Key Points
Question
Can 3-dimensional (3-D) printing technology be used to create short-segment mandibular fracture templates that reduce the time and cost of preoperative planning for repair?
Findings
In this feasibility study using data from 3 patients, the estimated time and cost for creating a 3-D–printed short-segment template with details sufficient for adequate precontouring of a fracture plate was much less than those for creating a perfected complete mandible model using equipment marketed for medical applications.
Meaning
Our proposed 3-D–printed site-specific short-segment mandibular fracture template prototype has potential time and cost benefits for practical application in mandibular fracture management.
This feasibility study explores the potential application of a 3-dimensional–printed short-segment mandibular template in the management of complex mandibular fractures.
Abstract
Importance
After reduction of complex mandibular fractures, contouring of the fracture plates to fixate the reduced mandibular segments can be time-consuming.
Objective
To explore the potential application of a 3-dimensional (3-D)-printed short-segment mandibular template in the management of complex mandibular fractures.
Design, Setting, and Participants
A feasibility study was performed at a tertiary academic center using maxillofacial computed tomography data of 3 patients with comminuted mandibular fractures who required preoperative planning with a perfected complete mandible model.
Interventions
Thresholding, segmentation, and realignment of the fractured mandible were performed based on computed tomography data. Each reduced mandible design was divided to create 3-D templates for 6 fracture sites: right and left angle, body, and symphyseal/parasymphyseal. Sessions were conducted with junior otolaryngology and plastic surgery residents, during which mandibular fracture plates were contoured in a “preoperative” setting against the 3-D–printed short-segment templates, and an “intraoperative” setting against the previously manufactured, complete mandible model. The previously manufactured, complete model served as a surrogate for the intraoperative mandible with the fracture site reduced.
Main Outcomes and Measures
The time for 3-D template printing, the “preoperative” (measure of the time consumed preoperatively), and “intraoperative” (measure of the time saved intraoperatively) times were recorded. Comparisons were made for cost estimates between a complete model and the 3-D–printed short-segment template. The operating room charge equivalent of the intraoperative time was also calculated.
Results
Of the 3 patients whose data were used, 1 was a teenager and 2 were young adults. The total time for 3-D modeling and printing per short-segment template was less than 3 hours. The median (range) intraoperative time saved by precontouring the fracture plates was 7 (1-14), 5 (1-30), and 7 (2-15) minutes, and the operating room charge equivalents were $350.35 ($50.05-$700.70), $250 ($50.05-$1501.50), and $350.35 ($100.10-$750.75) for the angle, body, and symphyseal/parasymphyseal segments, respectively. The total cost for a single 3-D–printed template was less than $20, while that for a perfected complete model was approximately $2200.
Conclusions and Relevance
We demonstrate that patient- and site-specific 3-D–printed short-segment templates can be created within the timeframe required for mandibular fracture repair. These novel 3-D–printed templates also demonstrate cost efficiency in the preoperative planning for complex mandibular fracture management compared with perfected models and facilitate plate contouring in a similar fashion. Estimation of reduced operative room cost and time with the application of these short-segment templates warrants studies in actual patient care.
Level of Evidence
NA.
