Abstract
Background
Early diagnosis of unilateral chronic lung allograft dysfunction (CLAD) is difficult because the unaffected contralateral lung functions as a reservoir in bilateral living-donor lobar lung transplantation (LDLLT). We previously reported the usefulness of 133Xe ventilation scintigraphy for detection of unilateral change, but the supply of 133Xe has been stopped globally. The present study aimed to examine the usefulness of inspiratory and expiratory computed tomography (I/E CT) volumetry for detection of unilateral change in CLAD patients.
Methods
This was a retrospective single-center, observational study using prospectively collected data. A total of 58 patients who underwent bilateral LDLLT from August 2008 to February 2017 were analyzed. Respiratory function tests, I/E CT were prospectively conducted. ΔLung volume was defined as the value obtained by subtracting expiratory lung volume from inspiratory lung volume.
Results
Fourteen (24%) cases were clinically diagnosed with CLAD, of which 10 (71%) were diagnosed as unilateral CLAD. ΔLung volume of bilateral lungs strongly correlated with forced vital capacity (r = 0.92, P < 0.01) and forced expiratory volume in 1 second (r = 0.80, P < 0.01). Regardless the phenotypes (bronchiolitis obliterans syndrome or restrictive allograft syndrome) of CLAD, Δlung volume onset/baseline significantly decreased compared with that in the non-CLAD group. Among the 10 unilateral CLAD patients, 3 with clinically suspected unilateral rejection yet did not show a 20% decline in forced expiratory volume in 1 second. In 2 of these, Δlung volume of unilateral lungs on the rejection side decreased by 20% or more.
Conclusions
Our findings suggest that I/E CT volumetry may be useful for assessment and early diagnosis of unilateral CLAD after bilateral LDLLT.
Lung transplantation is now widely performed as a treatment for end-stage respiratory diseases. However, the survival rate of patients who undergo lung transplantation is still insufficient and lower than for those who undergo other solid organ transplantations.1,2
Chronic lung allograft dysfunction (CLAD) is a major cause limiting long-term survival after lung transplantation.3-5 Chronic lung allograft dysfunction is mainly a result of chronic rejection, and early diagnosis and treatment with immune suppressors are crucial. However, early diagnosis of any unilateral change of CLAD, especially in bilateral living-donor lung lobar transplantation (LDLLT) is difficult because the unaffected contralateral lung functions as a reservoir.
Bronchiolitis obliterans syndrome (BOS), the most common form of obstructive CLAD, is diagnosed based on a respiratory function test, but ventilation scintigraphy is also useful as a support tool for diagnosis. We previously reported the usefulness of 133Xe ventilation scintigraphy for detection of unilateral change in BOS patients,6 but 133Xe cannot be used in clinical practice now because the supply of nuclide (133Xe) has been stopped globally. We therefore need an alternative examination method for the early diagnosis of unilateral CLAD. Various assessments of pulmonary function using imaging modalities have been reported recently, such as inspiratory and expiratory computed tomography volumetry (I/E CT volumetry),7-9 single photon emission CT of pulmonary perfusion and ventilation scintigraphy with technetium,10 and dual-energy Xenon CT.11 Among the abovementioned, I/E CT volumetry is simple and requires no special equipment, and it has been already reported that 3D-CT imaging is useful in lung transplantation.12 In the present study, we hypothesized that I/E CT volumetry would be able to replace 133Xe ventilation scintigraphy for detection of CLAD. Hence, we examined the usefulness of I/E CT volumetry for detection of unilateral change in CLAD patients.
MATERIALS AND METHODS
This study was a retrospective single-center, observational study approved by the Ethics Committee of Kyoto University Graduate School of Medicine (R1053). A total of 63 consecutive patients who underwent bilateral LDLLT from August 2008 to February 2017 in Kyoto University Hospital were enrolled. Pulmonary function tests (PFTs), I/E CT, and 133Xe ventilation scintigraphy were conducted at 3, 6, and 12 months after transplantation and once yearly thereafter. The exclusion criteria included in-hospital death and death within 3 months. After application of the exclusion criteria, 58 patients were retained (Figure 1).
FIGURE 1.
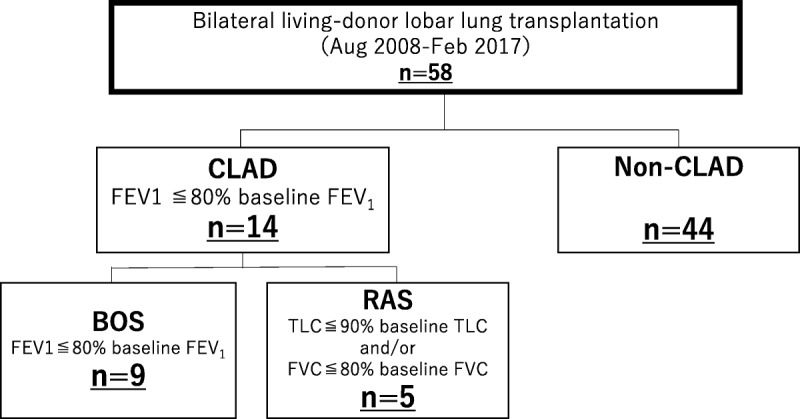
Study group cohort.
