Abstract
Study Design:
A retrospective case-control study.
Objectives:
To determine factors influencing the ability to achieve coronal balance following spinal deformity surgery.
Methods:
Following institutional ethics approval, the radiographs of 47 patients treated for spinal deformity surgery with long fusions to the pelvis, were retrospectively reviewed. The postoperative measurements included coronal balance, L4 tilt, and L5 tilt, levels fused, apical vertebral translation and maximum Cobb angle. L4 and L5 tilt angles were measured between the superior endplate and the horizontal. Sagittal parameters including thoracic kyphosis, lumbar lordosis, pelvic incidence, and sagittal vertical axis were recorded. Coronal balance was defined as the distance between the central sacral line and the mid body of C7 being ≤40 mm. Surgical factors, including levels fused, use of iliac fixation with and without connectors, use of S2A1 screws, interbody devices, and osteotomies. Statistical tests were performed to determine factors that contribute to postoperative coronal imbalance.
Results:
Of the 47 patients reviewed, 32 were balanced after surgery and 14 were imbalanced. Coronal balance was 1.30 cm from center in the balanced group compared to 4.83 cm in the imbalanced group (P < .01). Both L4 and L5 tilt were statistically different between the groups. Gender and the use of transverse connectors differed between the groups but not statistically.
Conclusions:
In adult spinal deformity patients undergoing primary fusions to the pelvis, the ability to level the coronal tilt of L4 and L5 had the greatest impact on the ability to achieve coronal balance in this small series. A larger prospective series can help validate this important finding.
Keywords: coronal balance, L4 tilt, L5 tilt, adult spinal deformity, pelvic fixation, sagittal balance
Introduction
Achieving spinal balance is one of the major goals of deformity surgery.1–3 While sagittal alignment has been shown to have the greatest effect on patient-related outcomes, imbalance in the coronal plane can also negatively affect patient satisfaction.4–14 There is a growing body of literature indicating that greater postoperative coronal imbalance is associated with increased pain, increased loss of function, and decreased quality of life.4,11,12 Unfortunately, achieving coronal balance in long scoliosis corrections can be difficult. Preoperative factors including increased body mass index, greater L4 coronal tilt toward the convexity, osteoporosis, and larger coronal curve magnitude15,16 affect the ability to achieve balance. Technical features, including magnitude of correction, the use of offset connectors, and the ability to level off the distal lumbar spine, may also have an effect.
In cases of lumbar scoliosis, the fractional lumbosacral curve can often be stiffer than the main curve and is usually the main site of neural compression.1,17 Leveling L4 and L5 in the coronal plane during the correction can provide foraminal decompression, as well as a more balanced platform for which to correct the main curve. Correction in the face of a tilted L4 or L5 can lead to coronal imbalance toward the convexity of the curve. Strategies to overcome this include accepting less curve correction, or more dedicated correction of the distal vertebral tilts with distraction/compression maneuvers and/or the use of interbody devices.
The purpose of this study was to identify the key aspects of curve correction that affect coronal balance in patients treated with long posterior fusion for adult spinal deformities.
Materials and Methods
Following institutional ethics approval and a review of a computerized database, 47 consecutive patients who underwent primary spinal fusions to the pelvis for correction of coronal adult spinal deformity were identified. All procedures were performed between 2005 and 2015 by the senior author at a single institution. Two observers not involved in patient care independently reviewed all medical records. Clinical notes, outcome analysis and preoperative, discharge, and 6-month follow-up standing 3-foot radiographs were reviewed. Radiographs and questionnaires were administered prospectively and reviewed retrospectively. One patient presenting with infection requiring immediate removal of her instrumentation was excluded.
