Abstract
Objective
To determine the effects of diets varying in carbohydrate to fat ratio on total energy expenditure.
Design
Randomized trial.
Setting
Multicenter collaboration at US two sites, August 2014 to May 2017.
Participants
164 adults aged 18-65 years with a body mass index of 25 or more.
Interventions
After 12% (within 2%) weight loss on a run-in diet, participants were randomly assigned to one of three test diets according to carbohydrate content (high, 60%, n=54; moderate, 40%, n=53; or low, 20%, n=57) for 20 weeks. Test diets were controlled for protein and were energy adjusted to maintain weight loss within 2 kg. To test for effect modification predicted by the carbohydrate-insulin model, the sample was divided into thirds of pre-weight loss insulin secretion (insulin concentration 30 minutes after oral glucose).
Main outcome measures
The primary outcome was total energy expenditure, measured with doubly labeled water, by intention-to-treat analysis. Per protocol analysis included participants who maintained target weight loss, potentially providing a more precise effect estimate. Secondary outcomes were resting energy expenditure, measures of physical activity, and levels of the metabolic hormones leptin and ghrelin.
Results
Total energy expenditure differed by diet in the intention-to-treat analysis (n=162, P=0.002), with a linear trend of 52 kcal/d (95% confidence interval 23 to 82) for every 10% decrease in the contribution of carbohydrate to total energy intake (1 kcal=4.18 kJ=0.00418 MJ). Change in total energy expenditure was 91 kcal/d (95% confidence interval −29 to 210) greater in participants assigned to the moderate carbohydrate diet and 209 kcal/d (91 to 326) greater in those assigned to the low carbohydrate diet compared with the high carbohydrate diet. In the per protocol analysis (n=120, P<0.001), the respective differences were 131 kcal/d (−6 to 267) and 278 kcal/d (144 to 411). Among participants in the highest third of pre-weight loss insulin secretion, the difference between the low and high carbohydrate diet was 308 kcal/d in the intention-to-treat analysis and 478 kcal/d in the per protocol analysis (P<0.004). Ghrelin was significantly lower in participants assigned to the low carbohydrate diet compared with those assigned to the high carbohydrate diet (both analyses). Leptin was also significantly lower in participants assigned to the low carbohydrate diet (per protocol).
Conclusions
Consistent with the carbohydrate-insulin model, lowering dietary carbohydrate increased energy expenditure during weight loss maintenance. This metabolic effect may improve the success of obesity treatment, especially among those with high insulin secretion.
Trial registration
ClinicalTrials.gov NCT02068885.
Introduction
Evidence from animal and human studies shows that biological factors strongly influence body weight.1 With weight loss, hunger increases and energy expenditure decreases—physiological adaptations that defend against long term weight change.2 Genetic factors are known to affect body weight, explaining some of the variance in body mass index (BMI) among people. However, genetic factors cannot explain why the average person today, compared with 40 years ago, seems to be “defending” a much higher body weight.
According to the carbohydrate-insulin model of obesity,3 4 5 6 the increased ratio of insulin to glucagon concentrations after consumption of a meal with a high glycemic load directs metabolic fuels away from oxidation and toward storage in adipose tissue. This physiological state is hypothesized to increase hunger and food cravings,7 lower energy expenditure, and predispose to weight gain, especially among those with inherently high insulin secretion. The carbohydrate-insulin model offers a physiological mechanism for understanding why obesity rates have increased since the 1970s in the United States, as dietary fats were replaced with high glycemic load foods, including refined grains and added sugars.8 9
This model has been challenged, primarily owing to lack of evidence from controlled feeding studies.10 11 12 13 14 A recent meta-analysis reported no meaningful difference in energy expenditure between low carbohydrate and low fat diets.11 The studies included in that analysis, however, were short term (mostly <2 weeks), whereas the process of adapting to a low carbohydrate, high fat diet seems to take at least two or three weeks.6 15 16 17 18 For this reason, transient effects of macronutrients cannot be distinguished from long term effects on the basis of existing evidence. We compared the effects of diets varying in carbohydrate to fat ratio on energy expenditure during weight loss maintenance through 20 weeks.
Methods
The study protocol has been previously published.19 We collected data on the campus of Framingham State University, Massachusetts, between August 2014 and May 2017. For implementing controlled feeding protocols with free living participants, we established a partnership with Sodexo, the food service contractor at Framingham State University.20 For the final year of the study, a satellite feeding site was established at Assabet Valley Regional Technical High School (Marlborough, MA). The study was known as the Framingham State Food Study, or (FS)2.
Design
We carried out a randomized controlled trial with run-in and test phases (fig 1). During the run-in phase, energy intake was restricted to promote 12% (within 2%) weight loss over 9-10 weeks. We randomly assigned participants who achieved the target weight loss to high, moderate, or low carbohydrate test diets for a 20 week test phase. During the test phase, participants’ energy intake was adjusted periodically to maintain weight loss within 2 kg of the level achieved before randomization. Participants were asked to weigh themselves daily using calibrated Wi-Fi scales (Withings, Cambridge, MA) during both phases. Study outcomes were assessed at several time points: pre-weight loss, start of trial (weeks −2 to 0, before randomization), midpoint of test phase (weeks 8 to 10), and end of test phase (weeks 18 to 20), as summarized in figure 1 and supplemental eTable 1.
Fig 1.
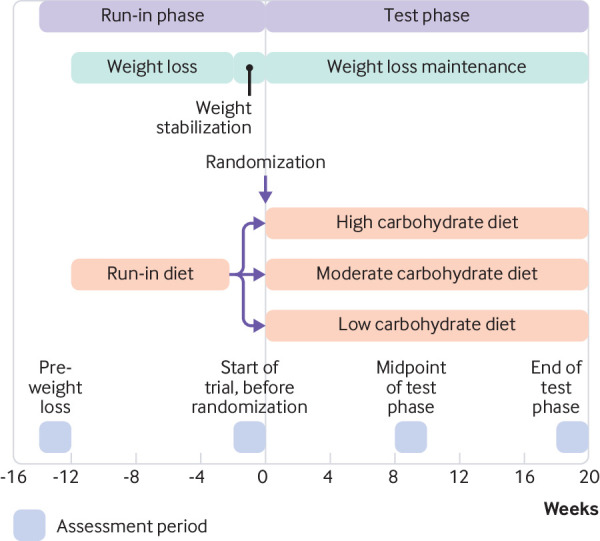
Study design
Participants
Adults aged 18 to 65 years, with a BMI (weight (kg)/(height (m)2) of 25 or higher and body weight less than 160 kg, were screened for participation before pre-weight loss assessments. Supplemental eTable 2 presents additional eligibility criteria. For each of three cohorts, recruitment occurred during the spring semester before the respective academic year (August to May) of study participation. Participants provided written informed consent at the time of enrolment. The stipend for participation was $3280 (£2559; €2880) over the course of the study, and meals were valued at $3220, for total compensation of $6500. (See supplemental methods for details on implementation of randomization.)
Dietary interventions
During the run-in phase, the macronutrient composition of the run-in diet was 45% of total energy from carbohydrate, 30% from fat, and 25% from protein. The target macronutrient composition of the run-in diet reflects ranges considered acceptable by the Institute of Medicine,21 with protein at the upper end of the range to enhance satiety during weight loss.22 We determined individual energy needs on the basis of resting requirements, estimated using a regression equation23 24 and multiplied by a physical activity factor of 1.5 (which corresponds to a light activity lifestyle).25 Energy intake was restricted to 60% of estimated needs. The research team monitored participants’ body weight and adjusted the amounts of food when necessary to achieve the target weight loss. At the end of the run-in phase, we adjusted energy intake to stabilize body weight on the basis of the recent rate of weight loss for each participant: energy intake during weight loss (kcal/d)+(rate of weight loss (kg/day)×7700 kcal/kg) (1 kcal=4.18 kJ=0.00418 MJ). During the test phase, high, moderate, and low carbohydrate diets varied in carbohydrate (60%, 40%, and 20% of total energy, respectively) and fat (20%, 40%, and 60%, respectively), with protein fixed at 20% (table 1). We controlled for protein, in view of its higher thermic effect,29 to provide a more specific test of the carbohydrate-insulin model. The relative amounts of added sugar (15% of total carbohydrate), saturated fat (35% of total fat), and sodium (3000 mg/2000 kcal) were held constant across diets. Based on regression of body weight (g) on time (days), a slope of 15 g or more each day over 14 days indicated the need to adjust energy intake to achieve weight stability within 2 kg of the start of trial weight. (See supplemental methods for details on menu development, quality control, and strategies to promote adherence.)
Table 1.
Dietary energy and macronutrient composition for test diets, calculated daily averages (for a 2000 kcal target)*
| Variables | Carbohydrate content | ||
|---|---|---|---|
| High | Moderate | Low | |
| Energy (kcal) | 2001 | 2001 | 2001 |
| Carbohydrate (g) | 305 | 205 | 105 |
| Carbohydrate (%)† | 59.2 | 39.7 | 20.3 |
| Glycemic index‡ | 49 | 46 | 30 |
| Glycemic load (g)‡ | 135 | 80 | 28 |
| Fat (g) | 48 | 92 | 137 |
| Fat (%)† | 20.9 | 40.1 | 59.6 |
| Saturated fat (%)§ | 5.9 | 13.7 | 20.9 |
| Monounsaturated fat (%)§ | 8.2 | 15.9 | 25.1 |
| Polyunsaturated fat (%)§ | 5.3 | 8.6 | 11.3 |
| Protein (g) | 102 | 104 | 103 |
| Protein (%)† | 19.9 | 20.2 | 20.1 |
| Fiber (g) | 33 | 28 | 22 |
| Food quotient¶ | 0.90 | 0.85 | 0.79 |
Values were calculated using Food Processor Nutrition Analysis Software (ESHA Research, Salem, OR).
Per cent of energy from macronutrients takes into account digestibility for some foods.
Glycemic index for each day was calculated by summing the weighted values for each food item: Σ(glycemic index for food item×proportion of total net carbohydrate contributed by item).26 Glycemic load was calculated as the product of the glycemic index and net carbohydrate for the day: (glycemic index/100)×net carbohydrate.27
Per cent of total energy. The target for saturated fat was 35% of total fat (equating to 7%, 14%, and 21% of total energy for high, moderate, and low carbohydrate diets, respectively). The remainder of the total fat target (20%, 40%, and 60% of total energy) was distributed between monounsaturated and polyunsaturated fat. The sum of saturated, monounsaturated, and polyunsaturated fat does not equal total fat because data on fat type were missing for some foods.
