Abstract
Introduction
The burden of poisoning exposures in Africa is a significant public health concern, yet only ten African countries have poisons information centres. The establishment of poisons centres was subsequently identified as a priority. This article focuses on workshop discussions with international multi-sector stakeholders in Eastern Africa regarding the possibility of a sub-regional poisons centre serving multiple countries.
Methods
The project was led by an independent consultant under the guidance of an international steering group. Steering group members provided input at international multi-stakeholder meetings and during monthly teleconferences.
Results
Participants of the stakeholder meetings agreed that the establishment of a sub-regional poisons centre in Eastern Africa was necessary and feasible. Virtual collaboration is possible due to recent technological developments, and the overall suggestion was for countries to establish their own poisons centres and to network and coordinate these centres through a network hub.
Conclusion
A number of benefits might result from such a poisons centre network hub, including: (1) Improved cooperation between countries on poisoning problems; (2) Harmonisation and strengthening of research and surveillance; (3) Common standards and best practices e.g. regulating chemicals, data management, and staff training; and (4) Greater bargaining power to secure resources. Further investigation is needed to identify the most suitable location for the network hub, the activities it should fulfil, and the availability of specialists in poisons information who could become members of the hub.
Keywords: Poisons centre, Africa, Stakeholder meetings, Network hub
Abstract
Introduction
La charge que représentent les expositions à l’empoisonnement en Afrique est une préoccupation de santé publique importante, et pourtant, seuls une dizaine de pays africains sont dotés de centres d’information antipoison. La création de centres antipoison a donc été identifiée comme une priorité. Cet article se concentre sur les discussions de l’atelier organisé avec les parties prenantes multisectorielles internationales en Afrique de l’Est concernant la possibilité de la création d’un centre antipoison sous-régional desservant plusieurs pays.
Méthodes
Le projet a été mené par un consultant indépendant, sous la direction d’un groupe de pilotage international. Les membres du groupe de pilotage ont apporté leur contribution lors de réunions internationales multipartites et de téléconférences mensuelles.
Résultats
Les participants des réunions des parties prenantes ont convenu que la mise en place d’un centre antipoison sous-régional en Afrique de l’Est était nécessaire et faisable. La collaboration virtuelle est possible grâce aux récents développements technologiques, et la suggestion générale était que les pays établissent leurs propres centres antipoison et mettent en réseau et coordonnent ces centres par le biais d’une tête de réseau.
Conclusion
Une telle tête de réseau de centres antipoison pourrait présenter un certain nombre d’avantages, notamment: (1) Une amélioration de la coopération entre les pays sur les problèmes d’empoisonnement; (2) Une harmonisation et un renforcement de la recherche et de la surveillance; (3) Des normes communes et des meilleures pratiques, par exemple la réglementation des produits chimiques, la gestion des données et la formation du personnel; (4) Une meilleure position de négociation pour obtenir des ressources. Une enquête plus approfondie est nécessaire pour identifier l’emplacement le plus approprié pour la tête de réseau, les activités qu’elle devra remplir et la disponibilité de spécialistes en information antipoison qui pourraient participer à cette tête de réseau.
African relevance
-
•
The article provides information about the existing poisons centres in Africa and the services they provide.
-
•
Poisoning exposures in Africa are challenging, under-reported, and present a significant public health burden.
-
•
To address the lack of poisons centres in Africa, this study was initiated to investigate the feasibility of a sub-regional poisons centre serving multiple countries.
