Abstract
Introduction and Background:
The abuse and misuse of topical corticosteroids, especially over the face, is an increasing problem encountered by dermatologists in India. Lack of patient awareness and the ease of obtaining topical corticosteroids without a prescription are important underlying factors. As the first point of contact, the pharmacist has an important role in controlling topical corticosteroid abuse.
Aims:
This study aimed to evaluate the knowledge, attitudes, and behavior regarding topical corticosteroids in a sample of pharmacy students.
Methods:
A cross-sectional survey was carried out among pharmacy students using convenience sampling method. A total of 110 questionnaires were distributed, and 103 valid responses were obtained.
Results:
Majority of the students were conversant of the fact that different classes of topical corticosteroids effectuate different effects. Majority of the students concurred on points such as topical corticosteroids can have significant cutaneous adverse effects, the important role pharmacist plays in preventing topical steroid abuse, and the need to hold fast dispensing of topical corticosteroids on a prescription-only basis. However, a significant gap in knowledge related to specific side effects and awareness of different classes of topical corticosteroids was noted. Moreover, there was no statistical significant difference in terms of knowledge and awareness regarding topical corticosteroid use between postgraduate and undergraduate students.
Conclusion:
In our study, although several students were aware of the potential adverse effects of topical corticosteroids, there were gaps in the awareness about specific classes and adverse effects. Knowledge regarding the ethical and rational use of topical corticosteroids should be disseminated among pharmacy students, and the dermatologists should play a key role in this.
Keywords: Clinical pharmacy, pharmacy students, topical corticosteroid, topical drug abuse, topical medications
Introduction
The abuse and misuse of topical corticosteroids (TC), especially over the face, is an increasing problem encountered by dermatologists in India. The exact magnitude of the problem is not clear, but there have been recent efforts to quantify the same. A multi-center trial from India by Saraswat et al., which screened 2926 patients with facial dermatosis, showed that 433 (14.8%) patients were using TC over a long period in an unsupervised manner. In this study, TC was being used for various purposes, including fairness/general purpose cream, after shave, and acne. Of note, was the fact that non-physician recommendations for TC were obtained in 257 (59.3%) of the patients, of which more than 90% were for potent/super-potent steroids. Even for physician prescriptions, a large number were given inappropriate refills.[1] The role of pharmacists is very crucial in preventing TC abuse, especially in the context of avoiding inappropriate refills for patients who are using TCs for various indications. Early awareness of the potential problems associated with TC abuse will help build a community of pharmacists who are more likely to contribute to the rational dispensing of TCs in the future. Therefore, it is important that pharmacy students are aware of the different types of TCs and the potential adverse effects of TC abuse. This study aims to assess the knowledge and attitudes of a sample of pharmacy students regarding TC use and abuse.
Methods
This study was designed as a cross-sectional survey carried out in a pharmacy college attached to a tertiary care hospital. The team responsible for conducting the survey comprised two dermatologists, two pharmacy students, and a professor of clinical pharmacy. The initiation phase commenced with validation of the questionnaire, after which the questionnaire was pilot tested among ten pharmacy students and was further refined. The questionnaire had one section dealing with basic demographics – age, year of study, and gender, followed by a general awareness section which covered awareness regarding different class/strengths of TCs and possible adverse effects. Further questions covered any prescribing experience, if present, and reflection on the role of pharmacists in preventing TC abuse. A convenience sampling method was used. The questionnaire was distributed to a convenience sample of pharmacy students in a single institute. The paper-based questionnaire was distributed to 110 pharmacy students, including both undergraduate and postgraduate students. A total of 103 valid responses were obtained (response rate of 93.6%). We also attempted to statistically compare the responses between postgraduate (36) and undergraduate students (67).
The reliability coefficient for the questionnaire (Cronbach's alpha) was 0.73. The study was exempt from review by the local ethics committee. Participation in the study was voluntary, and data confidentiality was ensured.
Results
The age group of the participants ranged from 21 to 25 years. There were 79 female and 24 male respondents. There were 36 postgraduate students and 67 undergraduate students. On the question of whether they had given any patient advice or suggestions regarding the use of TC, a majority said yes 63 (61.1%).