Chronic lung allograft dysfunction was defined as an irreversible decline in forced expiratory volume in 1 second (FEV1) to less than 80% of baseline for 3 weeks or longer. Furthermore, although BOS was defined as just a decline in FEV1, restrictive allograft syndrome (RAS) was defined as a persistent decline in total lung capacity greater than 10% and/or forced vital capacity (FVC) greater than 20%.13
We clinically suspected CLAD when the patient had FEV1 declines by 10% or more with or without symptom.
When we diagnosed as unilateral CLAD, the patients decreased FEV1 by 20% or more, and they also had obviously unilateral change in imaging examination (ie, emphysematous or fibrotic change). In unilateral CLAD patients, we classified healthy side of the lung as non-CLAD lung in this study.
I/E CT Volumetry
I/E CT images were obtained during respiratory pauses at the end of maximum inspiratory effort and expiratory effort using a multiditector Aquilion 64 CT scanner (Toshiba Medical Systems, Tochigi, Japan) with 0.5-mm collimation, a scan time of 500 ms, a peak tube voltage of 120 kVp and autoexposure control.9,14 I/E CT data were transferred to a workstation (SYNAPSE VINCENT; FUJIFILM, Tokyo, Japan), on which 3D lung models were reconstructed and each lung volume measured. ΔLung volume was defined as the value obtained by subtracting expiratory lung volume from inspiratory lung volume.
133Xe Ventilation Scintigraphy
133Xe ventilation scintigraphy was performed as previously described.15 Briefly, a gamma camera unit (Infinia; GE Healthcare, Milwaukee, WI, USA) was used to acquire posterior ventilation image from the patient after inhalation of 133Xe gas (370 MBq). Two minutes after starting, washout images were acquired until 8 minutes had elapsed.
The mean transit time (MTT) was computed using height-over-area method from the washout curve, as previously described.16
Statistical Analysis
All values are presented as the mean ± the standard deviation. Analyses were performed using JMP pro 12.2.0 software (SAS Institute, Cary, NC). To compare the means of the 3 groups, 1-way analysis of variance was performed and the Dunnett test was then conducted to determine differences. The correlations between PFTs and Δlung volume were calculated with the Pearson product moment correlation analysis. A P value <0.05 was considered statistically significant. Sensitivity, specificity, and area under the receiver operating characteristic curve (AUC) were calculated for differentiating between the CLAD and non-CLAD groups.
RESULTS
Patient Characteristics
Patient characteristics are shown in Table 1. No significant differences were found in mean age, gender, primary disease, and size match between non-CLAD, BOS, and RAS patients. Fourteen cases were clinically diagnosed with CLAD, of which 10 (71%) were diagnosed as unilateral CLAD.
TABLE 1.
Patient characteristics
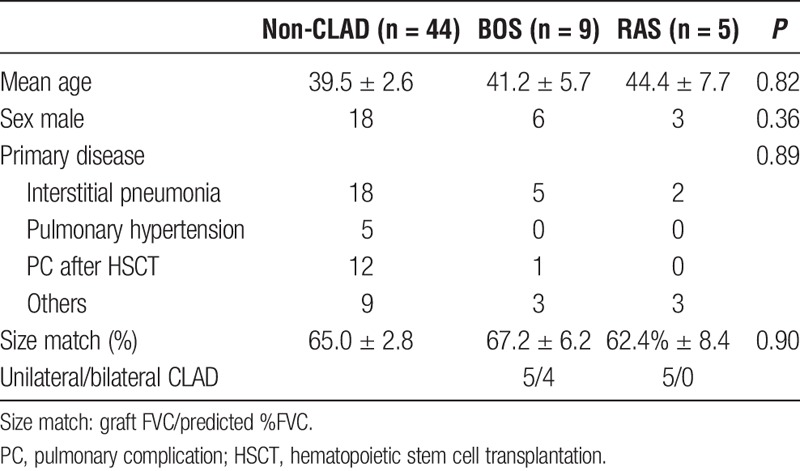
Relationship Between CT Volumetry and PFTs
Δlung volume of bilateral lungs was strongly related to FVC (r = 0.92, P < 0.01) and FEV1 (r = 0.80, P < 0.01) (Figures 2A-B).
FIGURE 2.
