Abstract
Introduction
Electronic Medical Records (EMRs) have shown benefit for clinical, organisational, and societal outcomes. In low-to-middle-income countries, the desire for EMRs will continue to rise as increasing trauma and infectious disease rates necessitate adequate record keeping for effective follow-up. 114 nations are currently working on national EMRs, with some using both a full EMR (Clinicom) and a paper-based system scanned to an online Enterprise Content Management (ECM) database.
Methods
The authors sought to evaluate the ability and completeness of the EMR at Khayelitsha Hospital (KH) to capture all Emergency Centre (EC) encounters classified as trauma. Based on the high trauma rates in the Khayelitsha area and equally high referral rates from KH to higher-level trauma centres, an assumption was made that its rates would mirror nationwide estimates of 40% of EC visits. Records from July 2012 to June 2013 were examined.
Results
3488 patients visited the EC in the month of July 2012. 10% were noted as trauma on Clinicom and within their records were multiple sections with missing information. The remaining months of Aug 2012–June 2013 had an average trauma load of 8%. On further investigation, stacks of un-scanned patient folders were identified in the records department, contributing to the unavailability of records from January 2013 to the time of study (June 2013) on ECM.
Conclusion
The results highlight difficulties with implementing a dual record system, as neither the full EMR nor ECM was able to accurately capture the estimated trauma load. Hospitals looking to employ such a system should ensure that sufficient funds are in place for adequate support, from supervision and training of staff to investment in infrastructure for efficient transfer of information. In the long run, efforts should be made to convert to a complete EMR to avoid the many pitfalls associated with handling paper records.
Keywords: Electronic Medical Records, South Africa, Trauma, Khayelitsha District Hospital
Abstract
Introduction
Les dossiers médicaux informatisés (DMI) ont prouvé leur intérêt en termes de résultats cliniques, organisationnels et sociétaux pour de nombreux hôpitaux. Dans les pays à faible et moyen revenu, la volonté de disposer de DMI continuera à progresser à mesure que les taux croissants de traumatismes et de maladies infectieuses exigent une tenue de dossiers adéquate afin d’assurer un suivi efficace. Cent quatorze pays travaillent actuellement à la mise en place de DMI nationaux, certains utilisant à la fois un système de DMI complet (Clinicom) ainsi qu’un système de documents au format papier scannés et ajoutés à une base de données de Gestion de contenu d’entreprise (GCE) en ligne.
Méthodes
Les auteurs ont cherché à évaluer la capacité et l’exhaustivité du système de DMI au sein de l’hôpital de Khayelitsha (HK) à saisir toutes les visites classées comme traumatismes. Sur la base des forts taux de traumatisme enregistrés dans la région de Khayelitsha, et des taux de renvoi proportionnellement élevés du HK vers des centres de traitement des traumatismes de plus haut niveau, l’hypothèse a été émise que les taux enregistrés dans cet hôpital reflèteraient les estimations nationales de 40 % des visites au CU. Les archives de juillet 2012 à juin 2013 ont été examinées.
Résultats
3488 patients ont consulté au CU au mois de juillet 2012. Dix pour cent ont été enregistrés comme traumatismes dans Clinicom, plusieurs sections de leur dossier comportant des informations manquantes. Les mois suivants d’août 2012 à juin 2013 indiquaient une proportion de traumatismes de 8 %. Après examen plus approfondi, des piles de dossiers de patients non scannés ont été identifiées au sein du service des dossiers, ceci contribuant à l’indisponibilité des dossiers de janvier 2013 jusqu’au moment de l’étude (juin 2013) dans le GCE.