Food quotient (FQ) calculated using the equation of Black et al.28 FQ=(carbohydrate(%)×1.00)+(fat(%)×0.71)+(protein(%)×0.81).
Study outcomes
Prespecified outcomes included energy expenditure, measures of physical activity, and metabolic hormones. To test for effect modification predicted by the carbohydrate-insulin model we assessed insulin secretion (insulin concentration 30 minutes after oral glucose)30 31 at pre-weight loss. Staff masked to dietary group assignment collected data on outcomes. Total energy expenditure (primary outcome) was assessed using the doubly labeled water method.32 33 34 35 Participants provided two pre-dose spot urine samples on separate days and seven post-dose samples at regular intervals over an assessment period of 14 days. Isotopic enrichments of urine samples were measured in duplicate using gas isotope ratio mass spectrometry.36 The equation of Ravussin et al37 was used to calculate total energy expenditure from carbon dioxide production (rCO2), with food quotient as a proxy for respiratory quotient.28 We expressed total energy expenditure in kcal per kg body weight, then normalized this to average start of trial body weight (82 kg) for analysis and reporting. This approach takes into account small changes in body weight that might occur during the test phase, within our definition of weight loss maintenance (within 2 kg of the start of the trial weight), and thereby improve precision. Some investigators discourage adjustment of total energy expenditure for weight because of confounding that would arise from individual differences in relations between total energy expenditure and body weight, body composition, and metabolically active mass.38 However, this problem, inherent to cross sectional comparisons between people, would not apply to the within individual comparisons over several months in our study, especially during weight loss maintenance when these relations would not change in any meaningful way. We also examined absolute total energy expenditure expressed as kcal/d, with and without body weight included as a covariate, and we obtained similar results. (See supplemental methods for details on measurement of body weight, resting energy expenditure by indirect calorimetry, energy intake, physical activity by accelerometry, skeletal muscle work efficiency by cycle ergometry, oral glucose tolerance testing, and assays of blood samples.)
Statistical analysis
Sample size calculations were based on data from a preliminary study.19 The target of 135 completers provided 80% power, with 5% type I error, to detect a difference of 237 kcal/d in total energy expenditure change between one diet group and the other two diet groups. This difference is smaller than the effect detected in the previous study39 and is consistent with a predicted effect of 50 kcal/d per 10% decrease in the contribution of carbohydrate to total energy intake.6
Before unmasking of diet group assignment, the primary outcome measure, total energy expenditure, was derived from a non-linear decay model fitted jointly to urinary disappearance curves of stable oxygen and hydrogen isotopes after oral administration of the doubly labeled water.19 We used the jackknife technique to smooth the parameter estimates and discarded a small number of incomplete or poorly fitting curves, deviant data points, and implausible values.
The prespecified analytic framework for the primary outcome was repeated measures analysis of variance spanning three time points (start of trial, midpoint of test phase, and end of test phase), with diet assignment as a three level independent variable (high, moderate, low carbohydrate). The value at pre-weight loss, rather than start of trial, was originally specified in the registry as the basis for calculating change scores, but this error was corrected in an amendment to the institutional review board protocol, before unmasking diet group assignment. (See protocol amendment history in supplement for details.)
The main model was unadjusted except for design factors (study site, cohort, and enrolment wave). A fully adjusted model for the primary outcome also included demographic characteristics (sex, ethnicity, race, and age); pre-weight loss values for BMI, percentage lean mass, and total energy expenditure; and weight loss from pre-weight loss to start of trial. An unstructured covariance matrix provided maximum flexibility in modeling correlation within participants over time. From parameters of the fitted model, taking account of all data, we constructed the mean test phase change in total energy expenditure for each diet (covariate adjusted change between start of trial and midpoint of the test phase and end of the test phase, the latter two averaged) and tested the hypothesis that this change was uniform across diets, using a two degrees of freedom F test with a P value threshold for significance of 0.05. When this hypothesis was rejected, the principle of closed testing40 permitted us to make the three pairwise comparisons of the different macronutrient diets with critical P value 0.05 while preserving a maximum 5% type I error rate for the set of four potential comparisons (one overall and three pairwise). The high versus low carbohydrate diet comparison was equivalent to a test for linear trend across the three diets according to their equally spaced carbohydrate content.
To test for effect modification, we divided the sample into thirds of pre-weight loss insulin secretion, fasting glucose, and fasting insulin; added appropriate interaction terms to the repeated measures model; and constructed contrasts to test for linear trend across thirds for the between diet differences in change during the test phase.
Secondary outcomes (resting energy expenditure, physical activity, and the metabolic hormones ghrelin and leptin) were analyzed similarly to total energy expenditure. For analysis, we log transformed the concentrations of the hormones and triglycerides. For reporting, we retransformed the adjusted mean and standard error to the original units (exp(mean log) ±exp(mean log)×(exp(SE log)–1)), and changes were expressed in percentage units (100%×(exp(change in log)–1)).
Analysis was performed on the full intention-to-treat sample and a per protocol subset comprising those participants who maintained weight loss within 2 kg of the start of trial weight during the test phase, the latter potentially providing a more precise effect estimate. After each analysis, we examined residual patterns to detect outliers or other departures from assumptions of the statistical model.
Recognizing that estimates of food quotient introduce some imprecision when calculating total energy expenditure, due in part to uncertainty in estimates of metabolizable energy,41 we conducted sensitivity analyses to determine how plausible errors in food quotient could influence results. To test for selective dropout, we compared pre-weight loss characteristics of participants who completed the end of the test phase assessment with those who did not. To fully assess the influence of missing data (dropouts and unusable data points), we performed an inverse probability weighted version of the primary analysis,42 constructing a logistic model for missingness and employing the fitted probabilities to assign weights in the primary analysis. We used SAS software version 9.4 for all computations (SAS Institute, Cary, NC).
Missing data and quality of fit
Two randomized participants were excluded from all analyses: one developed hypothyroidism and one provided unreliable data for doubly labeled water at the start of the trial and then withdrew before notification of diet assignment. Of 486 potential total energy expenditure values for use in the primary repeated measures analysis (162 participants×three time points), 457 were available (94%); for the per protocol analysis, 337 of 360 (94%) were available. The missing values were attributable to 24 missed doubly labeled water studies (nine during the midpoint of the test phase, and 15 at the end of the test phase) and five studies that yielded non-convergent curve fits or implausible parameters (one at the start of the trial, three during the midpoint of the test phase, and one at the end of the test phase). Neither the intention-to-treat nor the per protocol findings changed materially when we applied inverse probability weighting to compensate for the missing data. For secondary outcomes, the percentage of non-missing values varied between 94% (resting energy expenditure, physical activity, 459 of 486) and 95% (hormones, 460 of 486). Residual patterns showed a satisfactory fit to the repeated measures model in all cases, with no extreme outliers or pathological distributions.
Patient and public involvement
No patients were involved in setting the research question or the outcome measures, nor were they involved in developing plans for design or implementation of the study. No patients were asked to advise on interpretation or writing up of results. Study participants received a written summary of their clinically relevant results. We plan to invite study participants to Framingham State University for an oral presentation of findings after publication of the primary outcome. Information may be disseminated to the general public via any media coverage of study findings.
Results
Participants
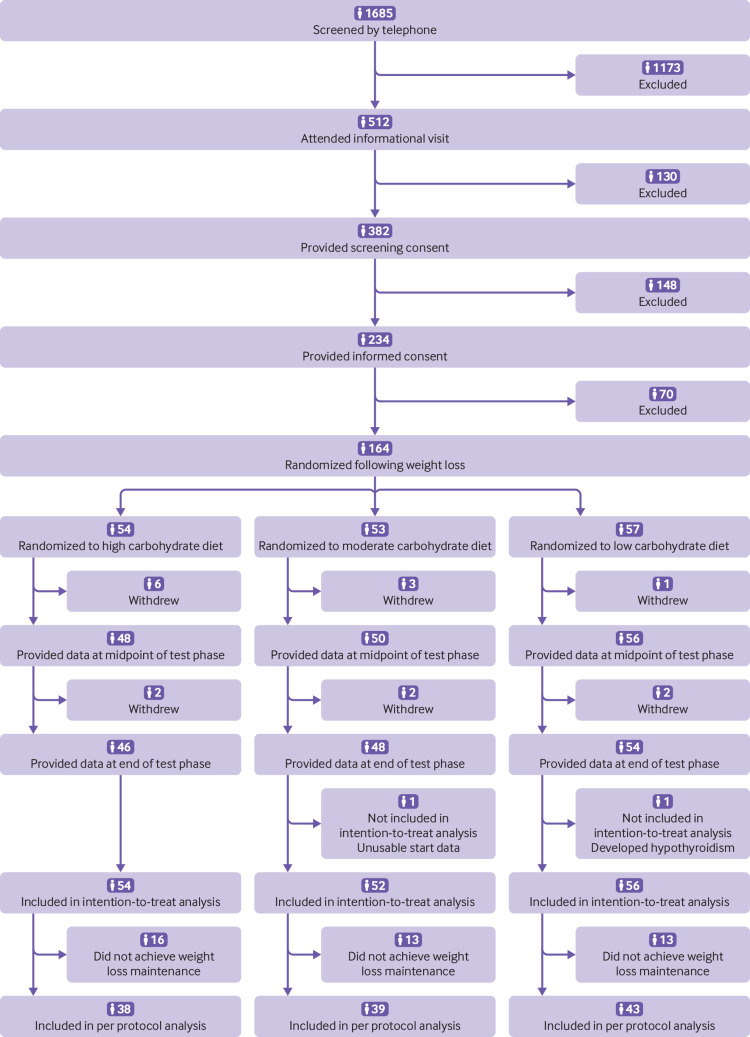
Of 1685 people screened, we enrolled 234 participants for the run-in phase (fig 2). Of these, 164 achieved 12% (within 2%) weight loss and were randomly assigned to one of three macronutrient diets for the test phase, comprising high (n=54), moderate (n=53), or low (n=57) levels of carbohydrate. Table 2 presents the characteristics of the randomized sample at the pre-weight loss time point. Each stratification factor in the randomization was balanced across the three diet groups according to Fisher’s exact test (P≥0.28). Among the 162 participants included in the intention-to-treat analysis, primary outcome data were available for 161 (99%) at the start of the trial, 150 (93%) at the midpoint of the test phase, and 146 (90%) at the end of the test phase.
Fig 2.
Participant flow (see supplementary figure for details of exclusions)
Table 2.
