Abstract
Introduction
Sub-Saharan Africa (SSA) has a need for blood and blood products that exceeds current availability. This unmet demand is evidenced by persistently high mortality rates associated with potentially reversible conditions such as haemorrhage and anaemia. This study reviews current literature on blood donation in SSA to identify common local motivators and deterrents to blood donation and highlights specific interventions that have successfully increased the number of blood donors in this region.
Methods
The authors searched the health literature to identify original studies conducted in SSA that addressed blood donation motivators and deterrents. Data were then extracted from each study to determine how often each study identified specific motivators and deterrents.
Results
Pro-social motivation, such as altruism and the desire to have a positive effect on the community, is the most frequently noted reason for people in SSA countries to donate blood. Negative attitudes and misconceptions towards blood donation, in addition to perceived negative health effects caused by donation, are the two most frequently mentioned reasons that dissuade individuals from donating blood.
Conclusion
Due to paucity of research on this topic, our understanding of blood donor behaviour in SSA is limited. Local traditions and cultures intimately shape individuals’ proclivity towards the donation process. In order to change the attitudes and behaviours of many potential donors in SSA it is important to address the deterrents to blood donation, as many represent misconceptions or culture-specific beliefs that may be the ultimate driving force dictating donor behaviour.
Keywords: Blood availability, Blood donation, Donor attitudes, Donor knowledge, Sub-Saharan Africa
Abstract
Contexte
L’Afrique sub-saharienne (ASS) a un besoin de sang et de produits sanguins en quantité supérieure à la disponibilité actuelle. Cette demande non satisfaite est démontrée par un maintien à un niveau élevé des taux de mortalité liés à des maladies potentiellement réversibles telles que l’hémorragie et l’anémie. Cette étude examine la littérature actuelle sur le don de sang en ASS afin d’identifier les facteurs de motivation et de dissuasion locaux communs en matière de don de sang et de mettre en évidence des interventions spécifiques qui sont parvenues à augmenter le nombre de donneurs de sang dans cette région.
Méthodes
les auteurs ont étudié la littérature dans le domaine de la santé afin d’identifier les études originales menées en ASS qui traitaient des facteurs de motivation et de dissuasion en matière de don de sang. Les données ont ensuite été extraites de chaque étude pour déterminer la fréquence à laquelle chaque étude a identifié des facteurs de motivation et de dissuasion spécifiques.
Résultats
La motivation pro-sociale, telle que l’altruisme et le désir d’avoir un impact positif sur la communauté, est la raison la plus fréquemment citée pour laquelle les personnes donnent leur sang en ASS. Les attitudes négatives et les idées fausses à l’égard du don de sang, outre la perception des effets sanitaires négatifs causés par le don, sont les deux raisons les plus fréquemment citées qui dissuadent les individus de donner leur sang.
Conclusion
En raison de la rareté des études sur ce sujet, notre compréhension du comportement des donneurs de sang en ASS est limitée. Les traditions et cultures locales façonnent intimement le penchant des individus à donner leur sang. Afin de changer les attitudes et les comportements de nombreux donateurs potentiels en ASS, il est important de lutter contre les facteurs de dissuasion en matière de don de sang, car bon nombre font état d’idées fausses ou de croyances spécifiques à la culture qui peuvent être la force motrice décisive conditionnant le comportement des donateurs.
African relevance
-
•
Sub-Saharan Africa has a substantial need for blood transfusions that greatly outweighs availability.
-
•
Mortality rates due to conditions associated with anaemia are persistently high.
-
•
There is a paucity of research investigating blood donor behaviour in this region.
-
•
Knowledge of blood donor behaviour is vital to the design of successful donation campaigns.
Introduction
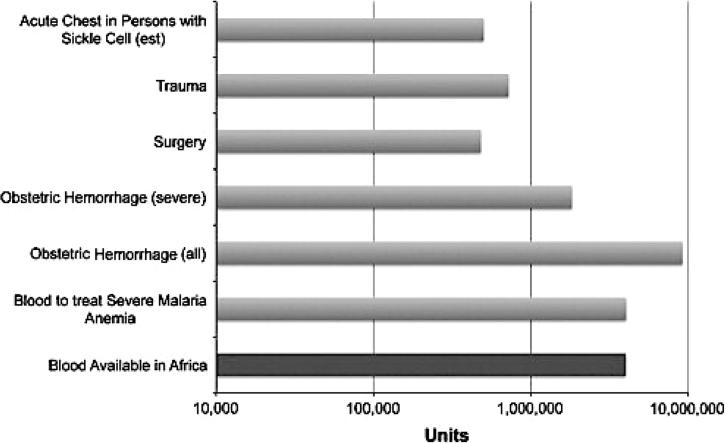
Transfusion of blood and blood products in the appropriate clinical setting can be a lifesaving measure. However, millions of patients in low-income countries (LICs) do not have timely access to this vital resource.1 Sub-Saharan Africa (SSA) has one of the largest and poorest populations in the world with substantial transfusion requirements and a need for blood and blood products that exceeds current availability (Fig. 1).2 This unmet need is demonstrated by continually high mortality rates associated with reversible conditions of acute blood loss including haemorrhage and anaemia.
Figure 1.
