access to hypertensive care. Effects of income, insurance, and source of care. Arch Intern Med. 1995; 155(14): 1497–1502. [PubMed] [Google Scholar]
- 7.Halm EA, Wisnivesky JP, Leventhal H. Quality and access to care among a cohort of inner-city adults with asthma: who gets guideline concordant care? Chest. 2005; 128(4): 1943–1950. [DOI] [PubMed] [Google Scholar]
- 8.Winters P, Tancredi D, Fiscella K. The role of usual source of care in cholesterol treatment. J Am Board Fam Med. 2010; 23(2): 179–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dinkler JM, Sugar CA, Escarce JJ, Ong MK, Mangione CM. Does age matter? Association between usual source of care and hypertension control in the US population: data from NHANES 2007–2012. Am J Hypertens. 2016; 29(8): 934–940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ahluwalia JS, McNagny SE, Rask KJ. Correlates of controlled hypertension in indigent, inner-city hypertensive patients. J Gen Intern Med. 1997; 12(1): 7–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.He J, Muntner P, Chen J, Roccella EJ, Streiffer RH, Whelton PK. Factors associated with hypertension control in the general population of the United States. Arch Intern Med. 2002; 162(9): 1051–1058. [DOI] [PubMed] [Google Scholar]
- 12.Rhee MK, Cook CB, Dunbar VG, et al. Limited health care access impairs glycemic control in low income urban African Americans with type 2 diabetes. J Health Care Poor Underserved. 2005; 16(4): 734–746. [DOI] [PubMed] [Google Scholar]
- 13.DeVoe JE, Fryer GE, Phillips R, Green L. Receipt of preventive care among adults: insurance status and usual source of care. Am J Public Health. 2003; 93(5): 786–791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bindman AB, Grumbach K, Osmond D, Vranizan K, Stewart AL. Primary care and receipt of preventive services. J Gen Intern Med. 1996; 11(5): 269–276. [DOI] [PubMed] [Google Scholar]
- 15.Blewett LA, Johnson PJ, Lee B, Scal PB. When a usual source of care and usual provider matter: adult prevention and screening services. J Gen Intern Med. 2008; 23(9): 1354–1360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Doescher MP, Saver BG, Fiscella K, Franks P. Preventive care. J Gen Intern Med. 2004; 19(6): 632–637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Petterson SM, Rabin D, Phillips RL, Jr, Bazemore AW, Dodoo MS. Having a usual source of care reduces ED visits. Am Fam Physician. 2009; 79(2): 94–95. [PubMed] [Google Scholar]
- 18.DeVoe JE, Tillotson CJ, Lesko SE, Wallace LS, Angier H. The case for synergy between a usual source of care and health insurance coverage. J Gen Intern Med. 2011; 26(9): 1059–1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Centers for Medicare and Medicaid Services. Data table section 5: what is the Medicare population’s access to care and how satisfied are they with their care? In: The Characteristics and Perceptions of the Medicare Population. Baltimore, MD: Centers for Medicare and Medicaid Services; 2013. [Google Scholar]
- 20.Ewald E, Loganathan S, Hasche J, Lochner K, Centers for Medicare and Medicaid Services Access to care among Medicare beneficiaries with and without depression. https://www.cms.gov/Research-Statistics-Data-and-Systems/Research/MCBS/Downloads/ATC_Depression_2017.pdf. Published Jun 2017.
- 21.Li C, Dick AW, Fiscella K, Conwell Y, Friedman B. Effect of usual source of care on depression among Medicare beneficiaries: an application of a simultaneous-equations model. Health Serv Res. 2011; 46(4): 1059–1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Smith MA, Bartell JM. Changes in usual source of care and perceptions of health care access, quality, and use. Med Care. 2004; 42(10): 975–984. [DOI] [PubMed] [Google Scholar]
- 23.DeVoe JE, Saultz JW, Krois L, Tillotson CJ. A medical home versus temporary housing: the importance of a stable usual source of care. Pediatrics. 2009; 124(5): 1363–1371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Freedman VA, Spillman BC. Disability and care needs among older Americans. Milbank Q. 2014; 92(3): 509–541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Anstey KJ, Wood J, Lord S, Walker JG. Cognitive, sensory and physical factors enabling driving safety in older adults. Clin Psychol Rev. 2005; 25(1): 45–65. [DOI] [PubMed] [Google Scholar]
- 26.National Health and Aging Trends Study. https://www.nhats.org/scripts/aboutNHATS.htm. Updated Jun 19, 2018.
