Abstract
AIM
To describe the histopathologic and clinical features of eyelid tumor cases from Tianjin Eye Hospital during 2002 to 2015.
METHODS
In this retrospective study, a total of 2228 cases of eyelid tumors with pathologic diagnoses were enrolled. The eyelid tumors were classified into three groups according to tumor origin: epidermal, adnexal and miscellaneous, including melanocytic, neural and vascular lesions. Inflammatory tumor-like lesions were excluded. The clinical characteristics of the eyelid tumors were analyzed, including age, gender and lesion location.
RESULTS
Most eyelid tumors were epidermal in origin (1080, 48.5%), followed by miscellaneous (885, 39.7%) and adnexal tumors (263, 11.8%). Among all the tumors, 292 (13.1%) were malignant lesions, 1910 (85.7%) benign and 26 (1.1%) premalignant lesions. Most malignant tumors originated from epidermal cells (60.0%), followed by adnexal cells (34.6%). The most common malignant tumors were basal cell carcinomas (56.5%) followed by sebaceous carcinoma (34.6%), squamous cell carcinomas (3.8%) and lymphoma/plasmocytoma (1.7%). The benign and premalignant eyelid lesions mostly originated from epidermal cells (46.4%) followed by miscellaneous cell sources (45.2%), including melanocytic nevus (33.8%), seborrheic keratosis (13.7%), squamous cell papilloma (13.0%) and epidermal cysts (11.5%).
CONCLUSION
Eyelid tumors are mostly epithelial in origin. Benign tumors are significantly more common than malignant tumors with an obvious female predominance, and the most frequent malignant tumor are basal cell carcinoma, sebaceous carcinoma and squamous cell carcinomas. The tumor clinical features varied among the different subtypes.
Keywords: eyelid tumors, benign tumors, malignant tumor, basal cell carcinoma, sebaceous carcinoma, squamous cell carcinoma, melanocytic nevus
INTRODUCTION
Eyelid tumors are the major neoplasms encountered in clinical ophthalmology practice. Because the eyelids contain numerous histological elements, a variety of benign and malignant tumors can originate in this location. Approximately 5%-10% of all skin cancers and 15% of all face tumors occur on the eyelid[1]. In addition, other studies have revealed the rapidly increasing incidences of skin cancer and even malignant eyelid tumors[2]–[3]. Understanding the clinical and histopathologic characteristics of eyelid tumors will benefit early diagnosis of eyelid tumors and protect patients from suffering.
However, the clinical features, prevalence and outcome of various eyelid tumor subtypes vary significantly, which can be attributed to the different geographic location, genetic background, socio-economic status, and healthcare policies, among other factors, for the affected patients[1]. Eyelid tumors are cosmetically disturbing to patients and ophthalmologists, who diagnose eyelid tumors based on biopsy. In addition to aesthetic issues, the tumors can affect the normal visual acuity and can change the shape of the eyelids[3].
Although some previous studies stressed the relative frequencies of benign and malignant eyelid tumors, the histological classification of eyelid tumors has been gradually refined[1],[4]. An updated histological classification system based on histologic origin and correlation with clinical features is necessary for eyelid tumors.
Therefore, we aimed to explore and analyze recent data on the relative frequency and clinical features of eyelid tumors from Tianjin Eye Hospital based on the updated histological classification system.
SUBJECTS AND METHODS
We retrospectively analyzed the medical records of patients who had histopathological reports of eyelid tumors that were surgically removed at the Tianjin Eye Hospital during 2002-2015, and 2228 cases of eyelid tumors were included. Before surgery, ophthalmologist gave a brief introduction of the surgery, also explained the aims of the data collection, then the written inform consent was collected. The collected data included age, gender, lesion location, clinical diagnosis and eyelid tumor classification. All the tumors were fixed in the 4% paraformaldehyde (PFA), then embedded in the paraffin. Hematoxyline eosin (H&E) staining was done with paraffin section in pathological lab in Tianjin Eye Hospital Department of Pathology. The eyelid tumor classification was performed using a previous large study by Deprez et al and Gundogan et al, which was based on the 1994 edition of the AFIP atlas of tumor pathology with references to the revised 2006 edition and other sources of skin and eyelid tumor classification. According to this classification scheme, eyelid tumors were summarized into three major kinds, including epidermal, adnexal and miscellaneous such as melanocytic, vascular, neural crest, or lymphoid/ metastatic tumors[5]–[6]. The study was conducted according to the Declaration of Helsinki principles.
RESULTS
A total of 2228 histologically confirmed eyelid tumors diagnosed within the past 14y were included in our study. Among these cases, 832 were males (37.3%) and 1396 were females (62.7%). The patient ages ranged from 1 to 98y, and the mean age was 51.16±15.4y.
