Abstract
Background:
Hypoglycemia and hypoglycemia unawareness are common in long-standing type 1 diabetes (T1D). This pilot study examined the real-world use of a smartphone application (app), which receives meter readings and logs hypoglycemic symptoms, causes, and treatments to reduce hypoglycemia.
Methods:
Adults with T1D and recent hypoglycemia synchronized their glucose meter to their smartphone and used the Joslin HypoMap™ app powered by Glooko to track hypoglycemic events. At baseline, and after 6 and 12 weeks of using the app, a blinded continuous glucose monitor (CGM; Dexcom G4) was used for 2 weeks and surveys administered.
Results:
Participants (n = 22) at baseline had mean (SD) age 43 (14) years, duration of diabetes 26 (13) years, A1c 8.0% (0.87) and 21/22 had reduced hypoglycemia awareness per Clarke Hypoglycemia Unawareness survey scores; 13 (59%) were “CGM completers” (CGM data available at baseline and follow-up). Most noncompletion related to time required/difficulties using the mobile app. After 6 weeks, 8/13 completers (62% of CGM completers, 36% of total participants) had reduced daytime minutes with glucose <54 mg/dL (mean ↓331 minutes) and 10/13 (77% of CGM completers; 45% of total participants) had reduced time ≤ 70 mg/dL (mean ↓449 minutes). This was not sustained at 12 weeks, at which time half of the completers had less time (“improved”). Five participants reported improved hypoglycemia awareness; 9 stated the app helped them better recognize hypoglycemia.
Conclusions:
Use of this phone app has the potential to help reduce daytime hypoglycemia in a subset of T1D adults with reduce hypoglycemia awareness; larger studies are needed.
Keywords: hypoglycemia, type 1 diabetes, apps, mobile, hypoglycemia awareness
All patients with type 1 diabetes (T1D) require insulin therapy, which puts them at risk for developing severe hypoglycemia. Hypoglycemia is responsible for increasing numbers of hospitalizations and emergency room visits, and contributes to worse quality of life.1-3 Hypoglycemia can cause cardiac arrhythmias, falls, seizures, loss of consciousness, and even death.4,5 The problem of serious hypoglycemia is greatest in long-standing diabetes, particularly in adults with T1D of >20 years duration.6 With longer duration of T1D, poor hypoglycemic awareness becomes more common, increasing the risk of frequent and severe hypoglycemia.4,7-9
In-person behavioral educational programs, such as blood glucose awareness training (BGAT), have been successfully employed to help individuals with reduced hypoglycemia awareness better anticipate, recognize, treat, and prevent serious hypoglycemia.10,11 BGAT was later adapted for delivery over the Internet.12,13 With increasing numbers of adults using smartphones, there has been increasing interest in the use of mobile diabetes applications (apps) to improve glycemic control, with varying success.14,15
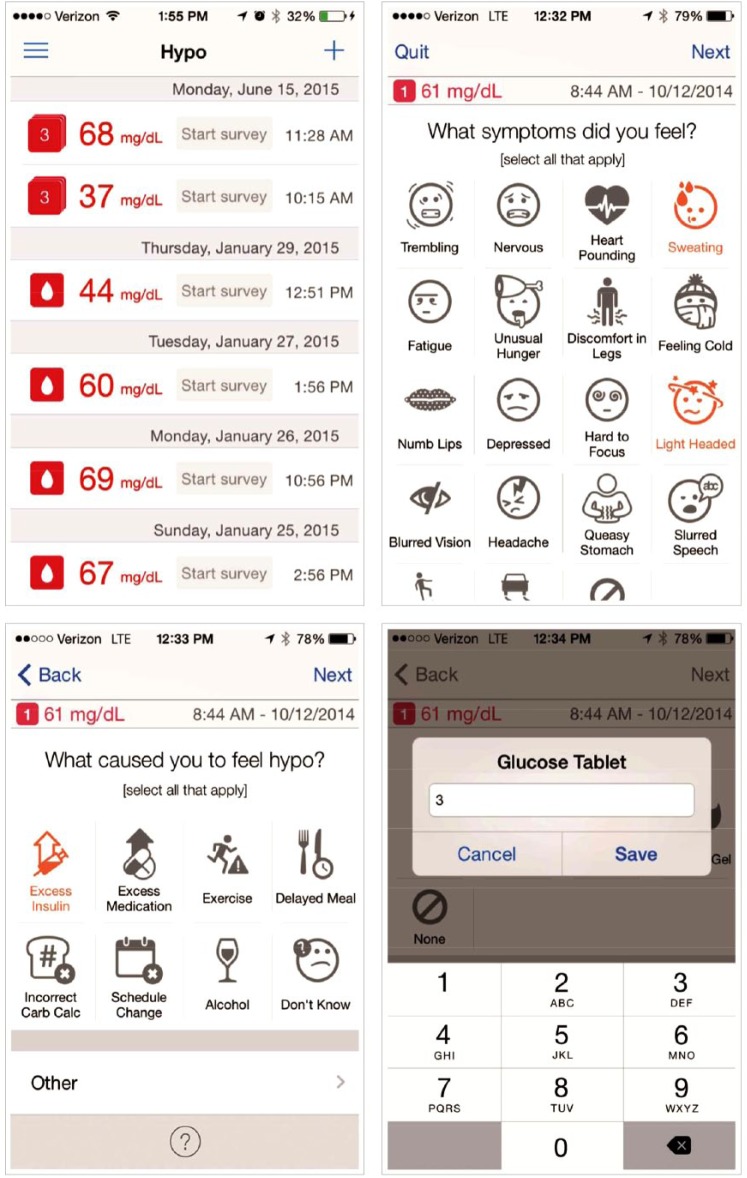