Introduction
Facial plastic and reconstructive surgery is heavily reliant on diagnostic medical imaging in the preoperative planning process.1 From bony reconstruction for congenital malformations2 or bony tumor resection3 to cosmetic rhinoplasty4 and complex facial fracture repair,5,6 medical imaging is frequently integral to planning the appropriate surgical or reconstructive approach. Three-dimensional (3-D) reconstructions displayed on 2-dimensional workstations are helpful, but limited in the benefit that they provide. Three-dimensional printing, also known as rapid prototyping, additive manufacturing, or solid-freeform technology,7 has revolutionized the field of plastic and reconstructive surgery.8,9,10,11,12 From medical models to implantable devices and tissues, 3-D printing often allows for a more precise understanding of the anatomy and visuospatial relationship between structures.13,14 Many physicians are reluctant to embrace potential clinical applications because of their misconceptions about the complexity of using 3-D printing in patient care or concerns about the cost-efficacy balance.13,15 However, with the decreasing cost of 3-D printers16 and the public accessibility and continuously improving usability of (open-source) processing software,17,18 the potential applications for this technology have skyrocketed. One application in plastic and reconstructive surgery is intramural printing of 3-D guides for the precontouring of plates used for facial fracture repair. Precontouring of plates is considered easier to perform than contouring plates intraoperatively. Given the potential for complications with mandibular fracture repair surgery, avenues for decreasing the challenges inherent to the surgery should be considered.19 The use of precontoured plates has also been shown to shorten operative times in reconstructive mandibular surgery.20,21,22
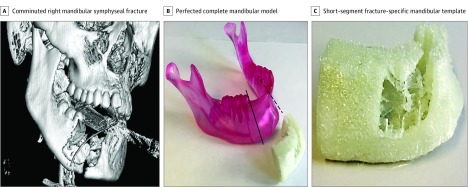
Our objective was to explore the theoretical and practical applications for rapid, inexpensive 3-D printing of a short-segment mandibular template prototype in mandibular fracture repair. The short-segment template is specific to a fracture site, and facilitates precontouring of plates while eliminating the unnecessary portions of a perfected complete mandible (Figure 1). We hypothesized that the preoperative use of the 3-D–printed fracture-specific, short-segment mandibular fracture templates is feasible and cost-effective and will shorten overall operative times. Our specific objectives were to demonstrate that (1) 3-D–printed patient- and fracture-specific mandibular templates can be created within the timeframe required for mandibular fracture surgery, (2) the use of these templates will shorten overall operative times for surgery, and (3) the application of these short-segment templates will be cost-effective.
Figure 1. 3-Dimensional–Printed Short-Segment Template.
A, Three-dimensional computed tomography reconstruction image showing a comminuted right mandibular symphyseal fracture. B, Perfected complete mandibular model with portions unnecessary for plate contouring to the left of the solid line and to the right of the dashed line. C, Short-segment fracture-specific mandibular template.
Methods
The study protocol was approved by the institutional review board of Washington University in St Louis School of Medicine. The institutional review board approved a waiver of informed consent due to the retrospective nature of the study. Patients with comminuted mandibular fractures, which required preoperative planning with a perfected complete mandible model, were identified for this study. Deidentified multislice computed tomography (CT) scans of these patients were used.
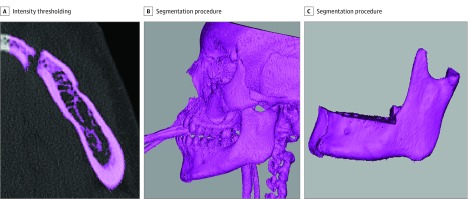
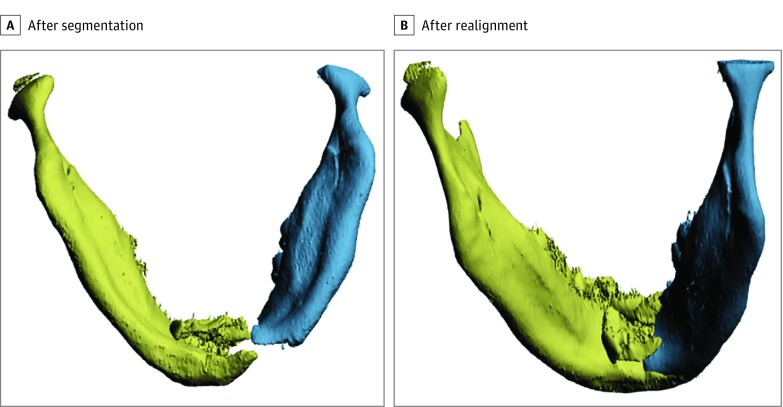
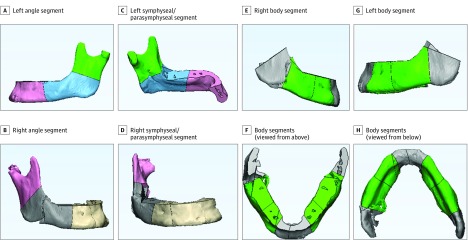
3-D Printing of Template
