Abstract
Objective:
Characterization of the severity of injury should account for both mortality and disability. The objective of this study was to develop a disability metric for thoracic injuries in motor vehicle crashes (MVCs), and compare the functional outcomes between the pediatric and adult populations.
Methods:
Disability risk (DR) was quantified using Functional Independence Measure (FIM) scores within the National Trauma Data Bank for the most frequently occurring Abbreviated Injury Scale (AIS) 2–5 thoracic injuries. Occupants with thoracic injury were classified as disabled or not disabled based on the FIM scale, and comparisons were made between the following age groups: pediatric, adult, middle-aged, and older occupants (ages 7–18, 19–45, 46–65, and 66+, respectively). For each age group, DR was calculated by dividing the number of patients who were disabled that sustained a given injury by the number of patients who sustained a given injury. To account for the effect of higher severity co-injuries, a maximum AIS adjusted DR (DRMAIS) was also calculated for each injury. DR and DRMAIS could range from 0 to 100% disability risk.
Results:
The mean DRMAIS for MVC thoracic injuries was 20% for pediatric occupants, 22% for adults, 29% for middle-aged adults, and 43% for older adults. Older adults possessed higher DRMAIS values for diaphragm laceration/rupture, heart laceration, hemo/pneumothorax, lung contusion/laceration, and rib and sternum fracture compared to the other age groups. The pediatric population possessed a higher DRMAIS value for flail chest compared to the other age groups.
Conclusion:
Older adults had significantly greater overall disability than each of the other age groups for thoracic injuries. The developed disability metrics are important in quantifying the significant burden of injuries and loss of quality life years. Such metrics can be used to better characterize severity of injury and further the understanding of age-related differences in injury outcomes, which can influence future age-specific modifications to AIS.
Keywords: disability, functional outcome, motor vehicle crash, thoracic injuries, pediatric trauma, elderly
INTRODUCTION
Thoracic injuries rank second only to head injuries in terms of the number of fatalities and serious injuries in United States motor vehicle crashes (MVCs) (Cavanaugh, 2002). For these thoracic injuries, there are differences in age-related injury risk. Occupants aged 40–64 and 65+ years are at a greater risk of sustaining a Maximum Abbreviated Injury Scale (MAIS) 3+ thoracic injury in comparison to 13–39 year old occupants in frontal MVCs (Morris, et al., 2003). The majority of the thoracic injuries in these frontal crashes result from restraint systems and a small proportion are caused by other interior vehicle components (Morris, et al., 2003). In addition to differences in injury risk, there are also age-related differences in mortality risk for thoracic injuries. Adults over the age of 18 had significantly greater mortality risk from thoracic injury compared to pediatric occupants aged 5–14 years old (Doud, et al., 2015). Although mortality risk is a useful measure for threat to life, it does not accurately capture the significant burden of injury or the severity of non-fatal injuries. This is especially critical for pediatric patients where mortality rates tend to be very low and loss of quality life years has the potential to be very high (Doud, et al., 2015).
To supplement data on mortality rates, studies have examined the societal effect of injuries including disability and functional life-years lost to injury (Kuppa, et al., 2001; Schoell, et al., 2016). Schoell et al. developed a metric quantifying the disability of specific injuries using Functional Independence Measure (FIM) scores within the National Trauma Data Bank-Research Data Set (NTDB-RDS). Disability was quantified for the top 95% most frequently occurring MVC injuries of severity 3, 4, and 5 on the Abbreviated Injury Scale (AIS) (Schoell, et al., 2016). Pairwise comparisons demonstrated that older adults (ages 66+) had significantly greater overall disability than pediatric, adult, and middle-aged occupants (ages 7–18, 19–45, and 46–65, respectively). This paper focused on head injuries and the higher disability risks and implications of such injuries on functional outcomes.
Since MVC-induced incidence, morbidity, and mortality of thoracic injuries increases with age, it is important to understand the disability of these injuries across different age groups. Changes due to development and aging can affect injury patterns and tolerances as well as the overall morbidity and mortality, especially for the thorax. For pediatric occupants, the relative compliance of the thoracic wall allows for increased risk of internal thoracic organ injury without necessarily inducing rib fractures (Eichelberger, 1993; Huelke, 1998). With aging, there is a decrease in skeletal and physiological resilience due to structural and material changes in the thorax (Burstein, et al., 1976; Schoell, et al., 2015; Zioupos, et al., 1998). In the elderly, thoracic injury tolerance has been shown to decrease by 20% for blunt loading and up to 70% for belt-loading (Zhou, et al., 1996). For the previously developed disability metric, the disability risk ranged from 0 to 90% disability for AIS 3, 4, and 5 thoracic injuries across the pediatric and adult age groups (Schoell, et al., 2016). The objective of this study was to further explore the disability metric for thoracic injuries by developing the disability metric for AIS 2, 3, 4, and 5 thoracic injuries and comparing the functional outcomes between the pediatric and adult populations.