Of all the cases, most eyelid tumors were epidermal in origin (1080, 48.5%), followed by miscellaneous (885, 39.7%) and adnexal tumors (263, 11.8%). There was an obvious female predominance among the three kinds of tumors; the female/male ratios were 1.0/1, 3.5/1 and 1.5/1 for the epidermal, miscellaneous and adnexal tumors, respectively, except for the malignant tumors that originated from epidermal cells (0.9/1) and the lymphoid and metastatic tumors (0.7/1). The epidermal and adnexal tumors tended to be located on the lower eyelid, where as the miscellaneous tumors were preferentially located on the upper eyelid (0.9/1, 0.7/1 and 1.5/1 for the upper/lower eyelid ratios, respectively).
In another analysis of all included cases, there were 292 (13.1%) malignant lesions, 1910 (85.7%) benign and 26 (1.1%) premalignant lesions. The mean age at diagnosis was 49.7y for patients with benign lesions and 63.5y for patients with malignant lesions. The malignant lesions were preferentially located on the lower eyelid and the benign lesions on the upper eyelid (0.7/1 and 1.1/1 for the upper/lower eyelid ratios for malignant and benign tumors, respectively), as shown in Tables 1 and 2.
Table 1. Histopathological classification and clinic features of the benign tumors.
| Type of benign tumor | Cases | All benign tumor (%) | Subtype tumor (%) | All tumor (%) | Mean age (range), y | Sex (F/M) | Location (U/L) |
| Tumors of the epidermis (900, 46.4%) | |||||||
| Benign tumors and cysts | 874 | 45.1 | 80.9 | 39.1 | 51 (1-86) | 1.1/1 | 1.1/1 |
| Premalignant tumors | 26 | 1.3 | 2.4 | 1.1 | 59 (26-75) | 1.6/1 | 0.9/1 |
| Adnexal tumors (162, 8.4%) | |||||||
| Hair follicle tumors | 127 | 6.6 | 48.3 | 5.7 | 49.8 (1-84) | 1.2/1 | 0.2/1 |
| Sebaceous gland tumors | 22 | 1.1 | 8.4 | 1.0 | 57 (7-83) | 1.2/1 | 1.2/1 |
| Tumors of eccrine and apocrine gland origin | 13 | 0.7 | 4.9 | 0.6 | 47 (9-72) | 3.3/1 | 0.9/1 |
| Miscellaneous tumors (874, 45.2%) | |||||||
| Melanocytic tumors | 671 | 34.7 | 75.8 | 30.1 | 33 (12-89) | 4.9/1 | 1.3/1 |
| Vascular tumors | 112 | 5.8 | 12.7 | 5.0 | 43.7 (3-79) | 1.3/1 | 1.8/1 |
| Other | 77 | 4 | 8.8 | 3.5 | 51.8 (28-74) | 2.3/1 | 5.4/1 |
| Tumors of neural crest origin | 14 | 0.7 | 1.5 | 0.6 | 42.8 (7-71) | 1.3/1 | 1.3/1 |
F/M: Female/male; U/L: Upper/lower eyelid.
Table 2. Histopathological classification and clinic features of the malignant tumor.
| Type of malignant tumor | Cases | All malignant tumor (%) | Subtype tumor (%) | All tumor (%) | Mean age (range), y | Sex (F/M) | Location (U/L) |
| Tumors of the epidermis (180, 61.7%) | |||||||
| Basal cell carcinoma | 165 | 56.5 | 15.3 | 7.4 | 63 (12-85) | 0.9/1 | 0.3/1 |
| Squamous cell carcinoma | 11 | 3.8 | 1 | 0.5 | 58 (40-80) | 1.2/1 | 1.8/1 |
| Papillary squamous cell carcinoma | 2 | 0.7 | 0.2 | 0.09 | 65 (54-76) | 1/1 | 1/1 |
| Basosquamous carcinoma | 2 | 0.7 | 0.2 | 0.09 | 53 (49-57) | 0/2 | 1/1 |
| Adnexal tumors (101, 34.6%) | |||||||
| Sebaceous gland carcinoma | 101 | 34.6 | 38.4 | 4.5 | 60 (20-98) | 1.9/1 | 2.1/1 |
| Miscellaneous tumors (11, 3.8%) | |||||||
| Lymphoid and metastatic tumors | 5 | 1.7 | 0.6 | 0.2 | 61 (35-71) | 0.7/1 | 4/1 |
| Melanocytic tumors | 4 | 1.4 | 0.5 | 0.2 | 66 (32-83) | 1/1 | 3/1 |
| Tumors of neural crest origin | 2 | 0.7 | 0.2 | 0.09 | 85 (84-85) | 1/1 | 0/2 |
F/M: Female/male; U/L: Upper/lower eyelid.
