Abstract
Purpose
A new magnetic resonance imaging (MRI) based scoring system for temporomandibular joint (TMJ) internal derangement was developed to predict disease severity and the likelihood of invasive treatment.
Patients and methods
Reports and images from bilateral TMJ MRI studies of 100 consecutive patients with TMJ pain were retrospectively reviewed. A Temporomandibular Joint Internal Derangement Score (TIDS) score was composed of 6 MRI characteristics: joint effusion, disc displacement, disc nonrecapture, disc degenerative changes, abnormal condyle translation, and condyle arthritis. The primary endpoint was whether disease severity merited invasive treatment (arthrocentesis, arthroscopy, arthroplasty, or discectomy). Primary analyses were conducted as univariate regression, with the level of significance set at p < .05. Multivariate regression was also used to assess the impacts of each variable upon the need for invasive treatment.
Results
Invasive treatment was performed in 29 patients and planned in an additional 9 patients. Patients with clinical bilateral pathology were no more likely to undergo invasive treatment than those with unilateral clinical pathology. Statistically significant correlations were found between bilateral invasive treatment and the presence of bilateral joint effusions (p = 0.0037) and disc displacement (p = 0.014), as well as with increasing values of right TIDS (p = 0.0015) and bilateral TIDS (p = 0.0090). Bilateral TIDS of greater than 6 was correlated with both bilateral invasive treatment (p = 0.0033) and with invasive treatment of any kind (p = 0.041). In each instance of TIDS > 6, the patient demonstrated multiple signs of bilateral TMJ pathology. On multivariate regression, only disc recapture failed to trend towards statistical significance in both the six and twelve component regressions, which trended towards significance only in the twelve component analysis.
Conclusion
A TIDS score was developed to serve as an adjunct to the clinical assessment of TMJ pathology. Bilateral TIDS score greater than 6 was statistically significantly correlated with the severity of TMJ pathology.
Keyword: Medical imaging
1. Introduction
Temporomandibular disorders are a varied collection of disorders, yet they often go untreated because as few as 3–7% of patients with temporomandibular joint (TMJ) pain seek medical attention [1]. The classification systems used until now classify temporomandibular disorders according to the Research Diagnostic Criteria for Temporomandibular Disorders into 3 subgroups: muscle disorders (Group I); disc displacements (Group II); and arthralgia, arthritis, and arthrosis (Group III) [2]. These, however, often coexist and can offer unclear guidelines for management, including splint therapy, arthrocentesis, arthroscopic lysis, lavage, arthrotomy, and discectomy, as well as total joint reconstruction [3].
Though effective for the identification of pain [4], the sensitivity and specificity of the clinical examination for temporomandibular disorders has been questioned in the literature, with the most accurate tests (clicks and crepitus) only accurately identifying joint effusion (JE) in 78.7% of cases [5]. Chaput's review of 8 studies demonstrated a failure of click, deviation, and pain to rule out internal derangement with reduction, and he recommended further studies in this field [6]. It has been shown that clinical accuracy fails with disc displacement without reduction [7]. While other imaging modalities, such as ultrasound, have been used [8], magnetic resonance imaging (MRI) has proven to be most effective for augmenting the clinical picture, whether in the oral maxillofacial or the dental setting [9]. Full clinical agreement with imaging has been found to be as low as 43% [10], necessitating the use of both imaging and physical examination in severe disease and for surgical planning [11].
Various imaging findings have been studied both in isolation and partially in relationship to one another, such as the work of Roh analyzing disc displacement, joint effusion, and degenerative changes [12]. Their individual associations with pain and dysfunction [13, 14] and their utilities as prognostic indicators for arthrocentesis have been partially analyzed [3]. Suenaga associated pain syndromes with internal derangement, joint effusion, osteoarthritis, and bone marrow edema [15], whereas others have focused on disc displacement and arthralgia [16]. An emphasis has also been placed on the disc-condyle relationship [17], even irrespective of disc displacement or arthritis [18]. Especially after mandibular condyle fracture, joint effusion has been used as a marker of TMJ disease severity [19]. Orlando supported joint effusion's importance and noted a relationship between joint effusion and disc displacement [20]. Regarding prognostic implications, TMJ osteoarthritis has proven itself as a key indicator of successful arthrocentesis [21]. MRI also serves to identify temporomandibular disorders mimics, such as rheumatoid arthritis presenting with synovial proliferation [22, 23]. Finally, while clinical signs such as contralateral ramus height [24] are insufficient to diagnose contralateral TMJ pathology in patients presenting with unilateral findings, MRI often can do so [25]. As of this writing, no study completely describes the predictive power of the multiple imaging abnormalities found on MRI on treatment choices and clinical outcomes.