Conclusion
Les résultats soulignent les difficultés associées à la mise en œuvre d’un système de tenue de dossiers double, car ni le DMI complet, ni le GCE ne pouvaient saisir avec précision la proportion estimée de traumatisme. Les hôpitaux qui cherchent à utiliser de tels systèmes devraient s’assurer que des fonds suffisants sont disponibles afin de permettre de soutenir adéquatement ce système, allant de la supervision et de la formation du personnel à l’investissement dans les infrastructures, afin de permettre un transfert d’informations efficace. À long terme, des efforts devraient être réalisés afin de pouvoir passer à un système de DMI et d’éviter les nombreux écueils associés à la tenue de dossiers au format papier.
African relevance
-
•
Electronic Medical Records (EMRs) have shown benefit for clinical, organisational, and societal outcomes.
-
•
In low- to- middle-income countries, the desire for EMRs will continue to rise as increasing trauma and infectious disease rates necessitate adequate record keeping for effective follow-up and research.
Introduction
A male passenger is extricated from a motor vehicle accident, and he is immediately expedited to an emergency centre (EC) complaining of chest pain. After a quick physical exam, the doctor determines that it is unlikely to be of muscular origin and proceeds to workup for a myocardial infarction. As the doctor was about to order sublingual nitroglycerin, she noticed from the patient’s record that he was currently on sildenafil, in which case nitroglycerin could cause massive vasodilation, severe hypotension, and death. Furthermore, as she was about to order aspirin, she again noticed that the patient was recently admitted for a massive gastrointestinal bleed, causing her to hold off on both medications. Two errors were thus averted in a span of minutes.
Error detection like this is one of the many benefits of Electronic Medical Records (EMRs). An EMR is “a longitudinal electronic record of patient health information generated by one or more encounters in any care delivery setting. Included in this information are patient demographics, progress notes, problems, medications, vital signs, past medical history, immunisations, laboratory data, and radiology reports”.1, 2, 3 In high-income countries, the popularity of EMRs has soared because of its many benefits,3, 4 which can be divided into three major spheres. First, they affect clinical outcomes by improving the quality of care and reducing medical errors, increasing “safety, effectiveness, and efficiency.”1 Secondly, they affect organisational outcomes by increasing revenue, averting costs from redundant tests and medications, and decreasing legal vulnerability of hospitals. Thirdly, they affect societal outcomes by facilitating research, promoting population health by making it easier to monitor diseases, and increasing job satisfaction among physicians.1, 5, 6Recognising these benefits, in 2009, the US government enacted the Health Information Technology for Economic and Clinical Health (HITECH) Act, which provides financial incentives for both hospitals and physicians to adopt EMR systems.1
The popularity of EMRs is not restricted to high-income countries, however. Many low- to middle-income countries (LMICs) have recognised the value of EMRs and have modified the technology to fit their needs within known resource constraints. According to a WHO survey, 114 nations are currently working on National EMR systems.7 They have been implemented in HIV management in South Africa, Kenya, Rwanda, Ghana, Lesotho, Zimbabwe, Mozambique, Sierra Leone, Uganda, and Tanzania, as well as in various countries in Central and Latin America.7 In Africa, the major impetus for this change is the rise in infectious diseases as the leading cause of death,8 with HIV and multi-drug resistant TB being major culprits. Patients with these conditions often require continuous treatments and long-term care, necessitating an efficient record keeping system.9, 10, 11 Some of these systems are “open source,” characterised by open-source codes that are freely available to anyone who wishes to examine or change them for his or her own purpose.11 Compared to proprietary systems, which more likely cater to wealthier customers in high-income countries,7 open-source systems are much cheaper because, among other things, they take away the burden of licensing and software upgrade costs and offer customisability for consumers.7, 10 This has provided more affordable systems such as the one implemented in 2012 at an urban emergency centre in Kumasi, Ghana.5
Although each of the nine provinces in South Africa employs a different system, one of the goals of the country is to fully integrate these systems to facilitate communication and achieve the full benefits.12 In the Western Cape, for example, Clinicom dominates the EMR market.13, 14 It is a proprietary system,15 controlled by JAC Computer Services, an IT specialist company that was awarded a contract to implement a fully electronic record system in which patient information is directly entered to the computer in 38 different hospitals and specialised care centres across the Western Cape.16 However, it has been plagued with challenges due to bandwidth requirements in health facilities and low levels of computer literacy and motivation to use the system correctly.14, 17 Furthermore, due to medico-legal requirements within the South African government and some resistance from clinicians to use full EMRs, some hospitals have chosen to also maintain paper records.3 To keep these organised and allow for sharing of these records both within the hospital and with neighbouring hospitals, the paper records are scanned and stored in an online database, an example of which is Enterprise Content Management (ECM).3