1. Introduction
The burden of poisoning exposures in Africa is a significant public health concern. However, only ten of 58 countries (17.2%) have poisons information centres (PICs). The true extent of acute poisonings in Africa is not known. It is difficult to obtain accurate figures since poisoning cases are usually poorly documented. Reasons include lack of resources and knowledge to diagnose poisoning, the fact that only certain acute poisonings are required to be reported to the local or national department of health, and low levels of death registration. Hence, it is difficult to obtain reliable epidemiological data. According to WHO estimates based on data from 2012, unintentional poisoning accounts for 39,800 deaths and 27,949,000 DALYs in the UN Africa region.1, 2
Acute poisoning is a manifestation and result of the interplay between psychological, economic, cultural, policy/legislation, and other regional factors. This is illustrated by the marked inter-population differences in the nature and magnitude of the problem, particularly when contrasting developed and developing countries. Studies have revealed that deliberate self-harm is a common form of acute poisoning in the developing world.3 The mortality rate is often high, due to (1) the inherent toxicity of the poisons taken, (2) the greater availability of highly toxic chemicals and products because of weak regulation, (3) ingestion of large doses, and (4) poor medical care.3 The lack of infrastructure and financial resources are further limitations that may have a profound effect on health strategies in Africa. Many countries have very limited resources to detect, measure, and manage the effect of chemicals on health, as exemplified by the lack of PICs, toxicological expertise among health professionals, and laboratory analytical facilities.
The Strategic Approach to International Chemicals Management (SAICM) is a global policy framework to foster the sound management of chemicals.4 Its goal is to produce and use chemicals in ways that will minimise significant adverse impacts on the environment and human health by 2020.4 Initial capacity-building activities for the implementation of SAICM objectives are supported by the Quick Start Programme (QSP), a fund administered primarily by the United Nations Environment Programme.5
The SAICM African regional group identified the establishment of PICs as a priority need, and the possibility of a sub-regional poisons centre serving multiple countries was suggested. The Zambia Environmental Management Agency (ZEMA), on behalf of the Eastern Africa sub-region, secured funding for the project from the Quick Start Programme. The World Health Organisation (WHO) was the executing agency for the project due to a long-standing programme of work directed at assisting countries to establish and strengthen PICs. The overall objectives of the project were: (1) To document the incidence of poisoning exposures in the East African sub-region; (2) To identify existing PIC services in the sub-region; (3) To identify the different models of PIC service provision and reasons for their establishment; and (4) To explore options to improve the availability of PIC services in Africa. The project was divided into three phases to meet the set objectives: Phase (1) An extensive literature review (objectives 1 & 2); Phase (2) A survey (objectives 1–3); and Phase (3) National and international multi-stakeholder consultations (objective 4).
2. Methods
An independent consultant under the guidance of a steering group (Table 1) conducted the 18-month project. The role of the steering group was to provide technical input and oversight of the project to ensure that it met its objectives. Steering group members attended the international multi-stakeholder meetings and provided further input during monthly teleconferences.