- 27.Kasper JD, Freedman VA, Kalton G, et al. National Health and Aging Trends Study (NHATS) User Guide Rounds 1–6 Final Release. Baltimore, Maryland: Johns Hopkins University School of Public Health; 2017. https://www.nhats.org/scripts/documents/NHATS_User_Guide_R1_R6_2017_Revised_12_12_17.pdf. [Google Scholar]
- 28.Löwe B, Kroenke K, Gräfe K. Detecting and monitoring depression with a two-item questionnaire (PHQ-2). J Psychosom Res. 2005; 58(2): 163–171. [DOI] [PubMed] [Google Scholar]
- 29.Montaquila J, Freedman VA, Edwards B, Kasper JD. National Health and Aging Trends Study Round 1 Sample Design and Selection. Baltimore, Maryland: Johns Hopkins University School of Public Health; 2012. https://www.nhats.org/scripts/sampling/NHATS%20Round%201%20Sample%20Design%2005_10_12.pdf. [Google Scholar]
- 30.D’Agostino RB, Lee M-L, Belanger AJ, Cupples LA, Anderson K, Kannel WB. Relation of pooled logistic regression to time dependent Cox regression analysis: the Framingham Heart Study. Stat Med. 1990; 9(12): 1501–1515. [DOI] [PubMed] [Google Scholar]
- 31.Singer JB, Willett JB. It’s about time: using discrete-time survival analysis to study duration and the timing of events. Educ Res. 1993; 18(2): 155–195. [Google Scholar]
- 32.Okoro CA, Strine TW, Young SL, Balluz LS, Mokdad AH. Access to health care among older adults and receipt of preventive services. Results from the Behavioral Risk Factor Surveillance System, 2002. Prev Med. 2005; 40(3): 337–343. [DOI] [PubMed] [Google Scholar]
- 33.Goins RT, Williams KA, Carter MW, Spencer M, Solovieva T. Perceived barriers to health care access among rural older adults: a qualitative study. J Rural Health. 2005; 21(3): 206–213. [DOI] [PubMed] [Google Scholar]
- 34.Rust G, Ye J, Baltrus P, Daniels E, Adesunloye B, Fryer GE. Practical barriers to timely primary care access: impact on adult use of emergency department services. Arch Intern Med. 2008; 168(15): 1705–1710. [DOI] [PubMed] [Google Scholar]
- 35.DeVoe JE, Petering R, Krois L. A usual source of care: supplement or substitute for health insurance among low-income children? Med Care. 2008; 46(10): 1041–1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kasper JD, Giovannini TA, Hoffman C. Gaining and losing health insurance: strengthening the evidence for effects on access to care and health outcomes. Med Care Res Rev. 2000; 57(3): 298–318, discussion 319–325. [DOI] [PubMed] [Google Scholar]
- 37.Jelleyman T, Spencer N. Residential mobility in childhood and health outcomes: a systematic review. J Epidemiol Community Health. 2008; 62(7): 584–592. [DOI] [PubMed] [Google Scholar]
- 38.Min L, Wenger N, Walling AM, et al. When comorbidity, aging, and complexity of primary care meet: development and validation of the Geriatric CompleXity of Care Index. J Am Geriatr Soc. 2013; 61(4): 542–550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Koroukian SM, Schiltz N, Warner DF, et al. Combinations of chronic conditions, functional limitations, and geriatric syndromes that predict health outcomes. J Gen Intern Med. 2016; 31(6): 630–637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Carder P, O’Keefe J, O’Keefe C, Office of the Assistant Secretary for Planning and Evaluation Compendium of residential care and assisted living regulations and policy: 2015 edition. https://aspe.hhs.gov/basic-report/compendium-residential-care-and-assisted-living-regulations-and-policy-2015-edition. Published Jun 15, 2015 Accessed Oct 31, 2017.
- 41.Kane RL, Mach JR. Improving health care for assisted living residents. Gerontologist. 2007; 47(supp 1): 100–109. [DOI] [PubMed] [Google Scholar]