To better understand the clinical significance of multiple MRI TMJ imaging findings on the rate of invasive procedures in the management of temporomandibular disorders, a simple yet comprehensive grading system was developed [26]. A TMJ internal derangement score (TIDS) was assigned 1 point for the presence of each of the following: joint effusion, disc displacement, disc non-recapture, disc degeneration, abnormal condyle translation, and condyle arthritis. Right, left, and bilateral composite scores were calculated for a set of 100 consecutive patients referred for MRI for pain and dysfunction of the TMJ, with the hypothesis that such a score would offer clinically useful prognostic value. This novel effort serves to synthesize the varied conclusions obtained in the literature and develop a composite TIDS score to predict disease severity and the likelihood of invasive treatment of temporomandibular disorders.
2. Methods
2.1. Patients and statistical analysis
Reports and images from bilateral TMJ MR imaging studies of 100 consecutive patients with TMJ pain from January 2005 to March 2012 were reviewed. This study group comprised of 82 females and 18 males, with a mean age of 38.9 (Table 1). Inclusion criteria were the presence of clinical unilateral or bilateral TMJ pain or dysfunction. No patients were excluded and consecutive patients were selected to more accurately portray the population of significant TMJ pathology in clinical practice. Indications for MRI were based on clinical diagnoses of TMJ pericapsular pain associated with clinically palpable clicking or malocclusion, audible clicking with stethoscope, intermittent jaw locking, decreased jaw opening despite conservative therapy, and arthritis diagnosed on conventional radiography (Panorex). Clinical assessments were conducted prior to MRI, approximately one month post-MRI, and three to six months post-MRI; the assessment scale ranged from 1 to 5, corresponding to minimal to severe symptoms. The oromaxillofacial surgeon completed survey questions before and after the MRI indicating whether the MRI findings changed therapeutic management and/or increased diagnostic confidence.
Table 1.
Patient characteristics: Basic patient characteristics were compiled (n = 100).
| Patient characteristics | Number of patients |
|---|---|
| Gender | |
| Female | 82 |
| Male | 18 |
| MRI pathology | |
| Unilateral | 18 |
| Bilateral | 78 |
| Nonea | 4 |
| Invasive treatment | |
| Unilateral | 7 |
| Bilateral | 31 |
| Any | 38 |
Note: Four patients were originally signed out with negative impressions, although each had one or more TIDS component described in the findings.
All MRI studies were initially interpreted by one of the faculty's board-certified fellowship-trained musculoskeletal radiologists per usual practice. The radiologists were blinded to pre- and post-imaging treatment decision-making and outcomes, which were recorded by the oral maxillofacial surgeon. The six components of the TIDS score were standard reported items when reviewing MRIs of the TMJ, minimizing observational bias. Due to the retrospective nature of this study, institutional review board approval was not required for this study. Helsinki declaration guidelines were followed for this investigation.
The primary endpoint for the study was whether disease severity merited invasive treatment (arthrocentesis, arthroscopy, arthroplasty, or discectomy). Additional data collected included: the type of invasive treatment conducted, whether the treatment was unilateral or bilateral, and whether additional invasive treatment was planned but not performed.
A modified intention-to-treat approach was used, in which all patients receiving TMJ MRI were included in the analysis of the primary outcome, regardless of follow up status. Primary analyses were conducted as univariate regression, with the level of significance set at p < .05. Multivariate regression was also used to assess the impacts of each variable upon the need for invasive treatment.
2.2. Magnetic resonance imaging
MRI of the bilateral temporomandibular joints was performed on a 1.5 Tesla magnet (General Electric; Milwaukee, WI, USA) with a dedicated circular-polarized transmit-and-receive TMJ coil per usual protocol including the following: localizer images; oblique sagittal T1, oblique sagittal proton density (PD), oblique sagittal T2, and oblique coronal T1 closed mouth sequences; oblique sagittal PD open mouth sequence. A nonferromagnetic oral device was used to obtain a reproducible open mouth position and to reduce motion.