Amount of blood currently available compared to the calculated estimated need for common transfusion indications in SSA.
Reproduced from Lund et al. (2013) with permission from Elsevier.
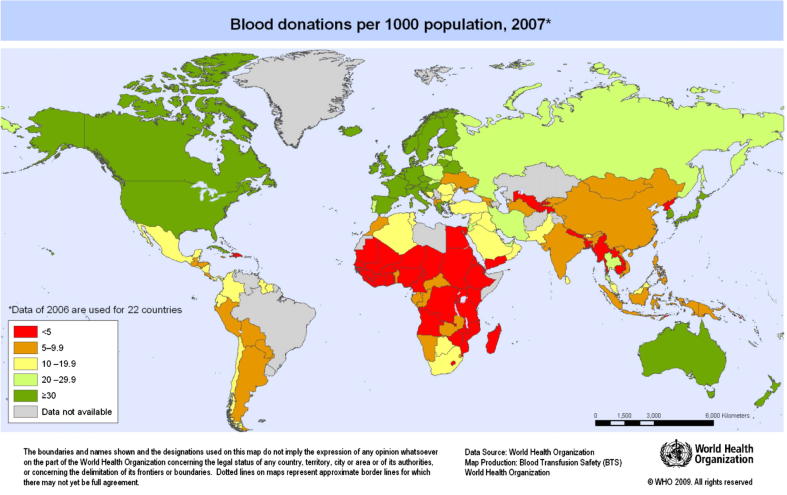
The World Health Organization (WHO) estimates that roughly 108 million units of blood are donated globally each year.3 Approximately half of these donations occur within high-income countries (HICs), which constitute only 18% of the world’s population.4 The disparity between HICs and LICs becomes more evident when comparing donation rates. The WHO estimates a blood donation rate of 1% would meet a nation’s most basic blood requirements.5 The median blood donation rate in HICs is 3.68%, 1.17% in middle-income countries, and only 0.39% in LICs (Fig. 2.3 Of the 75 countries with donation rates of <1%, 40 countries are in the WHO African Region.3, 4 In 2006, the countries in SSA collected less than half of their estimated minimum blood donation requirement.6 Overcoming these deficiencies is essential to not only meeting the transfusion needs of the population but also reaching three health-related Millennium Development Goals: reducing child mortality, improving maternal health, and combating HIV/AIDS, malaria, and other diseases.7
Figure 2.
Reproduced with permission of the WHO (Blood Transfusion Safety, 2009).
Anaemia is a major cause of child mortality in SSA and complicates one-third of childhood hospital admissions with febrile illnesses.8 The Fluid Expansion as Supportive Therapy (FEAST) trial conducted in East Africa found that 52% of severely anaemic children (haemoglobin <5 g/dL) who did not receive blood transfusions died within 8 h of hospital admission,8 90% of whom died within 2.5 h.8 In contrast, the mortality rate amongst those who received a blood transfusion on hospital admission dropped to 4%.8 This data emphasizes that prompt initiation of blood transfusion therapy is vital for the survival of these children.
SSA has the highest maternal mortality rate in the world, and post-partum haemorrhage, accounting for 33.9% of maternal deaths, is the leading cause.9 Of the estimated 536,000 maternal deaths that occur worldwide each year, 99% occur in developing countries, with more than half occurring in SSA.10 Access to safe blood could prevent up to one-quarter of these maternal deaths every year.5
A WHO Global Burden of Disease report lists trauma as a major cause of death and disability worldwide, and traumatic injuries are projected to disproportionately increase in LICs11, 12 where 90% of trauma-related deaths result from haemorrhage.3, 4, 5 The lack of blood and blood products to treat this projected increase will be felt the most in LICs, where the blood supply is already dwarfed by the current demand.