Surgical Procedure
All cases in this series had primary coronal deformities and underwent correction using posterior pedicle screw constructs with iliac fixation. Pedicle screws were placed at most levels in the construct, with screws placed in L4, L5, and S1 in all cases. Pelvic fixation was achieved with either iliac wing screws or S2-iliac screws at the discretion of the surgeon, with a higher percentage of more recent cases using S2 iliac fixation. If a large lateral offset was present between the S1 pedicle screw and the iliac wing screw, a transverse connector was used. Smith-Petersen’s osteotomies (Schwab type 2) were performed around the apex of the major curve to improve correction, as determined by the surgeon. Two cases required pedicle subtraction osteotomies. Posterior lumbar interbody fusion (PLIF) were used at the distal levels on the concavity (L3 to S1) if it was deemed necessary to augment fusion as an anterior column support, or if foraminal compression was present, whereby the cage was used to increase the foraminal area. Attempts to level L4 and L5 in the horizontal plane were performed through posterior distraction, either with a temporary rod or a screw distractor (Figure 1A-D), on the fractional lumbosacral concavity and supplemented with interbody support when deemed necessary. No anterior releases or anteriorly placed implants were performed in this series. Intraoperatively, tilt of the distal vertebrae was assessed clinically by gaging the relative levels of the right and left L4 screws relative to each other, and by prone posteroanterior radiographs (Figure 2).
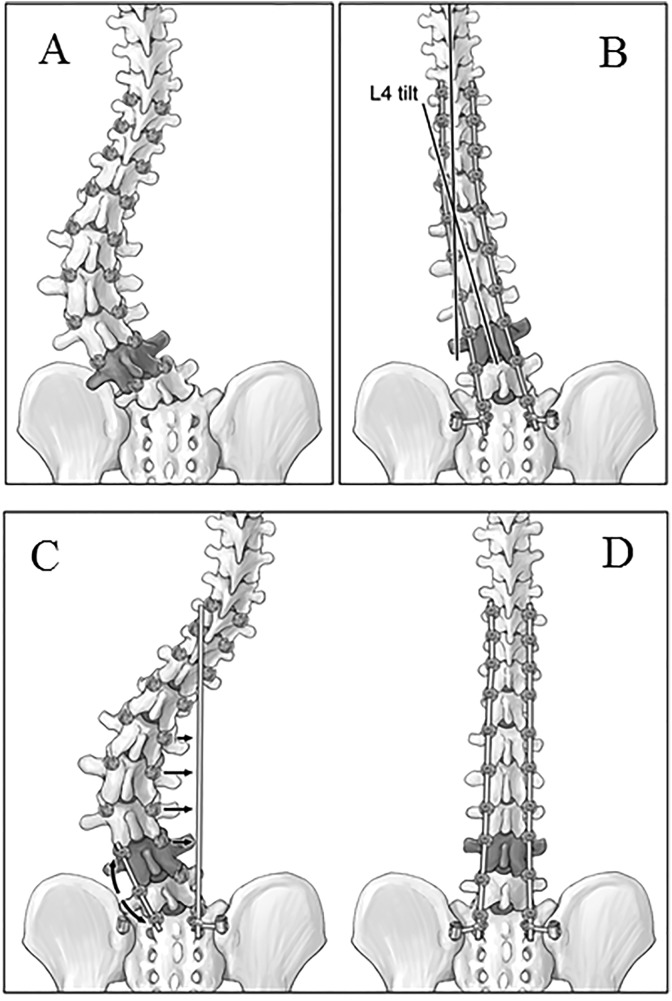
Figure 1.
Artist’s rendering demonstrating a preoperative scoliotic spine (A). Note L4 in dark. Correcting the main curve without leveling L4 in the coronal plane leads to coronal imbalance (B) toward the convexity of the main curve. A temporary rod is used to distract L4 to S1 on the concave side of the fractional lumbosacral curve (arrows) while the pre-contoured rod is applied to the concave side of the main curve (C), reducing the deformity to the rod (D). The concave distraction of the fractional curve provides direct decompression of the foramens. Concave compression and convex distraction of the main curve is used to complete the correction of the main curve.
Figure 2.
Preoperative standing anteroposterior radiograph (A) demonstrating an L4 coronal tilt angle of 26°. Following placement of the pedicle screws, distraction is applied between L4-5 and L5-S1 on the lumboscaral concavity (right side) until the L4 pedicles screws appear in line with each other clinically. Following placement of the left rod and correction of the deformity, the temporary right rod is removed, and the permanent right rod is placed. Intraoperative radiographic assessment (B) shows significant improvement in the L4 tilt to 7°. Interbody implants were not required to achieve this correction.
