Abstract
Objective
Cigarette smoking and smoking‐related diseases disproportionately affect low‐income populations. Health insurance coverage of smoking cessation treatments is increasingly used to encourage quitting. We assess the relationship between state Medicaid coverage of smoking cessation treatments and past‐year quitting in adult Medicaid beneficiaries.
Data Sources
2009–2014 National Health Interview Survey (NHIS); 2008–2013 indicators of state Medicaid coverage of smoking cessation treatments.
Study Design
A triple‐differencing specification based on differences in Medicaid cessation coverage policies across states as well as within‐state differences between Medicaid beneficiaries and a counterfactual group of low‐income adults not covered by Medicaid.
Data Collection/Extraction Methods
Individual‐level NHIS data with restricted geographical identifiers were merged with state‐year Medicaid coverage indicators.
Principal Findings
Combined coverage of both cessation counseling and medications in state Medicaid programs was associated with increased quitting, with an estimated mean increase in past‐year quitting of 3.0 percentage points in covered Medicaid beneficiaries relative to persons without coverage.
Conclusions
Combined coverage of both smoking cessation counseling and medication by state Medicaid programs could help reduce cigarette smoking among Medicaid beneficiaries.
Keywords: Smoking, tobacco‐dependence treatments, state health policies
Cigarette smoking is the leading cause of preventable disease and death in the United States, resulting in more than 480,000 deaths per year (U.S. DHHS 2014). Smoking costs the United States more than $300 billion per year in direct medical expenditure and lost productivity; health care costs for smoking‐attributable diseases account for nearly 9 percent of U.S. health care spending, or about $170 billion per year (Xu et al. 2015). The majority of smoking‐attributable expenses are borne by public programs; expenses related to the treatment of smoking‐related illnesses account for more than 15 percent of annual Medicaid spending, or almost $40 billion each year (Xu et al. 2015).
Smoking and smoking‐related health conditions are more common in low‐income populations (U.S. Department of Health and Human Services 2014). In 2015, the prevalence of cigarette smoking among U.S. adults living below the poverty level (26.1 percent) was nearly twice that of those living at or above the poverty level (13.9 percent). Moreover, between 2005 and 2015, smoking prevalence declined 32.8 percent among those living at or above the poverty level compared to 12.7 percent among those living below the poverty level (Jamal et al. 2016).
Medicaid is the largest insurance provider for low‐income persons in the United States (CMMS 2017). Traditional state Medicaid programs have increased coverage of smoking cessation treatments over the past decade, although coverage can vary widely across and within states, between the fee‐for‐service (FFS) population and managed care (MC) plans, and among different managed care plans (McMenamin et al. 2010; Singleterry et al. 2015; Ku et al. 2016). While Medicaid coverage of cessation treatments has increased over time, barriers to accessing these treatments, such as copayments and prior authorization, have persisted in traditional Medicaid programs (McMenamin et al. 2009; Singleterry et al. 2015). Given that the current Medicaid policy environment is characterized by substantial variation in the coverage of cessation treatments both across states and across populations within some states, opportunities exist for future optimization of coverage policies.
Smoking cessation treatments fall into two categories: counseling, including individual, group, and telephone counseling; and medications, including seven Food and Drug Administration (FDA)–approved cessation medications, comprised of five forms of nicotine‐replacement therapy (NRT) and two non‐nicotine prescription drugs. Improved insurance coverage of smoking cessation treatments can encourage quit attempts, use of cessation treatments, and cessation (Fiore et al. 2008). However, few published studies have examined the impact of state Medicaid cessation coverage on actual smoking cessation among smokers enrolled in Medicaid. Use of cessation medicines is higher among Medicaid beneficiaries with cessation benefits (Ku et al. 2016; Maclean, Pesko, and Hill 2017), yet evidence also suggests that, in the absence of concerted efforts to promote increased awareness and use of covered cessation treatments among Medicaid beneficiaries and their health care providers, relatively few cigarette smokers enrolled in Medicaid are aware of Medicaid cessation coverage and use covered medications (McMenamin et al. 2004; Murphy et al. 2005), and that initial increases in utilization of cessation medications following increases in coverage may not be sustained (Li and Dresler 2012). Moreover, the magnitude of the impact of Medicaid cessation coverage on smoking cessation is uncertain. One study from Massachusetts documented reductions in smoking prevalence among Medicaid beneficiaries following the introduction and promotion of a state Medicaid cessation coverage benefit (Land et al. 2010), but another study found no effects on smoking overall (Courtemanche and Zapata 2014). A study using cross‐state data from Medicaid beneficiaries to evaluate quitting as an outcome of a cessation coverage index showed mixed effects (Liu 2009). Subsequent studies evaluating Medicaid cessation coverage have found that more comprehensive coverage was associated with higher quit rates among pregnant women in 34 states (Adams et al. 2013) and among adult beneficiaries in 28 states (Greene, Sacks, and McMenamin 2014). However, the absence of a within‐state counterfactual may leave the estimates open to bias from cross‐state differences in smoking patterns that may not be unique to Medicaid, and to state‐level confounders such as concurrent state policy changes. For example, many states implemented statewide indoor smoking bans between 2000 and 2010, which was shown to reduce smoking, especially in low‐income persons (Carton et al. 2016). Thus, to date, evidence on the effects of Medicaid cessation coverage on smoking cessation has not been nationally representative, and it may have been subject to confounding from secular trends in quitting behavior in the general low‐income population that may be related to state uptake of coverage without being specific to Medicaid beneficiaries.
To help fill the aforementioned gaps in the literature, we assessed the effects of Medicaid cessation coverage on smoking cessation among Medicaid beneficiaries using a triple‐differencing framework, where unobserved state‐level confounders were addressed using a within‐state comparison group of low‐income persons not covered by Medicaid, in addition to cross‐state differences in Medicaid coverage trends. We used state‐level data on cessation coverage from 2008 to 2013 matched to individual‐level surveillance data on past‐year quitting from the National Health Interview Survey (NHIS) 2009–2014. This analysis covers the period immediately preceding the 2014 Medicaid expansion and reflects coverage effects for traditional Medicaid only. This may have policy relevance in a changing policy landscape where some states consider reintroducing a pre‐expansion Medicaid framework.