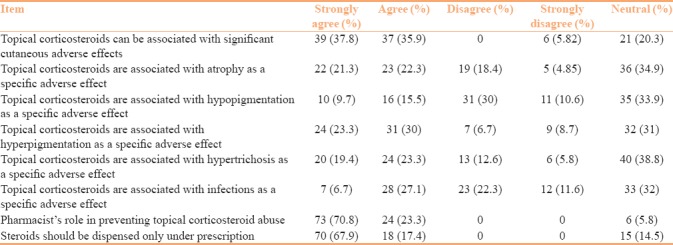
Details regarding the response to questions related to adverse effects of corticosteroids are given in Table 1.
Table 1.
Awareness about the adverse effects of topical corticosteroids
Regarding the role of pharmacists in the context of TC abuse, the main recurring themes based on the suggestions of the respondents included a role in patient counseling and patient education. Other roles mentioned include prescription auditing, limiting over-the-counter prescriptions, and monitoring and reporting adverse events.
Mann–Whitney U-test (two-tailed) was used to compare the ratings given for the two groups for the following questions:
Incidence of cutaneous adverse effect, effect of vehicles, suggestions given, and unsupervised use
No statistically significant difference was found between the two groups in any of the abovementioned questions.
Discussion
TC abuse, leading to various grades of skin damage, is one of the rampant menaces dermatologists are facing in their practice.[2] All preparations and in all vehicles tend to be carelessly purchased over the counter. In addition, prescriptions are often refilled without instructions and applied for wrong indications. The scarcity of qualified pharmacists to operate pharmacies and drug dispensaries is one reason this practice is rampant. Our study is an earnest attempt to ascertain the level of awareness, attitudes, and practices of qualified pharmacists regarding the use and misuse of TCs. The problem of TC abuse is a global issue now.[3,4] Pharmacists are key to addressing the problem of topical steroid abuse because in a country like India where patient awareness regarding drugs like TCs is low and people have easy access to the pharmacist in the pharmacy than they have to a qualified specialist.[1,5,6]
Previous studies have indicated that the pharmacist can play both positive and negative roles in the context of TC use.
In a questionnaire-based survey conducted among pharmacists who attended a continuing medical education program on pediatric atopic dermatitis, it was found that there was a significant knowledge gap regarding the safety and use of TCs among them. Their advice to patients resulted in poor compliance in the treatment of atopic dermatitis. This study also concluded that this is modifiable by adequate awareness programs preferably by dermatologists.[7] Another study by Lau and Donyai concluded that pharmacists showed gaps in the knowledge regarding the use of TCs in atopic eczema, even though they had good understanding of the use of emollients in the same disease.[8]
Another study conducted by Farrugia et al., in Australia, conducted among 201 patients and parents revealed that there is a certain amount of corticosteroid phobia among the population, which was attributed to inadequate information. General practitioners and pharmacists were more or less of the same level of inadequacy in educating the patients, and at times their statements contradicted adding to the confusion. The study also reaffirmed that pharmacists’ advice about corticosteroid use was very influential in patients’ compliance.[9] Another study from Saudi Arabia also concluded that the knowledge of primary care physicians regarding TCs is inadequate.[10]
In a study conducted in Jordan involving pharmacy students, it was observed that self-medication and even advising medication to others was very prevalent among pharmacy students. Analgesics and antibiotics were the most widely misused drugs in their study.[11] In our study, 38.2% of the respondents agreed that they had given advice regarding topical treatment to patients.
The positive aspects of our study were that a majority of the students were aware of the fact that different classes of TCs have differences in the final effects. The majority concurred on points such as topical corticosteroids can have significant cutaneous adverse effects, the importance of the role of the pharmacist in preventing topical steroid abuse, and the need to stick to dispensing TC on a prescription-only basis. However, a significant gap in knowledge related to specific side effects and awareness of different classes of TC was noted in our study. Especially of concern was the fact that many of the students were not sure of the two most dreaded complications – atrophy and pigmentary changes. This is really important as and when these students start handling TC prescriptions in the future. Training programs designed for pharmacy students to cover dermatotherapy must be as comprehensive as possible to overcome this knowledge deficit. We also found that there was no statistical significant difference in terms of knowledge and awareness regarding TC between the postgraduate and undergraduate students. We feel that this probably indicates that the coverage of dermatotherapy is minimal across both undergraduate and postgraduate teaching in pharmacy.