The data acquired from the multislice CT scans were saved in Digital Imaging and Communications in Medicine (DICOM) format. Following CT acquisition, various processes of design and 3-D modeling led to the 3-D printing of templates for application in plate contouring (eFigure 1 in the Supplement). Intensity thresholding of the deidentified maxillofacial CT data was performed. Intensity thresholding refers to the selection of CT pixels based on brightness. The brightness of pixels is, in turn, determined by the radiodensity of the tissues. The operator must select the appropriate range of intensity (brightness) to select only the bony tissue. Thresholding was followed by manual segmentation (Figure 2) either slice by slice or on 3-D reconstructions of the data. Following segmentation, the modeled pieces of the fractured mandible were realigned to imitate the optimally reduced postoperative position (Figure 3). Each reduced mandible model design was divided (Figure 4) into short-segment mandibular templates for 6 potential fracture sites—right/left angle, body, and symphyseal with or without parasymphyseal region. The minimum length of each 3-D–printed short-segment mandibular template was set at 6 cm so as to accommodate a 6-hole fracture plate. Templates were then converted to Standard Triangulation Language file format for printer compatibility. Both open-source and professional programs were used to create the 3-D–printed patient-specific mandibular fracture templates; printing costs, as well as design and print times, were recorded. The open-source software included InVesalius 3.0 (Centro de Tecnologia da Informação Renato Archer) for initial segmentation, and Blender 2.78 (Blender Institute BV) for object realignment, cutting, and file format conversion. The professional software was MIMICS (Materialise Interactive Medical Image Control System) Medical 19.0 for segmentation and 3-Matic 11.0 (Materialise) for realignment, cutting, and file format conversion. Template segments were then printed from polylactic acid filament on a low-cost printer (MakerGear M2) for all 6 sites for every case.
Figure 2. 3-Dimensional Modeling.
A, Intensity thresholding based on bone density. B and C, Segmentation procedure of multislice computerized tomography images.
Figure 3. The 2 Pieces of Fractured Mandible .
A, The 2 pieces in the scanned position after segmentation. B, The 2 pieces in the scanned position after realignment to imitate the reduced postoperative position.
Figure 4. Division of Optimally Reduced Mandible Into Template Segments.
Study Conduct
Study sessions were planned with junior residents in postgraduate year 1 and 2 with fewer than 5 open reduction and internal fixation (ORIF) mandibular procedures logged in their Accreditation Council for Graduate Medical Education (ACGME) case log. The postgraduate year 1 and 2 residents were selected to avoid bias from prestudy knowledge of mandibular fracture plating. The junior residents from the Departments of Otolaryngology and Plastic Surgery were asked to report the number of times that they had hands-on experience with plate bending, and the number of times that they had participated in a plating course. A cutoff of 5 for the cumulative hands-on experience based on ACGME case logs and a cutoff of 2 for self-reported plating course participation were used to identify residents for the present study. Instructional videos and links to additional information from the AO Foundation on bending techniques were provided to the participating residents well in advance of the study initiation. Prior to study commencement on the day of study sessions, participants were provided with a detailed explanation of the study procedures, the fundamentals of bending technique, and the gamut of instrumentation planned for use in the study. Two fellowship-trained attending surgeons specialized in facial plastic and reconstructive surgery (G.H.B.) and craniofacial surgery (K.B.P.) served as study session supervisors.