A smartphone app, designed to improve hypoglycemia awareness based on principles used in BGAT, provides a platform for patients to record symptoms, contributing factors, and treatments at the time of hypoglycemic events. When the patient’s glucose meter is synchronized with the app on their smartphone, hypoglycemic readings trigger a reminder from the app to enter information related to the event, specifically symptoms, treatment, and causation (Figure 1). The hypothesis is that tracking symptoms and events on mobile devices can improve hypoglycemia awareness thereby assisting patients to better detect and prevent future hypoglycemic events.
Figure 1.
Joslin HypoMap™ App.
The primary objective of this pilot study was to examine feasibility in the use of this app in a real-world clinic setting and determine if its use reduced hypoglycemic events and time in hypoglycemia in adults with T1D. A blinded Dexcom G4 Platinum Professional continuous glucose monitor (CGM) was used to measure time in hypoglycemia for 2 weeks prior to baseline and after 6 and 12 weeks of using the app. CGM metrics were computed overall and separately for daytime (6 am to 12 midnight) and nighttime (12 midnight to 6 am) hours. Hypoglycemia awareness was assessed using the Clarke survey.16 Patient satisfaction with use of the app was also evaluated. If this smartphone app can assist patients in reducing their risk of serious hypoglycemia and time in hypoglycemia, it could be of great benefit.
Methods
Participants and Procedures
Inclusion criteria were age ≥ 21 years with T1D and current use of a smartphone (iPhone or Android). Exclusion criteria included end-stage renal disease, dementia, severe visual impairment affecting their ability to read the screen of their smartphone, and current use of CGM. At the screening visit, after obtaining informed consent, participants completed the Clarke Hypoglycemia Unawareness survey. To qualify for continuation, participants were required to have 2 or more “R” responses on the survey indicating a lack of full awareness of hypoglycemia. For those without full awareness, a blinded Dexcom G4 Platinum Professional was placed. CGM data were collected for 2 weeks. Participants were given the option to return to the clinic in 7 days for a sensor change, or to receive instructions on how to change the sensor at home. The baseline visit was scheduled for approximately 2 weeks after placement of the first sensor.
At the baseline visit the CGM was downloaded. Subjects continued in the study if, on the CGM download, there were at least 4 readings of glucose <70 mg/dL including 2 readings of glucose <55 mg/dL during daytime hours. Following confirmation of eligibility, the Glooko app was downloaded to the participant’s smartphone. Participants then received the MeterSync Blue™ (Glooko Inc) which was needed to sync their glucose meter to their smartphone. They received training in the use of Glooko including instructions for synchronizing their glucose meter daily with their mobile device and in the use of the Joslin HypoMap™ app, designed by Dr Howard Wolpert and powered by Glooko.