Table 1.
List of steering committee members in alphabetical order.
| Member’s name | Affiliation | Country |
|---|---|---|
| Mr. Nick Edwards (Independent consultant) | Nick Edwards Consulting Ltd | London, United Kingdom |
| Mr. Christopher Kanema | Zambia Environmental Management Agency | Lusaka, Zambia |
| Mr. David Kapindula | Zambia Environmental Management Agency | Lusaka, Zambia |
| Ms. Carine Marks | Tygerberg Poison Information Centre | Cape Town, South Africa |
| Dr. Tom Menge | Poison Information and Management Centre; Kenyatta National Hospital | Nairobi, Kenya |
| Mr. Caesar Nyadedzor | Poison Information Centre | Accra, Ghana |
| Dr. Clare Roberts | Red Cross Children’s Hospital Poisons Centre | Cape Town, South Africa |
| Mrs. Hawa Senkoro | WHO Regional Office for Africa | Libreville, Gabon |
| Prof. Dexter Tagwireyi | Drug & Toxicology Information Service | Harare, Zimbabwe |
| Ms. Joanna Tempowski (supervisor of the project) | World Health Organization (WHO) | Geneva, Switzerland |
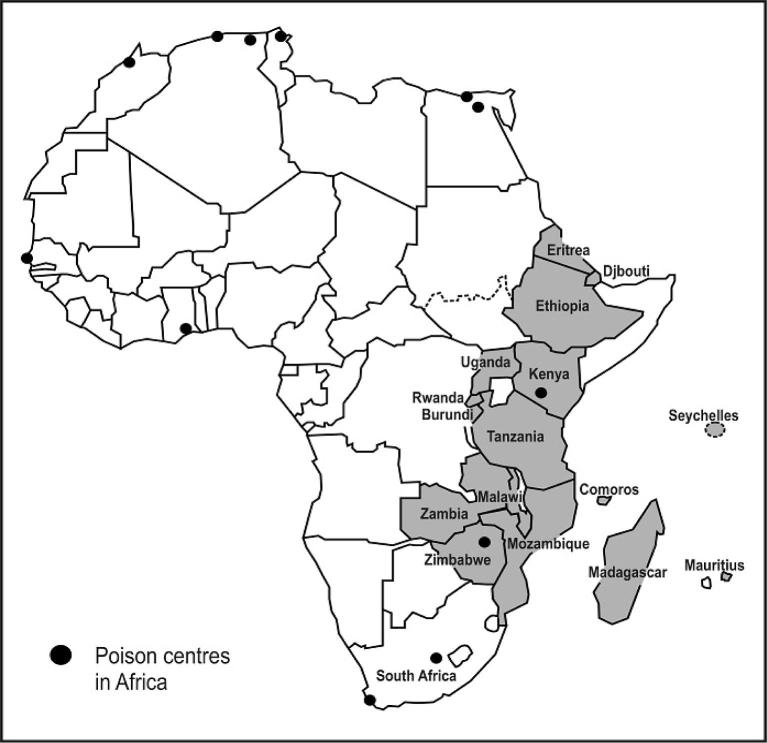
Sixteen countries (Fig. 1) within the Eastern Africa sub-region that have a SAICM National Focal Point (NFP) were included in the first two phases of the study. The SAICM NFP is the officially-designated representative for communication on SAICM issues and activities in countries. Somalia and South Sudan, which have no SAICM NFP, and Reunion and Mayotte, which are French overseas departments with different legal status and levels of autonomy, were excluded from the study.
Figure 1.
Map of Africa with the 16 countries with a SAICM NFP (in dark) in Eastern Africa that were included in the study. Each dot in the map represents a poisons centre.
The specific objectives of the multi-stakeholder consultation meetings were: (i) To identify and explore different models of PIC service provision, and (ii) To determine the requirements for the establishment of PIC services in Africa.
The main participating countries were Kenya and Zimbabwe, which have PICs, and the United Republic of Tanzania and Zambia, which do not. There were two international multi-stakeholder meetings, one at the start of the project (June 2012) and one towards the end (May 2013). National meetings were also held in Kenya, Zimbabwe, United Republic of Tanzania, and Zambia.
Participants for the national and international multi-stakeholder meetings were drawn from purposive sampling. They included members of PICs and poisons centre host institutions (e.g. hospitals); representatives of ministries of health, environment, agriculture, labour and industry; medical/nursing/pharmacist professional associations; SAICM NFPs and relevant non-government organisations such as those concerned with consumer safety and pesticide safety. Educational authorities and bodies (e.g. those involved in training of medical/nursing and other frontline health workers) and industry e.g. (CropLife Africa) were also invited.
During the first international multi-stakeholder meeting (June 2012) and the four national meetings (September to October 2012), stakeholders were informed about the roles and functions of PICs, and views were sought about the desirability and practicality of a sub-regional poisons centre. Participants were asked for ideas on how PIC services could be provided and funded. It was also recognised that there would be a need to agree on protocols and procedures to allow cross border operation, both in respect of ethical and medico-legal issues and also international legal issues.