Radiographical Analysis
Long cassette standing radiographs were performed preoperatively, on discharge from the hospital, and at the 6-month postoperative visit. Computed tomographic scans were also reviewed if available. Coronal radiographic measurements included the number of levels fused, coronal balance (measured between the C7 midline and the center of the sacrum), L4 tilt, L5 tilt, apical vertebral translation (AVT) and maximal Cobb angle. L4 and L5 tilt angles were measured between the superior endplate and the horizontal. Sagittal parameters including thoracic kyphosis (TK, T5-T12), lumbar lordosis (LL, T12-S1), pelvic incidence (PI), and sagittal vertical axis (SVA) were recorded.
Statistical Analysis
Patients were stratified into groups based on postoperative coronal balance. Imbalance was defined as 40 mm or greater between the central sacral line and the mid C7 vertebral body. Radiographic and clinical parameters were compared between groups using either Mann-Whitney U tests or paired t tests for continuous data, and Fisher exact tests for categorical data. Pearson’s correlational analysis was performed to determine the relationship between the postoperative distal vertebral tilt angles and coronal balance. P values less than .05 were considered significant. Calculations were performed with IBM SPSS Statistics Version 19 (IBM SPSS, Somers, NY, USA.)
Results
Of the 46 patients, 32 were balanced (Figure 3A-F) and 14 were imbalanced (Figure 4A-F) in the coronal plane after surgery (Table 1). There were 81% females in the balanced group compared with 93% in the imbalanced group. The mean age in the balanced group was 66.0 years compared with 62.7 years in the imbalanced group. All cases were performed for scoliosis. Eight patients had S2 iliac screws compared with 38 patients with iliac wing screws. Preoperatively, the average coronal balance and Cobb angle were 44.0 mm and 48.5° in the balanced group compared with 50.8 mm and 56.0° in the imbalanced group (P > .05) (Table 2). The L4 and L5 coronal tilts, respectively, were 22.8° and 13.1° in the balanced group compared with 26.1° and 16.7° in the imbalanced group (P > .05).
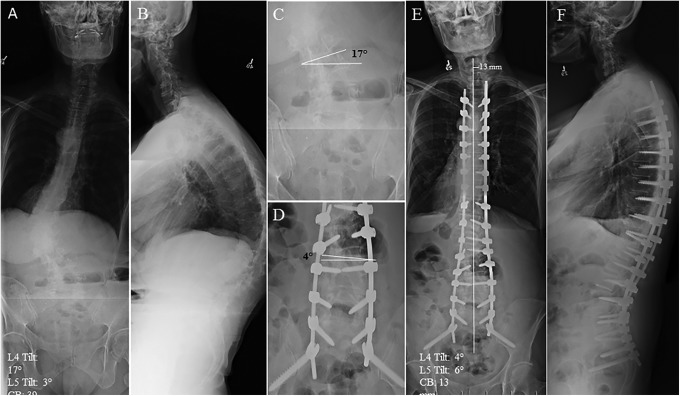
Figure 3.
Preoperative standing anteroposterior (A) and lateral (B) radiographs of a 67-year-old patient with degenerative scoliosis with 17° of L4 tilt and 39 mm of coronal imbalance to the right. Close-up view of the distal lumbar spine (C) highlights the coronal tilt of L4 that is reduced to 4° (D) following correction of the deformity. Postoperative standing anteroposterior (E) and lateral (F) radiographs demonstrate correction of the coronal balance to 13 mm and a well-aligned sagittal plane.
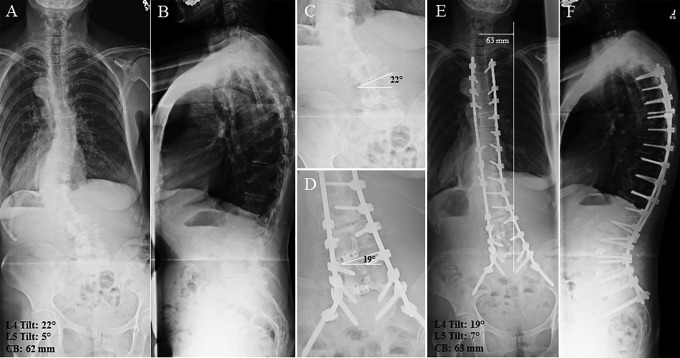
Figure 4.