Khayelitsha hospital (KH) is one that has both systems and will be at the centre of this report. KH is a 240-bed facility opened in 2012 to serve the estimated 400,000 people in the Khayelitsha area.18, 19, 20 2011 census data characterise the Khayelitsha population as predominantly Black African (55%), with 74% of households having monthly income of R3200 or less and 55% living in informal dwellings.20 2007 estimates show antenatal HIV prevalence of 33% and a high incidence of TB.19 According to the Institute of Development studies, police-released crime statistics for 2007/08 ranked Khayelitsha among the top areas in South Africa for murder, rape, and aggravated robbery.21 With respect to murder, its statistics are “over two and a half times the South African average of 41 per 100,000”.21 Of note, overall South African statistics are already over 20 times the murder rates of countries in Western Europe.21 The proposed causes of violent crime in Khayelitsha have been traced to poverty, transience of the population, and historical lack of effective policing.21, 22 Anecdotal evidence reveals a high incidence of trauma, including a recent BBC documentary that featured interviews with frontline doctors and members of rival gangs in the Khayelitsha township.23 There is also a significant rate of community assaults, although objective estimates are lacking.22 This is not unexpected, as 90% of traumatic deaths occur in LMICs.24 After infectious diseases, trauma is the leading cause of death in Africa.8, 25 South Africa specifically has one of the highest trauma rates in the world, accounting for up to 40% of all visits to the EC.26, 27 The National Injury Mortality Surveillance system revealed in 2007 that one-third of injury-related deaths were due to violence in South Africa, followed by traffic injuries.28 These numbers are slight underestimates, as efforts to create trauma databases still fail to identify many.28 At neighbouring Groote Schuur Hospital, a higher-level trauma centre that receives referrals of trauma cases from KH, a prospective recording of patients during a one-year period revealed 9236 cases of injury-related visits, with the most common causes including assault with a sharp (20.9%) or blunt object (17%), traffic collisions (18.8%), and falls (18.4%).28 It was reported that these injuries occurred in neighbouring townships including Khayelitsha.28 KH was therefore built with a 30% larger Accident and Emergency Unit than that of a standard district hospital29 to care for these patients.
With the popularity of EMRs rising in South Africa, for quality assurance it became necessary to evaluate the implementation of one of these systems in a South African hospital. The desire was to select a hospital that was representative of the burdens of hospitals in LMICs in hopes that by examining the successes and failures, other hospitals may be better equipped to emulate successful practices and avoid pitfalls. KH was selected for several reasons. First, trauma rates in South Africa have been heavily studied, with calculated estimates of its burden across the country. Khayelitsha is a low-income township with high rates of community assaults, anecdotal evidence of higher trauma rates, and objective evidence of frequent referrals of trauma patients to higher-level hospitals; by extrapolation, trauma-related visits to the EC in KH should be at least equal to the estimates of up to 40% of all EC visits attributable to trauma. Third, KH was built recently and with a dual medical record system in place from the beginning. Therefore, it would be less likely to have a backlog of paper records waiting to be scanned from previous years, as would be expected in an older hospital that had to change its system. Fourth, because the management strives for excellence in healthcare delivery, it has made KH a hub for research for people around the globe.22, 30
Methods
The EC at KH has five sections, each with its own registry based on the severity of the patient’s situation: the Green room, Asthma room, Trolley area, Resuscitation area, and Paediatrics. Each patient coming to the EC is given an episode folder containing their unique patient identification barcodes and form labels, while triage nurses assign severity codes using vital signs and other criteria specific for the South African Triage Scale (SATS). The SATS has been shown to predict patient outcomes with 75% sensitivity and 91% specificity when used as a triage tool in an EC.31 The validity and utility of this scale has been described elsewhere.31, 32 Based on the SATS code, patients are sent to different sections of the EC. A patient’s name, chief complaint, and ID number are recorded in the paper registry for each section. When healthcare professionals see a patient, hand-written notes and any other records are placed in folders. These are picked up by the clerks at the end of each day, who then transcribe the events onto the Clinicom Electronic Record system while the folders are sent to the records department to be scanned into the ECM system to be available electronically for future visits or if a patient needs to be transferred for higher-level care. Therefore, for each patient visit, there are three pieces of evidence: a short summary of their visit in one of the registries, the scanned copies of the doctor and any other notes onto the ECM system, and the Clinicom record of the same episode directly typed in either by the clinicians or the clerks.