Africa’s population is expected to more than double from 1.1 billion in 2014 to 2.4 billion by the year 2050.13 The majority of this additional population growth will be in SSA.13, 14 By the end of this century, 40% of the world’s population will be African, up from 15% in 2014, and 1.1 billion children under 18, or 47% of the world’s children, will be living in Africa.15 This population expansion will increase the need for blood and blood products, putting an additional strain on SSA’s transfusion services.14
Separate from the shortage of available blood, SSA faces numerous challenges to providing universal access to safe blood: the prevalence of transfusion-transmissible infections (TTIs) is high, the lack of infrastructure and human resources limits the efficacy and number of transfusion centres, inappropriate clinical use of blood leads to potentially unnecessary transfusions, and the chronic blood shortage is often exacerbated by unstable political environments and economies.16 To combat some of these challenges, the WHO Regional Office for Africa has implemented blood transfusion policies that aim to improve the safety as well as sufficiency of the region’s blood supply.16
To specifically address blood transfusion safety, the WHO, in consortium with other international humanitarian organizations, has urged all countries to obtain their blood supplies entirely from voluntary, non-remunerated donors (VNRD) by the year 2020.5, 6 Voluntary donors are considered safer because they are thought to have the lowest prevalence rates of TTIs.6 Compared to other types of blood donors, voluntary donors are more likely to donate blood regularly, thereby increasing the availability of blood and enabling transfusion centres to maintain constant and reliable supplies.8 This is particularly important in emergency situations when blood is needed immediately, or for multiple recipients.6 The strategy of relying exclusively on VNRDs has been challenged: a recent literature review on blood donor safety suggests that VNRDs do not have lower rates of TTIs than family or replacement donors, and sole reliance upon them increases the cost of blood acquisition of one unit of blood by two- to fivefold.17, 18
Most countries with donation rates below the 1% threshold continue to rely heavily on family or replacement donors, and in some instances on paid donors.5 In 2011, 62 countries reported national blood supplies based entirely on VNRDs; 68% of them developed nations.5 Forty countries continue to collect less than 25% of their blood supplies from VNRDs, and less than 9% of blood collected in LICs comes from voluntary donors.5 Achieving 100% voluntary blood donation will be challenging in SSA where, despite relying on all types of donors, many countries are still unable to meet the minimum need for blood transfusions from all sources combined.19 In order to limit the already existing blood shortage and maintain affordability of the blood supply in SSA, voluntary as well as family or replacement donors should be encouraged to donate regularly.17, 18
Irrespective of a country, blood donation rates fundamentally depend on the willingness of individuals and communities to donate blood. In order to ultimately provide universal access to safe blood, it is imperative to focus on recruiting more blood donors. While a family or replacement donor gives blood because a family member or friend is in immediate need of a transfusion, voluntary and repeat donors donate blood out of a personal desire to do so. Blood donation campaigns with messages that appeal to the perceptions, attitudes, and behaviours that influence an individual’s willingness to donate blood are therefore particularly effective recruiting strategies. Consequently, understanding and investigating personal and cultural motivators and deterrents to blood donation and structuring donor recruitment campaigns that appeal directly to that audience may bolster efforts to successfully recruit potential donors.
The importance of this outreach is evident in places where donor recruitment strategies have successfully increased blood donation rates. Club 25, launched in Zimbabwe in 1989, where students pledged to donate blood 25 times by the time they reached the age of 25, has been an effective and inexpensive way of targeting young donors.20 Today, Club 25 International is a youth-oriented global community of blood donors, reaching members in over 65 countries.21 The Club’s social networking features and use of social media is particularly appealing to young individuals because it allows members to connect with other donors around the world, make new friends, share stories, and “have fun while saving lives.”22 Voluntary blood donors in Ghana, some of whom became repeat donors, were recruited through a local radio broadcast, a low-cost strategy that appealed to the public through socially and culturally effective means.20
Although previous studies have identified factors that influence blood donation in the developed world, research on this topic in LICs, particularly SSA, is scarce. While available literature describes some of the drivers of donor behaviour in this region, it remains unknown how to use this information to recruit the critical mass of donors required to reach the WHO minimum blood donation rates. Additionally, the cultural constructs that influence an individual’s likelihood to donate blood are unclear. This literature analysis aims to identify common motivators and deterrents to blood donation in SSA and highlights specific interventions that have successfully increased the number of blood donors in the region.
Methods
Two researchers independently conducted a literature search using PubMed (1966–December 2014), Africa-Wide Information (1966–December 2014), and Scopus (1960–December 2014). All searches were conducted between May and December 2014. The results were then compared to ensure reliability and exhaustiveness.
Search strategies included controlled vocabulary terms and synonymous free-text words to capture the concepts of “blood donors,” “transfusions,” “motivators,” “deterrents,” “psychology,” and “Sub-Saharan Africa.” Search strategies were adjusted for syntax appropriate for each database/platform. [See Appendix A for PubMed search strategy.] Published original research papers that addressed blood donation motivators or deterrents, and were conducted in SSA, were included in the analysis. Results were not limited by language, date, or study design. Studies that did not specifically address motivators or deterrents to blood donation, and studies that were not conducted in the SSA region, were excluded.
The authors extracted data from each study, including the sample size, demographic characteristics of study participants, and study design (Table 1). Because each study used different terminology to identify various motivators and deterrents, the nomenclature was normalized so that a standard vocabulary could be used for analysis.
Table 1.
Original studies that addressed blood donation motivators or deterrents and were conducted in SSA.