Preoperative standing anteroposterior (A) and lateral (B) radiographs of a 61-year-old patient with degenerative scoliosis with 22° of L4 tilt, and 62 mm of coronal imbalance to the left. Close-up view of the distal lumbar spine (C) highlights the coronal tilt of L4 at 22° that remains high at 19° (D) following correction of the deformity. Postoperative standing anteroposterior (E) radiographs show coronal imbalance of 63 mm to the left. Well-balanced alignment is seen on the lateral (F) radiograph.
Table 1.
Demographics and Surgical Features.
| Coronal Balance (n = 32) | Coronal Imbalance (n = 14) | P | |
|---|---|---|---|
| Sex (male:female) | 6:26 | 1:13 | .41 |
| Age at surgery, years, mean (range) | 66.0 (47-77) | 62.7 (33-76) | .22 |
| Preoperative diagnosis, n | |||
| Degenerative scoliosis | 31 | 12 | .22 |
| Idiopathic scoliosis | 1 | 1 | .52 |
| Other | 0 | 1 | 0 |
| Levels fused, mean (range) | 12.0 (7-16) | 14.3 (9-17) | .01 |
| Osteotomies performed, n (%) | 11 (34) | 6 (43) | .58 |
| Pedicle subtraction osteotomies, n (%) | 0 (0) | 2 (14.3) | .09 |
| Interbody fusions, n (%) | 22 (69) | 8 (57) | .51 |
| Pelvic screws, n (%) | 24 (75) | 14 (100) | Not applicable |
| Offset connectors, n (%) | 19 (79) | 12 (86) | 1.00 |
| S2 alar screws, n (%) | 8 (25) | 0 | .08 |
Table 2.
Pre and Postoperative Coronal Radiographic Parameters.
| Measurement | Balanced Group (n = 32) | Imbalanced Group (n = 14) | P Between Groups |
|---|---|---|---|
| Coronal balance (mm) | |||
| Preoperative | 44.0 (3-149) | 50.8 (10-139) | .33 |
| Discharge | 17.6 (2-38) | 55.0 (40-86) | <.001 |
| Follow-up | 16.0 (0-36) | 51.3 (26-78) | <.001 |
| Coronal L4 tilt (°) | |||
| Preoperative | 22.8 (7-40) | 26.1 (17-36) | .13 |
| Discharge | 10.1 (2-24) | 18.3 (9-27) | <.001 |
| Follow-up | 11.2 (0-26) | 18.9 (10-29) | <.001 |
| Coronal L5 tilt (°) | |||
| Preoperative | 13.1 (1-28) | 16.7 (3-31) | .17 |
| Discharge | 7.1 (1-17) | 14.1 (3-27) | <.001 |
| Follow-up | 7.3 (0-16) | 13.8 (5-26) | .002 |
| Max Cobb angle (°) | |||
| Preoperative | 48.5 (29-83) | 56.0 (36-93) | .11 |
| Discharge | 19.3 (6-38) | 24.6 (7-47) | .05 |
| Follow-up | 20.5 (5-38) | 24.9 (8-35) | .06 |
| Mean Cobb correction | 56.5% (30.8-84) | 53.4% (30-78) | .64 |
| Apical vertebral translation (mm) | |||
| Preoperative | 42.6 (10-75) | 55.0 (37-79) | .01 |
| Discharge | 20.3 (0-45) | 41.2 (19-68) | <.001 |
| Follow-up | 21.3 (0-42) | 35.7 (6-59) | <.001 |
Coronal Parameters
Table 2 shows the coronal radiographic parameters of both groups preoperatively, at discharge from hospital, and at 6-month follow-up. Coronal balance was 16.0 mm in the balanced group and 51.3 mm in the imbalanced group (P < .001) after surgery. Both groups had significant improvements in coronal parameters; however, postoperative L4 and L5 tilts were significantly lower in the balanced group. L4 tilt was 11.2° compared with 18.9° in the imbalanced group (P < .001). L5 tilt was 7.3° compared with 13.8° in the imbalanced group (P < .001). Both L4 and L5 tilt were highly correlated with coronal imbalance, r = 0.75 and 0.61, respectively (P < .001).