After using the app for 6 weeks, and again at 12 weeks, participants returned for follow-up visits. At each of the 2 follow-up visits, the Clarke survey and a questionnaire assessing participant opinions on usability and satisfaction with the app were administered, and CGM data were collected for 2 weeks using a blinded Dexcom G4. HypoMap data from smartphones were collected through Glooko. A1c was recorded at baseline and 12 weeks.
This pilot study was conducted at the Joslin Diabetes Center at SUNY Upstate Medical University (Syracuse, NY) between December 2015 and December 2016. All visits were conducted in the clinic. This study was approved by the SUNY Upstate Institutional Review Board for the Protection of Human Subjects.
Analyses
The primary analysis compared the time spent in hypoglycemia and number of hypoglycemic episodes before and after use of the app. Each participant served as his/her own control. CGM metrics were computed overall and separately for daytime (6 am to 12 midnight) and nighttime (12 midnight to 6 am) hours. Two definitions of hypoglycemia were used: CGM glucose readings ≤ 70 mg/dL and < 54 mg/dL. A hypoglycemic episode was defined as at least 5 consecutive readings at these levels (devices collected data every 5 minutes). An episode was considered ended after 5 consecutive readings were above the cut-point.
If there were time gaps within an episode, gaps lasting less than 20 minutes were handled as follows: If the readings bracketing the gap were both below the cut-point for that episode, the episode was considered to be continuing. If the reading at the start of the gap was below the cut-point, but the next reading was above the cut-point, the episode was considered ended, and the time stamp of the final low reading was used as the ending time of the episode. Gaps of greater than 20 minutes also signaled the end of an episode, and again, the time stamp of the final low reading was used as the ending time of the episode.
Subjects were included in the analysis as CGM completers if they had CGM data at baseline and after using the app for at least 6 weeks, as well as at least 7 “analysis days” of data for an included visit, defined as at least 3 hours of night readings (midnight-6 am) and at least 6 hours of day readings (6 am-midnight), excluding gaps. The duration and number of hypoglycemic episodes at baseline were compared to those after 6 weeks and 12 weeks of using the app for each participant.
Hypoglycemia awareness was measured using the Clarke survey as follows: a score ≥4 was considered “reduced awareness,” 3 was coded as “partially aware,” and ≤2 was considered “aware.”
Results
Baseline characteristics of participants are shown in Table 1. Overall, mean age was 43 years (SD 14), and mean duration of diabetes 26 years (SD 13). Of the 28 participants who completed the screening visit, 22 continued participation. Reasons for withdrawal from the study at the baseline visit were (1) baseline CGM did not document sufficient hypoglycemia per protocol (n = 3), (2) technology difficulties (problems with app and phone compatibility, n = 2), and (3) one participant used the Dexcom G4 in her swimming pool twice at baseline, destroying 2 devices. Of the 22 participants, 13 (59%) were CGM completers. An additional participant completed all study questionnaires and procedures except for the CGM. Most of the reasons for noncompletion related to difficulties with the technology (difficulties using the app, problems with app and phone compatibility, using the app took too much time, difficulties synchronizing meter and app). One participant moved out of the area, and one participant decided to obtain and use a personal unblinded CGM. The mean A1c at baseline was 8.0% (SD 0.87) and at 12 weeks was 8.1% (SD 0.94).
Table 1.
Baseline Participant Characteristics (n = 22).
| Completers (n = 13)a | Noncompleters (n = 9) | Total (N = 22) | |
|---|---|---|---|
| Age (years), mean (SD) | 49 (13) | 36 (14) | 43 (14) |
| Gender, n (%) | |||
| Male | 9 (69%) | 4 (44%) | 13 (59%) |
| Female | 4 (31%) | 5 (56%) | 9 (41%) |
| Race/ethnicity, n (%) | |||
| African American | 2 (15%) | 1 (11%) | 3 (14%) |
| Non-Hispanic White | 11 (85%) | 8 (89%) | 19 (86%) |
| Duration of diabetes (years), mean (SD) | 31 (12) | 19 (12) | 26 (13) |
| Hypoglycemia awareness, n (%)b | |||
| Reduced awareness | 11 (85%) | 8 (89%) | 19 (86%) |
| Partial awareness | 1 (8%) | 1 (1%) | 2 (9%) |
| Aware | 1 (8%) | 0 (7%) | 1 (5%) |
Completer: attended at least 1 follow-up visit after using HypoMap for at least 6 weeks, had at least 7 analysis days of CGM with an analysis day defined as at least 3 hours of night readings (midnight-6 am) and 6 hours of day readings (6 am-midnight)] at each time point.