| Study | Country | Authors | Publication date and language | Sample size | Sample selection | Research method delivery |
|---|---|---|---|---|---|---|
| Emotional-motivational barriers to blood donation among Togolese adults: a structural approach | Togo | K. Alinon, K.; Gbati, P.C.; Sorum, E. Mullet | Transfusion Medicine 2013 English | 400 | Adults who are either university educated or are employed in the civil administration with a position of responsibility | Paper questionnaire administered by trained researchers. Factor analysis performed on 250 of the responses |
| Can family or replacement blood donors become regular volunteer donors? | Ghana | Asenso-Mensah, K | Transfusion 2013 English | 513 | Family replacement donors, at a blood donor clinic, who had just finished donating blood and who agreed to complete questionnaire and were eligible to be a repeat donor | Self-administered questionnaire |
| Knowledge, Attitude, and Practice of Voluntary Blood Donation among Healthcare Workers at the University of Benin Teaching Hospital, Benin City, Nigeria | Nigeria | Nwogoh, B.; Aigberadion,U.; Nwannadi, A. I. | Journal of Blood Transfusion 2013 English | 163 | Healthcare workers (non physicians) from different hospital department selected by quota sampling | Self-administered questionnaire |
| Attitudes towards blood donation and transfusion in Bamenda, Republic of Cameroon | Republic of Cameroon | Koster, J.; Hassall, O.W. | Transfusion Medicine 2011 English | Not reported | Clinical and laboratory staff, patients, relatives, blood donors, secondary school students and community members at one hospital | Direct observation, in-person interviews, focus group discussions and a simulation exercise. Different sample populations were selected for different research methods |
| Knowledge and behaviour towards voluntary blood donation among students of a tertiary institution in Nigeria | Nigeria | Salaudeen, A.G.; Odeh, E. | Nigerian Journal of Clinical Practice 2011 English | 400 | Students from one university selected using multistage sampling | Self-administered questionnaire |
| Community survey on blood donation practices in a northern state of Nigeria | Nigeria | Salaudeen, A.G.; Musa, O. I.; Awoyemi A.O.; Bolarinwa, A.O.; Adegboye, A. O.; Samuel, S.O. | Journal of Preventive Medicine and Hygiene 2011 English | 936 | Community members in Kwara State, North Central Nigeria, selected using multistage sampling | Semi-structured questionnaire administered by trained research assistants |
| Sociodemographic and attitudinal factors to blood donation in the urban population of Dakar, Senegal | Senegal | Duboz, Priscilla, Macia, Enguerran, Cunéo, Bernard | Transfusion 2010 English | 600 | Combined quota method (cross-section by age, sex, and town of residence) selecting subjects who represent the population of the department of Dakar age 20 and over | Structured in-person interview |
| Antenatal blood donation for pregnant Nigerian mothers: the husbands’ perspective | Nigeria | Obi, S.N. | Journal of Obstetrics and Gynaecology 2007 English | 640 | Husbands of pregnant mothers | Self-administered questionnaire |
| Lack of knowledge among blood donors in Burkina Faso (West Africa); potential obstacle to transfusion security | Burkina Faso | Nebie, K.Y.; Olinger, C.M.; Kafando, E.; Dahourou, H.; Diallo, S.; Kientega, Y.; Domo, Y.; Kienou, K.; Ouattara, S.; Sawadogo, I.; Ky, L.; Muller, C.P. | Transfusion Clinique at Biologique 2007 French | 544 | Blood donors from an urban teaching hospital selected using systematic sampling | Self-administered questionnaire |
| Socio-cultural barriers to voluntary blood donation for obstetric use in a rural Nigerian village | Nigeria | Neema, S.; Ahmed, F H.; Onuh, S O.; Umeora, M C.; Kibombo, R.; Umeora, O U | African Journal of Reproductive Health 2005 English | 143 | Patients’ relatives who declined donating blood | Structured in-person interview |
| Knowledge, attitudes, beliefs and motivations towards blood donations among blood donors in Lagos, Nigeria | Nigeria | Olaiya, M.A.; Alakija,W.; Ajala, A.; Olatunji, R.O. | Transfusion Medicine 2004 English | 542 | Blood donors in one hospital selected using systematic sampling | Self-administered questionnaire. Donors who could not read and write were assisted in filling out the questionnaires |
| Blood donation behaviour and beliefs among a sample of high school students in Mmabatho | South Africa | Mwaba, K., Keikelame,M.J. | Curationis 1995 English | 40 | Students, 20 female and 20 male, chosen at random in one high school | Self-administered questionnaire |
| Attitudes and beliefs toward blood donation among adults in Mwanza region, Tanzania | Tanzania | B. Jacobs, Z.A. Berege | East African medical journal 1995 English | 1423 | Residents of the Mwaza Region selected using multistage sampling | In-person structured interview |
| Attitudes of Nigerians toward blood donation and blood transfusion | Nigeria | Robert A. Okpara | Tropical and geographical medicine 1989 English | 246 | Questionnaires distributed to individuals in local markets, streets, government offices and students from the University of Calabar | Self-administered questionnaire |
| A survey in Benin City, Nigeria. Attitude to blood donation and blood transfusion | Nigeria | Oyarebu, K.A. | International journal of health education 1982 English | 210 | Cluster sampling of students, civil servants and unemployed individuals in Benin | Self-administered questionnaire |
The authors used the set of categories (taxonomies) created by Bednall and Bove in their meta-analysis on self-reported motivators and deterrents to donating blood in countries worldwide.23 Because the focus of their paper was not specific to donors in SSA, Bednall and Bove’s taxonomy was not entirely sufficient for our purposes, and categories were adjusted accordingly (Table 2, Table 3). Due to the considerable heterogeneity in population selection, size, survey delivery, and use of qualitative survey methods in the available literature, motivators and deterrents to blood donation were categorized and then quantified for analysis (Table 2, Table 3).
Table 2.