METHODS
Top 95% AIS 2, 3, 4, and 5 NASS-CDS Injuries
The top 95% most frequently occurring AIS 2, 3, 4, and 5 thoracic injuries in MVCs were identified using the 2000–2011 National Automotive Sampling System–Crashworthiness Data System (NASS-CDS) (National Highway Traffic Safety Administration, 2011). Moderate to critical thoracic injuries designated as AIS 2, 3, 4, and 5 injuries were selected as the primary focus of the study (AAAM, 2001). Differing from the previous disability metric study (Schoell, et al., 2016), AIS 2 injuries were added to the analysis to incorporate moderate rib and sternum fractures. Minor AIS 1 injuries are less likely to result in diminished functional outcomes and the most severe AIS 6 injuries are less survivable and less relevant to outcome studies involving morbidity. MVC occupants were grouped into four age groups: pediatric, adult, middle-aged, and older adult (ages 7–18, 19–45, 46–65, and 66+, respectively). For pediatric occupants, the top 95% most frequently occurring AIS 2–5 thoracic injuries consisted of a list of 18 unique AIS codes. For the stratified adult age groups, the top 95% most frequently occurring AIS 2–5 thoracic injuries consisted of a list of 32 unique AIS codes.
Disability Risk (DR)
Disability risk (DR) was calculated using the largest aggregation of trauma registry data, the NTDB-RDS version 7.1 years 2002–2006, as described in the previous study (American College of Surgeons, 2007; Schoell, et al., 2016). The NTDB is the largest aggregation of trauma registry data ever assembled. Data are collected from participating trauma centers on an annual basis and rigorously examined by NTDB administrators. MVC cases in NTDB were identified using the International Classification of Diseases version 9 injury coding lexicon (ICD-9). Codes exist for over 10,000 medical conditions, about 2,000 of which are physical injuries. ICD-9 codes from 800.0 to 959.9 encompasses all traumatic injuries. External cause of injury codes 810–819 correspond to MVC cases. A post-dot of 0 or 1 designates injury to the driver or passenger of the motor vehicle. As described, the MVC cases were selected from the NTDB and an AIS-98 to ICD-9 mapping approach was used to match each of the ICD-9 injury codes from the patient with its corresponding AIS code (Barnard, et al., 2013). FIM scores, which measure the level of disability and amount of assistance required to carry out daily living activities, were used to calculate DR (Uniform Data System for Medical Rehabilitation, 2007). The FIM instrument has been validated for use in children 7 years and older (Aitken, et al., 1999; Arthurs, et al., 2009; Winthrop, et al., 2005). The FIM instrument, which is collected at discharge, is composed of items that measure physical and cognitive function based on direct observation by a clinician. Physical function consists of items including aspects of self-care, sphincter control, and mobility. Cognitive function consists of items including aspects of communication and social cognition. The FIM instrument has been shown to be an internally consistent functional status measure (Stineman, et al., 1996). The FIM instrument in the NTDB-RDS contains a validated truncated form of the measure with three items evaluating the areas of self-feed, locomotion, and verbal expression. Each of the three items is graded on a scale of 1 to 4, with 1 indicating full functional dependence and 4 indicating full functional independence (Arthurs, et al., 2009; Brown, et al., 2010; Haider, et al., 2009; Haider, et al., 2011; Martin, et al., 2005; Martin, et al., 2005; Ottenbacher, et al., 1996; Spaniolas, et al., 2008). Patients in each of the four age groups were classified as disabled if any of the self-feed, locomotion, or verbal expression items possessed a FIM score of 1 or 2, indicating full functional or modified dependence.
Within each age group, for each of the top 95% most frequently occurring AIS 2, 3, 4, and 5 MVC thoracic injuries, the DR was calculated by dividing the number of disabled patients who sustained a specific injury by the number of patients who sustained the specific injury (Eq. (1)).
| (1) |
To account for the effect of higher severity co-injuries, an MAIS-adjusted DR (DRMAIS) was also calculated for each injury. The calculation of the DRMAIS for each injury includes only occupants with an MAIS equal to the AIS severity of the given injury (Eq. (2)). For example, if the given injury was an AIS 2, then occupants with AIS 3+ injuries would be excluded from the calculation. DR and DRMAIS for each injury within each age group resulted in possible values ranging from 0 to 1 corresponding to 0–100% disability risk.
| (2) |
DR and DRMAIS values for injuries on each of the respective top 95% lists were compared across the four age groups. One-way analysis of variance was used to examine group differences between age groups. Pairwise comparisons were also evaluated, using a conservative Bonferroni adjustment to account for multiple comparisons. All statistical analyses were performed using SAS 9.4 (SAS Institute, Cary, NC) and JMP Pro 12.0 (SAS Institute, Cary, NC). A p-value less than 0.05 was considered statistically significant.