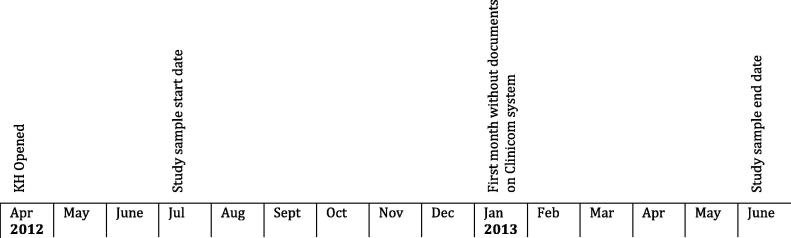
Since the hospital opened its doors in April 2012, the records before July were excluded from the audit to allow a few months of adjustment. Using a random number generator, July 2012 was selected for a detailed audit that involved transcription of individual records for completeness. All other months from July 2012 to June 2013 were also analysed (see Fig. 1 for the timeline). For the month of July 2012, a list of all the patients who visited the EC was extracted using the Clinicom system. From this list, those patient numbers that were designated as trauma were also extracted. For each patient with this designation, identification numbers were entered into the ECM system to find the specific record of that episode. Efforts were made to confirm that it was indeed a trauma case, defined as injury to tissue caused by physical harm from an external source.33 In each of the charts, all the information that could be gleaned was recorded, including demographic information, vital signs, and SATS numbers, as these gave an idea at the completeness of each chart. To ensure that all patient episodes were included, the Clinicom list was cross-referenced with those found on the paper registries. Furthermore, overall data from other months were used to identify and confirm trends. Children below the age of 12 or less than 150 cm were excluded from the sample for adequate comparability of injury severities, as a different version of the SATS is used for paediatric visits.
Figure 1.
Timeline of events at KH.
Approval for the study was granted by the Yale School of Medicine and by KH.
Results
On the Clinicom EMR, there were 3488 patients who visited the EC in July 2012. Of those, 288 were classified as trauma, giving a trauma load of 8% (288/3447). An additional 66 cases were found in one of the five paper registries available for each month. The other four registries could not be found. This brought the total trauma load to 10% (354/3488). For the remaining months (Aug 2012–June 2013), the average trauma rate was 8%. For some of these months, there were entire days without records despite a record of a trauma case in the paper registry that was found (see Table 1).
Table 1.