Motivators to Blood Donation.
| Motivator | Definition/example | Number of studies identifying specific motivators |
|---|---|---|
| I. Pro-social motivation | The desire to have a positive impact on other people or social collectives through blood donation | |
| Altruism | Motivation with the ultimate goal of increasing the welfare of one or more individuals (especially strangers) through blood donation without regard for social or material rewards. Ex: To save a life | 13 |
| Collectivism (community) | Motivation with the ultimate goal of increasing the welfare of a group or collective through blood donation. (In this category, the target group is the donor’s community.) Ex: Feeling of belonging to a community | 1 |
| Collectivism (friends or family) | As above. (In this category, the target group is the donor’s friends and family.) Ex: For a friend or relative needing blood. For a parent in hospital | 6 |
| II. Marketing communications | The use of promotional tools such as advertising, public relations, personal selling, sales promotion, and direct and online marketing to recruit and/or retain donors. Includes direct marketing, advertising and blood drives | 5 |
| III. Indirect reciprocity | Engaging in blood donation, in response to or in anticipation of an act in kind by a third party | |
| Upstream reciprocity (friends or family) | A motivation to help someone else, prompted by a friend or a family member receiving a blood product in the past. Ex: Previous bleeding in wife during delivery | 1 |
| Downstream reciprocity | A belief that if a person helps, he/she has a greater chance of receiving help in the future if needed. Ex: If I were in the same situation, I’d want someone to do the same thing. | 1 |
| Upstream (self) reciprocity | A motivation to help someone else, after having personally received a blood product in the past | 1 |
| Self-esteem | A desire to enhance attitudes of self-acceptance, self-approval, and self-respect. Ex: To get spiritual satisfaction. To feel good about myself | 1 |
| IV. Incentives | ||
| Money | 6 | |
| Blood test | Ex: To learn blood type, blood screen, infectious disease screen | 8 |
| Gift item | Ex: Refreshments, milk, beverages | 5 |
| Recognition | Ex: Certificate, publishing name in newspaper, announcing name over the radio | 7 |
| Perceived health benefits | Ex: Helps reduce obesity. Improves my health | 2 |
| V. Social norms | Expectations, obligations, and sanctions currently anchored in social groups. This includes participation in educational campaigns. Ex: Participation in antenatal blood donor programmes, under peer pressure, to be like my friends | 4 |
Table 3.
Deterrents to blood donation.
| Deterrent | Definition/example | Number of studies identifying specific deterrents |
|---|---|---|
| I. Low self-efficacy | Donors believe that they lack control over events that affect their lives and their own functioning, making donating seem too difficult | |
| Lifestyle barriers | Donor has time constraints and other commitments (work, family) they believe makes it too difficult for them to donate. Ex: Not enough time | 3 |
| Access barriers | Donor has difficulty getting to donation site or no donation site is in reachable proximity. Ex: It’s inconvenient to get to donation site | 1 |
| Perceived health limitations | Donor believes that his or her own health limits them from donating blood. Ex: Have not enough blood in the body; Female menstruation; Fasting; Not strong enough; Physically unfit | 12 |
| II. Lack of knowledge | Lack of information and understanding about the need and process of blood donation. Ex: Never heard about it; Inadequate knowledge about benefits of donation | 5 |
| III. Lack of marketing communications | Absence of promotional tools and direct marketing to recruit and/or retain donors. Ex: Never been asked to donate | 2 |
| IV. Ineffective incentives | Rewards offered to donor fail to increase motivation to donate blood. Ex: No remuneration; Would donate for financial gain | 3 |
| V. Fear | ||
| Pain/Needles | Fear of pain, needles and medical settings | 4 |
| Weakness/Fainting | Fear of becoming weak, dizzy or fainting during or after blood donation | 6 |
| Contagion | Fear of contracting a disease through blood donation. Ex: Most commonly stated are fears of contracting HIV, Hepatitis, or Gonorrhoea | 8 |
| Convulsions | Fear of having a seizure | 2 |
| Death or reduced life span | 3 | |
| Discovering illness | Fear of discovering an existing illness during the donor screening process. Ex: Fear of knowing my status; Fear of being HIV positive | 6 |
| Sexual failure | Ex: Loss of manhood; Loss of libido; Will become sterile | 4 |
| Perceived negative health effects | Donor is deterred from donating blood because of the perceived consequences a blood donation has on one’s health. Ex: Fever, high blood pressure, weight loss | 13 |
| VI. Negative attitude | A mental position or feeling towards certain ideas, facts, or persons. Ex: Exposure of [donated] blood to witchcraft; Donated blood may be sold; Blood viewed as sacred and spilling it outside of body is serious; Transfer of behavioural traits or character between donor and recipient after donation | 13 |
| VII. Family loyalty | Donor is unwilling to donate for non-relatives | 2 |
| VIII. Religious or cultural reasons | Donor is unwilling to donate for cultural reasons or because blood donation is against their religious belief | 10 |
Results
Fifteen studies investigating self-reported motivators and deterrents to blood donation were identified, conducted in eight countries in SSA, all qualitative (Table 1).24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38
Sample selection varied considerably by study. Eight of the 15 studies used convenience sampling,24, 26, 28, 30, 31, 34, 37, 38 three used quota sampling,25, 27, 29 three used multistage sampling,32, 33, 35 and one used cluster sampling36 to select their subjects. Two of the eight studies using convenience sampling made attempts to randomize their subject pools.31, 34
Nine studies used self-administered questionnaires.27, 29, 30, 31, 32, 34, 36, 37, 38 These questionnaires employed a variety of methods including open-ended questions, multiple-choice questions, and rating scales. In two studies, trained researchers were used to administer paper questionnaires.24, 32 Four studies included structured in-person interviews, and one study included focus group discussions and a simulation exercise.25, 26, 28, 35
There were a number of reasons that people were inclined to donate blood (Table 2). Pro-social motivation, the desire to have a positive effect on others or a community, includes altruism and collectivism towards family, friends, or the community. Altruism, the most frequently stated reason to donate blood, describes an individual’s motivation to become a donor to benefit another person, particularly a stranger. Collectivism refers to an individual’s motivation to help his or her family members, friends, or community. Incentives to blood donation are also important and among those, the desire to have one’s blood tested for blood type or blood-borne pathogens, as well as public recognition for donating blood were the most common.