The second international multi-stakeholder meeting (May 2013) included additional representatives from ministries of health from Ethiopia and Uganda. Participants were presented with the outcomes achieved thus far and information about the epidemiology of poisoning in the sub-region, results of the survey, and results from earlier consultations. The 38 participants were divided into groups to discuss the concept of sub-regional PIC services. They were to consider a number of options for providing PIC services (Table 2). For each option, participants had to identify advantages and disadvantages, prerequisites, and possible obstacles. After the meeting, a compilation of the comments on each option was circulated to meeting participants to rank each option in order of preference.
Table 2.
Possible options for providing poisons centre services in Eastern Africa.
| Option 1 | Create one ‘super-centre’ to serve the needs of Eastern Africa. This could be an expansion of an existing centre or the development of a new centre |
| Option 2 | Create a small number of PICs (grouped by language) to serve multiple countries in the sub-region. Where possible, these should build on existing centres, and not necessarily just those within Eastern Africa |
| Option 3 | The PIC service should be provided by means of an internet-based toxicology database, to which users must subscribe and that logs each contact. This could be maintained by a commercial entity or a PIC in Africa or abroad |
| Option 4 | Each country should be encouraged to create and maintain its own PIC service |
| Option 4 (variant) | Each country should be encouraged to create and maintain its own PIC service. These centres would be networked and coordinated through a network hub |
| Option 5 | The status quo should be maintained, i.e. no new PICs would be created |
3. Results
Participants of the international multi-stakeholder meetings made certain recommendations regarding the sustainability and standard operating procedures of a sub-regional PIC:
-
•
The telephone service would need to be multilingual and at a minimum would have to be able to handle enquiries in English, French, Portuguese, Arabic, and possibly Swahili.
-
•
There would need to be good telecommunications infrastructure linking all of the countries.
-
•
The centre would need to have up-to-date information on products, plants, and venomous animals from all countries in the sub-region, as well as information on clinical and laboratory services in each country.
-
•
There would need to be political support and agreement between the ministries of health, finance, trade, and justice of all countries involved.
-
•
There would need to be a protocol on how issues of accountability and medical liability would be handled in case a patient had an unexpectedly bad outcome.
-
•
Issues regarding patient confidentiality and product confidentiality need to be addressed.
-
•
There would need to be an international steering committee with all countries that were contributing to the centre’s funding represented.
-
•
There would need to be an adequate number of trained staff to handle a potentially large number of calls from 16 countries on a 24/7 basis.
-
•
There would need to be significant start-up investment for premises, IT and telecoms infrastructure, staffing and training.
Meeting participants recognised a number of benefits that might be derived from a sub-regional poisons centre:
-
•
Improved cooperation between countries on poisoning problems.
-
•
Harmonisation and strengthening of research and surveillance.
-
•
Common standards and best practices e.g. regulating chemicals, data management, and staff training.
-
•
A sub-regional centre could have greater bargaining power to secure resources.
-
•
It would be more economical to have a sub-regional centre than for each country to have its own centre.
A number of obstacles and disadvantages for setting up a sub-regional PIC were also recognised:
-
•
Who would be responsible for procuring funding? (Start-up and maintenance).
-
•
Language barriers between different countries.
-
•
Significant administrative workload to ensure that all user-countries were participating and paying their share for the service.
-
•
The host-country might become politically unstable, threatening continuation of the sub-regional service.
-
•
Political unwillingness to share information about poisoning events, patients, and products.
-
•
Medico-legal barriers (e.g. regulations and laws relating to standards of medical care, confidentiality, and liability).
-
•
A single sub-regional poisons centre would not always be accessible to all rural communities.
-
•
The host-country would benefit the most and professional training and experience relating to toxicology would be weakened in other countries.
There was a general support for the creation of PIC services and particularly the creation of individual national centres with a coordinating hub (option 4 variant), which was ranked first by the stakeholder group (Table 3).
Table 3.