Days of missing records for each study month.
| Month | No. of trauma cases on Clinicom | Dates without records |
|---|---|---|
| July 2012 | 288 | Missing day 5 |
| Aug | 335 | |
| Sept | 430 | |
| Oct | 388 | |
| Nov | 336 | Missing day 14, 29 |
| Dec | 441 | |
| Jan 2013 | 142 | Missing day 27 |
| Feb | 124 | Missing day 11 |
| March | 187 | Missing day 5, 6, 10, 23, 24, 27 |
| Apr | 177 | Missing day 3 |
| May | 235 | |
| June | 325 |
For the 354 trauma cases that were found on the Clinicom EMR for the month of July, patient identification numbers were typed into the ECM online database to look specifically at the episode and extract further data. 46 cases were excluded because patients were below 12 years of age. For the rest, 15% had missing or incomplete records, 73% had no time of arrival, 37% no time of triage, and 38% had no SATS code, some of which was due to missing vital signs.
For any patient who came into the hospital after January 1, 2013, if one searched for the record of their visit on the ECM online database, one would get an error message. Of note, this audit was conducted in July 2013.
Discussion
As said in the background, the actual proportion of EC visits attributed to trauma at KH is not known. However, based on estimates that nearly 40% of EC visits nationwide in South Africa are trauma-related, the notoriety of Khayelitsha as an area prone to violence, and the high rates of referrals from KH to higher-level trauma centres including Groote Schuur Hospital, the trauma load calculated in this study is most likely a gross underestimation. This was confirmed by additional cases found in the paper registries stored in a cabinet in the EC. As described earlier, each of the five sections in the EC keeps its own paper registry. Since only one of those registries could be found (and in it were 66 additional cases), it is safe to assume that more cases would have been found if all the paper registries were available, or ideally, if they were reflected in the Clinicom EMR. The low trauma load of 10% persisted throughout the months of August 2012–June 2013 despite the evidence of high trauma rates in the EC, confirming suspicions that these problems were not isolated to the month of July.
Incompletely filled paper charts, difficult to decipher handwriting, and missing notes are expected in any record system that depends on paper records and is one of the reasons full EMRs are the way of the future. Handwriting that is difficult to decipher leads to medical errors (e.g., administration of wrong medications). Furthermore, missing healthcare provider notes defeat the purpose of having a record system, while incompletely filled charts go against the “societal outcomes” benefit of EMRs mentioned earlier. EMRs should provide records at a glance to facilitate quality research, which is the foundation for development in the field of medicine. Since a working EC depends on effective triage, without “time to triage” and SATS codes, one cannot evaluate EC effectiveness and therefore figure out ways to improve. Incompletely filled charts are as detrimental as not filling charts at all and prevent healthcare professionals from doing their jobs effectively.
To have no online records after the month of January 2013 makes work very difficult for healthcare professionals, particularly considering that this audit was performed six months later. Some of the missing folders were stacked in the medical records department waiting to be scanned. These missing folders prevent doctors and nurses from accessing important patient information and more importantly, the benefits of EMRs outlined in the introduction cannot be realised. It has also led to another problem. For those patients called “super users” or “frequent flyers” who come into the EC multiple times a month, some healthcare professionals have learned to store these folders in their offices so they can refer to them on the patient’s next visit. The problem is that by keeping these files, they contribute to the cycle of missing folders.
