The term “reactive hypoglycemia” (RH) has traditionally been used to describe a condition characterized by recurrent episodes of symptomatic hypoglycemia (<70 mg/dL) occurring within 2-4 hours after a high carbohydrate meal in otherwise healthy individuals.1 Although the causes and mechanisms are not well understood, it has been suggested that early RH may be the result of an exaggerated glucagon-like-peptide-1 (GLP-1) response,2 and that greater carbohydrate loads, which lead to an increased incretin effect, may result in more severe reactive hypoglycaemia.3
When diagnosing RH, it must be shown to be associated with the sympathetic and/or neuroglycopenic symptoms associated with biochemical hypoglycaemia.2 Diagnosis is often based on mixed meal evaluation; however, a high percentage of symptomatic patients test negative when using this approach.2 Use of an oral glucose tolerance test has also been shown to be insufficient to diagnose the condition.3
Although periodic ambulatory blood glucose testing has been used to investigate this condition, this approach only provides a “snapshot” of postprandial blood glucose (BG) levels; it does not take into account the potential time lag between actual biochemical hypoglycemia and recognition of symptoms, which would prompt the individual to test his/her BG. During this lag period, glucose may actually be rising in response to the action of counterregulatory hormones and the true nadir may be missed.4
Use of continuous glucose monitoring (CGM) may improve diagnosis accuracy.2 We assessed the diagnostic value of short-term CGM use in patients without diabetes with suspected RH.
This retrospective analysis included 3 patients without diabetes (1 male, 2 female) with suspected RH. Median age was 33 (range: 31-35) years; median BMI 25.2 kg/m2 (range: 19.5-31.7) Patients were asked to wear Dexcom G4 CGM system (Dexcom, Inc, San Diego, USA) for 7 days. Data were then downloaded for analysis.
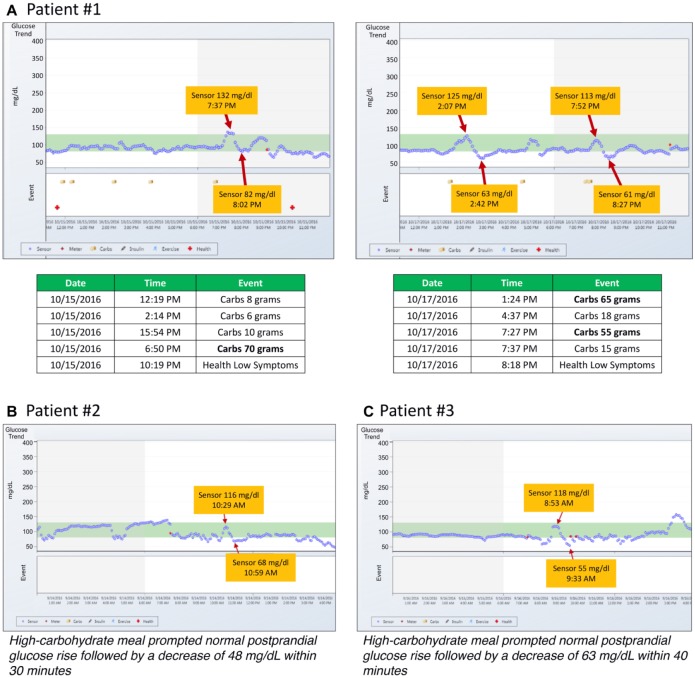
In one patient, a significant decrease in glucose was observed in response to high carbohydrate intake on two separate days (Figure 1A). These decreases occurred within approximately 30-40 minutes following peak postprandial glucose. Similar patterns following ingestion of high-carbohydrate meals were seen in the other study patients (Figure 1B and 1C). The magnitude and timing of the patterns did not appear to be associated with gender or BMI. All patients were counseled to modify their eating with a low-carbohydrate diet and frequent small split meals. These actions resolved their RH.
Figure 1.
Magnitude and timing of reactive hypoglycemia in three patients.
RH can result in debilitating symptoms similar to those experienced by patients with diabetes.2 Although dietary modification remains the first treatment of this disorder,2,5,6 individuals who do not respond to this treatment require further investigation. Utilization of CGM may provide a practical means for confirming RH in individuals without diabetes, facilitating early intervention with diet modification, assessment of treatment efficacy, and identification of individuals requiring more comprehensive evaluation.
Footnotes
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: CGP has received consulting fees from Insulet Corporation, Dexcom, Inc, Johnson & Johnson Diabetes Institute, LLC, Roche Diabetes Care, and Senseonics, Inc. QN, SP, and KC report no disclosures.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Sivakumar T, Sivakumar S, Chaychi L, Comi RJ. A review of the use of acarbose for the treatment of post-prandial syndrome (reactive hypoglycemia). Endocrinol Metabol Syndrome. 2012:S1. doi: 10.4172/2161-1017.S1-010. [DOI] [Google Scholar]
- 2. Brun JF, Fedou C, Mercier J. Postprandial reactive hypoglycemia. Diabetes Metab. 2000;26(5):337-351. [PubMed] [Google Scholar]
- 3. Vilsbøll T, Krarup T, Madsbad S, Holst JJ. Both GLP-1 and GIP are insulinotropic at basal and postprandial glucose levels and contribute nearly equally to the incretin effect of a meal in healthy subjects. Regul Pept. 2003;15:114(2-3):115-121. [DOI] [PubMed] [Google Scholar]
- 4. Olivetti I, Grassi G, Lambertenghi V, et al. Continuous glucose monitoring enhances the diagnostic value of mixed meal test in reactive hypoglycemia. Endocrine Abstracts. 2011;26:P710. [Google Scholar]
- 5. Scheen AJ, Lefèbvre PJ. Reactive hypoglycaemia, a mysterious, insidious but non dangerous critical phenomenon. Rev Med Liege. 2004;59(4):237-242. [PubMed] [Google Scholar]
- 6. Lefebvre PJ. Hypoglycemia or non-hypoglycemia. Diabetes 1991. In: Rifkin H, Colwell JA, Taylor SI. eds. Proceedings of the 14th International Diabetes Federation Congress Amsterdam: Excerpta Medica; 1991:757-761. [Google Scholar]