Defined by score on Clarke survey: reduced awareness score ≥ 4, partial awareness score = 3, and aware score ≤≤ 2.
At baseline (for CGM completers, n = 13), mean total CGM readings was 15787 minutes/participant (range 10446-19050). All 13 CGM completers had hypoglycemia at baseline: mean minutes/participant with glucose < 54 mg/dL was 506 (range 25-1260), and mean number of episodes/participant of glucose < 54 mg/dL was 6 (range 1-13); mean minutes/participant with glucose ≤ 70 mg/dL was 1119 (range 420-2075), mean % time/participant with glucose ≤ 70 mg/dL was 7.2% (range 2.7-18.4%), mean number of episodes of glucose ≤ 70 mg/dL was 11 (range 4-21).
Changes in time in hypoglycemia after using HypoMap for 6 weeks and 12 weeks are shown in Table 2. Overall, the majority of participant CGM completers had less daytime hypoglycemia at 6 weeks: 62% of CGM completers (36% of total participants) were “improved” with less time <54 mg/dL (mean ↓331 minutes) and 77% of CGM completers (45% of total participants) had less time ≤ 70 mg/dL (mean ↓449 minutes). This difference was not sustained at 12 weeks at which time 50% of CGM completers (23% of total participants) improved (fewer minutes in daytime hypoglycemia) and 50% of CGM completers did not improve (unchanged or more daytime hypoglycemia). Table 3 shows time in hypoglycemia in minutes/day for each participant at baseline, and 6 and 12 weeks after using HypoMap. Nine of the 13 CGM completers spent less time in hypoglycemia after using HypoMap.
Table 2.
Change in Time in Hypoglycemia After Use of the HypoMap App.
| Use of HypoMap |
6 weeks (n = 13) |
12 weeks (n = 10)a |
||
|---|---|---|---|---|
| Time in hypoglycemiab | Improved (↓ min) |
Not improved (↔↑ min) |
Improved (↓ min) |
Not improved (↔↑ min) |
| CGM: Glucose < 54 mg/dL | ||||
| Total change: Minutes: mean (range) |
n = 8 ↓403 (120-1095) |
n = 5 ↑354 (50-950) |
n = 6 ↓551 (255-1040) |
n = 4 ↑336 (140-695) |
| Nighttime change: | n = 4 | n = 9 | n = 5 | n = 5 |
| Minutes: mean (range) | ↓420 (25-880) | ↑266 (0-1100) | ↓353 (45-820) | ↑82 (0-160) |
| Daytime change: Minutes: mean (range) |
n = 8 ↓331 (50-670) |
n = 5 ↑96 (0-305) |
n = 5 ↓355 (85-505) |
n = 5 ↑234 (25-560) |
| CGM: Glucose ≤70 mg/dL | ||||
| Total change: Minutes: mean (range) |
n = 10 ↓467 (30-1480) |
n = 3 ↑737 (260-1520) |
n = 6 ↓721 (25-1220) |
n = 4 ↑829 (105-1535) |
| Nighttime change: | n = 5 | n = 8 | n = 4 | n = 6 |
| Minutes: mean (range) | ↓460 (70-1225) | ↑442 (0-1370) | ↓475 (90-1230) | ↑200 (0-675) |
| Daytime change: Minutes: mean (range) |
n = 10 ↓449 (30-1050) |
n = 3 ↑263 (150-375) |
n = 5 ↓577 (175-730) |
n = 5 ↑515 (50-1240) |
Improved = reduction in minutes in hypoglycemia. Not improved = unchanged or increased minutes in hypoglycemia.
One participant “completer” did not attend the week 12 visit, 2 did not have analyzable CGM data at week 12.
Nighttime: Midnight-6 am; daytime: 6 am-midnight.
Table 3.