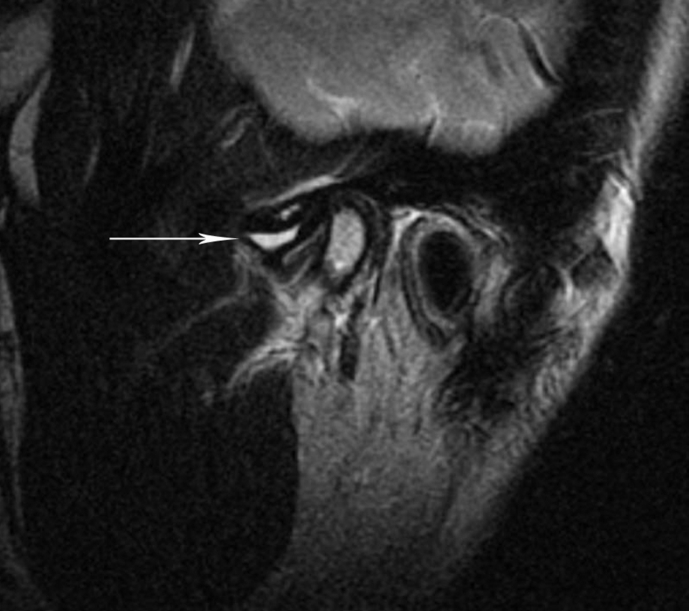
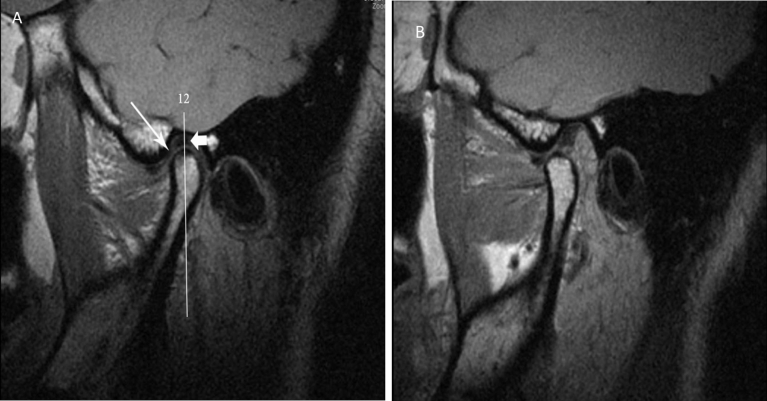
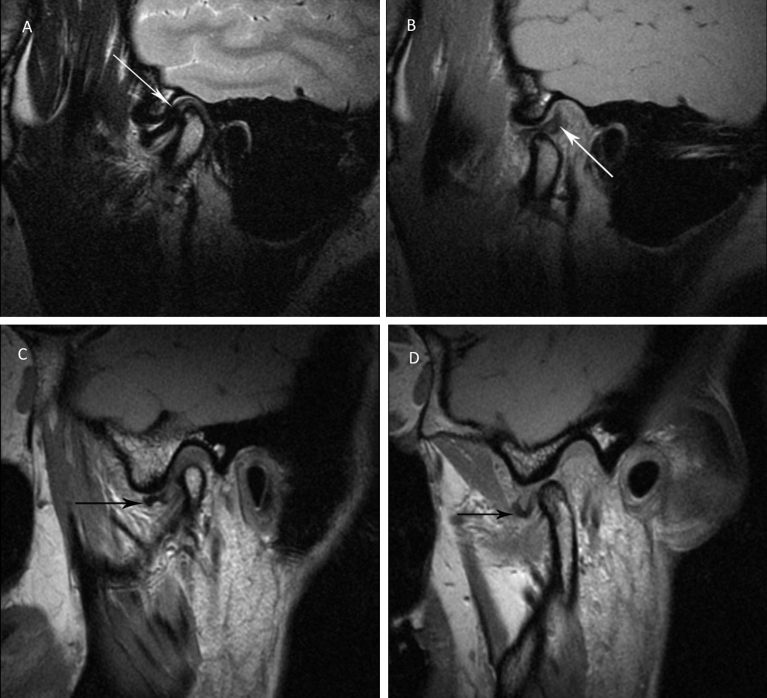
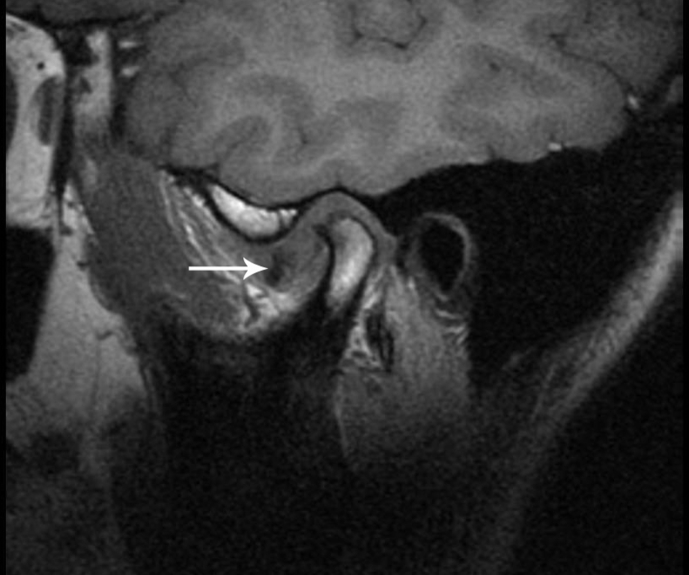
The presence of a joint effusion was identified when there was more than trace high T2 signal within the joint space (Fig. 1). Normal disc position of the disc was defined by the location of the posterior band of the disc at the superior or 12 o'clock position relative to the mandibular condyle and the interposition of intermediate zone of the disc between the mandibular condyle and the posterior temporal eminence in the closed-mouth position (Fig. 2); abnormal anterior, anteromedial, anterolateral, medial, lateral, posterior, posteromedial, and posterolateral disc displacements were defined by the location of the posterior band beyond greater than 10°, which included both disc subluxation (10–30°) and frank dislocation (greater than 30°). Disc nonrecapture was defined as the lack of recapture of a displaced disc in the open mouth position (Fig. 3). Disc degeneration was defined as increased T1, PD, or T2 signal within the substance of the disc, abnormal disc morphology, or disc perforation (Fig. 4). Normal condylar translation was defined as anterior translation of the mandibular condyle in the open mouth position such that the condyle was under the temporal eminence; abnormal condylar translation was the lack of normal condylar translation (Fig. 2). Condylar arthritis was defined as the presence of joint space narrowing, sclerosis, osteophytosis, subchondral cysts, erosions, marrow edema, and/or abnormal condyle morphology (Fig. 5).