Pre-weight loss characteristics of 164 study participants by diet group. Values are means (standard deviations) unless stated otherwise
| Characteristics | Carbohydrate content | ||
|---|---|---|---|
| High (n=54) | Moderate (n=53) | Low (n=57) | |
| Men | 12 (22) | 17 (32) | 20 (35) |
| Women | 42 (78) | 36 (68) | 37 (65) |
| Hispanic ethnicity,* No (%) | 8 (15) | 7 (13) | 10 (18) |
| Race, No (%)*: | |||
| White | 44 (81) | 41 (77) | 43 (75) |
| Black | 4 (7) | 7 (13) | 6 (11) |
| Asian | 2 (4) | 2 (4) | 1 (2) |
| Unknown/other | 4 (7) | 3 (6) | 7 (12) |
| Age (years) | 39.8 (15.1) | 37.3 (14.9) | 37.1 (13.3) |
| Weight (kg) | 88.4 (16.6) | 94.8 (19.7) | 91.2 (17.9) |
| Weight loss (% of pre-weight loss) | 10.6 (1.7) | 10.5 (1.8) | 10.3 (1.6) |
| Height (cm) | 166.7 (9.0) | 167.9 (11.2) | 168.5 (9.8) |
| Body mass index | 31.7 (4.3) | 33.5 (5.3) | 32.0 (4.8) |
| Total energy expenditure (kcal/d) | 2915 (686) | 3030 (788) | 3110 (680) |
| Resting energy expenditure (kcal/d) | 1654 (318) | 1751 (387) | 1695 (331) |
| Physical activity: | |||
| Total physical activity (counts/d, 000s)† | 510.0 (172.1) | 509.1 (146.4) | 525.2 (182.4) |
| MVPA (min/d)‡ | 26.4 (19.4) | 27.7 (19.5) | 29.7 (19.8) |
| Sedentary time (min/d)§ | 567.2 (91.0) | 591.8 (105.4) | 566.1 (97.1) |
| Skeletal muscle work efficiency at 10 W (%) | 11.1 (2.5) | 10.3 (2.6) | 11.1 (3.6) |
| Ghrelin level (pg/mL) | 648.6 (293.7) | 530.0 (281.0) | 558.2 (288.3) |
| Leptin level (ng/mL) | 31.3 (16.4) | 30.6 (19.0) | 27.5 (16.4) |
| Body composition: | |||
| Body fat mass (% of total mass) | 41.4 (5.5) | 41.1 (7.3) | 40.0 (5.8) |
| Lean body mass (% of total mass)¶ | 56.0 (5.3) | 56.3 (7.0) | 57.3 (5.6) |
| Abnormal fasting blood glucose, No (%)** | 18 (33) | 19 (36) | 16 (28) |
| Fasting glucose (mg/dL) | 97 (9) | 97 (9) | 99 (11) |
| Fasting insulin (μIU/mL) | 13.9 (6.8) | 15.6 (10.3) | 19.7 (21.1) |
MVPA=moderate to vigorous physical activity.
Determined by self report using fixed categories. White: a person having origins in any of the original peoples of Europe, the Middle East, or North Africa. Black: a person having origins in any of the black racial groups of Africa. Asian: a person having origins in any of the original peoples of the Far East, Southeast Asia, or the Indian subcontinent.
Quantified based on triaxial counts, representing a composite vector magnitude of three orthogonal planes (vertical, anteroposterior, mediolateral).43 Average accelerometer wear time was mean 14.8 (SD 1.3) hours per day.
Quantified using vertical axis count thresholds of Troiano et al.44
Defined as <100 counts per minute for vertical axis counts.43
Lean body mass does not include bone mineral content.
Fasting blood glucose ≥100 mg/dL.
During the run-in phase, mean weight loss for randomly assigned participants was 9.6 kg (SD 2.5 kg), corresponding to 10.5% (SD 1.7%) of pre-weight loss body weight. There was no difference between diet groups in weight loss from pre-weight loss to the start of the trial (P=0.65) or absolute body weight at the start of the trial (P=0.18). Among the randomly assigned participants (for whom energy intake was adjusted as needed to maintain weight loss during the test phase), 120 had data for the primary outcome and remained within the target of 2 kg of their start of trial weight, comprising the per protocol group (74% of the 162 included in the intention-to-treat analysis for the primary outcome). Covariates did not differ between these participants and those who did not maintain weight loss, except for age which had marginal significance (see supplemental eTable 4). Covariates also did not differ between participants who completed the end of the test phase assessment and those who did not (data not shown). Body weight tracked strongly during the test phase, as indicated by high within participant correlations from the start of the trial to the midpoint of the test phase and end of the test phase (r≥0.99). On average, body weight changed by less than 1 kg during the test phase, with no significant difference by diet group in either the intention-to-treat (P=0.43) or per protocol (P=0.19) analysis.
Forty adverse events were recorded for 36 participants throughout the trial (see supplemental eTable 5). Two serious adverse events were reported: emergency hospital admission for removal of an intrauterine device (unrelated to study participation) and laparoscopic cholecystectomy (possibly related to study participation). The number of participants (n=13) who had an adverse event or serious adverse event after randomization did not differ by diet group (P=0.34).
Total energy expenditure
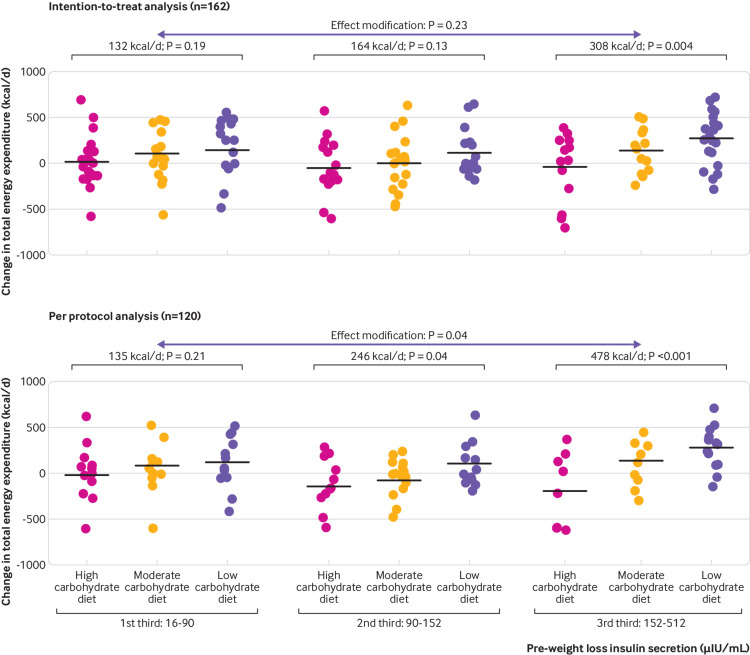
In the intention-to-treat analysis (n=162, P=0.002), total energy expenditure differed significantly by diet (fig 3, table 3), with a linear trend of 52 kcal/d (95% confidence interval 23 to 82) for every 10% decrease in the contribution of carbohydrate to total energy intake (1 kcal=4.18 kJ=0.00418 MJ). Compared with the high carbohydrate diet, change in total energy expenditure (mean, normalized to average start of trial body weight of 82 kg) was 91 kcal/d (95% confidence interval −29 to 210) greater on the moderate carbohydrate diet and 209 kcal/d (91 to 326) greater on the low carbohydrate diet. In the per protocol analysis (n=120, P<0.001) (fig 3), the respective differences were 131 kcal/d (−6 to 267) and 278 kcal/d (144 to 411). These results were similar with full adjustment for all prespecified covariates (sex, ethnicity, race, and age; pre-weight loss values for BMI, percentage lean mass, and total energy expenditure; and weight loss from pre-weight loss to the start of the trial): 76 kcal/d (−42 to 194) greater on the moderate carbohydrate diet and 185 kcal/d (69 to 302) greater on the low carbohydrate diet in the intention-to-treat analysis (P=0.008); and 111 kcal/d (−23 to 245) and 249 kcal/d (117 to 380) in the per protocol analysis (P=0.001). Supplemental eFigure 1 displays data on change at the individual level from the start of the trial through the test phase. Findings from both analyses remained materially unchanged with inverse probability weighting to compensate for missing data or when examining absolute total energy expenditure expressed in kcal/d. Total energy expenditure did not change significantly within any diet group between 10 and 20 weeks (P>0.43). Supplemental eTable 6 shows the relative insensitivity of total energy expenditure to the assumed value of food quotient, and eTable 7 shows the robustness of the observed effect of diet on total energy expenditure to substantial non-compliance.
Fig 3.
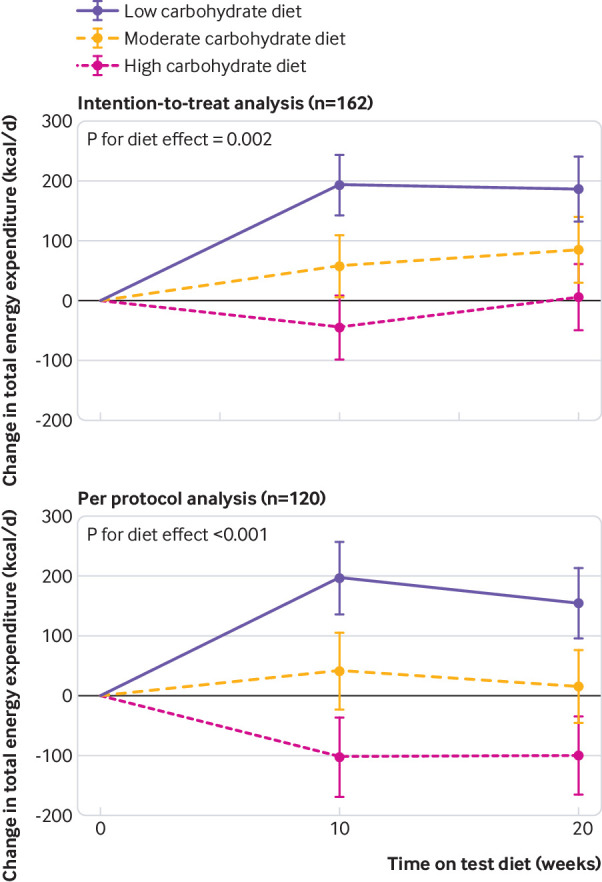
Change in total energy expenditure, the primary outcome, in intention-to-treat (top) and per protocol (bottom) analyses. Data are shown as mean change from start of test phase, with whiskers representing 1 standard error above and below the mean. P tests uniformity across diet groups for average of changes at midpoint and end of test phase
Table 3.