Epidermal tumors were the most frequent tumors (1080 tumors, 48.5%), and included benign (80.9%), premalignant (2.4%) and malignant (16.7%) lesions (exampled in Figure 1). Seborrheic keratosis was the most frequent epidermal tumor and accounted for 24.6% of epidermal tumors, 13.7% of benign tumors and 11.9% of all eyelid tumors. Squamous cell papilloma was the second most frequent epidermal tumor, followed by epidermal cysts, dermoid cysts, inverted follicular keratosis and keratoacanthoma. Dermoid cysts were mainly observed on the upper lids (5.7/1 for the upper/lower eyelid ratio) of young patients, whereas inverted follicular keratosis mainly occurred on the lower lids (0.9/1 for the upper/lower eyelid ratio) of elderly patients. There was only one patient with pilar sheath acanthoma, as shown in Table 3.
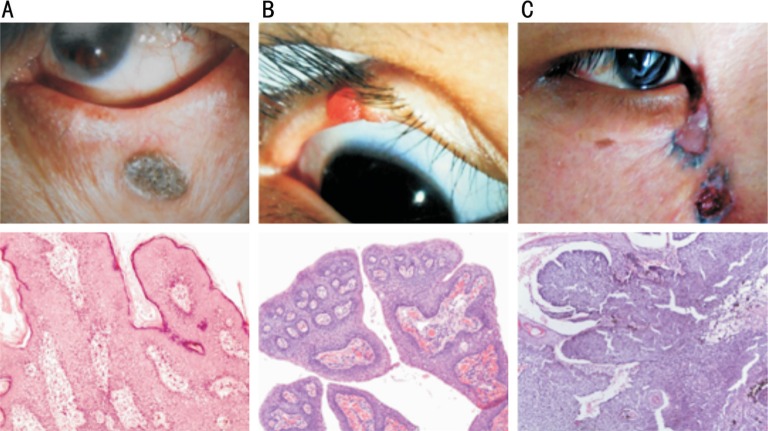
Figure 1. Examples of histopathologic views of epidermal tumors.
A: Seborrheic keratosis located at the lower eyelid of left eye (H&E 100×); B: Squamous papilloma located at the margin of upper eyelid of right eye (H&E 100×); C: Basal cell carcinoma located at the lower eyelid near the nasion of right eye (H&E 100×).
Table 3. Tumors of the epidermis (1080, 48.5%).
| Type of tumor | Cases | Epidermal tumors (%) | All tumors (%) | Mean age (range), y | Sex ratio (F/M) | Location (U/L) |
| Benign tumors and cysts (874, 80.9%) | ||||||
| Seborrheic keratosis | 266 | 24.6 | 11.9 | 57 (18-35) | 1/1 | 0.6/1 |
| Squamous cell papilloma | 252 | 23.3 | 11.3 | 45 (9-86) | 1.3/1 | 0.8/1 |
| Epidermal cyst | 222 | 20.5 | 10 | 54 (6-84) | 1/1 | 2.5/1 |
| Dermoid cyst | 74 | 6.9 | 3.3 | 25 (1-74) | 1.2/1 | 5.7/1 |
| Inverted follicular keratosis | 36 | 3.3 | 1.6 | 63 (37-86) | 1.1/1 | 0.9/1 |
| Keratoacanthoma | 23 | 2.1 | 1 | 63 (28-85) | 0.5/1 | 1.3/1 |
| Pilar sheath acanthoma | 1 | 0.09 | 0.04 | 51 (51-51) | 0/1 | 0/1 |
| Premalignant tumors (26, 2.4%) | ||||||
| Actinic/solar keratosis | 26 | 2.4 | 1.1 | 59 (26-75) | 1.6/1 | 0.9/1 |
| Malignant tumors (180, 16.7%) | ||||||
| Basal cell carcinoma | 165 | 15.3 | 7.4 | 63 (12-85) | 0.9/1 | 0.3/1 |
| Squamous cell carcinoma | 11 | 1 | 0.5 | 58 (40-80) | 1.2/1 | 1.8/1 |
| Papillary squamous cell carcinoma | 2 | 0.2 | 0.09 | 65 (54-76) | 1/1 | 1/1 |
| Basosquamous carcinoma | 2 | 0.2 | 0.09 | 53 (49-57) | 0/2 | 1/1 |
F/M: Female/male; U/L: Upper/lower eyelid.
Basal cell carcinomas were the most frequent malignant tumors (165 tumors, 91.7% of the epidermal malignant tumors). And there were 125 cases (75.8% of basal cell carcinoma) on the lower eyelid. Among the malignant epidermal tumors, there were 11 cases of squamous cell carcinoma, 2 cases of papillary squamous cell carcinoma, and 2 cases with basosquamous carcinoma.