The study had 2 components, a “preoperative” part, and an “intraoperative” part. The 3-D–printed short-segment mandibular templates were used for the preoperative part of the study. This portion of the study demonstrates the preoperative bending time of the fracture plate around a 3-D–printed short segment of the reduced mandible fracture site. The previously manufactured perfected complete mandible models were used as surrogates for the appropriately reduced mandibular fracture(s) during the intraoperative part of the study. These models were created for the repair of complex mandibular fractures by a craniofacial plating company with computer-aided drafting by a third-party design firm. During the study sessions, the junior residents contoured the mandibular fracture plates using the 3-D–printed short-segment mandibular templates to generate the preoperative bending time. The same junior residents also contoured the mandibular fracture plates using the previously manufactured perfected complete mandible models to generate the intraoperative time spent on plate bending. This was done for each of the 6 fracture sites. Straight and angled 6-hole fracture plates of 1.5 mm thickness were used. Adequate precautions were taken to mitigate the learning curve associated with these study procedures. These included recruitment of different residents for different study sessions conducted at different time intervals. Further variability was introduced within each session by altering the site of the fracture and sequences for the preoperative and intraoperative portions. The contoured plates created in the study sessions were used only for the study and were not saved for the purpose of patient care.
Quality Assessment
The residents bent the preoperative and intraoperative plates until a satisfactory contour quality was attained as confirmed by the 2 study session supervisors (K.B.P., G.H.B.). The contouring was not considered complete and the resident could not proceed to the next fracture site until a study session supervisor agreed that the contour of the plate appropriately matched the contour of the reduced fracture site.
Analysis
For objective 1, the time taken to convert the multislice CT data DICOM to a model design in Standard Triangulation Language format and to 3-D print a short-segment template was computed. For objective 2, the time taken for intraoperative plate contouring against the reduced mandible fracture was recorded for each specific site as a surrogate of the time saved intraoperatively. The operating room (OR) cost equivalent of the intraoperative time was computed based on Barnes Jewish Hospital’s billing data. For objective 3, the costs of the perfected complete model and that of the 3-D–printed short-segment templates were estimated. Comparisons between times and OR cost equivalents for different fracture sites were made using the t test or its nonparametric equivalent Mann-Whitney U test. Statistical analysis was conducted using SPSS software (IBM SPSS Statistics, release 24.0.0).
Results
Three consecutive patients who required preoperative planning with a perfected complete 3-D–printed mandible model from October 2015 to May 2016 were identified. All 3 patients presented with complex, comminuted and displaced, open mandibular fractures involving the symphysis and parasymphysis alone or in combination with the angle or the body segments. Of the 3 patients, 1 was a teenager and 2 were young adults, and the fractures were secondary to assault, gunshot wound, or motor vehicle crash.
Time and Cost Estimates for 3-D Modeling and Printing of Short-Segment Templates
The modeling time per mandible including intensity thresholding and segmentation was 1.0 hour with the professional software and 1.5 hours using the open-source software. Billing per mandible from the 3-D printing laboratory (G.S.) at our institution was as follows: approximately $30 for consultation per mandible ($80 for all 3), and $120 ($80/h) for modeling time using the open-source software. The materials cost per mandible was less than $4. The 3-D printing time per mandible for all 6 templates was approximately 4 hours, and the total cost was $40 at $10 per hour. Thus, per mandible, the total time for 3-D modeling was 1.5 hours with open-source software, the total time for 3-D printing of 6 site-specific templates was 4 hours, and the total cost was approximately $200. Per template, the combined modeling (open-source software) and 3-D printing time was less than 3 hours, and the 3-D printing cost was less than $20 (excluding the charges for consultation and modeling).