Fig. 1.
Joint effusion: Oblique sagittal T2 weighted magnetic resonance image of the temporomandibular joint in the closed mouth position demonstrates an area of high signal intensity (arrow) that represents a moderate effusion.
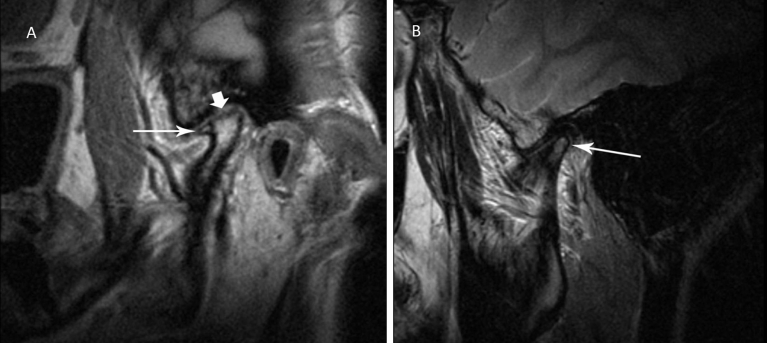
Fig. 2.
TMJ disc location and translation: Oblique sagittal proton density magnetic resonance images of the temporomandibular joint (A) in the closed mouth position demonstrate normal disc position. The angle between the posterior band (short white arrow) and the 12-o'clock line is less than ±10°. Normal disc morphology is seen with the intermediate zone (white arrow) interposed between the articular condyle and temporal bone. The same sequence in the open mouth position (B) demonstrates normal condylar translation and expected disc position between the condyle and temporal eminence centered in the intermediate zone.
Fig. 3.
Disc displacement with and without recapture: Oblique sagittal T2 weighted magnetic resonance images of the temporomandibular joint demonstrate that the disc is anteriorly displaced in the closed mouth position (arrow, A) but returns to the normal position – between the condyle and temporal eminence (recapture) on open mouth proton density sequence (arrow, B). Oblique sagittal proton density magnetic resonance image of the temporomandibular joint demonstrates that the disc is anteriorly displaced in the closed mouth position (arrow, C) and remains displaced (no recapture) from its normal location in open mouth position (arrow, D).
Fig. 4.
Deformed, degenerated, and displaced TMJ disc: Oblique sagittal T1 weighted magnetic resonance image of the temporomandibular joint demonstrates a deformed degenerated disc with abnormal intrinsic signal intensity and anterior disc displacement (arrow).
Fig. 5.
Condylar arthritis: Oblique sagittal proton density and T2 weighted magnetic resonance images of the temporomandibular joints demonstrate anterior spurring (long arrow, A), flattening of the condyle (short arrow, A), and bone marrow edema (arrow, B).
The presence and laterality of the following six MRI findings were assessed and recorded as present or absent: joint effusion, disc displacement, disc nonrecapture, disc degeneration, abnormal condylar translation, and condylar arthritis. 1 point was assigned for each MRI finding per side. The TMJ Internal Derangement Score (TIDS) was the summation score. Possible total score values ranged from 0 (normal MRI examination) to 12 (bilateral presence of all of the above mentioned findings), and from 0 to 6 for either right or left sides alone.
3. Results
3.1. TIDS characteristics
The presence of the six components of the TIDS score were individually evaluated and tabulated for each patient: joint effusion (JE), disc displacement (DDisp), disc nonrecapture (DNR), disc degenerative changes (DDeg), abnormal condyle translation (ACT), and condyle arthritis (CA). The laterality of each of these findings was also recorded (Table 2).
Table 2.
MRI findings: The spread of MRI findings in the patient cohort includes joint effusion (JE), disc displacement (DDisp), disc nonrecapture (DNR), disc degeneration (DDeg), abnormal condyle translation (ACT), and condyle arthritis (CA).
| Finding | None | Right | Left | Bilateral |
|---|---|---|---|---|
| JE | 58 | 8 | 11 | 23 |
| DDisp | 20 | 19 | 15 | 46 |
| DNR | 17 | 17 | 19 | 47 |
| DDeg | 49 | 17 | 4 | 30 |
| ACT | 31 | 13 | 13 | 43 |
| CA | 51 | 17 | 9 | 23 |
TIDS scores were calculated as a right-sided score, a left-sided score, and a bilateral composite score. The right-sided scores ranged from 1 to 6, the left-sided scores ranged from 1 to 5, and the composite scores ranged from 2 to 11.