Overall, it is evident there was some difficulty with the implementation of a dual system at KH. The Clinicom EMR was not adequately utilised. Some of the paper registries were missing at the time of the study, even though one could argue that if available, they would have been more accurate than the Clinicom system, since the one paper folder that was found recorded more trauma cases than the EMR during the same time period. Some of the records that were available on the online database were either incompletely filled out or missing whole sections. The stacks of records waiting to be scanned and the unavailability of these records in the online database hampered the effectiveness of the ECM online database. If the ultimate aim of the Western Cape and South Africa as a whole is to have a fully integrated EMR system, why has the paper record system persisted? A non-exhaustive list of reasons include: the medico-legal requirements by the South African Government to have ‘hardcopy’ documentation of patient records,3 the cultural difficulties to the clinician when his/her decision-making is available for everyone to see and judge, difficultly managing life and death situations in the EC while at the same time fiddling with a system that is relatively new, and the typical challenges associated with any new technology, such as the acquisition of typing skills and a minimal comfort level with technology.2, 3
One can posit that the aim of the dual system was to allow for a transition period whereby clinicians could continue to use paper records for documentation, which were scanned to the online database to be available for effective communication while these same clinicians slowly familiarise themselves with a full EMR system. The dual system, however, does not seem to be working at KH. In a resource-limited area, fixing this problem will involve short-term and long-term changes. In the short term, the goal is to figure out ways to optimise the ECM online database. This should involve increasing resources, manpower, supervision, and training.2 One example of a change in resources concerns the lack of vital signs in patient charts. It could be that temperature and blood pressure measurements are left out of patient charts because thermometers and blood pressure cuffs are scarce in the hospital. These vital signs, however, cannot be overlooked, as they are used to calculate patient severity scores, which have been shown to be sensitive and specific predictors of patient outcomes. It could also be that the healthcare workers do not know how to use these instruments. Or, it could be that the healthcare workers do not record these values because there is no accountability for not doing their jobs. All of these are possible reasons for incompletely filled out folders, and any hospital looking to use systems like this should first address these issues. Another example of lacking resources can be seen in the medical records department, where there are workers and adequate supervision, yet there are only a few scanners available in a hospital that serves the needs of the 400,000 residents of Khayelitsha. Meeting such demands is quite a difficult task to achieve, as evidenced by the stacks of folders waiting to be scanned in the records office. Although improvements in these areas require upfront costs, they are necessary to achieve the full advantages of the ECM online database.
In the long term, a complete conversion to a full EMR system that involves direct input of doctors’ and nurses’ notes into the computer will be the most ideal solution. Such a system should apply the “cradle to the grave” approach.6 For an efficient EMR system to be implemented, there must be important pieces in the toolkit, including the development of a system that has adaptable, interoperable, and scalable software while fostering relationships in the community to provide “technical, financial, and training support”.6 Since the Western Cape market is dominated by Clinicom, this would be the most likely system to be implemented. As expected, this is a larger undertaking, and requires a large investment to implement and maintain. Some solutions are available to help with funding. Governments like the US have provided incentives for “meaningful use” of this technology to healthcare facilities. The South African government can do the same, providing subsidies for hospitals that use the system and penalties for those that do not. Furthermore, there are cheaper and more malleable options for EMRs, such as open source versions, which would be much more feasible in a low-resource environment.
For any new technology, there is always a lag time for adjustment. This is another one of the pitfalls for the EMRs. The time can vary according to institution, with some institutions taking up to two years of dedicated effort to achieve full use.2 It could be that KH needs a few years for all the systems to come into place and fully realise the benefits of the installed records system. Further research should look at how efficient the system is in the coming years. Additionally, this study had only a small sample. Though KH is a large and fairly representative hospital of those in South Africa installing EMRs, this study only looked at the effects on one department in one large hospital. Future studies should look at more hospitals to determine whether there are common issues and solutions. Finally, as both the registry and Clinicom were incomplete, it was difficult to establish a gold standard for the trauma load at KH. It is possible that some of the encounters on Clinicom were incorrectly coded as non-trauma, thereby underestimating the trauma load.
Conclusion
The desire for EMRs in LMICs will continue to rise with increasing rates of trauma and infectious diseases. With this increased pressure, hospitals and governments have a few options. If they choose to employ semi-EMR systems like ECM (that require the scanning of paper records into a database), they should ensure that their budgets account for the difficulties encountered in this audit, including adequate training and supervision of workers and increased investment in necessary resources. In the long run, efforts should be made to transition into a full EMR system that does not depend on paper records. Like a building without a foundation, a hospital without an adequate records system will be more prone to breaking down.
Author contributions
E.O. and J.S. conceived of the original idea and designed the experiments with input from K.J. and L.W. E.O. collected the data and carried out the analysis in South Africa. L.W. provided the necessary clearance. E.O., J.S., and K.J. prepared the manuscript. All authors approved the final version.