Data and Methods
Data
State‐level data on Medicaid coverage of smoking cessation treatments during 2008–2013 were obtained from the American Lung Association (ALA 2016). Assessed cessation treatments included NRT (gum, patch, nasal spray, inhaler, or lozenge), prescription drugs (varenicline or bupropion), and counseling (individual or group). NRT and prescription drug coverage were combined to represent medication coverage. The counseling coverage includes individual and/or group counseling.
State Medicaid coverage can differ between fee‐for‐service (FFS) and managed care (MC) plans within a state. Throughout the study period, 12 states had different terms of cessation coverage across FFS and MC plans, while 39 states had at least 1 year of matching MC‐FFS coverage (Table 1). For state‐years with reported differences in MC‐versus‐FFS coverage, we assigned either MC or FFS coverage depending on whether the majority of the Medicaid population was enrolled in MC or FFS in the corresponding state‐year (KFF 2014). Sensitivity of the results to this assignation was examined by alternatively including and excluding state‐years with different MC and FFS cessation coverage.
Table 1.
Summary of State Medicaid Coverage of Smoking Cessation Treatments, 2008–2013
| State | Medication‐Only Coveragea | Counseling‐OnlyCoverageb | Combined Coveragec | MC‐FFS Overlapd |
|---|---|---|---|---|
| Alabama | No | No | No | No |
| Alaska | No | No | 2008–2013 | Yes |
| Arizona | 2008–2013 | No | No | Yes |
| Arkansas | No | 2012 | 2008–2011, 2013 | No |
| California | 2012–2013 | No | 2008–2011 | Yes |
| Colorado | 2008–2011, 2013 | No | No | Yes |
| Connecticut | No | No | 2011–2013 | Yes |
| Delaware | 2008–2010 | No | 2011–2013 | Yes |
| District of Columbia | No | No | No | No |
| Florida | No | 2009–2012 | 2008 | Yes |
| Georgia | No | No | No | Yes |
| Hawaii | 2010–2011 | No | No | Yes |
| Idaho | 2010–2013 | No | 2008–2009 | Yes |
| Illinois | 2008–2013 | No | No | Yes |
| Indiana | No | No | 2008–2013 | Yes |
| Iowa | No | No | 2008–2013 | No |
| Kansas | 2008–2009, 2012–2013 | No | No | Yes |
| Kentucky | 2010–2011 | No | No | Yes |
| Louisiana | 2008–2013 | No | No | Yes |
| Maine | No | 2012–2013 | 2008–2011 | No |
| Maryland | 2011–2013 | 2008 | No | No |
| Massachusetts | No | No | 2008–2013 | Yes |
| Michigan | No | No | 2010–2013 | Yes |
| Minnesota | No | No | 2008–2013 | Yes |
| Mississippi | 2008–2013 | No | No | Yes |
| Missouri | No | No | 2011–2013 | Yes |
| Montana | No | No | 2008–2013 | No |
| Nebraska | No | No | 2008–2013 | Yes |
| Nevada | No | No | 2008–2013 | Yes |
| New Hampshire | No | No | 2008–2013 | Yes |
| New Jersey | 2011–2013 | 2008 | No | Yes |
| New Mexico | 2012–2013 | No | No | No |
| New York | 2008–2010 | 2011–2012 | 2013 | Yes |
| North Carolina | 2008 | No | 2009–2013 | No |
| North Dakota | 2010–2013 | No | 2008–2009 | No |
| Ohio | 2008–2013 | No | No | Yes |
| Oklahoma | No | No | 2008–2013 | No |
| Oregon | No | No | 2008–2013 | Yes |
| Pennsylvania | No | No | 2008–2013 | Yes |
| Rhode Island | 2011 | 2008–2009 | 2010, 2012–2013 | Yes |
| South Carolina | 2008 | No | No | Yes |
| South Dakota | No | No | No | No |
| Tennessee | 2011–2013 | No | No | Yes |
| Texas | 2008–2013 | No | No | Yes |
| Utah | No | No | No | Yes |
| Vermont | 2008–2013 | No | No | Yes |
| Virginia | 2008 | No | 2012–2013 | Yes |
| Washington | No | No | 2008 | Yes |
| West Virginia | 2008–2013 | No | No | Yes |
| Wisconsin | No | No | 2008–2013 | Yes |
| Wyoming | No | No | 2008–2013 | Yes |
Coverage of at least one prescription drug (bupropion or varenicline) and at least one nicotine‐replacement therapy (gum, patch, spray, inhaler, lozenge).
Coverage of individual or group counseling for smoking cessation.
Coverage of both medication and counseling.
Denotes states with at least one year where MC and FFS cessation benefits overlap.
Source: Authors’ analysis of state‐level data on Medicaid coverage of smoking cessation treatments during 2008–2013 obtained from the American Lung Association.
A four‐level categorical factor was constructed at the state‐year level: (1) no coverage; (2) medication‐only coverage; (3) counseling‐only coverage; and (4) combined medication and counseling coverage (Table 1). Two binary variables denoted the presence of barriers: (1) copayments; and (2) other barriers, including prior authorization and duration use limits. Cigarette price was included as a state‐level control variable in all models (Orzechowski and Walker 2014).
We obtained individual‐level data on cigarette smoking history and demographic attributes from the IPUMS National Health Interview Survey (IPUMS NHIS) 2009–2014 sample adult files (Blewett et al. 2016). IPUMS NHIS is a consolidated extraction source for the public use NHIS files. The NHIS is a nationally representative cross‐sectional household interview survey of the civilian noninstitutionalized population of the United States (NCHS 2016). The examined outcome, past‐year quitting, is retrospective, and was defined as a binary indicator with a value of “1” indicating that the respondent reported quitting smoking within the past year and has not smoked for at least 30 days prior to the survey, and a value of “0” if the respondent is a current smoker.