3.2. Treatments and outcomes
Seventy five patients returned for follow-up. 29 of these patients underwent invasive treatment of some kind while invasive treatment was planned for an additional 9 patients. Out of 9 invasive procedures scheduled, arthrocentesis was planned in 3 cases, orthognathic surgery in 4 cases, and steroid injections in 2 cases. There was no statistically significant difference between the number of invasive procedures planned or performed in patients with bilateral TMJ pathology when compared to patients with unilateral TMJ pathology. All treatments performed and recommended were tabulated below (Table 3).
Table 3.
Treatment strategies: The number of patients with each treatment strategy in the patient cohort was tabulated. Please note that some patients had multiple treatments.
| Treatment strategy | Count |
|---|---|
| Oral splint therapy | 26 |
| Physical therapy | 57 |
| NSAIDs/muscle relaxants | 35 |
| Arthrocentesis | 19 |
| Arthroscopy | 0 |
| Arthroplasty | 5 |
| Discectomy | 6 |
| Total joint replacement | 0 |
| Invasive procedure planned | 9 |
Regarding clinical correlation, the pre-clinical assessment was found to have a mean score of 2.04 (range: 1–5), and it correlated with the need for unilateral treatment (p = 0.02), any invasive treatment performed (p = 0.002), and any invasive treatment needed (p = 0.005). The pre-clinical assessment, however, was not statistically correlated with unilateral or bilateral TIDS. Early and late post-treatment clinical assessments were not correlated with invasive treatment or TIDS. In the early post-treatment period, only 24% of patients improved, but with further time and therapy, 95% of patients improved in the late post-treatment period. 95% of patients overall had clinical improvement, with a mean improvement of 2.45 for patients requiring invasive treatment versus 1.71 for patients receiving other treatments. Finally, survey results showed that MRI changed management in 12% of cases and increased confidence in 93% of patients.
Statistically significant correlations (Table 4) were found between bilateral invasive treatment and the presence of bilateral joint effusions (p = 0.0037) and disc displacement (p = 0.014), as well as with increasing values of right TIDS (p = 0.0015) and bilateral TIDS (p = 0.0090). Any invasive treatment was correlated with bilateral joint effusions (p = 0.041) and higher right TIDS (p = 0.011). Furthermore, a bilateral TIDS of greater than 6 was correlated with both bilateral invasive treatment (p = 0.0033) and with invasive treatment of any kind (p = 0.041). Odds ratio trends for invasive treatment with joint effusion and condyle arthritis were 2.0 (0.89–4.6 [95% C.I.]; p = 0.09) and 2.1 (0.93–4.8 [95% C.I.]; p = 0.07), respectively.
Table 4.
Univariate analysis: The p values describe the correlation between various components of the TIDS score and invasive treatments. Note JE = joint effusion, DDisp = disc displacement, and CA = condyle arthritis.
| Bilateral invasive | Any invasive | |
|---|---|---|
| Bilateral JE | 0.0037 | 0.041 |
| Bilateral DDisp | 0.0145 | 0.30 |
| Bilateral CA | 0.0508 | 0.27 |
| Right unilateral TIDS | 0.0015 | 0.011 |
| Bilateral TIDS | 0.0090 | 0.070 |
Multivariate regression was conducted for bilateral and individual joints. For pathology requiring bilateral invasive treatment, the presence of bilateral joint effusion (p = 0.0016) and abnormal translation (p = 0.038) were statistically significant while bilateral displacement (p = 0.078), condyle degeneration (p = 0.091), and disc degeneration (p = 0.11) trended towards significance. When the analysis was expanded to 12 variables for the left and right components of each variable, right and left joint effusion (p = 0.0097 and p = 0.00067, respectively), left disc displacement (p = 0.011), left disc degeneration (p = 0.034), and left condyle degeneration (p = 0.023) reached statistical significance while right and left abnormal translation trended towards significance (p = 0.068 for each). Twelve variable regression for the need for any invasive treatment showed statistical significance for left joint effusion (p = 0.021), left disc displacement (p = 0.020), and left condyle degeneration (p = 0.013), as well as a trend towards significance for left disc recapture (p = 0.088).
4. Discussion
A bilateral composite TMJ internal derangement score (TIDS) greater than 6 was found to have a statistically significant correlation with severity of TMJ pathology, as evidenced by the requirement for bilateral invasive treatment or any invasive treatment. A value greater than 6 requires bilateral pathology, and at least one side must demonstrate at least 4 MRI findings of disease severity. Interestingly, in this patient cohort, each such case also demonstrated at least 2 findings of contralateral disease. In the two cases in which a unilateral TIDS score of 6 was assigned, the patients had composite TIDS scores of 11 and 10. Thus, in each instance of TIDS > 6, the patient also demonstrated multiple findings of TMJ pathology bilaterally, indicating that severity of bilateral disease may be an important factor in the TIDS threshold.