Conflict of interest statement
The authors have no conflict of interest.
Acknowledgements
We appreciate the sponsorship of the Down’s Fellowship and Yale School of Medicine. We also thank the staff and management at Khayelitsha Hospital for allowing us to be there.
Footnotes
Peer review under responsibility of African Federation for Emergency Medicine.
References
- 1.Menachemi N., Collum T.H. Benefits and drawbacks of electronic health record systems. Risk Manag Healthcare Policy. 2011;4:47–55. doi: 10.2147/RMHP.S12985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Payne T.H., tenBroek A.E., Fletcher G.S. Transition from paper to electronic inpatient physician notes. JAMIA. 2010;17(1):108–111. doi: 10.1197/jamia.M3173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weeks R. The successful implementation of an Enterprise Content Management System within the South African Healthcare Services Sector. In: Proceedings of PICMET ‘13: Technology Management for Emerging Technologies. 2013.
- 4.Blaya J.A., Fraser H.S., Holt B. E-health technologies show promise in developing countries. Health Aff. 2010;29(2):244–251. doi: 10.1377/hlthaff.2009.0894. [DOI] [PubMed] [Google Scholar]
- 5.Forson P.K., Oduro G., Forson M.S. The use of open source electronic medical records in an urban ED in Kumasi-Ghana. Afr J Emerg Med. 2013;3(4):S14. [Google Scholar]
- 6.The Promise of Electronic Medical Records. Rockefeller Foundation 2013; <http://www.rockefellerfoundation.org/uploads/files/b54cdca2-e5ba-473a-bc29-70aee1af9a19-silos-to.pdf>. Accessed November 13, 2013.
- 7.Webster P.C. The rise of open-source electronic health records. Lancet. 2011;377(9778):1641–1642. doi: 10.1016/s0140-6736(11)60659-4. [DOI] [PubMed] [Google Scholar]
- 8.Hardcastle T., Oteng R. Trauma care in Africa: Triumphs and Challenges. Afr J Emerg Med. 2011;1(2):53–54. [Google Scholar]
- 9.Forster M., Bailey C., Brinkhof M.W. Electronic medical record systems, data quality and loss to follow-up: survey of antiretroviral therapy programmes in resource-limited settings. Bull World Health Organ. 2008;86(12):939–947. doi: 10.2471/BLT.07.049908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Millard P., Bru J., Berger C. Open-source point-of-care electronic medical records for use in resource limited settings: systematic review and questionnaire surveys. BMJ Open. 2012 doi: 10.1136/bmjopen-2011-000690. < http://bmjopen.bmj.com/content/2/4/e000690.full.pdf+html>. Accessed December 15, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kalogriopoulos NA, Baran J, Nimunkar AJ, et al. Electronic medical record systems for developing countries: review. Conference proceedings: Annual International Conference of the IEEE Engineering in Medicine and Biology Society. IEEE Engineering in Medicine and Biology Society. Conference. 2009:1730–1733. [DOI] [PubMed]
- 12.Kahn T. Government paves the way for move to paperless hospitals. Health Systems Trust 2014; <http://www.hst.org.za/news/government-paves-way-move-paperless-hospitals>. Accessed December 13, 2013.
- 13.Dlodlo N. Potential applications of the internet of things technologies for South Africa’s Health Services. Adv Inf Technol Appl Comput. 2013;1 [Google Scholar]
- 14.Mars M., Seebregts C. Country case study for e-Health South Africa. eHealth Res Innov Platform. 2013 [Google Scholar]
- 15.Electronic Health Record for South Africa. Department of Health of Republic of South Africa 2008; <http://southafrica.usembassy.gov/root/pdfs/pepfar-hmis-docs/ndoh-e-hr-for-south-africa.pdf>. Accessed November 24, 2013.