Primary and secondary outcomes involving energy expenditure, physical activity, and metabolic hormones*
| Variables | No | Mean (SD) pre-randomization start of trial | Change: average(midpoint of test phase, end of test phase)−start of trial | ||
|---|---|---|---|---|---|
| Mean (95% CI) | P value between groups | Trend estimate (95% CI)† | |||
| Primary outcome: total energy expenditure (kcal/d) | |||||
| Intention-to-treat: | |||||
| High | 54 | 2640 (62) | −19 (−104 to 66) | 0.002 | 52 (23 to 82) |
| Moderate | 52 | 2504 (65) | 71 (−12 to 155) | ||
| Low | 56 | 2713 (64) | 190 (109 to 270) | ||
| Per protocol: | |||||
| High | 38 | 2711 (77) | −102 (−201 to −2) | <0.001 | 69 (36 to 103) |
| Moderate | 39 | 2577 (72) | 29 (−64 to 123) | ||
| Low | 43 | 2758 (70) | 176 (87 to 265) | ||
| Resting energy expenditure (kcal/d) | |||||
| Intention-to-treat: | |||||
| High | 54 | 1603 (24) | 34 (10 to 57) | 0.47 | 5 (−3 to 13) |
| Moderate | 51 | 1576 (25) | 46 (23 to 69) | ||
| Low | 56 | 1615 (24) | 54 (32 to 76) | ||
| Per protocol: | |||||
| High | 38 | 1601 (28) | 20 (−8 to 48) | 0.18 | 8 (−1 to 18) |
| Moderate | 38 | 1597 (27) | 28 (2 to 54) | ||
| Low | 43 | 1608 (26) | 53 (28 to 78) | ||
| Total physical activity (counts/d, 000s)‡ | |||||
| Intention-to-treat: | |||||
| High | 54 | 476.6 (23.3) | −26.3 (−52.0 to −0.6) | 0.13 | 4.8 (−3.9 to 13.6) |
| Moderate | 52 | 463.8 (24.9) | −42.4 (−67.7 to −17.1) | ||
| Low | 55 | 495.8 (23.9) | −6.9 (−31.0 to 17.1) | ||
| Per protocol: | |||||
| High | 38 | 493.2 (28.8) | −29.1 (−59.0 to 0.7) | 0.17 | 4.4 (−5.6 to 14.3) |
| Moderate | 39 | 481.3 (27.0) | −48.3 (−76.3 to −20.3) | ||
| Low | 42 | 521.3 (26.3) | −11.6 (−38.2 to 14.9) | ||
| Moderate to vigorous intensity physical activity (min/d)§ | |||||
| Intention-to-treat: | |||||
| High | 54 | 31.6 (2.6) | −3.6 (−6.3 to −0.9) | 0.09 | 0.7 (−0.2 to 1.6) |
| Moderate | 52 | 31.3 (2.7) | −4.8 (−7.5 to −2.1) | ||
| Low | 55 | 30.0 (2.6) | −0.9 (−3.4 to 1.6) | ||
| Per protocol: | |||||
| High | 38 | 33.4 (3.0) | −4.3 (−7.4 to −1.1) | 0.06 | 0.9 (−0.1 to 2.0) |
| Moderate | 39 | 33.0 (2.8) | −5.2 (−8.1 to −2.2) | ||
| Low | 42 | 32.2 (2.8) | −0.5 (−3.3 to 2.3) | ||
| Sedentary time (min/d)¶ | |||||
| Intention-to-treat: | |||||
| High | 54 | 592.1 (14.2) | 8.6 (−7.7 to 25.0) | 0.12 | −2.7 (−8.3 to 2.9) |
| Moderate | 52 | 604.7 (14.8) | 20.9 (4.8 to 37.0) | ||
| Low | 55 | 597.0 (14.6) | −2.3 (−17.6 to 13.0) | ||
| Per protocol: | |||||
| High | 38 | 593.6 (17.2) | 2.1 (−17.7 to 22.0) | 0.31 | 0.9 (−5.8 to 7.5) |
| Moderate | 39 | 611.0 (16.1) | 21.4 (2.8 to 40.0) | ||
| Low | 42 | 589.4 (15.7) | 5.6 (−12.0 to 23.1) | ||
| Skeletal muscle work efficiency at 10 W (%)** | |||||
| Intention-to-treat: | |||||
| High | 53 | 12.2 (0.3) | −0.1 (−0.8 to 0.5) | 0.66 | 0.1 (−0.1 to 0.3) |
| Moderate | 51 | 11.7 (0.4) | −0.0 (−0.6 to 0.6) | ||
| Low | 55 | 12.2 (0.3) | 0.3 (−0.3 to 0.9) | ||
| Per protocol: | |||||
| High | 38 | 12.1 (0.4) | −0.1 (−0.9 to 0.6) | 0.46 | 0.1 (−0.1 to 0.4) |
| Moderate | 38 | 11.9 (0.4) | −0.0 (−0.7 to 0.6) | ||
| Low | 42 | 12.2 (0.4) | 0.5 (−0.2 to 1.1) | ||
| Ghrelin (pg/mL and % change)†† | |||||
| Intention-to-treat: | |||||
| High | 54 | 693.2 (51.4) | -4.9 (−8.4 to −1.2) | 0.02 | −1.9 (−3.2 to −0.6) |
| Moderate | 51 | 640.1 (49.9) | −8.7 (−12.0 to −5.3) | ||
| Low | 56 | 598.2 (45.4) | −11.8 (−14.8 to −8.6) | ||
| Per protocol: | |||||
| High | 38 | 689.5 (63.0) | −5.9 (−10.1 to −1.5) | 0.02 | −2.1 (−3.7 to −0.6) |
| Moderate | 38 | 620.6 (52.8) | −8.0 (−11.8 to −4.0) | ||
| Low | 43 | 603.0 (49.0) | −13.5 (−16.9 to −10.0) | ||
| Leptin (ng/mL and % change)†† | |||||
| Intention-to-treat: | |||||
| High | 54 | 10.9 (1.6) | 34.2 (21.8 to 47.7) | 0.07 | −3.3 (−6.8 to 0.1) |
| Moderate | 51 | 9.8 (1.5) | 34.8 (22.6 to 48.2) | ||
| Low | 56 | 9.6 (1.4) | 17.9 (7.7 to 29.1) | ||
| Per protocol: | |||||
| High | 38 | 11.8 (2.2) | 47.6 (33.9 to 62.8) | 0.009 | −4.9 (−8.4 to −1.5) |
| Moderate | 38 | 8.6 (1.5) | 42.0 (29.4 to 55.8) | ||
| Low | 43 | 9.0 (1.5) | 21.9 (11.7 to 33.0) | ||
Means and changes were constructed and compared from repeated measures analysis of variance, unadjusted except for structural design variables (study site, cohort, enrolment wave).
Linear trend across diet groups for every 10% decrease in the contribution of carbohydrate to total energy intake. Estimates are equivalent to comparing the high with low carbohydrate diet, divided by 4 (with these two diet groups differing in carbohydrate by 40%).
Quantified based on triaxial counts, representing a composite vector magnitude of three orthogonal planes (vertical, anteroposterior, mediolateral).43 Average accelerometer wear time was mean 14.9 (SD 1.2) hours per day.
Quantified using vertical axis count thresholds of Troiano et al.44
Defined as <100 counts per minute for vertical axis counts.43
Efficiency is expressed as percentage ratio of power generated (with conversion of Watts to kcal/min using a factor of 0.01433) to energy expenditure above resting (kcal/min).45 46 Data not collected at midpoint of test phase. Change: end of test phase−start of trial. There were no significant group effects at 10 W (presented here), 25 W, and 50 W.
Hormone levels were log transformed for analysis. For reporting, the adjusted mean and standard error were retransformed to the original units (exp(mean log)±exp(mean log)×(exp(SE log)–1)), and changes were expressed in percentage units (100%×(exp(change in log)–1)).
The effect of dietary composition on total energy expenditure was most pronounced among those with high insulin secretion at pre-weight loss (fig 4). Among participants in the highest third of insulin concentration 30 minutes after oral glucose, the difference between low versus high carbohydrate diet was 308 kcal/d (101 to 514) in the intention-to-treat analysis and 478 kcal/d (232 to 724) in the per protocol analysis, with significant effect modification in the per protocol analysis. When evaluating effect modification by fasting glucose, insulin concentration, or insulin resistance, we observed similar but less strong patterns, with those in the highest thirds of pre-weight loss values for these characteristics showing the largest difference between diet groups (see supplemental eFigures 2 to 4).
Fig 4.
Effect modification by pre-weight loss insulin secretion (insulin concentration 30 minutes after oral glucose) in intention-to-treat and per protocol analyses. Pre-weight loss body weight differed by third (first third, 83.8 kg; second third, 92.8 kg; third third 98.4 kg, P<0.001 in the intention-to-treat analysis). Change in body weight during the test phase did not differ by third (P=0.08) or across diet groups (P=0.43)
Other outcomes
We assessed energy intake during the test phase among participants in the per protocol analysis, providing an estimate of energy requirements during weight loss maintenance. Although estimates of energy intake are less accurate and precise than total energy expenditure47 (and our methods would tend to selectively underestimate those with high energy expenditure, as considered in the supplemental methods), the results are generally consistent with the findings for total energy expenditure. Compared with levels at the start of the trial, energy intake changed in participants assigned to the high, moderate, and low carbohydrate test diets, respectively: 139 kcal/d (−4 to 282), 175 kcal/d (42 to 308), and 269 kcal/d (143 to 396), with an overall P=0.36. These differences strengthened among participants in the highest third of insulin secretion: 37 kcal/d (−249 to 323), −24 kcal/d (−293 to 245), and 340 kcal/d (132 to 548), with an overall P=0.05.
Resting energy expenditure, total physical activity, and moderate to vigorous intensity physical activity were marginally higher in the group assigned to the low carbohydrate diet (group differences or linear trends of borderline significance), with contrasting within group changes in some cases; whereas sedentary time and skeletal muscle work efficiency did not differ by diet (table 3). Ghrelin (intention-to-treat and per protocol analyses) and leptin (per protocol analysis only) differed significantly by diet. Ghrelin showed a steeper decline over the test phase in participants assigned to the low carbohydrate compared with high carbohydrate diet, and leptin showed a lesser incline.