While the clinical examination can localize pain to the TMJ, failing to observe severe asymptomatic disease results in false negatives that underestimate the likelihood of requiring invasive treatment [27]. Conversely, the high rate of osteoarthritis on TMJ imaging [28, 29], which varies widely by age group (25% in 20–49 but 70% in 73–75), could raise concerns about false positives on imaging [10, 27, 30, 31]. Indeed, in each case of a unilateral clinical presentation, at least one of the six criteria was identified on the contralateral side on MRI. However, using the TIDS score, an incidental finding of contralateral degeneration alone would not necessarily indicate the need for invasive treatment without the presence of additional TIDS components, mitigating concerns about false positives. In addition, a subthreshold TIDS score, especially in the presence of alternative MRI findings, would allow surgeons to avoid unnecessary surgery for many myofascial pain mimics.
The pre-clinical score was found to be correlated with the need for invasive treatment, but the score was not correlated with TIDS. These results are consistent with the literature discussing the lack of concordance between imaging and clinical aspects of TMJ pathology [10]. Therefore, TIDS serves as a useful adjunct to further describe the severity of a patient's pathology. This conclusion is supported by survey results which showed that imaging increased diagnostic confidence in 93% of cases and changed management in 12% of patients. The result that post-treatment clinical assessments were not correlated with the need for invasive treatment could indicate that those patients with symptoms were adequately treated. Since those patients with severe symptoms were more likely to receive invasive treatment, they subsequently had a greater improvement in symptoms and thus lowered their clinical assessment scores.
Overall, multivariate and univariate regression results were consistent with the initial hypothesis that each of the six components served to add to the prognostic value of the TIDS score. On univariate regression, bilateral joint effusions and disc displacement were correlated with bilateral invasive treatment while bilateral condyle arthritis trended towards significance. Joint effusion and condyle arthritis both had odds ratio trends (OR) > 2, consistent with findings in the literature regarding the importance of these variables [7, 12, 17, 19, 20]. On multivariate regression, only disc recapture failed to trend towards statistical significance in both the six and twelve component regressions; however, it trended towards significance in predicting the need for any invasive treatment (p = 0.088) in the twelve component analysis.
This study possesses intrinsic strengths and weaknesses. This study's sample size is similar to many studies considering clinical and MRI factors indicative of TMJ pathology, which have ranged from 61 to 149 patients [4, 5]. Nevertheless, only 18 patients had unilateral symptoms, which may explain why the left TIDS score did not achieve statistical significance in the secondary unilateral analysis; we hypothesize that with a larger sample size, statistical significance might have been demonstrated. Furthermore, sample size proved insufficient to rigorously develop a weighted grading system to account for individual component severities and their relative impacts. Requiting this lack of nuance, the TIDS score is simple and straightforward. It can be readily grasped and applied clinically, thereby potentially making it more clinically useful than a more complex scoring system. Additionally, regarding the referral process, individuals referred for MRI of the TMJ often present with significant pathology (e.g. for surgical planning), which could introduce a selection bias relative to the 25% or higher group of the overall population suffering from temporomandibular joint pathology [1, 32, 33]. Finally, future research to determine TIDS scores in asymptomatic or minimally symptomatic patients would be of great interest.
While this paper does not directly address why an MRI might be ordered for a specific patient in actual practice, we suspect that patients with greater symptoms may be more likely to undergo evaluation with MRI. Then, once the MRI is obtained, TIDS can help stratify patients for appropriate treatment. It may be intuitive that patients with more MRI findings may have a higher likelihood of needing invasive treatment, but even in our population of generally challenging diagnostic or treatment cases, the majority of patients did not require invasive treatment, thereby avoiding costs and possible side effects of unnecessary invasive treatments.
5. Conclusion
Analysis of treatments and outcomes after MRI imaging for temporomandibular disorders led to the development of a TIDS score composed of 6 MRI characteristics: joint effusion, disc displacement, disc nonrecapture, disc degenerative changes, abnormal condyle translation, and condyle arthritis. This score serves as a useful adjunct to the initial clinical assessment. A bilateral TIDS score greater than 6 was found to have a statistically significant correlation with severity of TMJ pathology, as evidenced by the requirement for bilateral invasive treatment or any invasive treatment. This result indicates that the presence of multiple imaging characteristics of TMJ disease bilaterally may be an important factor predictive of invasive treatment.
Declarations
Author contribution statement
Roman Michael Kowalchuk: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Jolly M. Caplash, Penelope B. Block: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data.