Ranking of options for improving PIC services in the sub-region.
| Options | Average score |
|---|---|
| Option 4 (variant) | 4.9 |
| Option 4 | 4.4 |
| Option 2 | 3.4 |
| Option 1 | 2.3 |
| Option 3 | 1.9 |
| Option 5 | 0.6 |
The concept of the network hub (Fig. 2) had originated in the national meeting in the United Republic of Tanzania, and its purpose and role were further elaborated during steering group discussions and at the second international meeting. It was felt that the network hub could provide the following:
-
•
Coordination of training of PIC staff. Capacity building through teaching and training could be offered to all health care providers in Africa e.g. via the development of an agreed training curriculum and training materials, as well as arranging training visits.
-
•
Promoting standardisation between PICs e.g. in treatment advice and documentation of enquiries.
-
•
Sign-posting, i.e. directing members to other resources / sources of assistance.
-
•
Advocacy on behalf of the PICs for national and international recognition and funding.
-
•
Toxicovigilance.
-
•
Contributing to the common good in terms of its role in chemical safety and public health.
Figure 2.
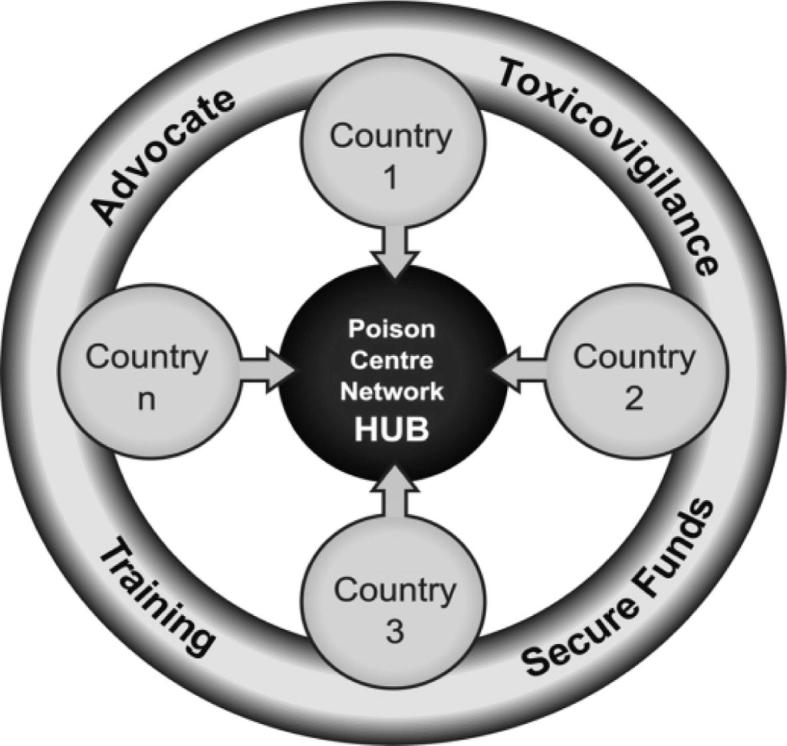
Poisons centre network hub concept.
During the course of the project, four countries (Uganda, Ethiopia, United Republic of Tanzania, and Zambia) started to work on plans to establish national PICs. A separate meeting was held between representatives from these countries. The project steering group provided feedback on the plans and some guidance on how to start, run, and fund a PIC.
4. Discussion
Participants of the international multi-stakeholder meetings agreed that the establishment of a sub-regional PIC in Eastern Africa was necessary and feasible, although there was a marked preference for national centres. If there were to be a sub-regional service, this would require political and financial support, technical input, and material resources. The governments involved should share the costs and a suitable formula would need to be devised. The possibility of support from industry was also mentioned; however, the basis of support and whether it could be purely financial or in kind was not explored.
The main barriers to the development and operation of a sub-regional PIC service were considered to be cultural, ethical, and medico-legal obstacles. The costs of initiating such a service and unsustainable funding were also seen as significant barriers.
This project encouraged countries to establish their own PICs in the Eastern Africa sub-region and to network and coordinate these through a network hub. The findings could be applied in any other sub-region in Africa or any other country that has more than one PIC. The hub could either be based at an existing PIC or could operate as a virtual centre, in a similar way to some professional associations (i.e. with dedicated officers but not necessarily with a fixed location). The hub would be supported by clinical toxicologists, analytical toxicologists, and any other person(s) who could contribute to this service.