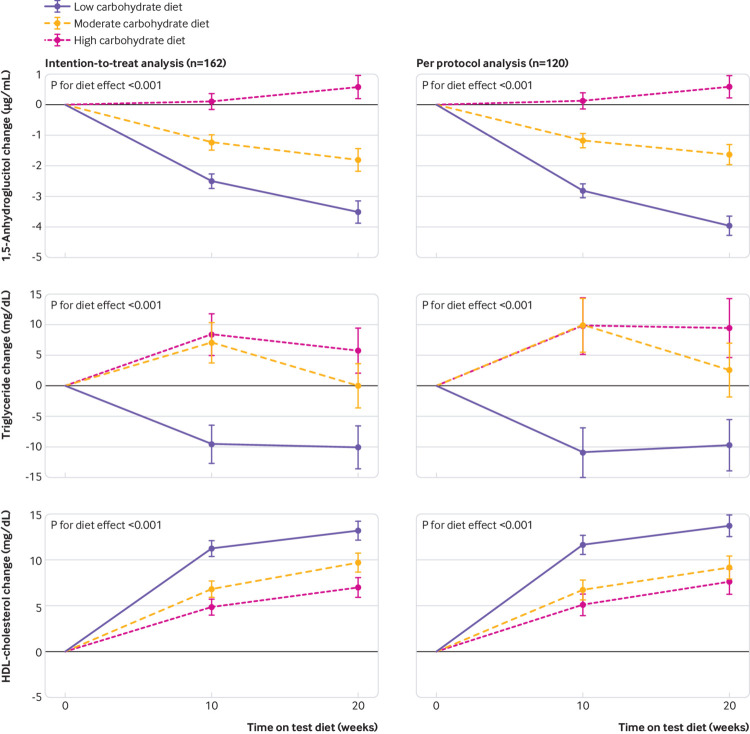
Process measures and biomeasures of compliance
Attention to treatment fidelity, as previously described,20 encompassed differentiation and consistency in the design of the diets (table 1) and integrity in the preparation of the diets. To monitor integrity, we carried out spot weight checks, comparing actual weight with target weight of menu items and documenting that 98% (743 of 760) were within 5 g (a level of deviation that would not compromise macronutrient differentiation). We found strong differentiation of 1,5-anhydroglucitol (a biomeasure of carbohydrate intake, see supplemental methods) among diet groups, ranging from lowest in those assigned to the low carbohydrate diet to highest in those assigned to the high carbohydrate diet (P<0.001; fig 5). Also, as expected, triglyceride levels increased with increasing carbohydrate content (P<0.001), whereas levels of high density lipoprotein cholesterol decreased (P<0.001).
Fig 5.
Biomeasures of compliance in intention-to-treat and per protocol analyses. Measures include 1,5-anhydroglucitol (upper), mean pre-weight loss value 17 μg/mL; triglycerides (middle), mean pre-weight loss value 78 mg/dL (retransformed); and high density lipoprotein cholesterol (lower), mean pre-weight loss value 48 mg/dL. Data are shown as mean change from start of test phase, with whiskers representing 1 standard error above and below the mean. P tests uniformity across diet groups for average of changes at midpoint and end of test phase. Left, intention-to-treat analysis; right, per-protocol analysis
Discussion
In this controlled feeding trial over 20 weeks, we found that total energy expenditure was significantly greater in participants assigned to a low carbohydrate diet compared with high carbohydrate diet of similar protein content. In addition, pre-weight loss insulin secretion might modify individual response to this diet effect. Taken together with preliminary reports on activation of brain areas involved in food cravings48 and circulating metabolic fuel concentration,49 results of the current Framingham State Food Study (FS)2 substantiate several key predictions of the carbohydrate-insulin model. Regardless of the specific mechanisms involved, the study shows that dietary quality can affect energy expenditure independently of body weight, a phenomenon that could be key to obesity treatment, as recently reviewed.50
The difference in total energy expenditure was 209 to 278 kcal/d or about 50 to 70 kcal/d increase for every 10% decrease in the contribution of carbohydrate to total energy intake (1 kcal=4.18 kJ=0.00418 MJ). This effect is comparable to that obtained by isotopic methods over one month intervention periods in a previous randomized crossover study with 21 adults39 and in a non-randomized crossover study with 17 men,51 after taking into account confounding by ongoing weight loss and other sources of bias.52 53 If this effect persisted—and we observed no attenuation from 10 to 20 weeks—it would translate into an estimated 10 kg weight loss after three years for a typical 30 year old man of height 178 cm, baseline weight 100 kg, and average activity level, assuming no change in energy intake (www.niddk.nih.gov/bwp). If reduction of glycemic load also decreased hunger and food intake,3 6 the long term benefits could be even greater.
The difference in total energy expenditure between low and high carbohydrate diets among those in the highest third of insulin secretion was more than double the difference for those with low insulin secretion, highlighting a subgroup who could do particularly well with restriction of total or high glycemic load carbohydrates. This finding is consistent with results from an animal study,54 a cohort study,55 mendelian randomization analysis,56 and clinical trials.30 31 57 In contrast, the recent DIETFITS (Diet Intervention Examining The Factors Interacting with Treatment Success) trial reported no effect modification by insulin secretion or genetic factors among 609 overweight adults assigned to low fat compared with low carbohydrate diets for 12 months.58 In that study, however, which relied on nutrition education and behavioral counseling, participants were instructed to “minimize or eliminate refined grains and added sugars and maximize intake of vegetables” and other minimally processed foods. Probably for this reason, the reported glycemic load of the low fat diet was very low for a diet that is by nature higher in total carbohydrate, and similar to the value for the lowest glycemic load diets in some previous intervention studies.59 Thus, the effects of predisposing risk factors might be attenuated on diets that are generally healthy and specifically low in glycemic load. In support of this possibility, a high genetic risk score for obesity predicted obesity among people consuming high glycemic load sugary beverages but not among non-consumers.60
Similar to our previous crossover study,39 the difference in total energy expenditure between diets was not primarily attributable to resting energy expenditure or physical activity level, which were marginally higher in participants assigned to the low carbohydrate diet (comparisons that could have been underpowered). Other potentially contributory components of energy expenditure include thermic effect of food, activity of brown adipose tissue, autonomic tone, nutrient cycling, fidgeting and related non-exercise activity thermogenesis,61 and changes in the efficiency of movement that we did not capture with cycle ergometry.45 46 62 63
A change in metabolism is suggested by hormonal responses to diet. Ghrelin, produced primarily in the stomach, was significantly lower in participants assigned to the low carbohydrate diet, a novel finding. Beyond effects on hunger, ghrelin has been reported to lower energy expenditure and promote fat deposition,64 65 providing another mechanistic explanation for our primary outcome. Leptin (an adipocyte hormone that signals body energy stores) was also lower in participants assigned to the low carbohydrate diet, suggesting improvement in leptin sensitivity.66 Prospective studies have observed that people with the greatest declines in leptin levels after weight loss have the lowest risk for weight regain.67 68 69
Strengths and limitations of this study
(FS)2 is a large controlled feeding study among free living participants and has several strengths: a sufficient duration of intervention to avoid confounding by transient metabolic adaptations to changes in macronutrient content15 16 17 18; the power to achieve a relatively precise effect estimate for the primary outcome; biomeasures showing substantial and sustained differentiation between diets (findings not characteristically observed in trials relying on nutrition education and behavioral counseling)70; measurement of total energy expenditure by the doubly labeled water method, the gold standard method for studies of free living people32 33 34 35; control for dietary protein and body weight, minimizing confounding by other potentially significant influences on total energy expenditure; and design of diets to reflect realistic and healthful examples of their respective macronutrient compositions.
The study has three main limitations, including potential measurement error, non-compliance, and generalizability. Firstly, measurement of total energy expenditure by the doubly labeled water method involves several assumptions, most notably that food quotient (reflecting dietary composition) equals respiratory quotient (reflecting the ratio of macronutrients oxidized). This assumption is generally valid during weight maintenance.28 Reassuringly, potential errors in estimation of food quotient would have only a modest effect, with a 0.01 shift in food quotient equating to about 1% change in total energy expenditure (see supplemental eTable 6). Results for the primary outcome remained robust throughout a range of plausible respiratory quotient values in sensitivity analyses (eTable 7). Additional evidence for the validity of our primary outcome derives from the effect modification, as there would be no reason why any systematic error in total energy expenditure should co-segregate with measures of insulin secretion and insulin resistance in the observed fashion.
Some investigators recently proposed a novel reason why the doubly labeled water method—used extensively in nutrition research for decades—would bias comparisons among diets varying in macronutrient ratio. According to this argument, presented in a post hoc analysis of an observational pilot study,71 increased de novo lipogenesis on a high carbohydrate diet could trap deuterium, leading to a lower total energy expenditure with doubly labeled water compared with whole room calorimetry that is artefactual. Concern arose from studies of pigs consuming an extremely high carbohydrate diet (90% of total energy intake) during their most rapid growth phase, gaining up to 0.65 kg per day.72 In this exceptional scenario, significant error could arise in estimates of total energy expenditure; however, statistical extrapolation predicted no error during weight maintenance. During weight maintenance in humans, rates of hepatic de novo lipogenesis are low on whole food, low sugar diets with carbohydrate intake up to 75% (substantially higher than our high carbohydrate diet, which was also low in sugar).73 74 Even with consumption of 50% excess carbohydrate, hepatic de novo lipogenesis was less than 5 g/d.75
Some76 but not all77 studies report moderate rates of de novo lipogenesis in adipose tissue, but it is not known how dietary composition might differentially affect this phenomenon. Indeed, adipocyte lipogenesis seems to be poorly responsive to changes in dietary carbohydrate,78 79 and high intakes of carbohydrate might not affect adipose gene expression or lipogenic activity during weight stability80 81 or after weight loss,82 as opposed to massive overfeeding.83 84 Moreover, a carefully controlled validation study reported that the doubly labeled water method was more accurate than whole room calorimetry, which tends to underestimate adaptive thermogenesis.85 Determination of total energy expenditure by doubly labeled water (but not whole room calorimetry) with 10% weight gain or loss corresponded closely with titration of energy requirements, suggesting that changes in metabolism after major perturbations of adipose tissue do not confound isotopic measurements. Thus, any bias of dietary composition on the accuracy of the doubly labeled water method during weight maintenance is highly speculative and unlikely to be meaningful.