Similarly, certain common deterrents prevented people from donating blood (Table 3). Most frequently mentioned were negative attitudes towards blood donation and perceived negative health effects caused by donation. Examples of negative attitudes include the belief that blood would be used for witchcraft or that there may be transference of character between donor and recipient of a blood transfusion. Perceived negative health effects on the donor’s health included hypertension, fever, and weight loss.
Discussion
Greater access to blood transfusions would substantially improve health outcomes in LICs. The majority of individuals who require blood transfusions in SSA are young and otherwise healthy.3 Unlike in HICs, where patients over 65 most commonly receive blood, up to 65% of blood transfusions in LICs are given to children under the age of 5. Nearly all blood transfusions in SSA are used for complications of childbirth, severe childhood anaemia, and haemorrhage due to trauma.4, 9 Limited transfusion capabilities contribute to premature deaths in this young age group and consequently increase the region’s years of potential life lost (YPLL). Unlike crude mortality rates, YPLL focuses on the social and economic consequences of mortality, thereby giving more weight to deaths among younger individuals. If premature deaths are prevented, individuals can maximally contribute to society during their lifetimes.39 In SSA, where the majority of blood transfusions are given to children and young individuals, stronger blood transfusion capabilities would undoubtedly lead to a decrease in YPLL.
Many of the attitudes and behaviours surrounding blood donation are shaped by cultural backgrounds, general beliefs, and previous experiences of individuals and communities. Understanding these variables is paramount to the design and implementation of successful blood donor recruitment campaigns. Factors that influence an individual’s decision to become a blood donor in SSA differ from those found among individuals in the developed world.36
Strategically applying our knowledge of the motivators of blood donation in SSA will likely enhance donation rates. Individuals across SSA value altruism and are generally willing to donate blood to save a life. The WHO focused its 2014 “Safe blood for saving mothers” blood donation campaign on increasing awareness about the importance of safe and timely access to blood as an essential component in preventing maternal deaths.40 Augmenting this important altruistic motivator with additional common incentives to donation, such as a small gift item, public recognition in the form of certificates, or mentioning donors in newspapers or over the radio, may present a realistic and cost-effective strategy that encourages more individuals to become donors.
The success of Club 25 may partially be attributed to a campaign whose design is based on first identifying and then effectively leveraging factors that motivate young individuals. By understanding how the behaviour of young individuals is shaped by their peers and social norms, Club 25 creates a forum through which members can connect with other like-minded individuals using social media networks.
Campaigns whose design strategy factors knowledge of what motivates specific individuals and groups to donate blood have clearly had some success. However, the overall low number of blood donors in SSA suggests that, for many potential donors, the deterrents to blood donation may overwhelm existing motivators. Although an individual may be motivated to donate his or her blood through a genuine desire to help others, his or her hesitancy to do so is often driven by a fear of blood donation or its perceived consequences. Although some fears, such as the fear of needles, may be difficult to overcome, other commonly stated fears are rooted in misinformation about the donation process.
While blood safety and supply in the WHO Africa Region has improved, overcoming deficiencies in current systems will be essential to meeting the region’s minimum requirements for blood availability.19, 41, 42 Investigations of culture-specific motivators as well as deterrents to blood donation can provide important information for constructing realistic, targeted, and ultimately successful strategies to encourage blood donation. Further research is needed to identify what governs individual donor behaviour. Finding and implementing the most effective and culturally appropriate communication tools to deliver a health campaign message will help ensure that the message not only reaches the largest number of people but also successfully motivates individuals to change their behaviour.
Few studies have investigated the determinants of blood donor behaviour and individual attitudes towards blood donation in SSA; of the more than fifty countries in this region, only eight have been included in prior research on this topic. Our results can therefore not be generalized to the entire subcontinent, and more research from other countries is needed in order to fully understand underlying factors that shape donor behaviour in this area of the world.
The variability of methodologies used in data gathering and reporting, as well as the frequent reliance on convenience sampling and self-reported data across all studies, made it difficult to statistically quantify their results. By investigating the frequency of particular factors that were mentioned across all studies, we attempted to identify broad themes regarding what motivates and deters individuals to donate blood. However, given the limitations in the reporting and quality of the available literature, we were not able to synthesize more meaningful data that takes into account sample sizes, for example.
Our literature search relied on articles that are published in PubMed, Africa-Wide Information, and Scopus, and any literature that is available outside of these databases has not been included in our analysis.
Conclusion
Blood donation in SSA is a rare event despite the substantial need for blood and blood products. While the region has the highest burden of need for blood, it has the lowest rates of donation. Local traditions and cultures intimately shape potential donors’ proclivity towards the donation process.