RESULTS
Disability Risk (DR) Sample Sizes
A summary of the sample sizes and population statistics used in the calculation of the DR can be found in Table 1. The sample sizes of occupants who were 7 years and older, alive at discharge, possessed an AIS 2, 3, 4, or 5 thoracic injury on the top 95% lists, and had a FIM score available included 7,135 pediatric, 19,298 adult, 21,801 middle-aged adult, and 7,903 older adult occupants. Classification of disability using the FIM scores determined that 27% of pediatric occupants (1,918 occupants), 25% of adults (4,760 occupants), 26% of middle-aged adults (5,623 occupants), and 39% of older adults (3,074 occupants) were disabled. The most frequently occurring type of disability based on the FIM component cited for each age group was locomotion alone followed by the combination of self-feeding, locomotion, and expression. Excluding patients with lower extremity and spinal injuries, the combination of self-feeding, locomotion, and expression was most prevalent within pediatric occupants and locomotion alone was still the most common disability for adults, middle-aged adults, and older adults. For this sample, the average and standard deviation of the number of injuries sustained was 7.2 ± 4.2 for pediatric occupants, 7.1 ± 4.2 for adult occupants, 6.5 ± 4.1 for middle-aged adult occupants, and 5.6 ± 3.6 for older adult occupants. The average Injury Severity Score (ISS) and standard deviation for each age group was 22.7 ± 12.7 for pediatric occupants, 21.7 ± 12.6 for adult occupants, 18.8 ± 11.6 for middle-aged adult occupants, and 16.9 ± 10.8 for older adult occupants.
Table 1.
Sample sizes and population statistics used in calculation of the disability risk (DR) and MAIS-adjusted disability risk (DRMAIS). The FIM column indicates the number of patients who had a FIM score available. The Disabled column indicates the number of patients and percentage of patients who were classified as disabled. The Injuries column designates the average number and standard deviation of injuries that the patients sustained. The ISS column designates the average ISS and standard deviation of the patients.
| Age Group | DR | DRMAIS | ||||||
|---|---|---|---|---|---|---|---|---|
| FIM n | Disabled n, % | Injuries Mean± SD | ISS Mean± SD | FIM n | Disabled n, % | Injuries Mean± SD | ISS Mean± SD | |
| Pediatric (7–18 YO) | 7,135 | 1,918 (27%) | 7.2 ± 4.2 | 22.7 ± 12.7 | 5,425 | 1,060 (20%) | 6.8 ± 4.0 | 19.7 ± 10.4 |
| Adult (19–45 YO) | 19,298 | 4,760 (25%) | 7.1 ± 4.2 | 21.7 ± 12.6 | 15,335 | 2,979 (19%) | 6.8 ± 4.0 | 19.5 ± 10.9 |
| Middle-Aged (46–65 YO) | 21,801 | 5,623 (26%) | 6.5 ± 4.1 | 18.8 ± 11.6 | 18,106 | 4,051 (22%) | 6.2 ± 4.0 | 17.5 ± 10.6 |
| Older Adult (66+ YO) | 7,903 | 3,074 (39%) | 5.6 ± 3.6 | 16.9 ± 10.8 | 6,684 | 2,437 (36%) | 5.3 ± 3.5 | 15.8 ± 10.2 |
Adjusted Disability Risk (DRMAIS) Sample Sizes
A summary of the sample sizes and population statistics used in the calculation of the DRMAIS can be found in Table 1. The sample sizes of occupants who were 7 years and older, alive at discharge, possessed an AIS 2, 3, 4, or 5 thoracic injury on the top 95% lists, had a FIM score available, and were included in the DRMAIS calculation included 5,425 pediatric, 15,335 adult, 18,106 middle-aged adult, and 6,684 older adult occupants. Classification of disability using the FIM scores determined that 20% of pediatric occupants (1,060 occupants), 19% of adults (2,979 occupants), 22% of middle-aged adults (4,051 occupants), and 36% of older adults (2,437 occupants) were disabled. Similar to the patients in the DR calculation, the most frequently occurring type of disability based on the FIM component cited for each age group was locomotion alone followed by the combination of self-feeding, locomotion, and expression. Excluding patients with lower extremity and spinal injuries, locomotion alone was the most cited disability for all age groups. For this sample, the average number of injuries including the standard deviation sustained was 6.8 ± 4.0 for pediatric occupants, 6.8 ± 4.0 for adult occupants, 6.2 ± 4.0 for middle-aged adult occupants, and 5.3 ± 3.5 for older adult occupants. The average ISS and standard deviation for each age group was 19.7 ± 10.4 for pediatric occupants, 19.5 ± 10.9 for adult occupants, 17.5 ± 10.6 for middle-aged adult occupants, and 15.8 ± 10.2 for older adult occupants.
DR and DRMAIS by Age Group
The DR and DRMAIS for the AIS 2–5 thoracic injuries ranged from 0 to 0.9 (0–90% disability risk). The mean, standard deviation, and median DR and DRMAIS values with interquartile ranges for the AIS 2, 3, 4, and 5 thoracic injuries on the top 95% lists for each age group are reported in Table 2. The sample sizes used in the calculation for both DR and DRMAIS for each age group can be found in Table A1. For the DR values, pairwise comparisons demonstrated that older adults had significantly greater overall disability than each of the other age groups: older adult (50.0 ± 15.4%) vs. pediatric (29.0 ± 13.7%), adult (30.9 ± 9.1%), and middle aged (34.7 ± 13.1%); all p<0.0001. The DR values ranged from 12.5% to 70% for pediatric occupants, 20% to 53% for adults, 0% to 67% for middle-aged adults, and 0% to 90% for older adults. For the DRMAIS values, pairwise comparisons also demonstrated that older adults had significantly greater DRMAIS values than each of the other age groups: older adult (42.9 ± 19.5%) vs. pediatric (19.6 ± 15.8%), adult (22.4 ± 12.5%), and middle aged (28.6 ± 15.7%); all p <0.01. The DRMAIS values ranged from 0% to 64% for pediatric occupants, 0% to 48% for adults, 0% to 64% for middle-aged adults, and 0% to 90% for older adults.