We considered our protocol too long to be logistically practical or financially feasible for an inpatient setting. Instead, we provided participants with fully prepared meals, and implemented strategies to promote compliance with the assigned diets.20 Despite these efforts, we recognize that non-compliance could have occurred, especially among those whose weight deviated beyond the prespecified definition of weight loss maintenance. However, this second limitation unlikely presented a threat to study integrity because sensitivity analysis showed robustness of the diet effect on total energy expenditure to substantial degrees of non-compliance, even with extreme assumptions (that any additional energy consumed on the low carbohydrate diet came from foods with macronutrients reflecting the high carbohydrate diet) (see supplemental eTables 6 and 7). Further, the primary outcome was strengthened in the per protocol analysis, including only participants who maintained weight loss throughout the test phase. By excluding those with objective evidence of non-compliance, the per protocol analysis should provide a more accurate estimate of the true diet effects.
The third limitation of our study is translation of findings from feeding studies to public health recommendations. However, aspects of the study design improve generalizability, including provision of food in the pragmatic setting of a university in collaboration with a food service contractor. More broadly, these results must be reconciled with the long term weight loss trials relying on nutrition education and behavioral counseling that find only a small advantage for low carbohydrate compared with low fat diets according to several recent meta-analyses.86 87 88 89 90 91 But inferences about efficacy from these trials are limited by characteristically poor long term compliance and lack of differentiation in dietary intake between groups, reflecting the difficulty of behavior change in the modern food environment. Furthermore, our study cannot prove that changes in carbohydrate to fat ratio alone mediate study findings. Although we constructed test diets as similar as possible (eg, controlling for protein content, amount of non-starchy vegetables, the ratio of saturated fat to total fat), unrecognized dietary factors could have contributed to the observed effects. This possibility, of relevance to translation, requires exploration in future mechanistically oriented research.
Conclusions and policy implications
Dietary composition seems to affect energy expenditure independently of body weight. A low glycemic load, high fat diet might facilitate weight loss maintenance beyond the conventional focus on restricting energy intake and encouraging physical activity. Additional research is warranted to examine the effects of glycemic load on body weight, with control of energy intake; to compare diets aiming to reduce glycemic index at prevailing carbohydrate levels (eg, the DIETFITS lower fat diet) compared with restricting total carbohydrate; to explore subgroup susceptibility based on insulin secretion and other biological factors; to determine whether extreme carbohydrate restriction (eg, with a ketogenic diet) confers unique advantages for obesity or specific conditions such as diabetes; and to explore the mechanisms relating dietary composition to energy expenditure. If metabolic benefits of reduced glycemic load diets are confirmed, development of appropriate behavioral and environmental interventions would be necessary for optimal translation to public health.
What is already known on this topic
Energy expenditure declines with weight loss, predisposing to weight regain
Little is, however, known about how dietary composition influences this adaptive metabolic response over the long term
What this study adds
A low carbohydrate diet could increase energy expenditure during weight loss maintenance
This metabolic effect could improve the effectiveness of obesity treatment
Acknowledgments
We thank the study participants for their time and commitment to advancing science; study nurses who conducted oral glucose tolerance tests; Framingham State University students who served as research assistants; consultants Helen Rasmussen (Tufts University), Janis Swain (Brigham and Women’s Hospital), and Jeff Volek (The Ohio State University); study safety officer Michael Agus (Boston Children’s Hospital); Boston Children’s Hospital research staff Teri Allers, Rachel Apone, Michaela Barhite, Gary Bradwin, Carissa Burton, Emily Caplan, Nicole Chenard, Kimberly Chin, Courtenay Devlin, Jillian Fergione, Maria Khan, Lesley Levitt, Amanda Gonsalves, Veronica Gragnano, Tessa Graham, Shannon Hourigan, Bridget Hron, Paul Lakin, Meghan Leary, Ethan Litman, Catherine Matero, Marlee McGurl, Carly Milliren, Anne Nero, Victoria Ravenelle, Lisa Robinson, Adrienne Salisbury, Megan Sandman, Amanda Scott, Linda Seger-Shippee, Kim Shimy, Kaitlyn Shannon, Rachael Sharpe, Caitlin Shaughnessy, Daniele Skopek, Tram Anh Tran, Benjamin Trapp, and Emma van Emmerik; Framingham State University employee Denise Harney; Sodexo employees David Garufi, Renae Gauvin, Carolyn Holland, Darline Hughes, Eric Johnson, Lauren Stone, and Denise Stultz; Assabet Valley Regional Technical High School employees Danielle Gervais, Jon Thering, Kelsey Viera, and Dina Wiroll; Baylor College of Medicine employee Zhensheng Chen; and SetPoint Health staff David Blackburn, Rob O’Neill, and Kristina Spellman for designing a study web portal.
We also thank faculty and staff of Boston Children’s Hospital, Framingham State University, and Sodexo who helped in establishing protocols as members of the Administrative, Recruitment, Assessment, and Intervention Workgroups; Framingham State University leadership Rita Colucci, Susanne Conley, Dale Hamel, Jonathan Lee, Daniel Magazu, and Linda Vaden-Goad for support throughout study design and execution; Sodexo leadership Ralph Eddy, Elizabeth Olson, and Beth Winthrop for help planning and conducting the dietary interventions; Assabet Valley Regional Vocational School District leadership Ernest F Houle and Kristopher Luoto for the opportunity to establish a satellite feeding site on campus; Jeffrey Flier (Harvard Medical School) and Steven Heymsfield (Pennington Biomedical Research Center) for critical review of the manuscript; and Marc Hellerstein (University of California at Berkeley) for providing expert opinion on de novo lipogenesis and related metabolic issues.
Web extra.
Extra material supplied by authors
Supplemental information: additional material
Supplemental information: figure 2 with full details of exclusions
Contributors: CBE (principal investigator) designed the study, secured funding, interpreted the data, and wrote the first draft of the manuscript. HAF (co-investigator, biostatistician) designed the study, and analyzed and interpreted the data. GLK (study director) acquired the data. JMWW (associate study director) calculated the diets and acquired the data. LB (nutrition research manager) calculated the diets and managed the dietary intervention. SKS (data and quality manager) performed randomization and monitored quality control of data acquisition. PKL (study director for Framingham State University) maintained partnerships. RRW (consultant) provided expertise on stable isotope modeling. WWW (co-investigator) conducted isotope-ratio mass spectrometry. DSL (principal investigator) designed the study, secured funding, interpreted the data, and wrote the first draft of the manuscript. CBE and DSL are the guarantors. CBE, HAF, and DSL had access to all of the data (including statistical reports and tables) in the study, take responsibility for the integrity of the data and the accuracy of the data analysis. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding: This work was conducted with grants from Nutrition Science Initiative (made possible by gifts from the Laura and John Arnold Foundation and Robert Lloyd Corkin Charitable Foundation), New Balance Foundation, Many Voices Foundation, and Blue Cross Blue Shield. DSL was supported by a mid-career mentoring award from the National Institute of Diabetes and Digestive and Kidney Diseases (K24DK082730). Nutrition Science Initiative monitored study progress and was given an opportunity to comment on the manuscript. The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; approval of the manuscript; and decision to submit the manuscript for publication. The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the study sponsors.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare: research support for the submitted work as described above; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work except as follows: CBE and DSL have conducted research studies examining the carbohydrate-insulin model funded by the National Institutes of Health and philanthropic organizations unaffiliated with the food industry; DSL received royalties for books on obesity and nutrition that recommend a low glycemic load diet.
Ethical approval: The study protocol was approved by the institutional review board at Boston Children’s Hospital.
Data sharing: The full dataset and statistical codes are available at Open Science Framework (https://osf.io/rvbuy/).
Transparency: The manuscript’s guarantors (CBE and DSL) affirm that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned and registered have been explained.