All patients in this cohort had improvement in coronal Cobb angles. There were no significant differences in postoperative maximum Cobb angles (20.5° vs 24.9°) or magnitude of Cobb angle correction (56.5% vs 53.4%) between the 2 groups. AVT was improved in the balanced group compared with the imbalanced group (21.3 vs 35.7 mm).
Sagittal Parameters
Improvements in sagittal parameters were seen in both groups following surgery (Table 3). Sagittal balance improved from 86.3 to 42.5 mm and from 74.4 to 53.0 mm in the coronally balanced and imbalanced groups, respectively. PI-LL improved from 29.8° to 12.4° in the balanced group and from 23.5° to 12.7° in the imbalanced group. There were no differences in sagittal parameters between the groups.
Table 3.
Pre- and Postoperative Sagittal Radiographic Parameters.
| Measurement | Balanced Group (n = 32) | Imbalanced Group (n = 14) | P Between Groups |
|---|---|---|---|
| Sagittal balance (mm) | |||
| Preoperative | 86.3 (-3—227) | 74.4 (27—185) | .54 |
| Discharge | 55.6 (0-145) | 53.1 (15-95) | .89 |
| Follow-up | 42.5 (-25-149) | 53.0 (9-93) | .59 |
| Lumbar lordosis (°) | |||
| Preoperative | 27.4 (-21.6-66.3) | 38.9 (-5-72.6) | .19 |
| Discharge | 55.6 (0-145) | 53.1 (15-95) | .31 |
| Follow-up | 41.4 (0-59) | 45.0 (29-57) | .26 |
| Thoracic kyphosis (°) | |||
| Preoperative | 23.4 (-25-74) | 26.9 (-10-65) | .75 |
| Discharge | 28.4 (3-43) | 30.0 (1-54) | .68 |
| Follow-up | 30.3 (0-50) | 34.8 (19-53) | .86 |
| Pelvic incidence–lumbar lordosis (°) | |||
| Preoperative | 29.8 (2-79) | 23.5 (4-51) | .39 |
| Discharge | 13.1 (1-33) | 12.8 (1-31) | .90 |
| Follow-up | 12.4 (1-34) | 12.7 (1-32) | .82 |
Outcomes
Coronally balanced patients had higher Scoliosis Research Society (SRS) self-image scores at their initial follow up after surgery compared to the imbalanced patients. Balanced patients recorded self-image scores of 3.68 (2.0-4.8) out of 5 compared with 3.13 (1.3-3.8) in the imbalanced group (P = .01). Balanced patients also showed greater improvement of their self-image domain scores from baseline, improving 1.45 points compared to 0.86 in the imbalanced patients (P = .02). For the other SRS domains, both groups showed improvements in all other self-reported domains; however, the differences between groups were not statistically significant.
Lower Thoracic Versus Upper Thoracic Fusions
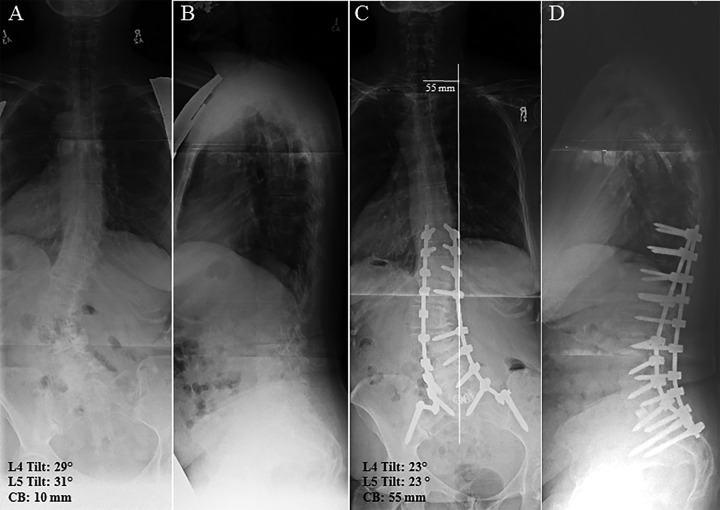
A total of 28 fusions extended from the upper thoracic spine to the pelvis compared with 18 fusions from the lower spine to the pelvis (Figure 5A-F). The data was run comparing long fusions and shorter fusions separately and no statistical differences were noted between the groups. The data for the short and long fusions was therefore combined.