Two hundred sixty-three adnexal tumors are described in Table 4 (exampled in Figure 2). The most common types originated from hair follicles and comprised 48.3% of adnexal tumors. Sebaceous gland tumors and tumors of eccrine and apocrine glands comprised 46.8% and 4.9% of adnexal tumors, respectively.
Table 4. Adnexal tumors (263, 11.8%).
| Type of tumor | Cases | Adnexal tumors (%) | All tumors (%) | Mean age (range), y | Sex ratio (F/M) | Location (U/L) |
| Sebaceous gland tumors (123, 46.8%) | ||||||
| Sebaceous carcinoma | 101 | 38.4 | 4.5 | 60 (20-98) | 1.9/1 | 2.1/1 |
| Sebaceous adenoma | 16 | 6.1 | 0.7 | 62 (7-83) | 1.7/1 | 1/1 |
| Sebaceous hyperplasia | 6 | 2.3 | 0.3 | 52 (28-70) | 0.5/1 | 2/1 |
| Hair follicle tumors (127, 48.3%) | ||||||
| Pilomatrixoma | 103 | 39.2 | 4.6 | 21 (1-84) | 1.3/1 | 0.1/1 |
| Trichoepithelioma | 20 | 7.6 | 0.9 | 49 (10-74) | 0.7/1 | 1.5/1 |
| Trichilemmoma | 1 | 0.4 | 0.04 | 68 (68-68) | 1/0 | 1/0 |
| Trichofolliculoma | 3 | 1.1 | 0.1 | 61 (49-70) | 2/1 | 3/0 |
| Tumors of eccrine and apocrine gland (13, 4.9%) | ||||||
| Hidrocystoma | 9 | 3.4 | 0.4 | 51 (9-72) | 2/1 | 0.8/1 |
| Syringoma | 4 | 1.5 | 0.18 | 43 (30-58) | 4/0 | 1/1 |
F/M: Female/male; U/L: Upper/lower eyelid.
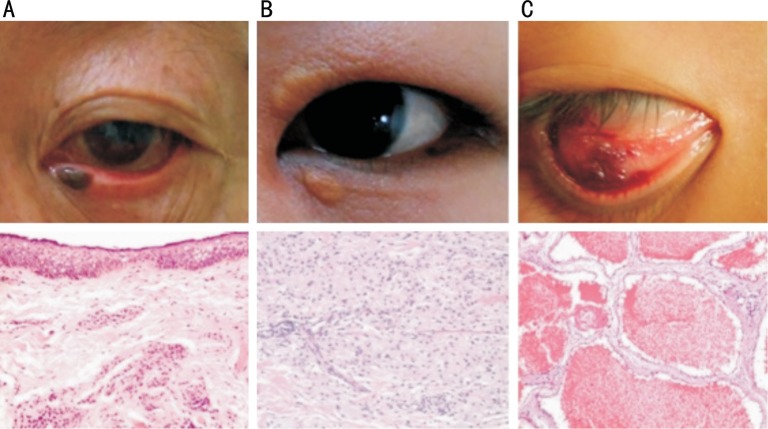
Figure 2. Examples of histopathologic views of adnexal tumors.
A: Sebaceous carcinoma located at the upper eyelid of right eye (H&E 100×); B: Pilomatrixoma located at the upper eyelid of left eye (H&E 100×).
The miscellaneous tumor types comprised 39.7% of all eyelid tumors (exampled in Figure 3). These tumors included many subtypes, such as the melanocytic, vascular, neural crest, lymphoid and metastatic tumors. Among these, melanocytic nevus was the most frequent and accounted for 73.9% of cases. Melanocytic nevus was also the most common tumor in our study (654 tumors, 29.4%). In this group of tumors, xanthelasma were the second most frequent tumor and accounted for 6.9% of cases. Both the melanocytic nevus and the xanthelasma groups showed female predominance (5/1 and 2.8/1 for the female/male ratios) and tended to located on the upper eyelid (1.3/1 and 5.8/1 for the upper/lower eyelid ratios), as shown in Table 5.