Table 2.
Mean, standard deviation, and median disability risk (DR) and MAIS-adjusted disability risk (DRMAIS) with interquartile ranges (IQR) for the top 95% AIS 2, 3, 4, and 5 thoracic injuries in each age group. Values are expressed as percentages.
| Age Group | DR (%) | DRMAIS (%) | ||||||
|---|---|---|---|---|---|---|---|---|
| Mean | Std Dev. | Median | IQR | Mean | Std Dev. | Median | IQR | |
| Pediatric (7–18 YO) | 29.0 | 13.7 | 26.6 | 20.1–35.2 | 19.6 | 15.8 | 16.7 | 10.8–27.0 |
| Adult (19–45 YO) | 30.9 | 9.1 | 29.2 | 23.5–36.8 | 22.4 | 12.5 | 20.6 | 13.8–29.7 |
| Middle-Aged (46–65 YO) | 34.7 | 13.1 | 32.8 | 25.4–41.0 | 28.6 | 15.7 | 27.8 | 19.4–36.1 |
| Older Adult (66+ YO) | 50.0 | 15.4 | 50.0 | 40.3–60.8 | 42.9 | 19.5 | 44.4 | 27.4–58.9 |
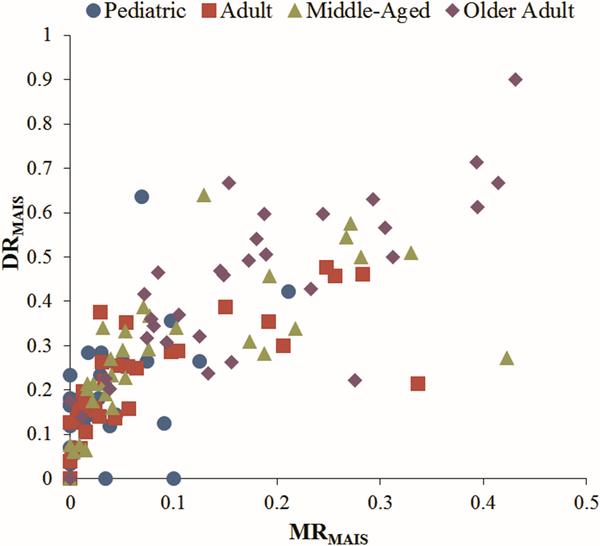
DRMAIS Correlation with MRMAIS
Further analysis was performed using the DRMAIS metric as it is a better estimate of the disability of an individual injury since it excludes the influence of occupants with higher severity co-injuries from the calculation. For pediatric and adult occupants, the DRMAIS for each injury was compared to its corresponding MAIS-adjusted mortality risk (MRMAIS) (Figure 1) (Doud, et al., 2015; Weaver, et al., 2013). The thoracic injuries across all the age groups had mortality risks below 50%, however, the associated disability risk ranged upwards to 90%. For low MRMAIS values (0 – 5%), there were large variations in DRMAIS with some injuries having high disability risks (0 – 38%). Linear regression models were fit to the data with R2 values of 0.239 for pediatric patients, 0.509 for adults, 0.445 for middle-aged adults, and 0.635 for older adults.
Figure 1.
MAIS-adjusted disability risk (DRMAIS) vs MAIS-adjusted mortality risk (MRMAIS) for the top 95% list AIS 2, 3, 4, and 5 thoracic injuries by age group
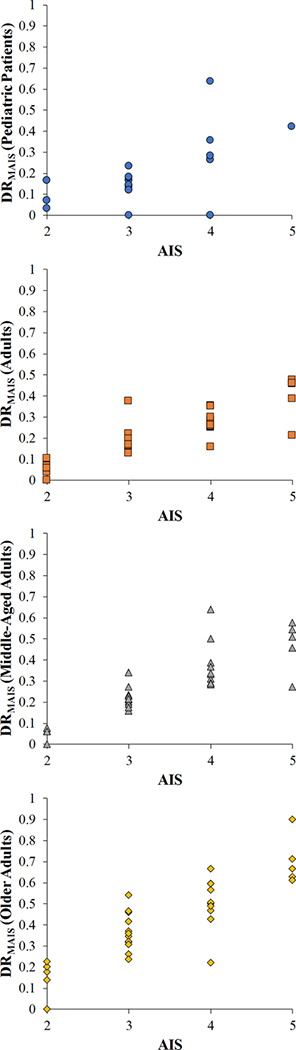
DRMAIS Correlation with AIS
The DRMAIS for each injury was compared to its corresponding AIS severity for each age group (Figure 2). Trends indicate increasing DRMAIS for increasing AIS severity for each of the age groups. However, within each AIS severity level, there is variation in the DRMAIS. For pediatric occupants, AIS 4 injuries possess DRMAIS values ranging from 0 to 64%. For adults, AIS 4 injuries possess DRMAIS values ranging from 16% to 35%. For middle-aged adults, AIS 4 injuries possess DRMAIS values ranging from 28% to 64%. For older adults, AIS 4 injuries possess DRMAIS values ranging from 22% to 67%. The ranges in disability within each AIS severity level were the largest within the older adults. Across different AIS severity levels, there are injuries with similar DRMAIS values. As such, the ranges overlap between AIS severity levels. Overall, the comparison of DRMAIS and AIS highlights the differences in the metrics and the ability to supplement one another to better characterize the severity of injury.