References
- 1. Maclean PS, Bergouignan A, Cornier MA, Jackman MR. Biology’s response to dieting: the impetus for weight regain. Am J Physiol Regul Integr Comp Physiol 2011;301:R581-600. 10.1152/ajpregu.00755.2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Leibel RL, Rosenbaum M, Hirsch J. Changes in energy expenditure resulting from altered body weight. N Engl J Med 1995;332:621-8. 10.1056/NEJM199503093321001 [DOI] [PubMed] [Google Scholar]
- 3. Ludwig DS. The glycemic index: physiological mechanisms relating to obesity, diabetes, and cardiovascular disease. JAMA 2002;287:2414-23. 10.1001/jama.287.18.2414 [DOI] [PubMed] [Google Scholar]
- 4. Ludwig DS, Friedman MI. Increasing adiposity: consequence or cause of overeating? JAMA 2014;311:2167-8. 10.1001/jama.2014.4133 [DOI] [PubMed] [Google Scholar]
- 5. Taubes G. The science of obesity: what do we really know about what makes us fat? An essay by Gary Taubes. BMJ 2013;346:f1050. 10.1136/bmj.f1050 [DOI] [PubMed] [Google Scholar]
- 6. Ludwig DS, Ebbeling CB. The Carbohydrate-Insulin Model of Obesity: Beyond “Calories In, Calories Out”. JAMA Intern Med 2018;178:1098-103. 10.1001/jamainternmed.2018.2933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lennerz B, Lennerz JK. Food addiction, high-glycemic-index carbohydrates, and obesity. Clin Chem 2018;64:64-71. 10.1373/clinchem.2017.273532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ford ES, Dietz WH. Trends in energy intake among adults in the United States: findings from NHANES. Am J Clin Nutr 2013;97:848-53. 10.3945/ajcn.112.052662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ludwig DS. Lowering the bar on the low-fat diet. JAMA 2016;316:2087-8. 10.1001/jama.2016.15473 [DOI] [PubMed] [Google Scholar]
- 10. Hall KD. A review of the carbohydrate-insulin model of obesity. Eur J Clin Nutr 2017;71:323-6. 10.1038/ejcn.2016.260 [DOI] [PubMed] [Google Scholar]
- 11. Hall KD, Guo J. Obesity energetics: body weight regulation and the effects of diet composition. Gastroenterology 2017;152:1718-27.e3. 10.1053/j.gastro.2017.01.052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Howell S, Kones R. “Calories in, calories out” and macronutrient intake: the hope, hype, and science of calories. Am J Physiol Endocrinol Metab 2017;313:E608-12. 10.1152/ajpendo.00156.2017 [DOI] [PubMed] [Google Scholar]
- 13. Schwartz MW, Seeley RJ, Zeltser LM, et al. Obesity pathogenesis: an Endocrine Society scientific statement. Endocr Rev 2017;38:267-96. 10.1210/er.2017-00111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bosy-Westphal A, Hägele F, Nas A. Impact of dietary glycemic challenge on fuel partitioning. Eur J Clin Nutr 2017;71:327-30. 10.1038/ejcn.2016.230 [DOI] [PubMed] [Google Scholar]
- 15. Owen OE, Caprio S, Reichard GA, Jr, Mozzoli MA, Boden G, Owen RS. Ketosis of starvation: a revisit and new perspectives. Clin Endocrinol Metab 1983;12:359-79. 10.1016/S0300-595X(83)80046-2 [DOI] [PubMed] [Google Scholar]
- 16. Vazquez JA, Adibi SA. Protein sparing during treatment of obesity: ketogenic versus nonketogenic very low calorie diet. Metabolism 1992;41:406-14. 10.1016/0026-0495(92)90076-M [DOI] [PubMed] [Google Scholar]
- 17. Yang MU, Van Itallie TB. Composition of weight lost during short-term weight reduction. Metabolic responses of obese subjects to starvation and low-calorie ketogenic and nonketogenic diets. J Clin Invest 1976;58:722-30. 10.1172/JCI108519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Phinney SD, Bistrian BR, Wolfe RR, Blackburn GL. The human metabolic response to chronic ketosis without caloric restriction: physical and biochemical adaptation. Metabolism 1983;32:757-68. 10.1016/0026-0495(83)90105-1 [DOI] [PubMed] [Google Scholar]
- 19. Ebbeling CB, Klein GL, Luoto PK, et al. A randomized study of dietary composition during weight-loss maintenance: Rationale, study design, intervention, and assessment. Contemp Clin Trials 2018;65:76-86. 10.1016/j.cct.2017.12.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Wong JM, Bielak L, Eddy RG, et al. An academia-industry partnership for planning and executing a community-based feeding study. Curr Dev Nutr 2018;2:nzy060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Institute of Medicine Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids. The National Academies Press, 2002. [DOI] [PubMed] [Google Scholar]
- 22. Halton TL, Hu FB. The effects of high protein diets on thermogenesis, satiety and weight loss: a critical review. J Am Coll Nutr 2004;23:373-85. 10.1080/07315724.2004.10719381 [DOI] [PubMed] [Google Scholar]
- 23. Frankenfield D, Roth-Yousey L, Compher C. Comparison of predictive equations for resting metabolic rate in healthy nonobese and obese adults: a systematic review. J Am Diet Assoc 2005;105:775-89. 10.1016/j.jada.2005.02.005 [DOI] [PubMed] [Google Scholar]
- 24. Mifflin MD, St Jeor ST, Hill LA, Scott BJ, Daugherty SA, Koh YO. A new predictive equation for resting energy expenditure in healthy individuals. Am J Clin Nutr 1990;51:241-7. 10.1093/ajcn/51.2.241 [DOI] [PubMed] [Google Scholar]
- 25.World Health Organization. Human Energy Requirements: Report of a Joint FAO/WHO/UNU Expert Consultation, Rome, Italy, 17-24 October 2001: United Nations, 2004:96. http://www.who.int/nutrition/publications/nutrientrequirements/9251052123/en/
- 26. Wolever TM, Jenkins DJ. The use of the glycemic index in predicting the blood glucose response to mixed meals. Am J Clin Nutr 1986;43:167-72. 10.1093/ajcn/43.1.167 [DOI] [PubMed] [Google Scholar]
- 27. Atkinson FS, Foster-Powell K, Brand-Miller JC. International tables of glycemic index and glycemic load values: 2008. Diabetes Care 2008;31:2281-3. 10.2337/dc08-1239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Black AE, Prentice AM, Coward WA. Use of food quotients to predict respiratory quotients for the doubly-labelled water method of measuring energy expenditure. Hum Nutr Clin Nutr 1986;40:381-91. [PubMed] [Google Scholar]
- 29. Eisenstein J, Roberts SB, Dallal G, Saltzman E. High-protein weight-loss diets: are they safe and do they work? A review of the experimental and epidemiologic data. Nutr Rev 2002;60:189-200. 10.1301/00296640260184264 [DOI] [PubMed] [Google Scholar]
- 30. Ebbeling CB, Leidig MM, Feldman HA, Lovesky MM, Ludwig DS. Effects of a low-glycemic load vs low-fat diet in obese young adults: a randomized trial. JAMA 2007;297:2092-102. 10.1001/jama.297.19.2092 [DOI] [PubMed] [Google Scholar]
- 31. Hron BM, Ebbeling CB, Feldman HA, Ludwig DS. Relationship of insulin dynamics to body composition and resting energy expenditure following weight loss. Obesity (Silver Spring) 2015;23:2216-22. 10.1002/oby.21213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Lam YY, Ravussin E. Analysis of energy metabolism in humans: A review of methodologies. Mol Metab 2016;5:1057-71. 10.1016/j.molmet.2016.09.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Schoeller DA. Recent advances from application of doubly labeled water to measurement of human energy expenditure. J Nutr 1999;129:1765-8. 10.1093/jn/129.10.1765 [DOI] [PubMed] [Google Scholar]
- 34. Wong WW. 90th Anniversary Commentary: Measurement of Energy Expenditure in Free-Living Humans by Using Doubly Labeled Water. J Nutr 2018;148:1660-2. 10.1093/jn/nxy107 [DOI] [PubMed] [Google Scholar]
- 35. Wong WW, Roberts SB, Racette SB, et al. The doubly labeled water method produces highly reproducible longitudinal results in nutrition studies. J Nutr 2014;144:777-83. 10.3945/jn.113.187823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Wong WW, Lee LS, Klein PD. Deuterium and oxygen-18 measurements on microliter samples of urine, plasma, saliva, and human milk. Am J Clin Nutr 1987;45:905-13. 10.1093/ajcn/45.5.905 [DOI] [PubMed] [Google Scholar]
- 37. Ravussin E, Harper IT, Rising R, Bogardus C. Energy expenditure by doubly labeled water: validation in lean and obese subjects. Am J Physiol 1991;261:E402-9. [DOI] [PubMed] [Google Scholar]
- 38. Ravussin E, Bogardus C. Relationship of genetics, age, and physical fitness to daily energy expenditure and fuel utilization. Am J Clin Nutr 1989;49(Suppl):968-75. 10.1093/ajcn/49.5.968 [DOI] [PubMed] [Google Scholar]
- 39. Ebbeling CB, Swain JF, Feldman HA, et al. Effects of dietary composition on energy expenditure during weight-loss maintenance. JAMA 2012;307:2627-34. 10.1001/jama.2012.6607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Bender R, Lange S. Adjusting for multiple testing--when and how? J Clin Epidemiol 2001;54:343-9. 10.1016/S0895-4356(00)00314-0 [DOI] [PubMed] [Google Scholar]
- 41. Sánchez-Peña MJ, Márquez-Sandoval F, Ramírez-Anguiano AC, Velasco-Ramírez SF, Macedo-Ojeda G, González-Ortiz LJ. Calculating the metabolizable energy of macronutrients: a critical review of Atwater’s results. Nutr Rev 2017;75:37-48. 10.1093/nutrit/nuw044 [DOI] [PubMed] [Google Scholar]
- 42. Seaman SR, White IR. Review of inverse probability weighting for dealing with missing data. Stat Methods Med Res 2013;22:278-95. 10.1177/0962280210395740 [DOI] [PubMed] [Google Scholar]
- 43. Chomistek AK, Yuan C, Matthews CE, et al. Physical activity assessment with the ActiGraph GT3X and doubly labeled water. Med Sci Sports Exerc 2017;49:1935-44. 10.1249/MSS.0000000000001299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc 2008;40:181-8. 10.1249/mss.0b013e31815a51b3 [DOI] [PubMed] [Google Scholar]
- 45. Baldwin KM, Joanisse DR, Haddad F, et al. Effects of weight loss and leptin on skeletal muscle in human subjects. Am J Physiol Regul Integr Comp Physiol 2011;301:R1259-66. 10.1152/ajpregu.00397.2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Goldsmith R, Joanisse DR, Gallagher D, et al. Effects of experimental weight perturbation on skeletal muscle work efficiency, fuel utilization, and biochemistry in human subjects. Am J Physiol Regul Integr Comp Physiol 2010;298:R79-88. 10.1152/ajpregu.00053.2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Park Y, Dodd KW, Kipnis V, et al. Comparison of self-reported dietary intakes from the Automated Self-Administered 24-h recall, 4-d food records, and food-frequency questionnaires against recovery biomarkers. Am J Clin Nutr 2018;107:80-93. 10.1093/ajcn/nqx002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Holsen L, Cerit H, Lennerz B, et al. Hypothalamic and nucleus accumbens cerebral blood flow vary as a function of long-term carbohydrate-to-fat ratio diets [abstract]. Neuropsychopharmacology (American College of Neuropsychopharmacology 56th Annual Meeting, Palm Springs) 2017;42:S150-1. https://www.nature.com/articles/npp2017264.pdf
- 49.Shimy K, Feldman HA, Klein GL, et al. A mechanistic examination of dietary composition on metabolic fuel availability [abstract].. Hormone Research in Paediatrics (10th International Joint Meeting of Pediatric Endocrinology; Washington DC) 2017;88(Suppl 1):S337. http://internationalmeeting2017.org/docs/ABSTRACTS_FINAL.pdf