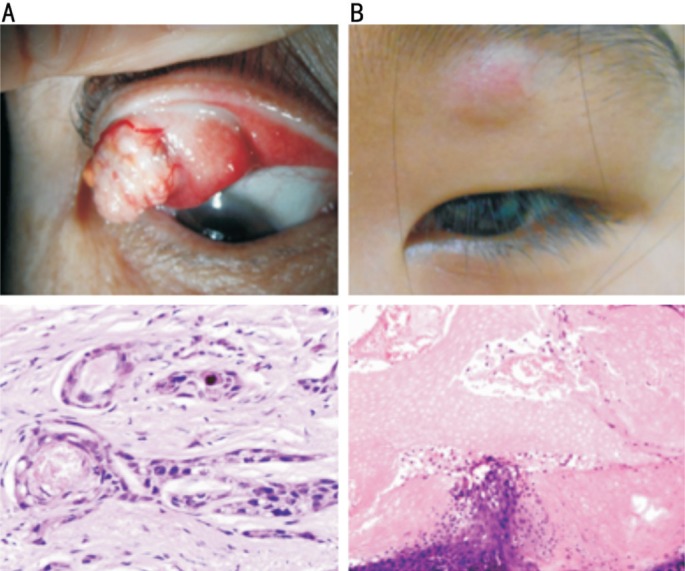
Figure 3. Examples of histopathologic views of miscellaneous tumors.
A: Melanocytic nevus located at the margin of lower eyelid near the inner canthus (H&E 100×); B: Xanthelasma located at the upper and lower eyelids near the inner canthus (H&E 100×); C: Cavernous hemangioma located at the inner side of lower eyelid (H&E 100×).
Table 5. The distribution of miscellaneous tumors (885, 39.7%).
| Type of tumor | Cases | Miscellaneous tumors (%) | All tumors (%) | Mean age (range), y | Sex ratio (F/M) | Location (U/L) |
| Melanocytic tumors (675, 76.3%) | ||||||
| Melanocytic nevus (common subtypes) | 654 | 73.9 | 29.4 | 46 (12-89) | 5/1 | 1.3/1 |
| Specific subtypes of melanocytic nevi | 14 | 1.6 | 0.6 | 35 (8-83) | 2.5/1 | 1/1 |
| Lentigo maligna | 3 | 0.3 | 0.1 | 19 (12-24) | 3/0 | 0/3 |
| Melanoma | 4 | 0.5 | 0.2 | 66 (32-83) | 1/1 | 3/1 |
| Vascular tumors (112, 12.7%) | ||||||
| Capillary hemangioma | 45 | 5.1 | 2 | 34 (3-76) | 1/1 | 2/1 |
| Cavernous hemangioma | 37 | 4.2 | 1.7 | 49 (25-79) | 2.4/1 | 1.6/1 |
| Arteriovenous hemangioma | 30 | 3.4 | 1.3 | 48 (11-76) | 0.9/1 | 1.6/1 |
| Tumors of neural crest origin (16, 1.7%) | ||||||
| Neurofibroma | 6 | 0.7 | 0.3 | 38 (13-71) | 2/1 | 2/1 |
| Schwannoma | 3 | 0.3 | 0.1 | 54 (33-68) | 0.5/1 | 0.5/1 |
| Solitary circumscribed neurinoma | 3 | 0.3 | 0.1 | 46 (30-60) | 2/1 | 0.5/1 |
| Traumatic neuroma | 2 | 0.2 | 0.09 | 33 (7-59) | 1/1 | 2/0 |
| Merkel cell carcinoma | 2 | 0.2 | 0.09 | 85 (84-85) | 1/1 | 0/2 |
| Lymphoid and metastatic tumors (5, 0.6%) | ||||||
| Lymphoma/plasmocytoma | 5 | 0.6 | 0.2 | 61 (35-71) | 0.7/1 | 4/1 |
| Other (77, 8.8%) | ||||||
| Xanthelasma | 61 | 6.9 | 2.7 | 54 (32-74) | 2.8/1 | 5.8/1 |
| Xanthogranuloma | 5 | 0.6 | 0.2 | 42 (28-54) | 1.5/1 | 5/0 |
| Fibrous histiocytoma | 5 | 0.6 | 0.2 | 50 (40-59) | 4/1 | 4/1 |
| Miscellaneous | 6 | 0.7 | 0.3 | 61 (51-74) | 0.5/1 | 2/1 |
F/M: Female/male; U/L: Upper/lower eyelid.
DISCUSSION
To the best of our knowledge, this study represents the largest biopsy series of eyelid tumors reported from China within the past decade. In our study, we found that the eyelid tumors primary originated from epidermal cells (1080, 48.5%), followed by miscellaneous cells (885, 39.7%) and adnexal cells (263, 11.8%). Of all the cases, there were 292 (13.1%) malignant lesions and 1910 (85.7%) benign and 26 (1.1%) premalignant lesions. In addition, both the malignant tumors and the benign tumors mainly originated from epidermal cells.