Figure 2.
MAIS-adjusted disability risk (DRMAIS) vs AIS severity for the top 95% list AIS 2, 3, 4, and 5 thoracic injuries by age group.
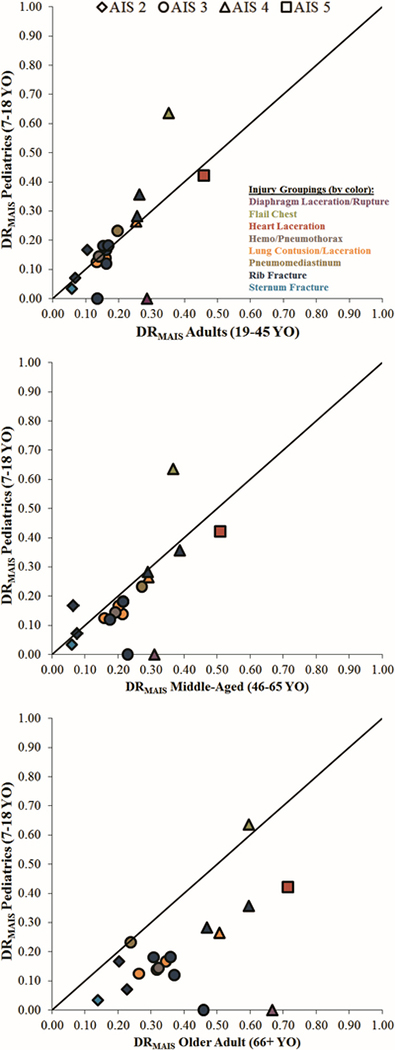
DRMAIS for Individual Thoracic Injuries by Age Group
To compare the differences in disability for individual thoracic injuries between the pediatric cohort and the stratified adult groups, the DRMAIS for each thoracic injury in the pediatric group is plotted for the same injury in each adult age group (Figure 3). Injuries appearing above the equivalency line demonstrate a greater DRMAIS for pediatric patients than for the given adult age group. Comparing pediatric patients with the adult group, the disability values across each of the AIS severity values were very similar, as the majority of injuries fell along the equivalency line. This pattern shifted when comparing the pediatric patients to the middle-aged adult group. The middle-aged adult group tended to have higher DRMAIS values across each of the AIS severity values. In comparing the older adult group and pediatric patients, the older adult group tended to have much higher DRMAIS values for each AIS severity value.
Figure 3.
DRMAIS for AIS 2, 3, 4, and 5 thoracic injuries for pediatric patients versus adults (top), middle-aged (middle), and older adults (bottom). DRMAIS for each injury in the pediatric group is plotted against the DRMAIS of that injury for the adult age groups. Injuries are categorized by AIS severity as noted in the legend. Injuries are also categorized by injury groupings as designated by color of marker. Injuries appearing above the equivalency line demonstrate a greater DRMAIS for pediatric patients than for the given adult age group.
DRMAIS for Grouped Thoracic Injuries by Age Group
Due to the large variations in the DRMAIS as well as small sample sizes on an individual injury level basis, further analysis was conducted by grouping the thoracic injuries into eight groups based on the structure of injury and injury type. Across the four age groups, there were 32 unique AIS thorax injury codes present. The eight injury groups included diaphragm laceration/rupture, flail chest, heart laceration, hemo/pneumothorax, lung contusion/laceration, pneumomediastinum, rib fracture, and sternum fracture. The DRMAIS was calculated for each injury group by age group (Table 3). Sample sizes for the calculation can also be found in Table 3. Older adults possessed higher DRMAIS values for diaphragm laceration/rupture, heart laceration, hemo/pneumothorax, lung contusion/laceration, rib fracture, and sternum fracture compared to the other age groups. The pediatric population possessed a higher DRMAIS value for flail chest compared to the other age groups. Middle-aged adults possessed a higher DRMAIS value for pneumomediastinum compared to the other age groups. For each individual thoracic injury plotted in Figure 3, the corresponding injury grouping is given in color to delineate the differences between the pediatric cohort and stratified adult groups.
Table 3.