The study sample consists of 11,170 low‐income adults with an estimated past‐year age range of 19–64 years who are not pregnant, are not on Medicare, and have Medicaid‐only insurance or family incomes not exceeding 150 percent of the federal poverty level (FPL). As determined by the evaluated outcome, the sample consists of current smokers and former smokers who quit in the past year. Medicare enrollment was an exclusion criterion because it can indicate disability in nonelderly persons as well as different coverage benefits; pregnant women were similarly excluded as they are subject to a special federal requirement for Medicaid cessation coverage. Because quitting outcomes are retrospective, the sample was merged with year‐lagged state coverage indicators. All individual‐level NHIS indicators were self‐reported.
Methods
The effect of cessation coverage on quitting among Medicaid beneficiaries was estimated using a differencing specification based on differences in Medicaid cessation coverage policies across and within states, as well as within‐state differences between Medicaid beneficiaries and counterfactual groups of low‐income adults not covered by Medicaid. The baseline model was specified as follows:
| (1) |
where denotes past‐year quitting for individual i in state j and year t. The outcome variable is 0 if the individual is a current everyday or some‐day smoker and 1 if the individual is a former smoker who reports having quit smoking within the past 12 months and has not smoked for at least 30 days. is a binary indicator equal to 1 if individual i is enrolled in Medicaid without other concurrent types of insurance, and 0 otherwise; is a vector of individual attributes, including age, gender, race, nativity, marital status, educational attainment, self‐reported health status, and children in the household; denotes real cigarette prices at the state‐year level. is a binary variable equal to 1 if state j in year t offers Medicaid coverage of cessation medications (at least one prescription medication and at least one over‐the‐counter NRT) without counseling coverage, and 0 otherwise. is a binary variable equal to 1 if state j in year t offers Medicaid coverage of cessation counseling (group or individual) without covering cessation medications, and 0 otherwise. is a binary variable equal to 1 if state j in year t offers Medicaid coverage of both medications and counseling, and 0 otherwise. The estimators of interest, β 5, β 6, and β 7, represent the average treatment effect among Medicaid beneficiaries of each coverage type.
Controls for state fixed effects, , were used to address unobserved state characteristics and/or state‐level policies that may affect both states’ cessation coverage policy and quitting patterns. For instance, states that do not offer coverage may differ from states with coverage in ways that may also be related to having disproportionately lower likelihood of quitting (such as population sentiment that both reduces Medicaid generosity and increases the likelihood of smoking). Therefore, omitting γ 0j may bias the relationship between state policy and cessation outcomes. To account for state‐level heterogeneity that varies over time, state‐specific time trends () were included via the interactions between state dummy variables and a linear time trend. To account for unobserved Medicaid‐specific changes in quitting over time, we include an interaction term between Medicaid status and a linear time trend (). In all specifications, year fixed effects, , control for secular time trends in quitting. The estimation was performed using linear probability models, where the error term, , was clustered at the state level. To test the sensitivity of the analysis to the composition of the sample, the baseline model in equation (1) was estimated using two alternative samples. First, to examine the possibility of measurement error from assigning either MC or FFS coverage in states where MC and FFS benefits differ, we used an alternative sample that excluded observations from state‐years with different MC and FFS benefits. Second, to assess comparability of the Medicaid treatment group to non‐Medicaid persons with a higher income threshold, we used a sample that raised the income threshold for the comparison group from 150 to 250 percent of FPL. Finally, to evaluate the role of access barriers in the presence of coverage, equation (1) was estimated with additional controls for Medicaid‐specific indicators of the presence of copayments and other barriers.
Statistical significance of all estimates was evaluated at p < .01, p < .05, and p < .10. All analysis was performed using sample adult weights with state‐level clustering using STATA 14.0 (College Station, TX: StataCorp LP).
Robustness Checks
Because the evaluation of Medicaid coverage effects is based on within‐state differences between Medicaid beneficiaries and the comparison group of low‐income persons not covered by Medicaid in addition to cross‐state variation in coverage, a primary empirical consideration is the appropriateness of the comparison groups. The ideal comparison group is similar in composition to the treatment group while being unaffected by the treatment variable. In this study, we have to address the possibility that the treatment variable (Medicaid coverage) may apply to some members of the within‐state comparison group (low‐income persons not covered by Medicaid), resulting in potential cross‐contamination between the groups; this is a risk because retrospective information on past‐year Medicaid coverage was not available. To reduce this risk, persons reporting breaks in Medicaid coverage in the past year, persons reporting concurrent enrollment in Medicaid and other types of insurance, and persons with private plans paid for by Medicaid were excluded from the treatment group.
We employed a number of robustness checks to further test the assumptions of the empirical model. First, we explored the sensitivity of the results to the choice of within‐state comparison group by constructing the counterfactual exclusively from persons who had been uninsured continuously over the past year. Although this reduced the size of the within‐state comparison group, limiting it to long‐term uninsured persons reduces the risk of including persons who may have had recent Medicaid coverage or private coverage mirroring Medicaid. This specification was the same as the baseline model in equation (1), except was defined as equal to 1 if person i is enrolled in Medicaid, and 0 if continuously uninsured for at least a year. Similarity between the estimates from this specification and the baseline estimates from equation (1) would provide some assurance for the assumption that cross‐contamination in the baseline models may not pose a primary threat to validity.
Next, a placebo test was conducted by replacing the original treatment group of Medicaid beneficiaries with a pseudotreatment group unaffected by Medicaid coverage rules, namely privately insured low‐income adults. This specification followed equation (1), except that the variable was replaced by a variable equal to 1 if person i was exclusively privately insured without a reported insurance interruption in the past year (pseudotreatment group), and 0 if he or she was continuously uninsured for at least a year (within‐state comparison group). In this case, estimating a significant treatment effect on the pseudotreatment group would raise concerns that privately insured low‐income adults, who are otherwise members of the original within‐state comparison group in the baseline specification, could be spuriously sharing quitting trends with Medicaid beneficiaries, biasing the original estimates.