Study Sessions and Time for Plate Contouring
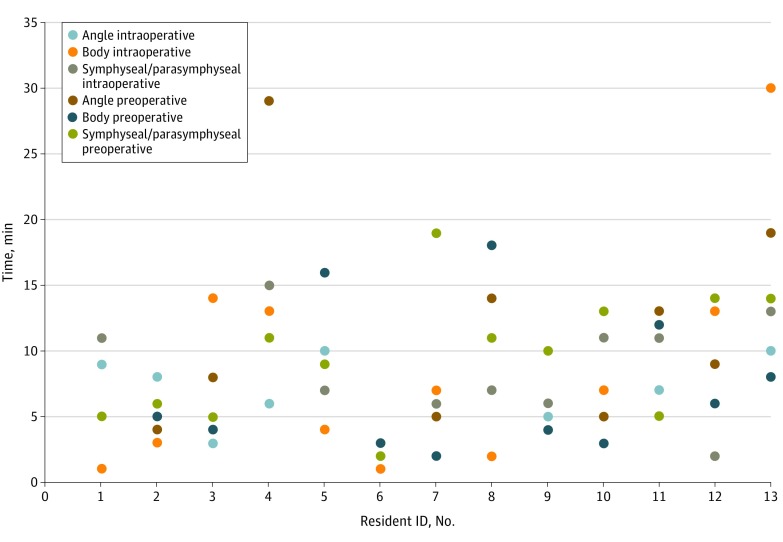
A total of 13 residents met the participation criteria and performed the plate contouring sessions. The distribution of fracture site–specific preoperative and intraoperative times is presented in Figure 5. Median values are reported due to the nonnormal distribution of the data. The median (range) preoperative time was 8 (3-29), 5 (2-18), and 10 (2-19) minutes for the angle, body, and symphyseal/ parasymphyseal segments while the intraoperative times were 7 (1-14), 5 (1-30), and 7 (2-15) minutes, respectively. Although comparison of the preoperative and intraoperative times was not a primary objective, we did not observe any major difference between these times for any of the sites. There were no statistically significant differences either for the median preoperative or the intraoperative times between the different fracture sites.
Figure 5. Distribution of Intraoperative and Preoperative Plate Contouring Times for Different Sites in the Resident Study Sessions.
Cost Estimates for the Perfected Complete Model
Based on the pricing information from the medical modeling firm (identity not disclosed), the cost estimate for a standard perfected complete mandibular model was approximately $2200.
Cost Estimates for OR Time Savings
We further calculated the OR charge equivalent based on the intraoperative time. The median (range) OR charge equivalent ($50.05/min at Barnes Jewish Hospital) of the intraoperative times was $350.35 ($50.05-$700.70), $250 ($50.05-$1501.50), and $350.35 ($100.10-$750.75), for the angle, body, and symphyseal/parasymphyseal segments, respectively.
Discussion
Repair of a comminuted and displaced mandibular fracture is a challenging problem. Based on CT data from previously managed comminuted fracture cases in which medical modeling was used, our feasibility study demonstrated that patient- and site-specific 3-D–printed short-segment mandibular templates can be created to facilitate preoperative planning within hours and at a very low cost.