Time in Hypoglycemia for Each Participant Before and After Use of the HypoMap App (Minutes/Day).
| Subjects (n = 13) | Baseline (min/day) | 6 weeks (min/day) | 12 weeks (min/day) |
|---|---|---|---|
| CGM: Glucose < 54 mg/dL | Improved | ||
| 102 | 19 | 20 | |
| 20 | 23 | 0 | |
| 23 | 76 | 3 | |
| 54 | 26 | 0 | |
| 46 | 32 | 8 | |
| 151 | 139 | N/A | |
| 22 | 8 | N/A | |
| 38 | 7 | N/A | |
| 87 | 15 | 32 | |
| Not improved | |||
| 30 | 79 | 72 | |
| 25 | 91 | 62 | |
| 17 | 5 | 26 | |
| 3 | 21 | 58 | |
| CGM: Glucose ≤≤ 70 mg/dL | Improved | ||
| 151 | 51 | 58 | |
| 73 | 52 | 20 | |
| 83 | 74 | 34 | |
| 73 | 22 | N/A | |
| 86 | 53 | N/A | |
| 163 | 46 | 74 | |
| Not improved | |||
| 144 | 161 | 156 | |
| 64 | 192 | 78 | |
| 93 | 185 | 226 | |
| 265 | 267 | N/A | |
| 39 | 17 | 74 | |
| 58 | 52 | 159 | |
| 63 | 81 | 60 | |
Changes in number of episodes of hypoglycemia were also calculated. At 6 weeks, 9 participants (69% of CGM completers, 41% of total participants) had fewer daytime episodes of glucose < 54 mg/dL (mean ↓4 episodes, range 1-9) and of glucose ≤ 70 mg/dL (mean ↓4 episodes, range 1-10). At 12 weeks, 6 participants (46% of CGM completers and 27% of total participants) had fewer daytime episodes of glucose < 54 mg/dL (mean ↓4 episodes, range 1-6).
Hypoglycemia awareness at baseline by category, using the score from the complete Clarke survey, is shown in Table 1. Table 4 shows the changes in “revised” scores over time. Revised scores were calculated after omitting questions 3 and 4 of the Clarke survey. Since these 2 questions ask about hypoglycemia awareness over the past 6 months and 1 year, they were not useful in assessing changes in scores after 6 and 12 weeks. Of the 14 participants who used the app and completed the Clarke surveys over time, 5 had reductions in scores after using HypoMap indicating better hypoglycemia awareness.
Table 4.
Change in Hypoglycemia Awareness (Revised Clarke Score) After Use of the HypoMap App.
| # subjects (total N = 14) |
Clarke Survey Revised scoresa |
Change in score |
||
|---|---|---|---|---|
| n | Baseline | 6 weeks | 12 weeks | Baseline-12 weeks |
| 5 | 5 | 5 | 5 | ↔ |
| 1 | 5 | 4 | 5 | ↔ |
| 1 | 5 | 3 | 0 | ↓↓↓↓↓ |
| 1 | 4 | 4 | 4 | ↔ |
| 1 | 4 | 4 | 2 | ↓↓ |
| 1 | 4 | 3 | 3 | ↓ |
| 1 | 3 | 5 | 2 | ↓ |
| 1 | 3 | 3 | 2 | ↓ |
| 1 | 2 | 5 | 4 | ↑↑ |
| 1 | 1 | 2 | 1 | ↔↔ |
Answers to questions 3 and 4 of the Clarke Survey were omitted in this table since the questions ask about hypoglycemia over the past 6 and 12 months. Higher scores reflect more hypoglycemia unawareness; ↓in score reflects better hypoglycemia awareness.
Participants were instructed to enter information related to their hypoglycemic episodes using the HypoMap surveys in the app (Figure 1). Of the 22 total participants, 20 (91%) had multiple hypoglycemic readings in their app but only 6 participants (27%) completed HypoMap hypoglycemia survey questions. Of the 72 surveys completed (1 survey per hypoglycemic episode), 39 episodes were associated with NO symptoms, 12 were associated with autonomic symptoms, 10 were associated with neuroglycopenic symptoms, and 11 were associated with both autonomic and neuroglycopenic symptoms. At 12 weeks, 12 participants had hypoglycemia readings in Glooko but only 1 CGM completer participant completed the HypoMap surveys. This participant completed the survey for 48 episodes, all episodes without symptoms; this participant did not have a reduction in time in hypoglycemia or in number of hypoglycemic episodes. An additional participant completed the surveys for 5 episodes, 3 of which were associated with neuroglycopenic symptoms and 2 with both autonomic and neuroglycopenic symptoms, but there were no CGM data for this participant.