Sample sizes and DRMAIS values for injury groupings for thoracic injuries by age group (I=Total Injured and D= Total Disabled). Values are expressed as percentages.
| Injury Grouping | Pediatric | Adult | Middle-Aged | Older Adult | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| I | D | DRMAIS (%) | I | D | DRMAIS (%) | I | D | DRMAIS (%) | I | D | DRMAIS (%) | |
| Diaphragm Laceration/Rupture | 6 | 0 | 0.0 | 99 | 34 | 34.3 | 117 | 39 | 33.3 | 49 | 28 | 57.1 |
| Flail Chest | 22 | 14 | 63.6 | 252 | 91 | 36.1 | 763 | 298 | 39.1 | 274 | 163 | 59.5 |
| Heart Laceration | 45 | 19 | 42.2 | 301 | 115 | 38.2 | 274 | 130 | 47.4 | 95 | 55 | 57.9 |
| Hemo/ Pneumothorax | 938 | 135 | 14.4 | 2281 | 322 | 14.1 | 2035 | 390 | 19.2 | 593 | 191 | 32.2 |
| Lung Contusion/Laceration | 3215 | 600 | 18.7 | 7708 | 1454 | 18.9 | 5930 | 1350 | 22.8 | 1618 | 596 | 36.8 |
| Pneumomediastinum | 30 | 7 | 23.3 | 76 | 15 | 19.7 | 81 | 22 | 27.2 | 21 | 5 | 23.8 |
| Rib Fracture | 2063 | 492 | 23.8 | 7416 | 1593 | 21.5 | 11976 | 2842 | 23.7 | 4788 | 1904 | 39.8 |
| Sternum Fracture | 59 | 2 | 3.4 | 292 | 17 | 5.8 | 929 | 56 | 6.0 | 598 | 83 | 13.9 |
DISCUSSION
MVC-induced thoracic injuries can result in varying levels of mortality and morbidity depending on the age of the occupant. Supplementation of mortality and AIS severity information with information regarding disability and functional outcomes can better characterize the severity of injuries especially for injuries with low mortality rates. In this study, a disability metric was quantified for the most frequently occurring AIS 2, 3, 4, and 5 MVC-induced thoracic injuries across the pediatric, adult, middle-aged adult, and older adult populations using FIM scores from the NTDB-RDS. Overall for both DR and DRMAIS, older adults had significantly higher disability risks from thoracic injury in comparison to pediatric patients, adults, and middle-aged adults. Further analysis of disability and comparison of functional outcomes across the different age groups was conducted using the DRMAIS metric as it provides a better estimate of the disability of an individual injury. Since most trauma patients sustain multiple injuries, the calculation of DR for lower severity injuries might be overestimated due to higher severity co-injuries. For example, the DR values for an AIS 450804.2 sternum fracture were 21%, 23%, 24%, and 32% for pediatric, adult, middle-aged, and older adult occupants, respectively. These AIS 2 sternum fractures are often accompanied by AIS 3+ injuries including rib fractures and hemo/pneumothorax injuries. By excluding such higher severity injuries, the DRMAIS calculation for this sternum fracture results in values of 3%, 6%, 6%, and 14% for pediatric, adult, middle-aged, and older occupants, respectively. Calculation of the true disability of an individual injury would require patients who sustained that injury in isolation. The number of occupants within an age group that sustained an isolated thoracic injury is zero for 25% of the injuries and less than 10 for 69% of the injuries. Since the sample sizes of occupants with isolated thoracic injuries are small, the calculation of DRMAIS provides the best estimation of disability, especially for multi-injured trauma patients.
Differences in disability, mortality, and AIS severity were observed in comparison to the DRMAIS metric. For both pediatric and adult occupants, there was wide variability in associated disability for injuries with low mortality and varying AIS severity. This observation highlights the ability of disability risk metrics to describe more information regarding injury severity, especially for injuries with low mortality risks. Such information could be used in the future to inform updates for age-specific modifications to AIS as age-related differences in injury outcomes are apparent.
To delineate the differences in disability for individual thoracic injuries across age groups, the pediatric cohort was compared to each stratified adult age group. The disability risks across each AIS severity between the pediatric cohort and adult occupants were very similar. Middle-aged adults tended to have higher disability across each AIS severity in comparison to the pediatric occupants. When compared to the pediatric cohort, older adults tended to have much higher disability across the majority of injuries for each AIS severity. An interesting injury comparison included an AIS 4 rib cage flail chest injury with lung contusion which resulted in 64% disability for pediatric occupants in comparison to adults (35%), middle-aged adults (37%), and older adults (60%). Clinically, pediatric occupants often sustain lung injuries without the presence of rib fractures while adults almost always sustain lung injuries in conjunction with rib fractures. When rib fractures are present in pediatric occupants, this often indicates severe trauma and thus can result in more debilitating outcomes as indicated by the higher disability risk (Garcia, et al., 1990; Holmes, et al., 2002).
Individual thoracic injuries were grouped into eight groups based on structure of injury and injury type to increase sample sizes and highlight differences across general injury groups. Overall, older adults had higher associated disability for the majority of the injury groups with pediatric patients having higher associated disability for flail chest injuries and with middle-aged adults having higher associated disability for pneumomediastinum injuries. With rib fractures being the most frequent AIS 3+ chest injury in MVCs and the decrease in injury tolerance due to structural and material changes with age, older adults exhibiting higher disability risk falls in line with the given trends (Kent, et al., 2005; Leport, et al., 2011). Rib fractures can also result in hemothorax, pneumothorax, and lung contusions and can lead to further disability. Blunt thoracic aortic injuries, while not heavily prevalent, have been shown to lead to high rates of morbidity and mortality due to the inability of patients to undergo aortic repair (Arthurs, et al., 2009). Similar to the findings in this study, the most prevalent disability associated with patients with blunt thoracic aortic injuries was locomotion.