Roman O. Kowalchuk, Katia Kaplan-List: Contributed reagents, materials, analysis tools or data; Wrote the paper.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Competing interest statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
References
- 1.Bag Asim K. Imaging of the temporomandibular joint: an update. World J. Radiol. 2014;6(8):567. doi: 10.4329/wjr.v6.i8.567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lobbezoo F., Drangsholt M., Peck C., Sato H., Kopp S., Svensson P. Topical review: new insights into the pathology and diagnosis of disorders of the temporomandibular joint. J. Orofac. Pain. 2004 Summer;18(3):181–191. PMID: 15508997. [PubMed] [Google Scholar]
- 3.Emshoff Rüdiger, Rudisch Ansgar. Temporomandibular joint internal derangement and osteoarthrosis: are effusion and bone marrow edema prognostic indicators for arthrocentesis and hydraulic distention? J. Oral Maxillofac. Surg. January 2007;65(1):66–73. doi: 10.1016/j.joms.2005.11.113. [DOI] [PubMed] [Google Scholar]
- 4.Ohlmann Brigitte. Prediction of TMJ arthralgia according to clinical diagnosis and MRI findings. Int. J. Prosthod. 2006;19(4) PMID: 16900815. [PubMed] [Google Scholar]
- 5.Manfredini Daniele. Predictive value of clinical findings for temporomandibular joint effusion. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2003;96(5):521–526. doi: 10.1016/s1079-2104(03)00475-x. [DOI] [PubMed] [Google Scholar]
- 6.Chaput Ève. The diagnostic validity of clinical tests in temporomandibular internal derangement: a systematic review and meta-analysis. Physiother. Canada. 2012;64(2):116–134. doi: 10.3138/ptc.2010-54. Epub 2012 Apr 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tognini F. Is clinical assessment valid for the diagnosis of temporomandibular joint disk displacement? Minerva Stomatol. 2004;53(7-8):439–448. PMID: 15278022. [PubMed] [Google Scholar]
- 8.Weiss Pamela F. High prevalence of temporomandibular joint arthritis at disease onset in children with juvenile idiopathic arthritis, as detected by magnetic resonance imaging but not by ultrasound. Arthritis Rheumatol. 2008;58(4):1189–1196. doi: 10.1002/art.23401. [DOI] [PubMed] [Google Scholar]
- 9.Simmons H. Clifton, III, Julian Gibbs S. Initial TMJ disk recapture with anterior repositioning appliances and relation to dental history. CRANIO®. 1997;15(4):281–295. doi: 10.1080/08869634.1997.11746022. PMID: 9481990. [DOI] [PubMed] [Google Scholar]
- 10.Paesani Daniel. Accuracy of clinical diagnosis for TMJ internal derangement and arthrosis. Oral Surg. Oral Med. Oral Pathol. 1992;73(3):360–363. doi: 10.1016/0030-4220(92)90135-d. PMID: 1545969. [DOI] [PubMed] [Google Scholar]
- 11.Vogl Thomas J. The value of MRI in patients with temporomandibular joint dysfunction: correlation of MRI and clinical findings. Eur. J. Radiol. 2016;85(4):714–719. doi: 10.1016/j.ejrad.2016.02.001. [DOI] [PubMed] [Google Scholar]
- 12.Roh H.S., Kim W., Kim Y.K., Lee J.Y. Relationships between disk displacement, joint effusion, and degenerative changes of the TMJ in TMD patients based on MRI findings. J. Craniomaxillofac. Surg. 2012 Apr;40(3):283–286. doi: 10.1016/j.jcms.2011.04.006. Epub 2011 Jul 13. [DOI] [PubMed] [Google Scholar]
- 13.Tore A. Larheim, Per-Lennart Westesson, Tsukasa Sano. MR grading of temporomandibular joint fluid: association with disk displacement categories, condyle marrow abnormalities and pain. Int. J. Oral Maxillofac. Surg. April 2001;30(2):104–112. doi: 10.1054/ijom.2000.0017. [DOI] [PubMed] [Google Scholar]
- 14.Emshoff R., Brandlmaier I., Bertram S., Rudisch A. Relative odds of temporomandibular joint pain as a function of magnetic resonance imaging findings of internal derangement, osteoarthrosis, effusion, and bone marrow edema. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2003 Apr;95(4):437–445. doi: 10.1067/moe.2003.95. [DOI] [PubMed] [Google Scholar]
- 15.Suenaga Shigeaki. The usefulness of diagnostic imaging for the assessment of pain symptoms in temporomandibular disorders. Jpn. Dent. Sci. Rev. 2016;52(4):93–106. doi: 10.1016/j.jdsr.2016.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shaefer Jeffry R. Analysis of criteria for MRI diagnosis of TMJ disc displacement and arthralgia. Int. J. Dent. 2012;2012 doi: 10.1155/2012/283163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yang Zhongjun. Magnetic resonance imaging (MRI) evaluation for anterior disc displacement of the temporomandibular joint. Med. Sci. Mon. Int. Med. J. Exp. Clin. Res. 2017;23:712. doi: 10.12659/MSM.899230. PMID: 28176754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Takatsuka Shigeyuki. Disc and condyle translation in patients with temporomandibular disorder. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2005;99(5):614–621. doi: 10.1016/j.tripleo.2004.08.024. [DOI] [PubMed] [Google Scholar]