Computer-aided reconstructed and perfected models of fractured mandibles are often created to facilitate preoperative planning, including contouring of plates. Contouring plates in a preoperative setting is generally easier to perform and saves time compared with intraoperative contouring. Customized precontoured plates can also be created in addition to computer-aided perfected mandibular models. The use of precontoured plates has been shown to reduce OR time from 17% to 60%, with an average of 20%.23 However, these perfected models or customized precontoured plates are manufactured by a third-party medical modeling or craniofacial plating company. Application of these customized, perfected models or precontoured plates is not optimal for mandibular fractures, given the usual prolonged turnaround times ranging from 10 days to 3 weeks.15 The costs associated with these products can also be considerable. With advances in 3-D printing technology, the printing time is no longer prohibitive,16 and its routine use seems more practical in facial trauma surgery now than it did a few years ago. Furthermore, 3-D printers are now low enough in cost and compact enough for in-office use.17 The cost of the MakerGear printer used in our study was $1825; lower-cost desktop printers are also available. So far, reports have been published on the use of rapid 3-D prototyping technique to generate a complete craniofacial model to help surgeons replicate fracture lines, reduce replicated fracture, and contour plates.13 However, a propos of mandibular fractures, we believe that creation of a perfected, complete mandibular model for preoperative planning is redundant. First, there may not be much utility in creating a perfected model to help surgeons plan an approach to reduction because fracture reduction is greatly affected by intraoperative factors that cannot be comprehensively determined outside intraoperative settings. Second, the perfected model seems superfluous for the purpose of precontouring mandibular plates because the area of practical importance to facilitate precontouring is usually a few centimeters on either side of the actual mandibular fracture (Figure 1). Hence, complete mandibular models with additional embellishments of dentition, colored structures, foramina, etc, are not essential to preoperative contouring; however, exceptional situations can exist such as complex angle-to-angle fractures. We therefore confined the 3-D–printed mandibular template prototype to approximately 6 cm with sufficient space on either side of the fracture line, anticipating that it would serve a similar purpose albeit at a lower cost and printing time than a complete model. Furthermore, previous reports on rapid 3-D printing technology to create mandible models, although sparse, have used professional software.13 Open-source software is now available that further facilitates application of this technology without increasing the costs.18 Interactive modules accompanying the open-source software, as well as online sources, allow users to acquire 3-D visualization and modeling skills. The use of open-source software in our feasibility study did not affect the quality of 3-D modeling, and the total modeling time exceeded that with the professional software by only 30 minutes. We demonstrate that the open-source software has potential for rapid in-office 3-D printing of patient- and site-specific templates to facilitate preoperative planning in a time-sensitive manner without having to rely on a third party.
Furthermore, we estimate shortened overall operative times, even in the hands of residents with minimal experience in ORIF. The shortened OR time as indicated by the intraoperative measure in our study ranged from 1 to 14 minutes for the angle, 1 to 30 minutes for the body, and 2 to 15 minutes for the symphyseal/parasymphyseal segments. We attribute the wide range to different levels of innate plate-bending skills because all residents had an overall low exposure to ORIF. Similar variation was noted for the preoperative times. Despite the variation, the contours of the preoperative and intraoperative plates were comparable. These observations support our hypothesis that the use of 3-D–printed short-segment templates in preoperative planning for mandibular fracture repair can contribute to reduced OR time. However, accurate projections on reduced operative time from use of the 3-D–printed short-segment template would require application of the technology in actual patient care.
Last, with the objective of reconciling the time efficiency against the production time and cost of creating a 3-D model, we observed that our prototype for a 3-D–printed short-segment mandibular template is also cost efficient for the preoperative planning. The costs for a third party to manufacture a perfected mandibular model range from $2000 to $6000 depending on the material and technology.15 Given the average cost of a perfected complete mandibular model of more than $2000, creating a site-specific short-segment mandibular template using our proposed prototype will cost less than $20, similar to costs reported in other studies that have used in-office printers.15 The 3-D printing material is quite inexpensive: a 2-pound (0.9-kg) spool of the polylactic acid filament used to create our prototype costs approximately $15 to $20. Less than 0.2 kg was used to create all 6 templates for a case in our study. The estimated cost of less than $20 for our prototype does not include consultation fees. For our feasibility study, we enlisted the help of a craniofacial laboratory analyst with expertise in 3-D printing. However, as noted herein, the 3-D modeling skills can be acquired by surgeons by using the open-source software. Surgeon learning of the 3-D modeling techniques and installation of an in-office printer will further drive the patient care and economic benefits. Thus, our feasibility study showed that 3-D printing of short-segment mandibular fracture templates can have immediate applications in the management of patients with complex mandibular fractures necessitating preoperative planning in less time and at lower costs than complete mandibular models. Our 3-D–printed short-segment fracture template prototype was patient and site specific, and included enough details to allow for accurate precontouring of the plate across the mandibular fracture.