A number of authors have described their experiences with eyelid tumors. The largest study, published by Deprez and Uffer[1], described the frequencies of 5504 eyelid tumors. The authors reported that benign tumors represented 84% of all eyelid tumors, and the five most common tumor subtypes were squamous cell papilloma (26%), seborrheic keratosis (21%), melanocytic nevus (20%), hidrocystoma (8%), and xanthoma/xanthelasma (6%). In our study, the five most frequent subtypes were melanocytic nevus (29.3%), seborrheic keratosis (11.9%), squamous cell papilloma (11.3%), epidermal cyst (10%), and pilomatrixoma (4.6%). Huang et al[4] reported that in Taiwan, the most frequent benign subtypes were intradermal nevus (57.8%) followed by seborrheic keratosis (12.6%), xanthelasma (11.2%) and epidermal cyst (8.2%). The similarities and differences in the incidence rates of benign tumors can mainly be attributed to racial and regional factors.
Most benign eyelid tumors in the present study occurred in relatively young individuals compared with malignant eyelid tumors, which was similar to results from other studies[7]–[8]. Nevi were the most frequent benign lesions in this series and accounted for 33.8% of benign tumors. Compared with other results, these tumors tend to be more numerous in the Asian population[4]. Seborrheic keratosis (13.7%) was the second most common benign eyelid lesion in our study and was well delineated, elevated and often dark. In our study, seborrheic keratosis occurred in both sexes equally and primarily occurred on the lower eyelid (0.6/1 for the upper/lower eyelid ratio). Similar trends have been shown in previous studies[4],[9]. Prolonged exposure to sunlight seems to be an important predisposing factor[10], explaining why the tumor occurs more frequently on the lower eyelid[11].
Squamous cell papilloma was the most frequent benign tumor in the Gundogan et al's[7] and Deprez and Uffer's studies[1]. However, squamous cell papilloma was the third most common benign tumor in our study and accounted for 13.0% of all benign tumors. Xu et al[12] reported that 13.5% of benign tumors were squamous cell papilloma. These variations among studies should be noted. More importantly, the eyelids represent a frequent site for numerous malignant tumors, which generally present subtle symptoms or can imitate benign tumors[13]. We focused on the malignant eyelid tumors as the general consensus is that the incidence of malignant eyelid tumors is increasing[2],[14].
The study by Deprez and Uffer[1] reported that basal cell carcinoma accounted for 86% of all malignant tumors. In China, Xu et al[12] described 2639 eyelid neoplasms from the Beijing Tongren Eye Center. The authors found that the predominant non-benign eyelid tumors were basal cell carcinoma (41.3%). In our study, basal cell carcinoma still ranked first (56.5%). The differences among studies deserve to be emphasized. The possible explanations for these results may be the different classification criteria and varying sources of patients.
Basal cell carcinoma was the most frequent malignancy and usually involves the lower eyelid and medial canthus with a slow growth cycle[15]–[16]. It accounts for 80%-90% of all malignant tumors in western countries and Singapore[2],[17]–[18]. In the current study, it represented 56.5% of the malignant tumors, where in Taiwan[4] the incidence of basal cell carcinoma was 57.8%, 41.3% in Beijing[12], 32.6% in Japan[19] and 30%-40% in India and Korea[3]. These variations might be related to differences in geography and genetics. A male predominance (0.9/1) and preferred location on the lower eyelid (0.3/1) was demonstrated in our study, which was in agreement with the results of a previous study[1].
Sebaceous carcinoma was the second most common form of malignant eyelid tumor in our study. It often arises in the meibomian glands of the eyelid and results from the malignant proliferation of sebaceous cells[20]. The rich of meibomian glands in the upper eyelid can explain the preferred location of these tumors[21]. In our study, 101 cases of sebaceous carcinoma (34.6%) were diagnosed. There was a relative female predominance (1.9/1), and these tumors tended to located on the upper eyelid (2.1/1). Previous studies[21] have shown a higher incidence of sebaceous gland carcinoma in females, and the female/male ratio ranges from 1.5 to 1.6, which might be explained by the genetic and radical variations. Studies based on the Chinese, Japanese, Indian and Singaporean populations have shown sebaceous carcinoma rates were 38.6%, and 37.5%, 31.2% and 10.2%, respectively[12],[17],[22]–[23]. However, in the United States, sebaceous carcinoma represents 5% of all malignant neoplasms that arise in the periocular region[5],[24]. The rate of sebaceous carcinoma varies according to the ethnicity of the population and tends to be greater in Asians than in Europeans and Americans[2],[12],[25].
Squamous cell carcinoma can be associated with significant morbidity because these tumors are locally invasive and can metastasize. In addition, widely varying incidence rates have been described for squamous cell carcinoma. In western countries, it is the second most common malignancy of the eyelid accounts for 5%-10% of all eyelid malignancies[26]–[27]. In the Philippines, the incidence has been reported as 17.1%[28] and 48.1% in Japan[29]. In current study, there were only 11 patients with squamous cell carcinoma, which comprised 3.8% of the malignant eyelid tumor cases, and the tumors were located mainly on the lower eyelid, which was consistent with the report by Deprez and Uffer[1].