Another condition for identification in the baseline model is the presence of parallel trends before the intervention across outcomes in the treatment and comparison groups. Because the interventions evaluated in this analysis are multiple (three types of cessation coverage), and because they occurred at different times within states, a visual examination of outcome trends cannot provide a clean pre–post‐depiction of shared (or diverging) trend patterns across treatment and comparison groups. We thus examined the plausibility of the parallel trends assumption by estimating regressions that check for Medicaid‐specific outcome differentials that might have occurred prior to the actual shifts in coverage. We used a Granger‐type specification which mirrored the baseline specification in equation (1) while also including, in addition to the original coverage variables, a set of binary precoverage variables and interacting these with Medicaid status. These precoverage indicators take on a value of 1 during the 2 years prior to the change in coverage, 0 otherwise, and are mutually exclusive with the indicators of actual coverage. Because variation in these precoverage indicators occurs only within states that change coverage during the study period, their variation is more limited than that for the actual coverage indicators, reducing the statistical power of the test. Nonetheless, significant coefficients on the interaction terms between Medicaid and the precoverage variables would indicate that Medicaid beneficiaries might have experienced differential outcomes relative to their non‐Medicaid counterparts even before the change in Medicaid coverage, potentially violating the parallel trends assumption in the baseline models.
Although limiting the sample to persons with family incomes not exceeding 150 percent of FPL helps to reduce dissimilarities between Medicaid beneficiaries and their non‐Medicaid counterfactuals, some demographic differences remain. These differences can be problematic for identification, especially if they are prominent between Medicaid beneficiaries in treatment states (i.e., states with combined medication and counseling coverage) and Medicaid beneficiaries in comparison states (i.e., states with no coverage), because of the possibility that such differential composition may affect the introduction of coverage at the state level. However, the demographic composition of Medicaid beneficiaries is fairly balanced across treatment and comparison states, and a comparison of the sample characteristics of Medicaid beneficiaries between states with and without combined coverage revealed relatively few statistical differences (Table 2). Demographic differences were more pronounced between Medicaid beneficiaries in combined‐coverage states and their within‐state counterfactual group of low‐income adults not covered by Medicaid, where the latter are more likely to be younger, male, married, white, better educated, and healthier (Table 2). However, as these differences are at the within‐state level, they would be less likely to confound the estimated average treatment effects of state‐level coverage policies.
Table 2.
Mean Sample Characteristics (%)
| Medicaid Beneficiaries | Low‐Income Adults Not on MEDICAID | p‐Values from Wald's Test of Statistical Significance of Differences between | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall | States with Combined Coverage | States without Combined Coverage | Overall | States with Combined Coverage | States without Combined Coverage | |||||||
| (1) | (2) | (3) | (4) | (5) | (6) | (1)–(4) | (2)–(5) | (3)–(6) | (2)–(3) | (3)–(4) | (2)–(4) | |
| n | 3,602 | 2,151 | 1,451 | 7,568 | 4,246 | 3,322 | ||||||
| Quit in past year | 8.4 | 9.8 | 6.4 | 8.8 | 9.1 | 8.5 | 0.530 | 0.466 | 0.023 | 0.001 | 0.003 | 0.286 |
| Age | ||||||||||||
| 19–34 | 40.7 | 39.8 | 42.0 | 47.1 | 47.0 | 47.2 | 0.000 | 0.000 | 0.006 | 0.218 | 0.001 | 0.000 |
| 35–44 | 22.0 | 22.3 | 21.6 | 19.2 | 19.9 | 18.3 | 0.006 | 0.065 | 0.033 | 0.682 | 0.087 | 0.011 |
| 45–54 | 22.1 | 22.8 | 21.0 | 19.5 | 19.5 | 19.6 | 0.007 | 0.010 | 0.308 | 0.218 | 0.231 | 0.005 |
| 55–64 | 15.2 | 15.1 | 15.4 | 14.1 | 13.5 | 14.9 | 0.165 | 0.102 | 0.703 | 0.863 | 0.305 | 0.272 |
| Male | 34.4 | 37.0 | 30.4 | 53.5 | 53.4 | 53.7 | 0.000 | 0.000 | 0.000 | 0.001 | 0.000 | 0.000 |
| U.S. born | 90.9 | 87.6 | 95.9 | 87.7 | 87.3 | 88.3 | 0.000 | 0.730 | 0.000 | 0.000 | 0.000 | 0.900 |
| Married | 18.5 | 18.6 | 18.2 | 23.4 | 22.9 | 23.9 | 0.000 | 0.001 | 0.000 | 0.803 | 0.000 | 0.000 |
| Race | ||||||||||||
| White | 59.0 | 59.7 | 58.0 | 65.9 | 68.4 | 62.7 | 0.000 | 0.000 | 0.054 | 0.485 | 0.001 | 0.000 |
| Hispanic | 11.9 | 15.1 | 7.2 | 13.1 | 12.0 | 14.5 | 0.121 | 0.005 | 0.000 | 0.000 | 0.000 | 0.057 |
| Black | 25.5 | 20.9 | 32.3 | 16.8 | 14.3 | 20.0 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
| Other | 3.6 | 4.3 | 2.6 | 4.2 | 5.2 | 2.8 | 0.190 | 0.157 | 0.582 | 0.006 | 0.001 | 0.729 |
| Education | ||||||||||||
| Less than high school | 36.9 | 36.2 | 37.8 | 23.9 | 21.8 | 26.7 | 0.000 | 0.000 | 0.000 | 0.496 | 0.000 | 0.000 |
| High school or GED | 34.8 | 33.7 | 36.4 | 36.1 | 36.5 | 35.4 | 0.297 | 0.043 | 0.641 | 0.169 | 0.851 | 0.069 |
| Some college or associate degree | 25.0 | 26.3 | 23.0 | 33.2 | 34.5 | 31.5 | 0.000 | 0.000 | 0.000 | 0.071 | 0.000 | 0.000 |
| College degree or higher | 3.3 | 3.7 | 2.7 | 6.8 | 7.1 | 6.3 | 0.000 | 0.000 | 0.000 | 0.185 | 0.000 | 0.000 |
| Child under 18 in family | 56.0 | 54.3 | 58.4 | 40.3 | 39.9 | 40.8 | 0.000 | 0.000 | 0.000 | 0.055 | 0.000 | 0.000 |
| Health reported as poor/very poor | 39.7 | 38.7 | 41.3 | 21.2 | 21.0 | 21.5 | 0.000 | 0.000 | 0.000 | 0.164 | 0.000 | 0.000 |
Notes: Sample consists of persons aged 19–64 years (past‐year estimated), not pregnant, not covered by Medicare, enrolled in Medicaid or with family incomes not exceeding 150% of the federal poverty level (FPL), who are either current smokers or former smokers who quit in the past year. *p < .1, **p < .05, ***p < .01.