Limitations
We are unable to present the data for application of these novel templates in actual patient care. Because this was a feasibility study, we wanted to explore the application of these templates in an experimental setting to obtain the time and cost information. Furthermore, we have not demonstrated the 3-D modeling technique learning by surgeons using the open-source software. We aimed to assess the association of open-source software use with quality and time first in the hands of a 3-D printing expert (G.S.), and then proceed with the training of surgeons to complete our long-term objectives of attaining self-reliance in rapid in-office 3-D printing. Recent studies evaluating surgical team–performed 3-D modeling with open-source software in mandibular reconstruction have emphasized the importance of surgeon learning toward achieving precision in the technique.24,25
Conclusions
Patient- and fracture site–specific 3-D–printed short-segment mandibular templates can be created within the timeframe required for repair of complex, comminuted mandibular fractures at lower costs than the complete, perfected mandibular models. The 3-D–printed short-segment mandibular templates facilitated preoperative plate contouring in a fashion similar to the perfected mandible models and have the potential to reduce operative times. However, a reliable estimation of the OR cost and time will require further studies in actual patient care. The quality for 3-D modeling using open-source software was comparable to that with the professional software.
eFigure. Diagram illustrates the workflow following CT acquisition through the processes of design, 3D-printing and application for plate contouring
References
- 1.Papadopoulos MA, Christou PK, Christou PK, et al. . Three-dimensional craniofacial reconstruction imaging. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93(4):382-393. [DOI] [PubMed] [Google Scholar]
- 2.James WJ, Slabbekoorn MA, Edgin WA, Hardin CK. Correction of congenital malar hypoplasia using stereolithography for presurgical planning. J Oral Maxillofac Surg. 1998;56(4):512-517. [DOI] [PubMed] [Google Scholar]
- 3.Santler G, Kärcher H, Ruda C. Indications and limitations of three-dimensional models in cranio-maxillofacial surgery. J Craniomaxillofac Surg. 1998;26(1):11-16. [DOI] [PubMed] [Google Scholar]
- 4.Ewart CJ, Leonard CJ, Harper JG, Yu J. A simple and inexpensive method of preoperative computer imaging for rhinoplasty. Ann Plast Surg. 2006;56(1):46-49. [DOI] [PubMed] [Google Scholar]
- 5.Kozakiewicz M, Elgalal M, Loba P, et al. . Clinical application of 3D pre-bent titanium implants for orbital floor fractures. J Craniomaxillofac Surg. 2009;37(4):229-234. [DOI] [PubMed] [Google Scholar]
- 6.Tepper OM, Sorice S, Hershman GN, Saadeh P, Levine JP, Hirsch D. Use of virtual 3-dimensional surgery in post-traumatic craniomaxillofacial reconstruction. J Oral Maxillofac Surg. 2011;69(3):733-741. [DOI] [PubMed] [Google Scholar]
- 7.Gross BC, Erkal JL, Lockwood SY, Chen C, Spence DM. Evaluation of 3D printing and its potential impact on biotechnology and the chemical sciences. Anal Chem. 2014;86(7):3240-3253. [DOI] [PubMed] [Google Scholar]
- 8.Azuma M, Yanagawa T, Ishibashi-Kanno N, et al. . Mandibular reconstruction using plates prebent to fit rapid prototyping 3-dimensional printing models ameliorates contour deformity. Head Face Med. 2014;10:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Parthasarathy J. 3D Modeling, custom implants and its future perspectives in craniofacial surgery. Ann Maxillofac Surg. 2014;4(1):9-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hanasono MM, Skoracki RJ. Computer-assisted design and rapid prototype modeling in microvascular mandible reconstruction. Laryngoscope. 2013;123(3):597-604. [DOI] [PubMed] [Google Scholar]