There are several limitations. The NTDB-RDS is not a population sample as it is skewed toward more severely injured patients from trauma centers. Since NTDB-RDS is a large national database, this type of retrospective review of a convenience sample introduces such bias. This database was selected for the large sample size of MVC occupants as well as the ability to characterize disability using the FIM instrument. Another important limitation involves pre-injury health status and pre-existing comorbidities which were not considered in these analyses. Such information would have an effect especially on older occupants and disability. Future work includes examining such conditions and adjusting the calculation of disability for these potential confounders. For this analysis, there were small sample sizes on an individual injury basis for a given age group. To combat these sample sizes, the analysis was focused on the most frequently occurring AIS 2, 3, 4, and 5 thoracic injuries, and subsequent analyses grouped similar injuries into major injury groups. Some injuries or injury groups still resulted in small sample sizes, which indicate that these injuries might be infrequent, even in NTDB-RDS, which is the largest aggregation of trauma registry data. In calculating the DR and DRMAIS, there is potential for a floor and ceiling effect. Overall, there were very few injuries with 0% disability and no injuries with 100% disability; thus, the normal approximation to the binomial—and subsequent one-way analysis of variance—is appropriate for analyses. Furthermore, we performed a sensitivity analysis in which we perturbed the data at the tails of the distribution resulting in a normal distribution that extended beyond 0, and all significance levels and conclusions remained.
In conclusion, a disability-based metric was computed for the most frequently occurring MVC-induced thoracic injuries for different age groups. Similar to varying levels of incidence and mortality associated with thoracic injuries, there were age-related differences in disability risk and injury outcomes. Overall, for thoracic injuries, older adults had significant greater overall disability than each of the other age groups. These differences across age groups highlight the effects of development and aging on the risk of morbidity. Supplemented with AIS severity and mortality risk, this information can lead to a better characterization of the severity of injury and better capture the significant burden of non-fatal injuries. The characterization of injury severity by age can help further the understanding of age-related differences in injury outcomes, which can affect future age-specific modifications to AIS.
Supplementary Material
ACKNOWLEDGEMENTS
The authors would like to acknowledge the National Science Foundation (NSF) Center for Child Injury Prevention Studies at the Children’s Hospital of Philadelphia (CHOP) for sponsoring this study and its Industry Advisory Board (IAB) members for their support, valuable input and advice. This publication was also supported by the National Institutes of Health (NIH), Eunice Kennedy Shriver National Institute of Child Health and Human Development, grant K08HD073241. The views presented are those of the authors and not necessarily the views of CHOP, the NSF, the IAB members, or the NIH.
NTDB data was provided by the Committee on Trauma, American College of Surgeons (ACS). NTDB Version 7.1 Chicago, IL, 2007. The content reproduced from the NTDB remains the full and exclusive copyrighted property of the American College of Surgeons. ACS is not responsible for any claims arising from works based on the original data, text, tables, or figures.
REFERENCES
- 1.AAAM. The Abbreviated Injury Scale. 2001;1990 Revision, Update 98.
- 2.Aitken ME, Jaffe KM, DiScala C, Rivara FP. Functional outcome in children with multiple trauma without significant head injury. Arch Phys Med Rehabil. 1999;80(8):889–895. [DOI] [PubMed] [Google Scholar]
- 3.American College of Surgeons. National Trauma Data Bank - Research Data System. Vol RDS 7.1. Chicago, IL: American College of Surgeons Committee on Trauma; 2007. [Google Scholar]
- 4.Arthurs ZM, Starnes BW, Sohn VY, Singh N, Martin MJ, Andersen CA. Functional and survival outcomes in traumatic blunt thoracic aortic injuries: an analysis of the National Trauma Databank. J Vasc Surg. 2009;49(4):988–994. [DOI] [PubMed] [Google Scholar]
- 5.Barnard RT, Loftis KL, Martin RS, Stitzel JD. Development of a robust mapping between AIS 2+ and ICD-9 injury codes. Accid Anal Prev. March 2013;52:133–143. [DOI] [PubMed] [Google Scholar]
- 6.Brown JB, Stassen NA, Cheng JD, Sangosanya AT, Bankey PE, Gestring ML. Trauma center designation correlates with functional independence after severe but not moderate traumatic brain injury. J Trauma Acute Care Surg. 2010;69(2):263–269. [DOI] [PubMed] [Google Scholar]
- 7.Burstein AH, Reilly DT, Martens M. Aging of bone tissue: mechanical properties. J Bone Joint Surg Am. 1976;58(1):82–86. [PubMed] [Google Scholar]