Figure 5.
Preoperative standing anteroposterior (A) and lateral (B) radiographs of a 58-year-old patient with degenerative scoliosis with 29° of L4 tilt and 10 mm of coronal imbalance to the left. Anteroposterior radiographs following a T10 to pelvis construct shows persistent L4 tilt of 23° (C). Correction of the curve proximal to the tilted L4 resulted in coronal imbalance toward the convexity of 55 mm. Well-balanced alignment is seen on the lateral (D) radiograph.
Other Factors
Other factors investigated included the use of osteotomies, interbody fusion devices, S2 iliac screws, and the use of transverse offset connectors between the main construct and pelvic instrumentation. None of these factors differed between the balanced and imbalanced groups.
Discussion
Our findings demonstrate that leveling the L4 and L5 vertebrae in the coronal plane is key to achieving coronal alignment following adult spinal deformity surgery extending to the pelvis. Providing a more level base in the distal lumbar spine provides a more horizontal platform from which to correct the main curve, preventing imbalance toward the convexity. Coronally balanced patients showed an average L4 tilt of 11.2° while imbalanced patients had a significantly higher average tilt of 18.9°. Similar results were seen with the L5 tilt. We believe that the distal location of these obliquities in the spine magnifies the offset of the coronal plumb line, leading to the coronal imbalance. For example, a 5° coronal deviation from the central sacral line at L4 can hypothetically lead to the development of a coronal imbalance of approximately 35 mm at C7 with a corrected spine. Demographic factors, sagittal factors and the degree of correction did not differ between groups and did not significantly influence coronal balance or early outcome scores. Improved AVT correlated with the improvement in L4 tilt.
Determining coronal balance intraoperatively can be difficult as many centers do not have access to long cassette radiographs intraoperatively. However, an intraoperative posteroanterior lumbar radiograph can be performed offering the necessary visualization of the coronal tilt of L4 and L5. Recognizing the correction of the L4 and L5 tilts intraoperatively may provide the surgeon with the required information to make better judgements on the overall coronal balance achieved.
Lumbar tilt or obliquity in the coronal plane has been used as a predictor of outcomes in adult spine deformities previously. Jimbo et al15 discovered that L4 tilt was a predictor for the progression of preexisting degenerative lumbar scoliosis. Schwab et al14 showed that L3 and L4 obliquities were significantly correlated with pain in patients with adult scoliosis. Cecchinato et al18 were able to obtain both coronal and sagittal balance in previously imbalanced scoliosis patients through posterior osteotomies. However, our data is the first to highlight the importance of manipulating lumbar vertebral tilt to achieve coronal balance in long constructs with pelvic fixation for adult deformity, where correction of the main coronal curve is performed.
Posterior distraction of the lumbosacral concavity through a temporary short rod provides direct foraminal decompression, however, is a kyphosing technique. By distracting through the concavity, which is relatively hyperlordotic, and over a lordotic rod, the negative impact is minimized. Furthermore, placing an appropriately lordosed permanent rod on the contralateral side allows for obtaining the desired sagittal plane in the final construct. Concave distraction was the preferred method of correction of the lumbosacral fractional curve over convex compression for its beneficial effects on the foraminal compression. As seen in Table 3, a balanced lordosis was achieved in the final constructs in both groups, with PI-LL less than 15°, which was our goal in these cases of older deformity patients.
The amount of main curve correction can influence the coronal balance. Correction of the curve in the presence of fixed obliquity of L4 would likely create significant coronal offset. In this cohort, curve correction was similar between both groups, and L4 and L5 tilt became the key factor contributing to coronal balance. Patients with coronal balances more affected by the fractional lumbosacral curve than the main lumbar curve are particularly at risk for postoperative coronal imbalance. The use of interbody devices to help free up the lumbosacral curve was not associated with improved coronal balance in this series. We postulate that perhaps because of the position of the nerve root on the concavity, some of these implants were placed from the convexity, which may have negated the beneficial effects of the interbody device.