- 16.Healthcare Technology is Changing Lives in the Western Cape. News 24 2012; <http://www.news24.com/MyNews24/Healthcare-Technology-is-Changing-Lives-in-the-Western-Cape-20121010>. Accessed May 15, 2013.
- 17.eHealth strategy South Africa 2012. National eHealth Strategy, South Africa. 2012.
- 18.Moyo S., Cox H.S., Hughes J. Loss from treatment for drug resistant tuberculosis: risk factors and patient outcomes in a community-based program in Khayelitsha, South Africa. PLoS One. 2015;10(3):e0118919. doi: 10.1371/journal.pone.0118919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Coetzee D., Hilderbrand K., Boulle A. Outcome after two years of providing antiretroviral treatment in Khayelitsha, South Africa. AIDS. 2004;18:887–895. doi: 10.1097/00002030-200404090-00006. [DOI] [PubMed] [Google Scholar]
- 20.City of Cape Town-2011 Census Suburb Khayelitsha. Statistics South Africa. 2013.
- 21.Nleya N., Thompson L. Survey methodology in Violence-prone Khayelitsha, Cape Town, South Africa. IDS Bull. 2009;40(3) [Google Scholar]
- 22.Forgus S., Delva W., Hauptfleisch C. Community v. non-community assault among adults in Khayelitsha: A case count and comparison of injury severity. South Afr Med J. 2014;104(4):299. doi: 10.7196/samj.7615. [DOI] [PubMed] [Google Scholar]
- 23.Hamid R. Reggie Yates’s Extreme South Africa: Knife Crime ER. BBC2014.
- 24.Petroze R., Calland F., Mukarugwiza F. Role of outcomes assessment in injury surveillance in resource-limited settings (poster) Afr J Emerg Med. 2011;1:147–150. [Google Scholar]
- 25.Curry E. South Africa: New, Assertive Women’s Voices in Local Elections. Inter Press Service News Agency [Press release]. 2011; Jan 28, 2011: <http://www.ipsnews.net/2011/01/south-africa-new-assertive-womens-voices-in-local-elections/>. Accessed May 17, 2013.
- 26.Wallis L.A. Trauma Care in South Africa-a call to arms. South Afr Med J. 2011;101(3) doi: 10.7196/samj.4802. [DOI] [PubMed] [Google Scholar]
- 27.Wallis L.A., Garach S.R., Kropman A. State of emergency medicine in South Africa. Int J Emerg Med. 2008;1(2):69–71. doi: 10.1007/s12245-008-0033-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nicol A., Knowlton L.M., Schuurman N. Trauma surveillance in Cape Town, South Africa: an analysis of 9236 consecutive trauma center admissions. JAMA Surg. 2014 doi: 10.1001/jamasurg.2013.5267. [DOI] [PubMed] [Google Scholar]
- 29.Rossouw H. New Khayelitsha Hospital Officially Opened. Western Cape Government [Press Release]. 2012; April 2012: <http://www.westerncape.gov.za/news/new-khayelitsha-hospital-officially-opened>. Accessed May 15, 2013.
- 30.Griggs R., Andronikou S., Nell R. World Federation of Pediatric Imaging (WFPI) volunteer outreach through tele-reading: the pilot project in South Africa. Pediatr Radiol. 2014;44(6):648–654. doi: 10.1007/s00247-014-2948-6. [DOI] [PubMed] [Google Scholar]
- 31.Twomey M., Wallis L.A., Thompson M.L. The South African triage scale (adult version) provides valid acuity ratings when used by doctors and enrolled nursing assistants. Afr J Emerg Med. 2012;2(1):3–12. doi: 10.1016/j.ienj.2011.08.002. [DOI] [PubMed] [Google Scholar]
- 32.Gottschalk S.B., Warner C., Burch V.C. Warning Scores in Triage – Is there a point? Afr J Emerg Med. Sept 2012;2(3):103–107. [Google Scholar]
- 33.Trauma. Merriam Webster Dictionary; 2015.