In conclusion, the histological origin and classification of eyelid tumors has been gradually refined. We analyzed the eyelid tumors based on the updated classification system, including the origin, pathological nature and clinical features. Our study provides a large set of epidemiological data for eyelid tumors from China. This large series suggested that most eyelid tumors were epithelial in origin. The rate of benign tumors was significantly greater than that of malignant tumors, and the tumors primarily originated from epithelial cells with an obvious female predominance. The malignant tumors that also mainly originated from epithelial cells tended to located on the lower eyelid.
Acknowledgments
Conflicts of Interest: Yu SS, None; Zhao Y, None; Zhao H, None; Lin JY, None; Tang X, None.
REFERENCES
- 1.Deprez M, Uffer S. Clinicopathological features of eyelid skin tumors. A retrospective study of 5504 cases and review of literature. Am J Dermatopathol. 2009;31(3):256–262. doi: 10.1097/DAD.0b013e3181961861. [DOI] [PubMed] [Google Scholar]
- 2.Lin HY, Cheng CY, Hsu WM, Kao WH, Chou P. Incidence of eyelid cancers in Taiwan: a 21-year review. Ophthalmology. 2006;113(11):2101–2107. doi: 10.1016/j.ophtha.2006.06.001. [DOI] [PubMed] [Google Scholar]
- 3.Mak ST, Wong AC, Io IY, Tse RK. Malignant eyelid tumors in Hong Kong 1997-2009. Jpn J Ophthalmol. 2011;55(6):681–685. doi: 10.1007/s10384-011-0077-4. [DOI] [PubMed] [Google Scholar]
- 4.Huang YY, Liang WY, Tsai CC, Kao SC, Yu WK, Kau HC, Liu CJ. Comparison of the clinical characteristics and outcome of benign and malignant eyelid tumors: an analysis of 4521 eyelid tumors in a tertiary medical center. Biomed Res Int. 2015;2015:453091. doi: 10.1155/2015/453091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shields JA, Shields CL. Sebaceous adenocarcinoma of the eyelid. Int Ophthalmol Clin. 2009;49(4):45–61. doi: 10.1097/IIO.0b013e3181b7f059. [DOI] [PubMed] [Google Scholar]
- 6.Nemoto Y, Arita R, Mizota A, Sasajima Y. Differentiation between chalazion and sebaceous carcinoma by noninvasive meibography. Clin Ophthalmol. 2014;8:1869–1875. doi: 10.2147/OPTH.S69804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gundogan FC, Yolcu U, Tas A, Sahin OF, Uzun S, Cermik H, Ozaydin S, Ilhan A, Altun S, Ozturk M, Sahin F, Erdem U. Eyelid tumors: clinical data from an eye center in Ankara, Turkey. Asian Pac J Cancer Prev. 2015;16(10):4265–4269. doi: 10.7314/apjcp.2015.16.10.4265. [DOI] [PubMed] [Google Scholar]
- 8.Asproudis I, Sotiropoulos G, Gartzios C, Raggos V, Papoudou-Bai A, Ntountas I, Katsanos A, Tatsioni A. Eyelid tumors at the university eye clinic of ioannina, greece: a 30-year retrospective study. Middle East Afr J Ophthalmol. 2015;22(2):230–232. doi: 10.4103/0974-9233.151881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Roh NK, Hahn HJ, Lee YW, Choe YB, Ahn KJ. Clinical and histopathological investigation of seborrheic keratosis. Ann Dermatol. 2016;28(2):152–158. doi: 10.5021/ad.2016.28.2.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pieh S, Kuchar A, Novak P, Kunstfeld R, Nagel G, Steinkogler FJ. Long-term results after surgical basal cell carcinoma excision in the eyelid region. Br J Ophthalmol. 1999;83(1):85–88. doi: 10.1136/bjo.83.1.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cook BE, Jr, Bartley GB. Treatment options and future prospects for the management of eyelid malignancies: an evidence-based update. Ophthalmology. 2001;108(11):2088–2098. quiz 2099–2100, 2121. doi: 10.1016/s0161-6420(01)00796-5. [DOI] [PubMed] [Google Scholar]
- 12.Xu XL, Li B, Sun XL, Li LQ, Ren RJ, Gao F, Jonas JB. Eyelid neoplasms in the Beijing Tongren Eye Centre between 1997 and 2006. Ophthalmic Surg Lasers Imaging. 2008;39(5):367–372. doi: 10.3928/15428877-20080901-18. [DOI] [PubMed] [Google Scholar]