Patient satisfaction scores were based on a 5-point scale, strongly disagree (1) to strongly agree (5). At the 6-week visit, with 17 participants completing the survey: 13/17 agreed/strongly agreed that they were satisfied with the app to track hypoglycemia episodes (mean score 4.0 ± 1.2), 9/17 agreed/strongly agreed that they were more involved in their care using the app (mean score 3.7 ± 1.2), 9/17 agreed/strongly agreed that the intervention helped them better recognize hypoglycemia episodes (mean score 3.7 ± 1.2), 6/17 agreed/strongly agreed that they felt they had less hypoglycemia using the app (mean score 2.9 ± 1.2) and 13/17 agreed/strongly agreed that the app was “easy to use” (mean score 4.2 ± 1.1). At 12 weeks, with 14 participants completing surveys: 9/14 agreed/strongly agreed that they were satisfied with the app to track hypoglycemia episodes (mean score 3.5 ± 1.6), 9/14 agreed/strongly agreed that they were more involved in their care using the app (mean score 3.4 ± 1.7), 9/14 agreed/strongly agreed that the intervention helped them better recognize hypoglycemia episodes (mean score 3.5 ± 1.5), 6/14 agreed/strongly agreed that they felt they had less hypoglycemia using the app (mean score 3.2 ± 1.1), and 11/14 agreed/strongly agreed that the app was “easy to use” (mean score 4.1 ± 1.3).
Discussion
T1D is increasing in prevalence, and people with T1D are living longer.17-19 Since hypoglycemia unawareness and high rates of hypoglycemia relate to longer duration of T1D, the problem of severe hypoglycemia is growing. Several strategies have been employed to address this problem, including the use of new insulin regimens and new technologies such as sensor-augmented insulin pumps and CGM with multiple daily injections.20 In the future, closed-loop systems and islet replacement therapies should be of great benefit. While we await these solutions, structured education and behavioral interventions such as BGAT, HAATT (Hypoglycemia Anticipation, Awareness and Treatment Training), HypoAware, and HyPOS have been used with some success.10-12,21-23 The use of a smartphone app to deliver such an intervention is particularly appealing given the widespread use and portability of smartphones and the relative low cost of such an intervention.
In this pilot study of the HypoMap app, 9 and 6 participants (41% and 27% of total participants) reported that the app was helpful in recognizing and reducing hypoglycemia after 6 and 12 weeks respectively. The study was conducted in our diabetes center, a “real-world” setting. There were no adherence criteria for use of the app during participation. Data from blinded CGM confirmed improvement 6 weeks after training in the use of the app (reduction in minutes and episodes of glucose ≤ 70 mg/dL and < 54 mg/dL) in 10 individuals (77% of CGM completers, 45% of total participants) and 8 (62% of completers, 36% of total participants) respectively. The fact that these reductions were seen primarily during the day (as anticipated with use of a phone app) supports the premise that the app played a role in this improvement. Lesser effects at 12 weeks may be related to lower use of the app over time. Physiological differences could also be responsible for differing effectiveness of the intervention. Psychoeducation programs are unlikely to be successful in individuals with extremely poor or absent hypoglycemia awareness that is not reversible. Although our sample in this pilot study was small, CGM completers were older and had longer duration T1D which are characteristics associated with more hypoglycemia and hypoglycemia unawareness. Targeting individuals with diminished hypoglycemia awareness who have the potential to recover some awareness with reducing hypoglycemia is an area for future study.
There was one participant who scored “aware” (2 “R” responses) on the baseline Clarke Hypoglycemia Awareness survey and higher scores (“reduced awareness”) on the 2 follow-up surveys. At baseline, this individual had many hypoglycemic episodes of which he was unaware. With more frequent testing during the study, he realized that he had been having unrecognized hypoglycemia. This points to a limitation of the Clarke survey in assessing hypoglycemia awareness.
Of interest is that 9 participants agreed/strongly agreed that they were satisfied with using the app to track hypoglycemia at 12 weeks, but only 2 participants completed HypoMap surveys in Glooko. It is possible that the transfer of the hypoglycemic readings to the app, displaying a diary of the hypoglycemic episodes and reminding the participants to complete the hypoglycemia surveys (Figure 1) may have been helpful even without completion of the HypoMap surveys.