Conclusion
With TCs being used extensively as over-the-counter drugs, especially for wrong indications, such as fairness, the role of the first contact person becomes important. In our study, while there appeared to some awareness regarding the potential adverse effects of TCs, there is still a need to strengthen the clinical awareness about adverse effects of various medications at a deeper level. Knowledge regarding the ethical and rational use of TCs should be disseminated among pharmacy students, and dermatologists should play a key role in this. Lectures in dermatological therapy conducted by the dermatologist, during both undergraduate and postgraduate phases of pharmacy training, could help in increasing the awareness of the clinical contexts of TC use. More extensive multi-center surveys are also warranted in both pharmacy and medical undergraduates-to assess present awareness and device interventions to improve awareness related to TCs in future.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Saraswat A, Lahiri K, Chatterjee M, Barua S, Coondoo A, Mittal A, et al. Topical corticosteroid abuse on the face: A prospective, multicenter study of dermatology outpatients. Indian J Dermatol Venereol Leprol. 2011;77:160–6. doi: 10.4103/0378-6323.77455. [DOI] [PubMed] [Google Scholar]
- 2.Dey VK. Misuse of topical corticosteroids: A clinical study of adverse effects. Indian Dermatol Online J. 2014;5:436–40. doi: 10.4103/2229-5178.142486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kumar S, Goyal A, Gupta YK. Abuse of topical corticosteroids in India: Concerns and the way forward. J Pharmacol Pharmacother. 2016;7:1–5. doi: 10.4103/0976-500X.179364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Al Hawsawi K, Alaauldeen S, Albarnawi N, Mashrai H, Alosaimi R, Alsufyani H, et al. Prevalence of misuse of topical corticosteroids among populations in western region of Saudi Arabia. Int J Adv Res. 2017;5:297–307. [Google Scholar]
- 5.Nagesh TS, Akhilesh A. Topical steroid awareness and abuse: A Prospective study among dermatology outpatients. Indian J Dermatol. 2016;61:618–21. doi: 10.4103/0019-5154.193666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ashique KT, Chandrasekhar D. Role of clinical pharmacist in cosmeto-vigilance of misuse and abuse of topical corticosteroids. Indian J Dermatol. 2017;62:213. doi: 10.4103/ijd.IJD_686_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smith SD, Lee A, Blaszczynski A, Fischer G. Pharmacists’ knowledge about use of topical corticosteroids in atopic dermatitis: Pre and post continuing professional development education. Australas J Dermatol. 2016;57:199–204. doi: 10.1111/ajd.12339. [DOI] [PubMed] [Google Scholar]
- 8.Lau WM, Donyai P. Knowledge, attitude and advice-giving behaviour of community pharmacists regarding topical corticosteroids. Pharmacy (Basel) 2017;5:pii: E41. doi: 10.3390/pharmacy5030041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Farrugia LL, Lee A, Fischer G, Blaszczynski A, Carter SR, Smith SD, et al. Evaluation of the influence of pharmacists and GPs on patient perceptions of long-term topical corticosteroid use. J Dermatolog Treat. 2017;28:112–8. doi: 10.1080/09546634.2016.1213353. [DOI] [PubMed] [Google Scholar]
- 10.Alsukait SF, Alshamlan NM, Alhalees ZZ, Alsuwaidan SN, Alajlan AM. Topical corticosteroids knowledge, attitudes, and practices of primary care physicians. Saudi Med J. 2017;38:662–5. doi: 10.15537/smj.2017.6.17586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alkhatatbeh MJ, Alefan Q, Alqudah MA. High prevalence of self-medication practices among medical and pharmacy students: A study from Jordan. Int J Clin Pharmacol Ther. 2016;54:390–8. doi: 10.5414/CP202451. [DOI] [PubMed] [Google Scholar]