Pro-social motivation, which includes altruism and collectivism, reflects a desire to have a positive effect on others or a community and is the most commonly stated factor that drives individuals in SSA to donate their blood. Incentives such as public recognition or small gift items also motivate donors, and may present realistic and cost-effective ways to augment blood donor recruitment campaigns. Perceived negative health effects and negative attitudes towards blood transfusion are commonly stated deterrents to donation. Many of these factors are misconceptions or culture-specific beliefs that may be the ultimate driving force dictating donor behaviour.
Culturally appropriate educational initiatives must be developed to address these issues. Public health workers hoping to create effective campaigns to increase blood donations in SSA must understand existing cultural barriers, and should not assume generalizability of their methods to SSA or from other parts of the world. To recruit the critical mass of donors required for minimum donation rates, existing altruism-focused campaigns in SSA must also directly confront deterrents to blood donation and deliver their campaign message using the most effective communication strategies for their target audience.
Conflict of interest
The authors declare no conflict of interest.
Footnotes
Peer review under responsibility of African Federation for Emergency Medicine.
Appendix A.
Search Strategy for PubMed
“Blood Transfusion”[Mesh] OR “blood donors”[mesh]) AND (“Motivation”[Mesh] OR deterrent∗ OR motivat∗ OR “blood donors/psychology”[Mesh] OR “blood donor∗”) AND “Africa South of the Sahara”[Mesh] AND English[lang].
References
- 1.World Bank. Country and Lending groups, <http://data.worldbank.org/about/country-and-lending-groups>; 2015 [accessed 22 February, 2015].
- 2.Lund T.C., Hume H., Allain J.P. The blood supply in Sub-Saharan Africa: needs, challenges, and solutions. Transfus Apher Sci. 2013;49:416–421. doi: 10.1016/j.transci.2013.06.014. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. World blood donor day, <http://www.who.int/campaigns/world-blood-donor-day/2013/en/>; 2014 [accessed 17 February, 2014].
- 4.World Health Organization. Blood safety and availability, <http://www.who.int/mediacentre/factsheets/fs279/en/>; 2014 [accessed 17 February, 2014].
- 5.World Health Organization . A Global Framework for Action; Geneva: 2010. International Federation of Red Cross and Red Crescent Societies. Towards 100% Voluntary Blood Donation. [Google Scholar]
- 6.World Health Organization . 2009. WHO Global Consultation on 100% Voluntary Non-Remunerated Donation of Blood and Blood Components, Geneva. [Google Scholar]
- 7.Millennium Project. Millennium Development Goals, <http://www.unmillenniumproject.org/goals/>; 2015 [accessed 3 March, 2015].
- 8.Kiguli S., Maitland K., George E.C. Anaemia and blood transfusion in African children presenting to hospital with severe febrile illness. BMC Med. 2015;13:21. doi: 10.1186/s12916-014-0246-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khan K.S., Wojdyla D., Say L. WHO analysis of causes of maternal death: a systematic review. Lancet. 2006;367:1066–1074. doi: 10.1016/S0140-6736(06)68397-9. [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization, UNICEF, UNFPA, et al. 2007. Maternal Mortality in 2005: Estimates Developed by WHO, UNICEF, UNFPA, and the World Bank, Geneva. [Google Scholar]
- 11.World Health Organization. Cause-Specific Mortality: Regional Estimates for 2008, <http://www.who.int/healthinfo/global_burden_disease/estimates_regional/en/index.html> 2015 [accessed 25 January, 2015].
- 12.World Health Organization . 2008. Global Burden of Disease: 2004 Update, Geneva. [Google Scholar]
- 13.Population Reference Bureau. World population data sheet, <http://www.prb.org/DataFinder/Geography/Data.aspx?loc=246>; 2015 [accessed 3 March, 2015].
- 14.Dzik W.S., Delaney M. The future of transfusion and Africa. Transfusion. 2014;54:2791–2794. doi: 10.1111/trf.12823. [DOI] [PubMed] [Google Scholar]
- 15.You D., Hug L., Anthony D. 2014. Generation 2030: Africa. New York, NY. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.World Health Organization. Blood safety, <http://www.afro.who.int/en/clusters-a-programmes/hss/blood-safety-laboratories-a-health-technology/programme-components/blood-safety.html>; 2015 [accessed 25 January, 2015].
- 17.Allain J.P. Volunteer safer than replacement donor blood: a myth revealed by evidence. ISBT Sci Ser. 2010;5:169–175. [Google Scholar]
- 18.Allain J.P., Sarkodie F., Asenso-Mensah K. Relative safety of first-time volunteer and replacement donors in West Africa. Transfusion. 2010;50:340–343. doi: 10.1111/j.1537-2995.2009.02444.x. [DOI] [PubMed] [Google Scholar]
- 19.World Health Organization, Regional Office for Africa . 2014. Status of Blood Safety in the WHO African Region: Report of the 2010 Survey. Geneva. [Google Scholar]
- 20.Tagny C.T., Owusu-Ofori S., Mbanya D. The blood donor in Sub-Saharan Africa: a review. Transfus Med. 2010;20:1–10. doi: 10.1111/j.1365-3148.2009.00958.x. [DOI] [PubMed] [Google Scholar]
- 21.Club 25. Club 25 International: How it Works, <http://club25online.org/static/page/id/howitworks>; 2015 [accessed 3 February, 2015].