- 50.Muller MJ, Geisler C, Heymsfield SB, et al. Recent advances in understanding body weight homeostasis in humans. F1000Res 2018;7:pii: F1000 Faculty Rev-1025. [DOI] [PMC free article] [PubMed]
- 51. Hall KD, Chen KY, Guo J, et al. Energy expenditure and body composition changes after an isocaloric ketogenic diet in overweight and obese men. Am J Clin Nutr 2016;104:324-33. 10.3945/ajcn.116.133561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Ludwig DS, Ebbeling CB. Raising the bar on the low-carbohydrate diet. Am J Clin Nutr 2016;104:1487-8. 10.3945/ajcn.116.142182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Friedman MI, Appel S. Energy expenditure and body composition changes after an isocaloric ketogenic diet in overweight and obese men: a secondary analysis of energy expenditure and physical activity. bioRxiv. The Preprint Server for Biology, 2018, 10.1101/383752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Pawlak DB, Kushner JA, Ludwig DS. Effects of dietary glycaemic index on adiposity, glucose homoeostasis, and plasma lipids in animals. Lancet 2004;364:778-85. 10.1016/S0140-6736(04)16937-7 [DOI] [PubMed] [Google Scholar]
- 55. Chaput JP, Tremblay A, Rimm EB, Bouchard C, Ludwig DS. A novel interaction between dietary composition and insulin secretion: effects on weight gain in the Quebec Family Study. Am J Clin Nutr 2008;87:303-9. 10.1093/ajcn/87.2.303 [DOI] [PubMed] [Google Scholar]
- 56. Astley CM, Todd JN, Salem RM, et al. Genetic Evidence That Carbohydrate-Stimulated Insulin Secretion Leads to Obesity. Clin Chem 2018;64:192-200. 10.1373/clinchem.2017.280727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Pittas AG, Das SK, Hajduk CL, et al. A low-glycemic load diet facilitates greater weight loss in overweight adults with high insulin secretion but not in overweight adults with low insulin secretion in the CALERIE Trial. Diabetes Care 2005;28:2939-41. 10.2337/diacare.28.12.2939 [DOI] [PubMed] [Google Scholar]
- 58. Gardner CD, Trepanowski JF, Del Gobbo LC, et al. Effect of low-fat vs low-carbohydrate diet on 12-month weight loss in overweight adults and the association with genotype pattern or insulin secretion: The DIETFITS randomized clinical trial. JAMA 2018;319:667-79. 10.1001/jama.2018.0245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Larsen TM, Dalskov SM, van Baak M, et al. Diet, Obesity, and Genes (Diogenes) Project Diets with high or low protein content and glycemic index for weight-loss maintenance. N Engl J Med 2010;363:2102-13. 10.1056/NEJMoa1007137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Qi Q, Chu AY, Kang JH, et al. Sugar-sweetened beverages and genetic risk of obesity. N Engl J Med 2012;367:1387-96. 10.1056/NEJMoa1203039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Levine JA, Eberhardt NL, Jensen MD. Role of nonexercise activity thermogenesis in resistance to fat gain in humans. Science 1999;283:212-4. 10.1126/science.283.5399.212 [DOI] [PubMed] [Google Scholar]
- 62. Rosenbaum M, Goldsmith R, Bloomfield D, et al. Low-dose leptin reverses skeletal muscle, autonomic, and neuroendocrine adaptations to maintenance of reduced weight. J Clin Invest 2005;115:3579-86. 10.1172/JCI25977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Rosenbaum M, Vandenborne K, Goldsmith R, et al. Effects of experimental weight perturbation on skeletal muscle work efficiency in human subjects. Am J Physiol Regul Integr Comp Physiol 2003;285:R183-92. 10.1152/ajpregu.00474.2002 [DOI] [PubMed] [Google Scholar]
- 64. Cummings DE, Foster-Schubert KE, Overduin J. Ghrelin and energy balance: focus on current controversies. Curr Drug Targets 2005;6:153-69. 10.2174/1389450053174569 [DOI] [PubMed] [Google Scholar]
- 65. Mihalache L, Gherasim A, Niţă O, et al. Effects of ghrelin in energy balance and body weight homeostasis. Hormones (Athens) 2016;15:186-96. 10.14310/horm.2002.1672 [DOI] [PubMed] [Google Scholar]
- 66. Ye Z, Liu G, Guo J, Su Z. Hypothalamic endoplasmic reticulum stress as a key mediator of obesity-induced leptin resistance. Obes Rev 2018;19:770-85. 10.1111/obr.12673 [DOI] [PubMed] [Google Scholar]
- 67. Crujeiras AB, Goyenechea E, Abete I, et al. Weight regain after a diet-induced loss is predicted by higher baseline leptin and lower ghrelin plasma levels. J Clin Endocrinol Metab 2010;95:5037-44. 10.1210/jc.2009-2566 [DOI] [PubMed] [Google Scholar]
- 68. Erez G, Tirosh A, Rudich A, et al. Phenotypic and genetic variation in leptin as determinants of weight regain. Int J Obes (Lond) 2011;35:785-92. 10.1038/ijo.2010.217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Mavri A, Stegnar M, Sabovic M. Do baseline serum leptin levels predict weight regain after dieting in obese women? Diabetes Obes Metab 2001;3:293-6. 10.1046/j.1463-1326.2001.00134.x [DOI] [PubMed] [Google Scholar]
- 70. Sacks FM, Bray GA, Carey VJ, et al. Comparison of weight-loss diets with different compositions of fat, protein, and carbohydrates. N Engl J Med 2009;360:859-73. 10.1056/NEJMoa0804748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Hall KD, Guo J, Chen KY, et al. Potential bias of doubly labeled water for measuring energy expenditure differences between diets varying in carbohydrate. bioRxiv. The Preprint Server for Biology, 2018, 10.1101/403931. [DOI] [Google Scholar]
- 72. Haggarty P, McGaw BA, Fuller MF, Christie SL, Wong WW. Water hydrogen incorporation into body fat in pigs: effect on double/triple-labeled water method. Am J Physiol 1991;260:R627-34. [DOI] [PubMed] [Google Scholar]
- 73. Parks EJ, Krauss RM, Christiansen MP, Neese RA, Hellerstein MK. Effects of a low-fat, high-carbohydrate diet on VLDL-triglyceride assembly, production, and clearance. J Clin Invest 1999;104:1087-96. 10.1172/JCI6572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Hudgins LC, Seidman CE, Diakun J, Hirsch J. Human fatty acid synthesis is reduced after the substitution of dietary starch for sugar. Am J Clin Nutr 1998;67:631-9. 10.1093/ajcn/67.4.631 [DOI] [PubMed] [Google Scholar]
- 75. Schwarz JM, Neese RA, Turner S, Dare D, Hellerstein MK. Short-term alterations in carbohydrate energy intake in humans. Striking effects on hepatic glucose production, de novo lipogenesis, lipolysis, and whole-body fuel selection. J Clin Invest 1995;96:2735-43. 10.1172/JCI118342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Strawford A, Antelo F, Christiansen M, Hellerstein MK. Adipose tissue triglyceride turnover, de novo lipogenesis, and cell proliferation in humans measured with 2H2O. Am J Physiol Endocrinol Metab 2004;286:E577-88. 10.1152/ajpendo.00093.2003 [DOI] [PubMed] [Google Scholar]
- 77. Guo ZK, Cella LK, Baum C, Ravussin E, Schoeller DA. De novo lipogenesis in adipose tissue of lean and obese women: application of deuterated water and isotope ratio mass spectrometry. Int J Obes Relat Metab Disord 2000;24:932-7. 10.1038/sj.ijo.0801256 [DOI] [PubMed] [Google Scholar]
- 78. Diraison F, Yankah V, Letexier D, Dusserre E, Jones P, Beylot M. Differences in the regulation of adipose tissue and liver lipogenesis by carbohydrates in humans. J Lipid Res 2003;44:846-53. 10.1194/jlr.M200461-JLR200 [DOI] [PubMed] [Google Scholar]
- 79. Hudgins LC, Baday A, Hellerstein MK, et al. The effect of dietary carbohydrate on genes for fatty acid synthase and inflammatory cytokines in adipose tissues from lean and obese subjects. J Nutr Biochem 2008;19:237-45. 10.1016/j.jnutbio.2007.02.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Chong MF, Hodson L, Bickerton AS, et al. Parallel activation of de novo lipogenesis and stearoyl-CoA desaturase activity after 3 d of high-carbohydrate feeding. Am J Clin Nutr 2008;87:817-23. 10.1093/ajcn/87.4.817 [DOI] [PubMed] [Google Scholar]
- 81. Letexier D, Pinteur C, Large V, Fréring V, Beylot M. Comparison of the expression and activity of the lipogenic pathway in human and rat adipose tissue. J Lipid Res 2003;44:2127-34. 10.1194/jlr.M300235-JLR200 [DOI] [PubMed] [Google Scholar]
- 82. Viguerie N, Vidal H, Arner P, et al. Nutrient-Gene Interactions in Human Obesity--Implications for Dietary Guideline (NUGENOB) project Adipose tissue gene expression in obese subjects during low-fat and high-fat hypocaloric diets. Diabetologia 2005;48:123-31. 10.1007/s00125-004-1618-x [DOI] [PubMed] [Google Scholar]
- 83. Aarsland A, Chinkes D, Wolfe RR. Hepatic and whole-body fat synthesis in humans during carbohydrate overfeeding. Am J Clin Nutr 1997;65:1774-82. 10.1093/ajcn/65.6.1774 [DOI] [PubMed] [Google Scholar]
- 84. Minehira K, Vega N, Vidal H, Acheson K, Tappy L. Effect of carbohydrate overfeeding on whole body macronutrient metabolism and expression of lipogenic enzymes in adipose tissue of lean and overweight humans. Int J Obes Relat Metab Disord 2004;28:1291-8. 10.1038/sj.ijo.0802760 [DOI] [PubMed] [Google Scholar]
- 85. Rosenbaum M, Ravussin E, Matthews DE, et al. A comparative study of different means of assessing long-term energy expenditure in humans. Am J Physiol 1996;270:R496-504. [DOI] [PubMed] [Google Scholar]
- 86. Bueno NB, de Melo IS, de Oliveira SL, da Rocha Ataide T. Very-low-carbohydrate ketogenic diet v. low-fat diet for long-term weight loss: a meta-analysis of randomised controlled trials. Br J Nutr 2013;110:1178-87. 10.1017/S0007114513000548 [DOI] [PubMed] [Google Scholar]
- 87. Johnston BC, Kanters S, Bandayrel K, et al. Comparison of weight loss among named diet programs in overweight and obese adults: a meta-analysis. JAMA 2014;312:923-33. 10.1001/jama.2014.10397 [DOI] [PubMed] [Google Scholar]
- 88. Mancini JG, Filion KB, Atallah R, Eisenberg MJ. Systematic review of the mediterranean diet for long-term weight loss. Am J Med 2016;129:407-415.e4. [DOI] [PubMed] [Google Scholar]
- 89. Mansoor N, Vinknes KJ, Veierød MB, Retterstøl K. Effects of low-carbohydrate diets v. low-fat diets on body weight and cardiovascular risk factors: a meta-analysis of randomised controlled trials. Br J Nutr 2016;115:466-79. 10.1017/S0007114515004699 [DOI] [PubMed] [Google Scholar]
- 90. Sackner-Bernstein J, Kanter D, Kaul S. Dietary intervention for overweight and obese adults: comparison of low-carbohydrate and low-fat diets. A meta-analysis. PLoS One 2015;10:e0139817. 10.1371/journal.pone.0139817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Tobias DK, Chen M, Manson JE, Ludwig DS, Willett W, Hu FB. Effect of low-fat diet interventions versus other diet interventions on long-term weight change in adults: a systematic review and meta-analysis. Lancet Diabetes Endocrinol 2015;3:968-79. 10.1016/S2213-8587(15)00367-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental information: additional material
Supplemental information: figure 2 with full details of exclusions