- 11.Chae MP, Rozen WM, McMenamin PG, Findlay MW, Spychal RT, Hunter-Smith DJ. Emerging applications of bedside 3D printing in plastic surgery. Front Surg. 2015;2:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gray E, Maducdoc M, Manuel C, Wong BJF. Estimation of nasal tip support using computer-aided design and 3-dimensional printed models. JAMA Facial Plast Surg. 2016;18(4):285-291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wagner JD, Baack B, Brown GA, Kelly J. Rapid 3-dimensional prototyping for surgical repair of maxillofacial fractures: a technical note. J Oral Maxillofac Surg. 2004;62(7):898-901. [DOI] [PubMed] [Google Scholar]
- 14.Ren J, Zhou Z, Li P, et al. . Three-dimensional planning in maxillofacial fracture surgery: computer-aided design/computer-aided manufacture surgical splints by integrating cone beam computerized tomography images into multislice computerized tomography images. J Craniofac Surg. 2016;27(6):1415-1419. [DOI] [PubMed] [Google Scholar]
- 15.Mendez BM, Chiodo MV, Patel PA. Customized “in-office” three-dimensional printing for virtual surgical planning in craniofacial surgery. J Craniofac Surg. 2015;26(5):1584-1586. [DOI] [PubMed] [Google Scholar]
- 16.Ventola CL. Medical applications for 3D printing: current and projected uses. P T. 2014;39(10):704-711. [PMC free article] [PubMed] [Google Scholar]
- 17.Velasco I, Vahdani S, Ramos H. Low-cost method for obtaining medical rapid prototyping using desktop 3D printing: a novel technique for mandibular reconstruction planning. J Clin Exp Dent. 2017;9(9):e1103-e1108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McAllister P, Watson M, Burke E. A cost-effective, in-house, positioning and cutting guide system for orthognathic surgery. J Maxillofac Oral Surg. 2018;17(1):112-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen CL, Zenga J, Patel R, Branham G. Complications and reoperations in mandibular angle fractures [published online January 4, 2018]. JAMA Facial Plast Surg. doi: 10.1001/jamafacial.2017.2227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hanasono M, Skoracki R. 117B: Improving the speed and accuracy of mandibular reconstruction using preoperative virtual planning and rapid prototype modeling. Plast Reconstr Surg. 2010;125(suppl):80. [DOI] [PubMed] [Google Scholar]
- 21.Lethaus B, Poort L, Böckmann R, Smeets R, Tolba R, Kessler P. Additive manufacturing for microvascular reconstruction of the mandible in 20 patients. J Craniomaxillofac Surg. 2012;40(1):43-46. [DOI] [PubMed] [Google Scholar]
- 22.Strong EB, Fuller SC, Wiley DF, Zumbansen J, Wilson MD, Metzger MC. Preformed vs intraoperative bending of titanium mesh for orbital reconstruction. Otolaryngol Head Neck Surg. 2013;149(1):60-66. [DOI] [PubMed] [Google Scholar]
- 23.Salgueiro MI, Stevens MR. Experience with the use of prebent plates for the reconstruction of mandibular defects. Craniomaxillofac Trauma Reconstr. 2010;3(4):201-208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ganry L, Quilichini J, Bandini CM, Leyder P, Hersant B, Meningaud JP. Three-dimensional surgical modelling with an open-source software protocol: study of precision and reproducibility in mandibular reconstruction with the fibula free flap. Int J Oral Maxillofac Surg. 2017;46(8):946-957. [DOI] [PubMed] [Google Scholar]
- 25.Ganry L, Hersant B, Quilichini J, Leyder P, Meningaud JP. Use of the 3D surgical modelling technique with open-source software for mandibular fibula free flap reconstruction and its surgical guides. J Stomatol Oral Maxillofac Surg. 2017;118(3):197-202. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure. Diagram illustrates the workflow following CT acquisition through the processes of design, 3D-printing and application for plate contouring