Source: Authors’ analysis of data from the National Health Interview Survey 2009–2014.
Limitations
This study had several limitations. First, measurement error may be introduced in the coverage indicators by assigning a single coverage classification (either FFS or MC) in state‐years where FFS and MC Medicaid coverage differs. We addressed this issue by checking the sensitivity of the estimates to excluding observations from state‐years with such assigned coverage values. Some state coverage misclassifications may be present due to the possibility of reporting errors in the process of collecting and interpreting state Medicaid cessation coverage data (Singleterry et al. 2015), and coverage data for the District of Columbia (DC) were not available for 2011–2013. Second, because the NHIS survey did not collect information on the utilization of evidence‐based cessation services or the amount of copay for those services, we are unable to assess the direct impacts of Medicaid coverage or removing out‐of‐pocket costs on the use of these services (Fiore et al. 2008; CGTF 2016). Third, misidentification of past‐year insurance enrollment remains possible for some individuals, resulting in potential cross‐contamination between the treatment group of Medicaid beneficiaries and their low‐income, non‐Medicaid counterfactuals. However, a number of robustness checks indicate that the extent to which this limitation may affect the results was minimal. Fourth, Medicaid beneficiaries are expected to have different demographic characteristics from their within‐state low‐income counterparts because Medicaid eligibility is determined by certain demographic qualifiers. However, as long as these group differences are not systematically related to state variation in Medicaid cessation coverage, this would not be expected to confound the analysis estimates. Income data were missing for approximately 5 percent of the final sample, which can reduce the statistical power of the estimation. All covariates were measured as of time of survey and were used to retroactively determine their past‐year values, which may introduce measurement error. Finally, recall bias is possible in reporting past quitting behavior.
Results
In at least one of the years between 2008 and 2013, 29 states offered combined coverage, 25 states offered medication‐only coverage, and 7 states offered counseling‐only coverage. Four states and DC had no cessation coverage throughout the study period (Table 1). Unadjusted past‐year quit rates were comparable for Medicaid beneficiaries and low‐income adults not enrolled in Medicaid (8.4 and 8.85 percent, respectively; Table 2). Differences in quitting within those groups become apparent when stratified by type of coverage. For instance, quitting among Medicaid adults was higher in states with combined coverage (9.8 percent) compared to states without combined coverage (6.4 percent); in contrast, quitting among non‐Medicaid adults did not show as much variation across state Medicaid coverage policies.
Results from estimating Equation (1) indicate that combined Medicaid coverage of cessation counseling and medications was associated with increased quitting (Table 3). Coverage of medications only, coverage of counseling only, and presence of copayments and other barriers to use were not found to have a statistically significant effect on quitting among Medicaid beneficiaries relative to comparable non‐Medicaid adults. The estimated average treatment effect of introducing combined coverage of cessation counseling and medications on past‐year quit rates in Medicaid was 3.0 percentage points in the baseline specification (Table 3). Relative to the average past‐year quit rate among Medicaid beneficiaries of 8.4 percent, this corresponds to a semi‐elasticity of 0.33, indicating that combined coverage was associated with a 33 percent rise in the average past‐year quit rates. Past‐year quitting was positively associated with Hispanic ethnicity, being married, and being more educated, and it was negatively associated with age and being US‐born. The findings from the baseline model were robust to limiting the analysis to the 39 states with matching FFS‐MC coverage terms, where the average treatment effect of having combined coverage was estimated at 4.5 percentage points. The findings were also robust to adjusting for barriers to coverage, which were not found to have Medicaid‐specific effects on quitting. In the specification raising the income threshold for the low‐income comparison group from 150 to 250 percent of FPL, the average treatment effect was smaller and less significant than that in the baseline model, perhaps pointing to potentially larger relevance of coverage in lower‐income persons (Table 3). Because the variation in some coverage indicators, including counseling‐only coverage and presence of barriers, was relatively limited, it is possible that this might have attenuated the estimated effects.
Table 3.
Coefficients from Linear Probability Models of Recent Quitting, 2008–2013
| (1) | (2) | (3) | (4) | |
|---|---|---|---|---|
| Baseline sample | X | X | X | X |
| Include only state‐years with matching MC and FFS benefits (39 states) | X | |||
| Raise income threshold of low‐income comparison group not on Medicaid to 250% FPL | X | |||
| Control for barriers to coverage | X | |||
| Has Medicaid | −0.025 | −0.044 | −0.001 | −0.005 |
| (0.250) | (0.103) | (0.979) | (0.833) | |
| Coverage | ||||
| Medication only | 0.003 | 0.033 | 0.023 | 0.007 |
| (0.887) | (0.308) | (0.159) | (0.747) | |
| Counseling only | −0.009 | 0.021 | 0.026 | −0.003 |
| (0.733) | (0.816) | (0.260) | (0.908) | |
| Combined | 0.027 | 0.031 | 0.040** | 0.026 |
| (0.303) | (0.417) | (0.043) | (0.319) | |
| Interaction terms | ||||