- 22.Club 25. Club 25 International: About-Why, What, How, <http://club25online.org/static/page/id/about>; 2015 [accessed 3 February, 2015].
- 23.Bednall T.C., Bove L.L. Donating blood: a meta-analytic review of self-reported motivators and deterrents. Transfus Med Rev. 2011;25:317–334. doi: 10.1016/j.tmrv.2011.04.005. [DOI] [PubMed] [Google Scholar]
- 24.Alinon K., Gbati K., Sorum P.C. Emotional-motivational barriers to blood donation among Togolese adults: a structural approach. Transfus Med. 2013 doi: 10.1111/tme.12082. [DOI] [PubMed] [Google Scholar]
- 25.Duboz P., Macia E., Cuneo B. Sociodemographic and attitudinal factors to blood donation in the urban population of Dakar, Senegal. Transfusion. 2010;50:2713–2720. doi: 10.1111/j.1537-2995.2010.02750.x. [DOI] [PubMed] [Google Scholar]
- 26.Koster J., Hassall O.W. Attitudes towards blood donation and transfusion in Bamenda, Republic of Cameroon. Transfus Med. 2011;21:301–307. doi: 10.1111/j.1365-3148.2011.01079.x. [DOI] [PubMed] [Google Scholar]
- 27.Mwaba K., Keikelame M.J. Blood donation behaviour and beliefs among a sample of high school students in Mmabatho. Curationis. 1995;18:2–3. doi: 10.4102/curationis.v18i3.1356. [DOI] [PubMed] [Google Scholar]
- 28.Neema S., Ahmed F.H., Onuh S.O. Socio-cultural barriers to voluntary blood donation for obstetric use in a rural Nigerian village. Afr J Reprod Health. 2005;9:72–76. [PubMed] [Google Scholar]
- 29.Nwogoh B., Aigberadion U., Nwannadi A.I. Knowledge, attitude, and practice of voluntary blood donation among healthcare workers at the University of Benin Teaching Hospital, Benin City, Nigeria. J Blood Transfus. 2013;2013:797830. doi: 10.1155/2013/797830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Obi S.N. Antenatal blood donation for pregnant Nigerian mothers: the husbands’ perspective. J Obstet Gynaecol. 2007;27:467–469. doi: 10.1080/01443610701405986. [DOI] [PubMed] [Google Scholar]
- 31.Olaiya M.A., Alakija W., Ajala A. Knowledge, attitudes, beliefs and motivations towards blood donations among blood donors in Lagos, Nigeria. Transfus Med. 2004;14:13–17. doi: 10.1111/j.0958-7578.2004.00474.x. [DOI] [PubMed] [Google Scholar]
- 32.Salaudeen A.G., Odeh E. Knowledge and behaviour towards voluntary blood donation among students of a tertiary institution in Nigeria. Niger J Clin Pract. 2011;14:303–307. doi: 10.4103/1119-3077.86773. [DOI] [PubMed] [Google Scholar]
- 33.Salaudeen A.G., Musa O.I., Awoyemi A.O. Community survey on blood donation practices in a northern state of Nigeria. J Prev Med Hyg. 2011;52:21–25. [PubMed] [Google Scholar]
- 34.Nebie K.Y., Olinger C.M., Kafando E. Lack of knowledge among blood donors in Burkina Faso (West Africa); potential obstacle to transfusion security. Transfus Clin Biol. 2007;14:446–452. doi: 10.1016/j.tracli.2007.12.005. [DOI] [PubMed] [Google Scholar]
- 35.Jacobs B., Berege Z.A. Attitudes and beliefs about blood donation among adults in Mwanza region, Tanzania. East Afr Med J. 1995;72:345–348. [PubMed] [Google Scholar]
- 36.Oyarebu K.A. A survey in Benin City, Nigeria. Attitude to blood donation and blood transfusion. Hygie. 1982;1:17–20. [PubMed] [Google Scholar]
- 37.Okpara R.A. Attitudes of Nigerians towards blood donation and blood transfusion. Trop Geogr Med. 1989;41:89–93. [PubMed] [Google Scholar]
- 38.Asenso-Mensah K., Achina G., Appiah R. Can family or replacement blood donors become regular volunteer donors? Transfusion. 2014;54:797–804. doi: 10.1111/trf.12216. [DOI] [PubMed] [Google Scholar]
- 39.Gardner J.W., Sanborn J.S. Years of potential life lost (YPLL)–what does it measure? Epidemiology. 1990;1:322–329. doi: 10.1097/00001648-199007000-00012. [DOI] [PubMed] [Google Scholar]
- 40.World Health Organization. World blood donor day: Safe blood for saving mothers, <http://www.who.int/campaigns/world-blood-donor-day/2014/event/en/> 2014 [accessed 17 February, 2014].
- 41.Centers for Disease C, Prevention Progress toward strengthening national blood transfusion services-14 countries, 2008–2010. MMWR Morb Mortal Wkly Rep. 2011;60:1577–1582. [PubMed] [Google Scholar]
- 42.World Health Organization. Regional office for Africa, <http://www.who.int/about/regions/afro/en/>; 2015 [accessed 3 March, 2015].