Many phone apps are available, but there is a paucity of information concerning their actual use and effectiveness. Challenges using phone apps to improve glycemic control have been reviewed.14,15 In this small pilot clinic-based study, contributing factors for not using the app included technical issues (some participants had older smartphones and meters that caused difficulty with the sync function, some participants living in rural areas lost connectivity due to poor Internet connections), the added time/burden of entering data (the participant who entered the most data was not employed and was without household or caregiver responsibilities), difficulty keeping Bluetooth “on” at all times (had to carry MeterSync Blue™ since they were instructed to sync daily, complaints that Bluetooth “used up too much battery”). Future studies could include additional contacts to assist participants with some of these technical challenges when starting use of the app and over time. It is hoped that, in the future, as the technology becomes easier to use and less complex (more automated), reducing the burden for the patient and the provider, digital solutions will be more helpful and widely used.
A strength of this study was the use of CGM to assess hypoglycemia. The major limitations are the small number of participants and the high rate of noncompleters. Larger studies will be needed to confirm our findings.
Conclusion
The smartphone app HypoMap has the potential to help a subset of adults with long-standing T1D better recognize hypoglycemia and reduce time in hypoglycemia. Its use should be further studied and considered, as an inexpensive option within a menu of available interventions, to assist appropriate patients in lowering their risk of hypoglycemia.
Acknowledgments
We thank Dr Howard Wolpert for sharing HypoMap with us and Dr Roy Beck for his review of this manuscript.
Footnotes
Abbreviations: app, application; BGAT, blood glucose awareness training; CGM, continuous glucose monitor; Joslin HypoMap™ app, HypoMap; N/A, not available; T1D, type 1 diabetes.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: SB and RSW have participated in multicenter clinical trials sponsored by Diasome Pharmaceuticals Inc, Calibra Medical Inc, Mylan GmbH Inc, and Medtronic Minimed Inc.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The T1D Exchange and Leona M and Harry B Helmsley trust provided funding, Dexcom provided Dexcom 4 continuous glucose monitors for this study, and Glooko Inc supplied MeterSync Blue™ and waived subscription fees for use of Glooko.
ORCID iD: Ruth S. Weinstock  http://orcid.org/0000-0001-5859-5666
http://orcid.org/0000-0001-5859-5666
References
- 1. Geller AI, Shehab N, Lovegrove MC, et al. National estimates of insulin-related hypoglycemia and errors leading to emergency department visits and hospitalizations. JAMA Intern Med. 2014;174(5):678-686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lipska KJ, Ross JS, Wang Y, et al. National trends in US hospital admissions for hyperglycemia and hypoglycemia among Medicare beneficiaries, 1999 to 2011. JAMA Intern Med. 2014;174(7):1116-1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Laiteerapong N, Karter AJ, Liu JY, et al. Correlates of quality of life in older adults with diabetes: the diabetes and ageing study. Diabetes Care. 2011;34(8):1749-1753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cryer PE. Hypoglycemia in type 1 diabetes mellitus. Endocrinol Metab Clin North Am. 2010;39(3):641-654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gill GV, Woodward A, Casson IF, Weston PJ. Cardiac arrhythmia and nocturnal hypoglycaemia in type 1 diabetes—the “dead in bed” syndrome revisited. Diabetologia. 2009;52(1):42-45. [DOI] [PubMed] [Google Scholar]
- 6. Weinstock RS, Xing D, Maahs DM, et al. Severe hypoglycemia and diabetic ketoacidosis in adults with type 1 diabetes: results from the T1D exchange clinic registry. J Clin Endocrinol Metab. 2013;98(8):3411-3419. [DOI] [PubMed] [Google Scholar]