- 8.Cavanaugh JM. Biomechanics of Thoracic Trauma Accidental Injury: Springer; 2002:374–404. [Google Scholar]
- 9.Doud AN, Weaver AA, Talton JW, et al. Mortality risk in pediatric motor vehicle crash occupants: accounting for developmental stage and challenging Abbreviated Injury Scale metrics. Traffic Inj Prev. 2015;16(sup2):S201–S208. [DOI] [PubMed] [Google Scholar]
- 10.Eichelberger M Pediatric Trauma: prevention, acute care, rehabilitation: Pmph Bc Decker; 1993. [Google Scholar]
- 11.Garcia VF, Gotschall CS, Eichelberger MR, Bowman LM. Rib fractures in children: a marker of severe trauma. J Trauma Acute Care Surg. 1990;30(6):695–700. [PubMed] [Google Scholar]
- 12.Haider AH, Chang DC, Haut ER, Cornwell EE, Efron DT. Mechanism of injury predicts patient mortality and impairment after blunt trauma. J Surg Res. 2009;153(1):138–142. [DOI] [PubMed] [Google Scholar]
- 13.Haider AH, Crompton JG, Oyetunji T, et al. Mechanism of injury predicts case fatality and functional outcomes in pediatric trauma patients: the case for its use in trauma outcomes studies. J Pediatr Surg. 2011;46(8):1557–1563. [DOI] [PubMed] [Google Scholar]
- 14.Holmes JF, Sokolove PE, Brant WE, Kuppermann N. A clinical decision rule for identifying children with thoracic injuries after blunt torso trauma. Ann Emerg Med. 2002;39(5):492–499. [DOI] [PubMed] [Google Scholar]
- 15.Huelke DF. An overview of anatomical considerations of infants and children in the adult world of automobile safety design. Annu Proc Assoc Adv Automot Med. 1998;42:93–113. [Google Scholar]
- 16.Kent R, Sang-Hyun L, Darvish K, Wang S. Structural and material changes in the aging thorax and their role in crash protection for older occupants. Stapp Car Crash J. 2005;49:231. [DOI] [PubMed] [Google Scholar]
- 17.Kuppa S, Wang J, Haffner M, Eppinger R. Lower Extremity Injuries and Associated Injury Criteria. In: National Highway Traffic Safety Administration, ed. 17th International Technical Conference on the Enhanced Safety of Vehicles Vol 457. Amsterdam, The Netherlands 2001. [Google Scholar]
- 18.Leport T, Baudrit P, Potier P, Trosseille X, Lecuyer E, Vallancien G. Study of rib fracture mechanisms based on the rib strain profiles in side and forward oblique impact. Stapp Car Crash J. 2011;55:199. [DOI] [PubMed] [Google Scholar]
- 19.Martin MJ, Mullenix PS, Steele SR, et al. Functional outcome after blunt and penetrating carotid artery injuries: analysis of the National Trauma Data Bank. J Trauma Acute Care Surg. 2005;59(4):860–864. [DOI] [PubMed] [Google Scholar]
- 20.Martin MJ, Weng J, Demetriades D, Salim A. Patterns of injury and functional outcome after hanging: analysis of the National Trauma Data Bank. Am J Surg. 2005;190(6):838–843. [DOI] [PubMed] [Google Scholar]
- 21.Morris A, Welsh R, Hassan A. Requirements for crash protection of older drivers. Annu Proc Assoc Adv Automot Med. 2003;47:165–179. [PMC free article] [PubMed] [Google Scholar]
- 22.National Highway Traffic Safety Administration. National Automotive Sampling System: Department of Transportation; 2011. [Google Scholar]
- 23.Ottenbacher KJ, Hsu Y, Granger CV, Fiedler RC. The reliability of the functional independence measure: a quantitative review. Arch Phys Med Rehabil. 1996;77(12):1226–1232. [DOI] [PubMed] [Google Scholar]
- 24.Schoell SL, Weaver AA, Talton JW, et al. Functional outcomes of motor vehicle crash head injuries in pediatric and adult occupants. Traffic Inj Prev. 2016;17(sup1):27–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schoell SL, Weaver AA, Vavalle NA, Stitzel JD. Age-and sex-specific thorax finite element model development and simulation. Traffic Inj Prev. 2015;16(sup1):S57–S65. [DOI] [PubMed] [Google Scholar]
- 26.Spaniolas K, Velmahos GC, Alam HB, De Moya M, Tabbara M, Sailhamer E. Does improved detection of blunt vertebral artery injuries lead to improved outcomes? Analysis of the National Trauma Data Bank®. World J Surg. 2008;32(10):2190–2194. [DOI] [PubMed] [Google Scholar]
- 27.Stineman MG, Shea JA, Jette A, et al. The Functional Independence Measure: tests of scaling assumptions, structure, and reliability across 20 diverse impairment categories. Arch Phys Med Rehabil. November 1996;77(11):1101–1108. [DOI] [PubMed] [Google Scholar]
- 28.Uniform Data System for Medical Rehabilitation. The FIM System 2007.
- 29.Weaver AA, Barnard RT, Kilgo PD, Martin RS, Stitzel JD. Mortality-based quantification of injury severity for frequently occuring motor vehicle crash injuries. Annu Proc Assoc Adv Automot Med. 2013;57:235–245. [PMC free article] [PubMed] [Google Scholar]
- 30.Winthrop AL, Brasel KJ, Stahovic L, Paulson J, Schneeberger B, Kuhn EM. Quality of life and functional outcome after pediatric trauma. J Trauma Acute Care Surg. 2005;58(3):468–474. [DOI] [PubMed] [Google Scholar]
- 31.Zhou Q, Rouhana SW, Melvin JW. Age effects on thoracic injury tolerance. Stapp Car Crash J. 1996;40:137–148. [Google Scholar]
- 32.Zioupos P, Currey J. Changes in the stiffness, strength, and toughness of human cortical bone with age. Bone. 1998;22(1):57–66. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.