| Medicaid × Medication‐only coverage | 0.010 | 0.033 | −0.005 | 0.015 |
| (0.585) | (0.166) | (0.772) | (0.466) | |
| Medicaid × Counseling only coverage | 0.043 | 0.036 | 0.017 | 0.035 |
| (0.102) | (0.619) | (0.504) | (0.193) | |
| Medicaid × Combined coverage | 0.030* | 0.045** | 0.018 | 0.037* |
| (0.100) | (0.048) | (0.298) | (0.075) | |
| Age | −0.001*** | −0.001* | −0.001*** | −0.001*** |
| (0.001) | (0.089) | (0.000) | (0.001) | |
| Male | −0.004 | −0.005 | −0.002 | −0.003 |
| (0.605) | (0.557) | (0.736) | (0.645) | |
| US born | −0.036*** | −0.028* | −0.015 | −0.038*** |
| (0.008) | (0.066) | (0.186) | (0.006) | |
| Married | 0.025*** | 0.034*** | 0.017*** | 0.023*** |
| (0.003) | (0.002) | (0.008) | (0.009) | |
| Race (relative to white) | ||||
| Hispanic | 0.023* | 0.022* | 0.038*** | 0.023* |
| (0.053) | (0.095) | (0.000) | (0.057) | |
| Black | −0.009 | −0.020** | −0.006 | −0.009 |
| (0.199) | (0.017) | (0.397) | (0.210) | |
| Other | −0.026* | −0.029 | −0.007 | −0.028* |
| (0.066) | (0.105) | (0.581) | (0.050) | |
| Education (relative to less than high school) | ||||
| High school or GED | 0.005 | 0.006 | 0.012* | 0.006 |
| (0.517) | (0.525) | (0.091) | (0.452) | |
| Some college or associate degree | 0.038*** | 0.040*** | 0.038*** | 0.038*** |
| (0.000) | (0.000) | (0.000) | (0.000) | |
| College degree or higher | 0.069*** | 0.064*** | 0.077*** | 0.070*** |
| (0.000) | (0.001) | (0.000) | (0.000) | |
| Health reported as poor/very poor | −0.002 | −0.001 | 0.001 | −0.006 |
| (0.802) | (0.890) | (0.836) | (0.449) | |
| Child under 18 in family | −0.012 | −0.010 | −0.013** | −0.012 |
| (0.127) | (0.255) | (0.030) | (0.111) | |
| Cigarette prices | 0.049 | 0.054 | 0.035 | 0.040 |
| (0.250) | (0.398) | (0.355) | (0.351) | |
| Medicaid × Copayment required | −0.020 | |||
| (0.192) | ||||
| Medicaid × Presence of barriers other than copayment | −0.012 | |||
| (0.379) | ||||
| n | 11,170 | 7,991 | 16,379 | 10,870 |
Notes: p‐Values in parentheses. Standard errors clustered by state. All models control for state fixed effects, year fixed effects, state‐specific time trends, and Medicaid‐specific time trend. *p < .10, **p < .05, ***p < .01.
Source: Authors’ analysis of data from the National Health Interview Survey 2009–2014.
We depicted differences in the outcome trends of treatment and comparison groups by plotting the average quit rates of each group over time (Figure 1). Because coverage changes occur in different years across states, the figure cannot depict average trends in relation to a defined pre‐ and postintervention point, nor can it be used to infer the presence or absence of parallel pre‐intervention trends. However, for illustrative purposes, it shows patterns that are consistent with the hypothesis of Medicaid coverage effects: A rise in the quit trends among Medicaid beneficiaries was observed for individuals in states that covered or started covering both counseling and medications during the study period, in contrast to flat or decreasing quit trends among groups without such coverage.
Figure 1.
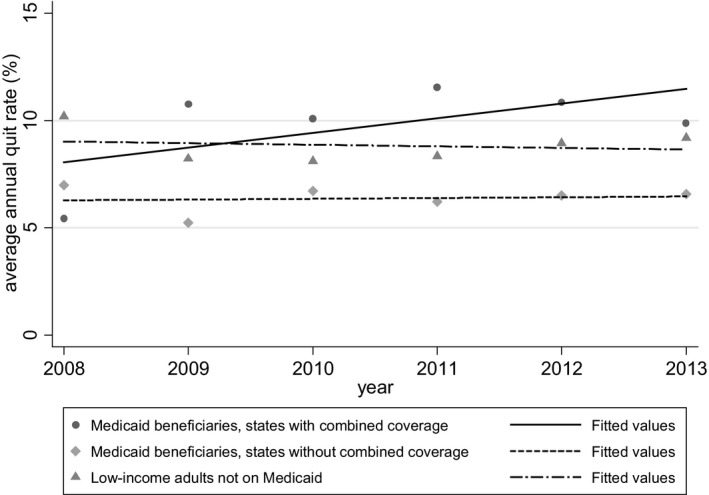
Average Quit Rates over Time, by Group
Source: Authors’ analysis of data from the National Health Interview Survey 2009–2014.
Summary estimates from the specification checks are presented in Table 4. Results from a model using the long‐term uninsured as the within‐state counterfactual to Medicaid beneficiaries were similar to those from the baseline estimation (dual‐coverage effect of 0.30 vs. 0.33, respectively). The placebo model using a pseudotreatment group of low‐income privately insured individuals revealed no Medicaid coverage effects, alleviating concerns about spurious trends shared by Medicaid beneficiaries and their privately insured counterfactuals in the baseline models. Finally, no precoverage differentials were detected among Medicaid beneficiaries relative to their non‐Medicaid counterparts, providing support for the baseline assumption that the main estimates reflect post‐treatment divergence in quit rates in the treatment group.
Table 4.
Select Coefficients from Robustness Models
| (0) | (1) | (2) | (3) | |
|---|---|---|---|---|
| Has Medicaid | −0.025 | −0.000 | 0.101** | −0.015 |
| (0.250) | (0.993) | (0.023) | (0.470) | |
| Coverage | ||||
| Medication only | 0.003 | 0.007 | −0.013 | −0.024 |
| (0.887) | (0.760) | (0.639) | (0.612) | |
| Counseling only | −0.009 | 0.020 | 0.036 | −0.110*** |
| (0.733) | (0.547) | (0.332) | (0.006) | |
| Combined | 0.027 | 0.027 | 0.020 | −0.054 |
| (0.303) | (0.290) | (0.593) | (0.358) | |
| Interaction terms | ||||
| Medicaid × Medication‐only coverage | 0.010 | 0.010 | 0.033 | |
| (0.585) | (0.609) | (0.304) | ||
| Medicaid × Counseling‐only coverage | 0.043 | 0.013 | −0.066 | |
| (0.102) | (0.677) | (0.105) | ||
| Medicaid × Combined coverage | 0.030* | 0.033* | 0.025 | |
| (0.100) | (0.096) | (0.429) | ||
| Precoverage indicators | ||||
| Medication only | −0.043 | |||
| (0.409) | ||||
| Counseling only | −0.107* | |||
| (0.062) | ||||
| Combined | −0.074 | |||
| (0.217) | ||||
| Interaction terms, precoverage indicators | ||||
| Medicaid × Medication‐only coverage | 0.025 | |||
| (0.249) | ||||
| Medicaid × Counseling‐only coverage | 0.024 | |||
| (0.565) | ||||
| Medicaid × Combined coverage | −0.024 | |||
| (0.310) | ||||
| n | 11,170 | 7,586 | 5,501 | 11,170 |
Notes: (0) Baseline model. (1) Sensitivity model where the within‐state comparison group is low‐income long‐term uninsured only. (2) Placebo model replacing the baseline Medicaid treatment group with a pseudotreatment group composed of low‐income privately insured adults; within‐state comparison group is low‐income long‐term uninsured. (3) Granger‐type specification with added indicators for the 2 years prior to actual change in coverage.