While nonsignificant in this study, the use of connectors in theory could be important for coronal balance. Placing rods directly into the iliac wing screws may lead to an oblique takeoff of the construct, if a small angle is introduced at this site. Using connectors can minimize this offset and lead to a more vertical takeoff of the distal construct. The high incidence of use of connectors likely negated the significance of this factor in our series. Alternatively, angular problems could be addressed with the use of S2 iliac screws, as their medial placement in the sacrum rather than the pelvis would be better aligned with the construct.19,20 We were unable to find studies directly relating the use of S2 iliac instrumentation with improved coronal balance; however, in our series, there was a trend toward achieving improved coronal balance with S2 iliac screws as compared with iliac wing screws. Further confounding the effects of the S2AI screws is that they were used in the latter part of the study when perhaps we were more experienced at leveling the distal segments.
Previous studies have demonstrated the maintenance of sagittal alignment as the most important factor for positive outcomes4–11,13,14 following spinal deformity surgery. There is a growing body of literature correlating coronal imbalance with a negative effect on patient outcomes.4,11,12,21 Pluomis et al12 showed that patients with coronal imbalance, defined as >5 cm in their study, showed a negative correlation with both mental health, vitality and physical function scores. In a large retrospective analysis, Koller et al11 determined that patients with coronal imbalance at follow-up had poorer clinical outcomes following deformity correction. Daubs et al6 defined coronal imbalance as coronal plumb line greater than 4 cm, and while they could not show that absolute malalignment affected Oswestry Disability Index scores, they discussed that any sort of postsurgical improvement in coronal balance trended to improve outcome scores. With the sagittal parameters equal in both groups in this series, horizontalizing the L4 and L5 vertebrae appears to be a key step in obtaining this coronal balance.4,11,12 This was associated with improved SRS self-image scores in this current series.
Limitations of our study include its sample size and retrospective design. These results are based on the techniques of a single surgeon and may not be extrapolated to other centers. While the impact of the L4 tilt was so significant even in this small series, other factors, such as the use of S2 iliac screws, may show significant impact in a larger series. Further research and larger sample sizes investigating the potential surgical techniques to achieve coronal balance are warranted. While the primary focus of this report is to demonstrate factors that were associated with obtaining improved coronal balance following adult deformity surgery, long-term follow-up is required to determine whether the coronal balance will influence outcome, fusion, and revision rates in these patients.
Conclusion
In spinal fusions for adult scoliosis, horizontal leveling of L4 and L5 leads to better coronal balance and self-reported self-image scores following adult spinal deformity surgery with fusions to the pelvis. The magnitudes of residual L4 and L5 tilts positively correlated with the magnitude of the coronal imbalance in this small series. A larger prospective series can help validate this important finding.
Footnotes
Authors’ Note: Research ethics board approval was granted prior to start of research (REB #14-7597-AE).
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: SJL serves as a consultant to Stryker, Medtronic, and AOSpine and receives money for travel, conferences, and teaching from Stryker, Medtronic, AOSpine, Depuy, and L&K.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: So Kato, MD  http://orcid.org/0000-0003-0835-2724
http://orcid.org/0000-0003-0835-2724
References
- 1. Aebi M. The adult scoliosis. Eur Spine J. 2005;14:925–948. [DOI] [PubMed] [Google Scholar]