- 19.Takahashi Tetsu. Magnetic resonance evidence of joint effusion of the temporomandibular joint after fractures of the mandibular condyle: a preliminary report. CRANIO®. 2004;22(2):124–131. doi: 10.1179/crn.2004.016. [DOI] [PubMed] [Google Scholar]
- 20.Orlando Bruno. Risk of temporomandibular joint effusion related to magnetic resonance imaging signs of disc displacement. Med. Oral Patol. Oral Cir. Bucal. 2009;14(4):E188–E193. PMID: 19333188. [PubMed] [Google Scholar]
- 21.Emshoff R., Rudisch A., Bösch R., Strobl H. Prognostic indicators of the outcome of arthrocentesis: a short-term follow-up study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2003 Jul;96(1):12–18. doi: 10.1016/s1079-2104(03)00219-1. [DOI] [PubMed] [Google Scholar]
- 22.Larheim T.A. Role of magnetic resonance imaging in the clinical diagnosis of the temporomandibular joint. Cells Tissues Organs. 2005;180(1):6–21. doi: 10.1159/000086194. [DOI] [PubMed] [Google Scholar]
- 23.Yilmaz Hasan Huseyin. Clinical and magnetic resonance imaging findings of the temporomandibular joint and masticatory muscles in patients with rheumatoid arthritis. Rheumatol. Int. 2012;32(5):1171–1178. doi: 10.1007/s00296-010-1743-4. [DOI] [PubMed] [Google Scholar]
- 24.Ahn Sug-Joon, Lee Seung-Pyo, Nahm Dong-Seok. Relationship between temporomandibular joint internal derangement and facial asymmetry in women. Am. J. Orthod. Dentofac. Orthop. 2005;128(5):583–591. doi: 10.1016/j.ajodo.2004.06.038. [DOI] [PubMed] [Google Scholar]
- 25.de Leeuw Reny. Hard and soft tissue imaging of the temporomandibular joint 30 years after diagnosis of osteoarthrosis and internal derangement. J. Oral Maxillofac. Surg. 1996;54(11):1270–1280. doi: 10.1016/s0278-2391(96)90480-2. PMID: 8941176. [DOI] [PubMed] [Google Scholar]
- 26.Kowalchuk R.M., Kaplan-List K., Caplash J.M., Block P. ACR Annual Meeting and Chapter Leadership Conference (AMCLC), Washington, D.C. 2014. Temporomandibular joint(TMJ) Internal Derangement Score (TIDS): a New MRI-Based Scoring System for TMJ Internal Derangement: patient stratification based on the degree of TMJ pathology can help guide the most appropriate treatment. [Google Scholar]
- 27.Haley Dennis P. The relationship between clinical and MRI findings in patients with unilateral temporomandibular joint pain. J. Am. Dent. Assoc. 2001;132(4):476–481. doi: 10.14219/jada.archive.2001.0210. PMID: 11315378. [DOI] [PubMed] [Google Scholar]
- 28.Mejersjö Christina. Therapeutic and prognostic considerations in TMJ osteoarthrosis: a literature review and a long-term study in 11 subjects. CRANIO®. 1987;5(1):69–78. PMID: 3467870. [PubMed] [Google Scholar]
- 29.Kalladka Mythili. Temporomandibular joint osteoarthritis: diagnosis and long-term conservative management: a topic review. J. Indian Prosthodont. Soc. 2014;14(1):6–15. doi: 10.1007/s13191-013-0321-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bernhardt Olaf. Prevalence and clinical signs of degenerative temporomandibular joint changes validated by magnetic resonance imaging in a non-patient group. Ann. Anat. Anat. Anzeiger. 2007;189(4):342–346. doi: 10.1016/j.aanat.2007.02.008. [DOI] [PubMed] [Google Scholar]
- 31.Schmitter M. Prevalence of clinical and radiographic signs of osteoarthrosis of the temporomandibular joint in an older persons community. Dentomaxillofac. Radiol. 2010;39(4):231–234. doi: 10.1259/dmfr/16270943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Murphy Meghan K. Temporomandibular joint disorders: a review of etiology, clinical management, and tissue engineering strategies. Int. J. Oral Maxillofac. Implants. 2013;28(6):e393. doi: 10.11607/jomi.te20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Poveda Roda Rafael. Review of temporomandibular joint pathology: Part I: classification, epidemiology and risk factors. Med. Oral Patol. Oral Cirugía Bucal. 2007;12(4):292–298. PMID: 17664915. [PubMed] [Google Scholar]