The project had stimulated four countries to develop proposals for creating their own PIC. In one country, the United Republic of Tanzania, this has come to fruition and the poisons centre has recently opened. One of the project outputs was a toolkit for establishing a PIC. This will be published shortly as part of the summary report of the project.
The international multi-stakeholder meeting’s participants were representatives from the four close-study countries (Kenya, United Republic of Tanzania, Zambia and Zimbabwe), two additional countries (Ethiopia and Uganda), the steering committee, representatives from the Food and Agricultural Organisation (FAO), and Crop Life Africa. Due to financial constraints, representatives from other countries that were part of the wider study were not included.
While the hub concept was well-liked, there was some ambivalence regarding its establishment and members. A comprehensive survey or Delphi-study6 should be carried out to identify the most suitable location, the activities it should fulfil, and the availability of professionals with expertise on different aspects of toxicology who could become members of the hub.
5. Conclusion
PICs are needed to meet the current and future burden presented by poisoning. It is important that future PIC platforms in Africa are realistic, appropriate, and cost-effective. Due to important technological developments (telephonic and computing), virtual collaboration is now possible and can be utilised globally by PIC teams. Although reliance on technology is not always straightforward, it can be cost-effective and can give an opportunity for experts to collaborate so that their joint knowledge can contribute to PIC developments.
Conflict of interest
This project was funded by the Quick Start Programme of the Strategic Approach to International Chemicals Management (SAICM) (project number X.04.G.ZMB). Nick Edwards and Dexter Tagwireyi were paid from project funds for work carried out as part of the project. The other authors declare no conflict of interest.
Footnotes
This is an Open Access article published under the CC BY-NC-ND 3.0 IGO license which permits users to download and share the article for non-commercial purposes, so long as the article is reproduced in the whole without changes, and provided the original source is properly cited. This article shall not be used or reproduced in association with the promotion of commercial products, services or any entity. There should be no suggestion that WHO endorses any specific organisation, products or services. The use of the WHO logo is not permitted. This notice should be preserved along with the article’s original URL.
References
- 1.Estimates for 2002–12. Cause-specific mortality. World Health Organization; Geneva: 2014. Disease and injury country mortality estimates, WHO Member States 2012. World Health Organization; [cited 2015 Jul 14]; < http://www.who.int/healthinfo/global_burden_disease/estimates/en/index1.html>. [Google Scholar]
- 2.Estimates for 2002–12. Disease burden. World Health Organization; Geneva: 2014. DALY estimates: WHO Member States, 2012. World Health Organization; [cited 2015 Jul 14]; < http://www.who.int/healthinfo/global_burden_disease/estimates/en/index2.html>. [Google Scholar]
- 3.Eddleston M. Patterns and problems of deliberate self-poisoning in the developing world. QJM. 2000;93:715–731. doi: 10.1093/qjmed/93.11.715. [DOI] [PubMed] [Google Scholar]
- 4.SAICM – Strategic Approach to International Chemicals Management; [cited 2015 Jun 29]; <http://www.unep.ch/saicm/index.php?menuid=2&pageid=256>.
- 5.QUICK START PROGRAMME [Internet]. Rotterdam Convention; <http://www.pic.int/Implementation/TechnicalAssistance/Funding/SAICMQuickStartProgramme/tabid/2449/language/en-US/Default.aspx>.
- 6.Timbie J.W., Damberg C.L., Schneider E.C. A conceptual framework and protocol for defining clinical decision support objectives applicable to medical specialties. BMC Med Inform Decis Mak. 2012;12(93):1–12. doi: 10.1186/1472-6947-12-93. < http://www.biomedcentral.com/1472-6947/12/93>. [DOI] [PMC free article] [PubMed] [Google Scholar]