- 7. Weinstock RS, DuBose SN, Bergenstal RM, et al. Risk factors associated with severe hypoglycemia in older adults with type 1 diabetes. Diabetes Care. 2016:39(4):603-610. [DOI] [PubMed] [Google Scholar]
- 8. DuBose SN, Weinstock RS, Beck RW, et al. Hypoglycemia in older adults with type 1 diabetes (T1D). Diabetes Technol Ther. 2016;18(12):765-771. [DOI] [PubMed] [Google Scholar]
- 9. Hepburn DA, Patrick AW, Eadington DW, Ewing DJ, Frier BM. Unawareness of hypoglycemia in insulin-treated patients: its prevalence and relationship to autonomic neuropathy. Diabet Med. 1990;7(8):711-717. [DOI] [PubMed] [Google Scholar]
- 10. Cox D, Gonder-Frederick L, Polonsky W, Schlundt D, Julian D, Clarke W. A multicenter evaluation of blood glucose awareness training-II. Diabetes Care. 1995;18(4):523-528. [DOI] [PubMed] [Google Scholar]
- 11. Cox DJ, Gonder-Frederick L, Polonsky W, Schlundt D, Kovatchev B, Clarke W. Blood glucose awareness training (BGAT-2): long term benefits. Diabetes Care. 2001;24(4):637-642. [DOI] [PubMed] [Google Scholar]
- 12. Cox D, Ritterband L, Magee J, Clarke W, Gonder-Frederick L. Blood glucose awareness training delivered over the Internet. Diabetes Care. 2008;31(8):1527-1528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Rondags SM, de Wit M, van Tulder MW, Diamant M, Snoek FJ. HypoAware-a brief and partly web-based psycho-educational group intervention for adults with type 1 and insulin-treated type 2 diabetes and problematic hypoglycaemia: design of a cost-effectiveness randomized controlled trial. BMC Endocr Disord. 2015;15:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hood M, Wilson R, Corsica J, Bradley L, Chirinos D, Vivo A. What do we know about mobile applications for diabetes self-management? A review of reviews. J Behav Med. 2016;39(6):981-994. [DOI] [PubMed] [Google Scholar]
- 15. Bonoto BC, de Araujo VE, Godoi IP, et al. Efficacy of mobile apps to support the care of patients with diabetes mellitus: a systematic review and meta-analysis of randomized controlled trials. JMIR Mhealth Uhealth. 2017;5(3):e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Clarke WL, Cox DJ, Gonder-Frederick LA, Julian D, Schlundt D, Polonsky W. Reduced awareness of hypoglycemia in adults with IDDM. A prospective study of hypoglycemic frequency and associated symptoms. Diabetes Care. 1995;18(4):517-522. [DOI] [PubMed] [Google Scholar]
- 17. Ioacara S, Lichiardopol R, Ionescu-Tirgoviste C, et al. Improvements in life expectancy in type 1 diabetes patients in the last six decades. Diabetes Res Clin Pract. 2009; 86(2):146-151. [DOI] [PubMed] [Google Scholar]
- 18. Mayer-Davis EJ, Lawrence JM, Dabelea D, et al. Incidence trends of type 1 and type 2 diabetes among youths, 2002-2012. N Engl J Med. 2017;376(15):1419-1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Maahs DM, West NA, Lawrence JM, Mayer-Davis EJ. Chapter 1: epidemiology of type 1 diabetes. Endocrinol Metab Clin North Am. 2010;39(3):481-497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Little SA, Leelarathna L, Barendse SM, et al. Severe hypoglycaemia in type 1 diabetes: underlying drivers and potential strategies for successful prevention. Diabetes/Metab Res Rev. 2014;30(3):175-190. [DOI] [PubMed] [Google Scholar]
- 21. Cox DJ, Kovatchev B, Koev D, et al. Hypoglycemia anticipation, awareness and treatment training (HAATT) reduces occurrence of severe hypoglycemia among adults with type 1 diabetes mellitus. Int J Behav Med. 2004;11(4):212-218. [DOI] [PubMed] [Google Scholar]
- 22. Rondags SMPA, de Wit M, van Twisk JW, Snoek FJ. Effectiveness of HypoAware, a brief partly web-based psychoeducational intervention for adults with type 1 and insulin-treated type 2 diabetes and problematic hypoglycemia: a cluster randomized controlled trial. Diabetes Care. 2016;39(12):2190-2196. [DOI] [PubMed] [Google Scholar]
- 23. Hermanns N, Kulzer B, Kubiak T, Krichbaum M, Haak T. The effect of an education programme (HyPOS) to treat hypoglycaemia problems in patients with type 1 diabetes. Diabetes Metab Res Rev. 2007;23(7):528-538. [DOI] [PubMed] [Google Scholar]