- 13.Dekmezian MS, Cohen PR, Sami M, Tschen JA. Malignancies of the eyelid: a review of primary and metastatic cancers. Int J Dermatol. 2013;52(8):903–926. quiz 922–923, 926. doi: 10.1111/ijd.12089. [DOI] [PubMed] [Google Scholar]
- 14.Balasoiu AT, Manescu MR, Balasoiu M, Avramoiu I, Pirici I, Burcea M, Mogoanta L, Mocanu CL. Histological and immunohistochemical study of the eyelid basal cell carcinomas. Rom J Morphol Embryol. 2015;56(2 Suppl):803–810. [PubMed] [Google Scholar]
- 15.Iljin A, Zielinski T, Antoszewski B, Sporny S. Clinicopathological analysis of recurrent basal cell carcinoma of the eyelid. Postepy Dermatol Alergol. 2016;33(1):42–46. doi: 10.5114/pdia.2015.48039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ben Simon GJ, Lukovetsky S, Lavinsky F, Rosen N, Rosner M. Histological and clinical features of primary and recurrent periocular Basal cell carcinoma. ISRN Ophthalmol. 2012;2012:354829. doi: 10.5402/2012/354829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee SB, Saw SM, Au Eong KG, Chan TK, Lee HP. Incidence of eyelid cancers in Singapore from 1968 to 1995. Br J Ophthalmol. 1999;83(5):595–597. doi: 10.1136/bjo.83.5.595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lim VS, Amrith S. Declining incidence of eyelid cancers in Singapore over 13 years: population-based data from 1996 to 2008. Br J Ophthalmol. 2012;96(12):1462–1465. doi: 10.1136/bjophthalmol-2012-302032. [DOI] [PubMed] [Google Scholar]
- 19.Abe M, Ohnishi Y, Hara Y, Shinoda Y, Jingu K. Malignant tumor of the eyelid-clinical survey during 22-year period. Jpn J Ophthalmol. 1983;27(1):175–184. [PubMed] [Google Scholar]
- 20.Nemoto Y, Arita R, Mizota A, Sasajima Y. Differentiation between chalazion and sebaceous carcinoma by noninvasive meibography. Clin Ophthalmol. 2014;8:1869–1875. doi: 10.2147/OPTH.S69804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang JK, Liao SL, Jou JR, Lai PC, Kao SC, Hou PK, Chen MS. Malignant eyelid tumours in Taiwan. Eye (Lond) 2003;17(2):216–220. doi: 10.1038/sj.eye.6700231. [DOI] [PubMed] [Google Scholar]
- 22.Obata H, Aoki Y, Kubota S, Kanai N, Tsuru T. Incidence of benign and malignant lesions of eyelid and conjunctival tumors. Nippon Ganka Gakkai Zasshi. 2005;109(9):573–579. [PubMed] [Google Scholar]
- 23.Kale SM, Patil SB, Khare N, Math M, Jain A, Jaiswal S. Clinicopathological analysis of eyelid malignancies-a review of 85 cases. Indian J Plast Surg. 2012;45(1):22–28. doi: 10.4103/0970-0358.96572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shields JA, Demirci H, Marr BP, Eagle RC, Jr, Shields CL. Sebaceous carcinoma of the eyelids: personal experience with 60 cases. Ophthalmology. 2004;111(12):2151–2157. doi: 10.1016/j.ophtha.2004.07.031. [DOI] [PubMed] [Google Scholar]
- 25.Mulay K, Aggarwal E, White VA. Periocular sebaceous gland carcinoma: a comprehensive review. Saudi J Ophthalmol. 2013;27(3):159–165. doi: 10.1016/j.sjopt.2013.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Inaba K, Ito Y, Suzuki S, Sekii S, Takahashi K, Kuroda Y, Murakami N, Morota M, Mayahara H, Sumi M, Uno T, Itami J. Results of radical radiotherapy for squamous cell carcinoma of the eyelid. J Radiat Res. 2013;54(6):1131–1137. doi: 10.1093/jrr/rrt069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sun MT, Andrew NH, O'Donnell B, McNab A, Huilgol SC, Selva D. Periocular squamous cell carcinoma: TNM staging and recurrence. Ophthalmology. 2015;122(7):1512–1516. doi: 10.1016/j.ophtha.2015.04.002. [DOI] [PubMed] [Google Scholar]
- 28.Domingo RE, Manganip LE, Castro RM. Tumors of the eye and ocular adnexa at the Philippine Eye Research Institute: a 10-year review. Clin Ophthalmol. 2015;9:1239–1247. doi: 10.2147/OPTH.S87308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Abe M, Ohnishi Y, Hara Y, Shinoda Y, Jingu K. Malignant tumor of the eyelid-clinical survey during 22-year period. Jpn J Ophthalmol. 1983;27(1):175–184. [PubMed] [Google Scholar]