p‐Values in parentheses. Standard errors clustered by state. All models control for age, gender, nativity, marital status, race, education, children in household, health status, cigarette price, state fixed effects, year fixed effects, state‐specific time trends, and Medicaid‐specific time trend. *p < .10, **p < .05, ***p < .01.
Source: Authors’ analysis of data from the National Health Interview Survey 2009–2014.
Conclusion
We used the variation of Medicaid smoking cessation coverage during 2008–2013 across states and within states over time as well as between treatment and comparison groups within states to evaluate the effect of coverage on cigarette smoking cessation among Medicaid beneficiaries. The analysis indicated that combined state Medicaid coverage of cessation counseling and medications increased quit rates among Medicaid beneficiaries relative to low‐income persons not on Medicaid and Medicaid beneficiaries in states without such coverage. Coverage of cessation medications or counseling alone, as well as the presence of coverage barriers such as copayments, did not have a significant effect on cessation. These findings can contribute to a better understanding of how various elements in Medicaid cessation coverage may influence cessation outcomes.
Tobacco dependence is a chronic condition, with many smokers making repeated quit attempts before they achieve long‐term success (Fiore et al. 2008). Health care providers can draw on a number of evidence‐based treatment options to assist smokers in quitting, including counseling and medication. In the present study, combined coverage of cessation counseling and medications was found to increase quitting. This is consistent with the conclusion of the 2008 Public Health Service Clinical Practice Guideline and the 2015 U.S. Preventive Services Task Force tobacco cessation recommendation, which state that cessation counseling and FDA‐approved medications are more effective when used together (Fiore et al. 2008; Siu 2015).
The conclusions of this study are consistent with, and highlight the continued relevance of, previous studies that have found a significant association between improved state Medicaid cessation coverage and quitting smoking. Greene, Sacks, and McMenamin (2014) was the first study to evaluate the effects of Medicaid cessation coverage using temporal state coverage variation, albeit among a limited set of states and without within‐state counterfactuals; the present estimates expand the implications of this study to a nationally representative triple‐differencing framework. Similarly, although our study sample excluded pregnant women, the findings align with prior results for pregnant women (Adams et al. 2013), which found lower smoking rates in women with combined state Medicaid coverage of cessation counseling and medications than in women with coverage of medications only or no coverage. While the present analysis did not capture the effects of changes in Medicaid eligibility and coverage that occurred in 2014, when the Affordable Care Act Medicaid expansion and a federal provision barring state Medicaid programs from excluding cessation medications from coverage took effect, the results are consistent with the implications of recent research that compared smoking trends in expansion and nonexpansion states and linked Medicaid expansion to an approximate 1.9 percentage‐point reduction in cigarette smoking (Simon, Soni, and Cawley 2017), and to a 2.1 percentage‐point increase in recent quitting (Koma et al. 2017) among childless low‐income adults.
In summary, smoking continues to disproportionately affect the health and well‐being of lower‐income populations in the United States. Using recent data, this study provides evidence that combined coverage of both smoking cessation counseling and medication by state Medicaid programs could reduce cigarette smoking among Medicaid beneficiaries.
Supporting information
Appendix SA1: Author Matrix.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: Special thanks to Anne DiGiulio of the American Lung Association (ALA) for sharing ALA data on state Medicaid coverage of cessation counseling and medications and for assisting with the interpretation of these data. Special thanks to Karon Lewis for help with dataset management. The authors thank Brandy Lipton, Sandra Decker, Daniel Polsky, and the anonymous referees for valuable comments and suggestions.
Disclosures: None.
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- Adams, E. A. , Markowitz S., Dietz P. M., and Tong V. T.. 2013. “Expansion of Medicaid Covered Smoking Cessation Services: Maternal Smoking and Birth Outcomes.” Medicare and Medicaid Research Review 3 (3): E1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Lung Association . 2016. “State Tobacco Cessation Coverage. Updates and Historical Data Provided Through Correspondence with the American Lung Association” [accessed on April 1, 2017]. Available at http://www.lungusa2.org/cessation2/
- Blewett, L. A. , Rivera Drew J. A., Griffin R., King M. L., and Williams K.. 2016. IPUMS Health Surveys: National Health Interview Survey, Version 6.2. Minneapolis, MN: University of Minnesota. [Google Scholar]
- Carton, T. W. , Darden M., Levendis J., Lee S. H., and Ricket I.. 2016. “Comprehensive Indoor Smoking Bans and Smoking Prevalence: Evidence from the BRFSS.” American Journal of Health Economics 2 (4): 535–56. [Google Scholar]
- Centers for Medicare & Medicaid Services . 2017. “Medicaid Eligibility” [accessed on April 1, 2017]. Available at https://www.medicaid.gov/medicaid/eligibility/
- Community Guide Task Force on Community Preventive Services . 2016. “Reducing Tobacco Use and Secondhand Smoke Exposure: Reducing Out‐of‐Pocket Costs for Evidence‐Based Cessation Treatments Web Site” [accessed on April 1, 2017]. Available at http://www.thecommunityguide.org/tobacco/outofpocketcosts.html