- 2. Bradford DS, Tay BKB, Hu SS. Adult scoliosis: surgical indications, operative management, complications, and outcomes. Spine (Phila Pa 1976). 1999;24:2617–2629. [DOI] [PubMed] [Google Scholar]
- 3. Oskouian RJ, Jr, Shaffrey CI. Degenerative lumbar scoliosis. Neurosurg Clin N Am. 2006;17:299–315. [DOI] [PubMed] [Google Scholar]
- 4. Acaroglu E, Guler UO, Olgun ZD, et al. ; European Spine Study Group. Multiple regression analysis of factors affecting health-related quality of life in adult spinal deformity. Spine Deform. 2015;3:360–366. [DOI] [PubMed] [Google Scholar]
- 5. Birknes JK, White AP, Albert TJ, Shaffrey CI, Harrop JS. Adult degenerative scoliosis: a review. Neurosurgery. 2008;63(3 suppl):94–103. [DOI] [PubMed] [Google Scholar]
- 6. Daubs MD, Lenke LG, Bridwell KH, et al. Does correction of preoperative coronal imbalance make a difference in outcomes of adult patients with deformity? Spine (Phila Pa 1976). 2013;38:476–483. [DOI] [PubMed] [Google Scholar]
- 7. During J, Goudfrooij H, Keessen W, Beeker TW, Crowe A. Toward standards for posture: postural characteristics of the lower back system in normal and pathologic conditions. Spine (Phila Pa 1976). 1985;10:83–87. [PubMed] [Google Scholar]
- 8. Glassman SD, Berven S, Bridwell K, Horton W, Dimar JR. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine (Phila Pa 1976). 2005;30:682–688. [DOI] [PubMed] [Google Scholar]
- 9. Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F. The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976). 2005;30:2024–2029. [DOI] [PubMed] [Google Scholar]
- 10. Kim MK, Lee SH, Kim ES, Eoh W, Chung SS, Lee CS. The impact of sagittal balance on clinical results after posterior interbody fusion for patients with degenerative spondylolisthesis: a pilot study. BMC Musculoskelet Disord. 2011;12:69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Koller H, Pfanz C, Meier O, et al. Factors influencing radiographic and clinical outcomes in adult scoliosis surgery: a study of 448 European patients. Eur Spine J. 2016;25:532–548. [DOI] [PubMed] [Google Scholar]
- 12. Ploumis A, Liu H, Mehbod AA, Transfeldt EE, Winter RB. A correlation of radiographic and functional measurements in adult degenerative scoliosis. Spine (Phila Pa 1976). 2009;34:1581–1584. [DOI] [PubMed] [Google Scholar]
- 13. Schwab FJ, Lafage V, Farcy JP, Bridwell KH, Glassman S, Shainline MR. Predicting outcome and complications in the surgical treatment of adult scoliosis. Spine (Phila Pa 1976). 2008;33:2243–2247. [DOI] [PubMed] [Google Scholar]
- 14. Schwab FJ, Smith VA, Biserni M, Gamez L, Farcy J-PC, Pagala M. Adult scoliosis: a quantitative radiographic and clinical analysis. Spine (Phila Pa 1976). 2002;27:387–392. [DOI] [PubMed] [Google Scholar]
- 15. Jimbo S, Kobayashi T, Aono K, Atsuta Y, Matsuno T. Epidemiology of degenerative lumbar scoliosis: a community-based cohort study. Spine (Phila Pa 1976). 2012;37:1763–1770. [DOI] [PubMed] [Google Scholar]
- 16. Thompson JP, Transfeldt EE, Bradford DS, Ogilvie JW, Boachie-Adjei O. Decompensation after Cotrel-Dubousset instrumentation of idiopathic scoliosis. Spine (Phila Pa 1976). 1990;15:927–931. [DOI] [PubMed] [Google Scholar]
- 17. Kostuik JP, Hall BB. Spinal fusions to the sacrum in adults with scoliosis. Spine (Phila Pa 1976). 1983;8:489–500. [DOI] [PubMed] [Google Scholar]
- 18. Cecchinato R, Berjano P, Aguirre MFI, Lamartina C. Asymmetrical pedicle subtraction osteotomy in the lumbar spine in combined coronal and sagittal imbalance. Eur Spine J. 2015;24(suppl 1):S66–S71. [DOI] [PubMed] [Google Scholar]
- 19. O’Brien JR, Warren DY, Bhatnagar R, Sponseller P, Kebaish KM. An anatomic study of the S2 iliac technique for lumbopelvic screw placement. Spine (Phila Pa 1976). 2009;34:E439–E442. [DOI] [PubMed] [Google Scholar]
- 20. Sponseller P. The S2 Portal to the ilium. Semin Spine Surg. 2007;2:83–87. [Google Scholar]
- 21. Ploumis A, Simpson AK, Cha TD, Herzog JP, Wood KB. Coronal spinal balance in adult spine deformity patients with long spinal fusions: a minimum 2-5 year follow-up study. J Spinal Disord Tech. 2015;28:341–347. doi:10.1097/BSD.0b013e3182aab2ff. [DOI] [PubMed] [Google Scholar]