- Courtemanche, C. J. , and Zapata D.. 2014. “Does Universal Coverage Improve Health? The Massachusetts Experience.” Journal of Policy Analysis and Management 33: 36–69. [DOI] [PubMed] [Google Scholar]
- Fiore, M. C. , Jaén C. R., Baker T. B., Bailey W. C., Benowitz N. L., Curry S. J., Dorfman S. F., Froelicher E. S., Goldstein M. G., Healton C. G., Henderson P. N., Heyman R. B., Koh H. K., Kottke T. E., Lando H. A., Mecklenburg R. E., Mermelstein R. J., Mullen P. D., Orleans C. T., Robinson L., Stitzer M. L., Tommasello A. C., Villejo L., Wewers M. E., Murray E. W., Bennett G., Heishman S., Husten C., Morgan G., Williams C., Christiansen B. A., Piper M. E., Hasselblad V., Fraser D., Theobald W., Connell M., and Leitzke C.. 2008. Treating Tobacco Use and Dependence: 2008 Update–Clinical Practice Guidelines, Rockville, MD: U.S. Department of Health and Human Services, Public Health Service, Agency for Healthcare Research and Quality. [Google Scholar]
- Greene, J. , Sacks R. M., and McMenamin S. B.. 2014. “The Impact of Tobacco Dependence Treatment Coverage and Copayments in Medicaid.” American Journal of Preventive Medicine 46 (4): 331–6. [DOI] [PubMed] [Google Scholar]
- Jamal, A. , King B. A., Neff L. J., Whitmill J., Babb S. D., and Graffunder C. M.. 2016. “Current Cigarette Smoking among Adults — United States, 2005–2015.” Morbidity and Mortality Weekly Report. 65 (44): 1205–11. [DOI] [PubMed] [Google Scholar]
- Kaiser Family Foundation . 2014. “Total Medicaid Managed Care Enrollment” [accessed on April 1, 2017]. Available at http://kff.org/medicaid/state-indicator/total-medicaid-mc-enrollment/
- Koma, J. W. , Donohue J. M., Barry C. L., Huskamp H. A., and Jarlenski M.. 2017. “Medicaid Coverage Expansions and Cigarette Smoking Cessation among Low‐Income Adults.” Medical Care. 55 (12): 1023–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ku, L. , Bruen B. K., Steinmetz E., and Bysshe T.. 2016. “Medicaid Tobacco Cessation: Big Gaps Remain in Efforts to Get Smokers to Quit.” Health Affairs. 35 (1): 62–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Land, T. , Warner D., Paskowsky M., Cammaerts A., Wetherell L., Kaufmann R., Zhang L., Malarcher A., Pechacek T., and Keithly L.. 2010. “Medicaid Coverage for Tobacco Dependence Treatments in Massachusetts and Associated Decreases in Smoking Prevalence.” PLoS ONE 5: e9770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, C. , and Dresler C. M.. 2012. “Medicaid Coverage and Utilization of Covered Tobacco‐Cessation Treatments: The Arkansas Experience.” American Journal of Preventive Medicine. 42 (6): 588–95. [DOI] [PubMed] [Google Scholar]
- Liu, F. 2009. “Effect of Medicaid Coverage of Tobacco‐Dependence Treatments on Smoking Cessation.” International Journal of Environmental Research and Public Health 6 (12): 3143–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maclean, J. C. , Pesko M. F., and Hill S. C.. 2017. The Effect of Insurance Expansion on Smoking Cessation Medication use: Evidence from Recent Medicaid Expansions. NBER Working Paper 23450.
- McMenamin, S. B. , Halpin H. A., Ibrahim J. K., and Orleans C. T.. 2004. “Physician and Enrollee Knowledge of Medicaid Coverage for Tobacco Dependence Treatments.” American Journal of Preventive Medicine. 26 (2): 99–104. [DOI] [PubMed] [Google Scholar]
- McMenamin, S. , Halpin H., Bellows N., Husten C., and Rosenthal A.. 2009. “State Medicaid Coverage for Tobacco‐Dependence Treatments—U.S., 2007.” Morbidity and Mortality Weekly Report 58 (43): 1199–204. [PubMed] [Google Scholar]
- McMenamin, S. , Halpin H., Ingram M., and Rosenthal A.. 2010. “State Medicaid Coverage for Tobacco‐Dependence Treatments—U.S., 2009.” Morbidity and Mortality Weekly Report 59 (41): 1340–2. [PubMed] [Google Scholar]
- Murphy, J. M. , Mahoney M. C., Hyland A. J., Higbee C., and Cummings K. M.. 2005. “Disparity in the Use of Smoking Cessation Pharmacotherapy among Medicaid and General Population Smokers.” Journal of Public Health Management and Practice 11 (4): 341–5. [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics . 2016. “National Health Interview Survey 2009–2014. Public‐use Data File and Documentation” [accessed on April 1, 2017]. Available at http://www.cdc.gov/nchs/nhis/data-questionnaires-documentation.htm
- Orzechowski, W. , and Walker R.. 2014. The Tax Burden on Tobacco: Historical Compilation, Volume 49. Arlington, VA: Orzechowski & Walker Consulting. [Google Scholar]
- Simon, K. , Soni A., and Cawley J.. 2017. “The Impact of Health Insurance on Preventive Care and Health Behaviors: Evidence from the First Two Years of the ACA Medicaid Expansions.” Journal of Policy Analysis and Management 36 (2): 390–417. [DOI] [PubMed] [Google Scholar]
- Singleterry, J. , Jump Z., DiGiulio A., Babb S., Sneegas K., MacNeil A., Zhang L., and Williams K. S.. 2015. “State Medicaid Coverage for Tobacco Cessation Treatments and Barriers to Coverage – United States, 2014–2015.” Morbidity and Mortality Weekly Report. 64 (42): 1194–9. [DOI] [PubMed] [Google Scholar]
- Siu, A. L. , and for the U.S. Preventive Services Task Force . 2015. “Behavioral and Pharmacotherapy Interventions for Tobacco Smoking Cessation in Adults, Including Pregnant Women: U.S. Preventive Services Task Force Recommendation Statement.” Annals of Internal Medicine 163: 622–34. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services . 2014. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, CDC; Available at http://www.surgeongeneral.gov/library/reports/50-years-of-progress/full-report.pdf [Google Scholar]
- Xu, X. , Bishop E. E., Kennedy S. M., Simpson S. A., and Pechacek T. F.. 2015. “Annual Healthcare Spending Attributable to Cigarette Smoking: An Update.” American Journal of Preventive Medicine. 48 (3): 326–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.