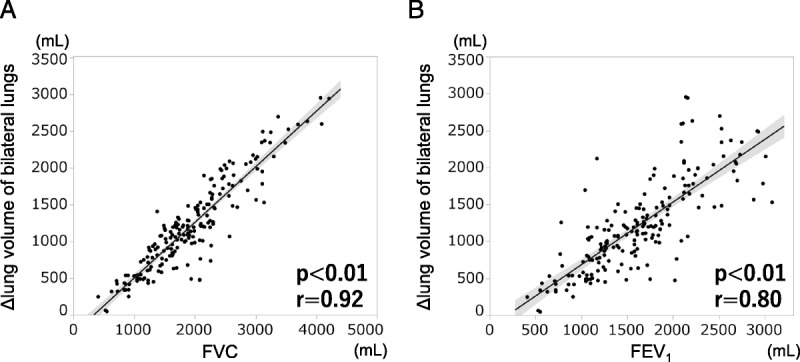
Correlation analysis (A) between Δlung volume of bilateral lungs and FVC. (B) Between Δlung volume of bilateral lungs and FEV1. r, correlation coefficient.
Comparison between onset or latest and baseline of Δlung volume and inspiratory lung volume is shown in Figure 3. In both the BOS and RAS group, Δlung volume onset/baseline was significantly decreased compared to that in the non-CLAD group. For diagnosis of CLAD, the AUC using an inward surface vector was 0.87, with an optimum cutoff of 0.80 with 73% sensitivity and 98% specificity.
FIGURE 3.
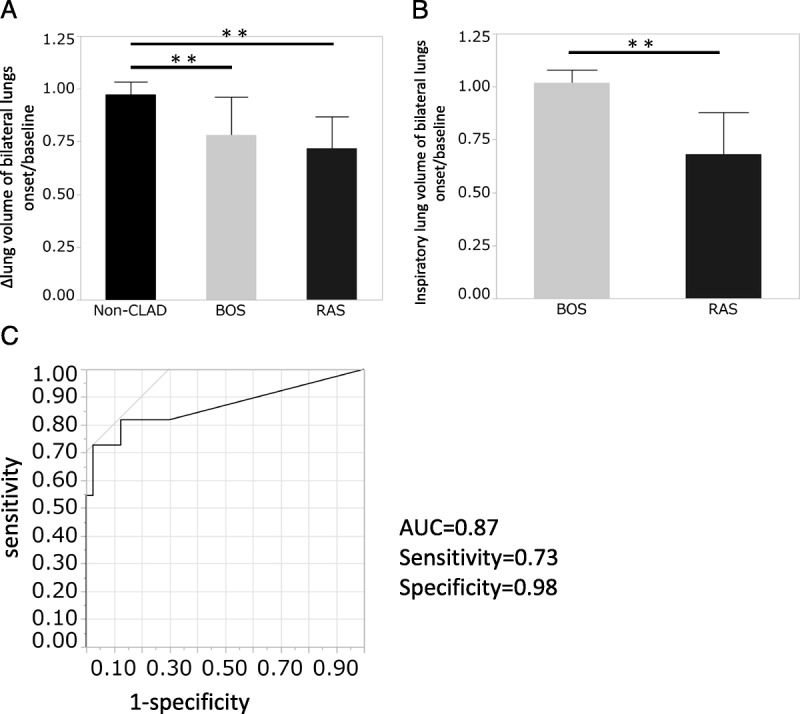
A, ΔCT volume of bilateral lungs onset or latest/baseline in the 3 groups. B, Inspiratory CT volume onset or latest/baseline. C, ROC curve analysis for diagnosis of CLAD using ΔCT volume onset or latest/baseline. Bars and error bars show mean and standard deviation; **P < 0.01. ROC, receiver operating characteristic.
133Xe Ventilation Scintigraphy of Unilateral Lungs
The results of the MTT of unilateral lungs are shown in Figure 4. The MTT of BOS lungs was significantly longer than the other 2 groups (Figure 4A). ΔLung volume of unilateral lungs was negatively related to MTT (r = −0.34, P < 0.01) (Figure 4B).
FIGURE 4.

A, MTT of unilateral lungs divided into the 3 groups, non-CLAD lungs, BOS lungs, and RAS lungs. B, Correlation analysis between Δlung volume of unilateral lungs and MTT of unilateral lungs. Bars and error bars show mean and standard deviation; *P < 0.05, **P < 0.01. r: correlation coefficient.
I/E CT Volumetry in Unilateral CLAD Patients
Among the 10 unilateral CLAD patients, 1 patient was excluded by deficit data and remaining 9 patients were analyzed. Among them, 3 patients had clinically suspected rejection of the unilateral lung yet did not show a 20% decline in FEV1. In 2 of these, Δlung volume of unilateral lungs on the rejection side was decreased by 20% or more, and the remaining 1 case was also decreased by 15% at the time.
A representative case is shown in Figure 5. She was suspected of CLAD on the left lung at 2 years after transplant. Compared with the previous year, the left expiratory lung volume was increased, and the right was decreased, though both inspiratory lung volumes were similar. Therefore, Δlung volume of the left lung was decreased by more than 20%, whereas Δlung volume of the right lung was increased.
FIGURE 5.
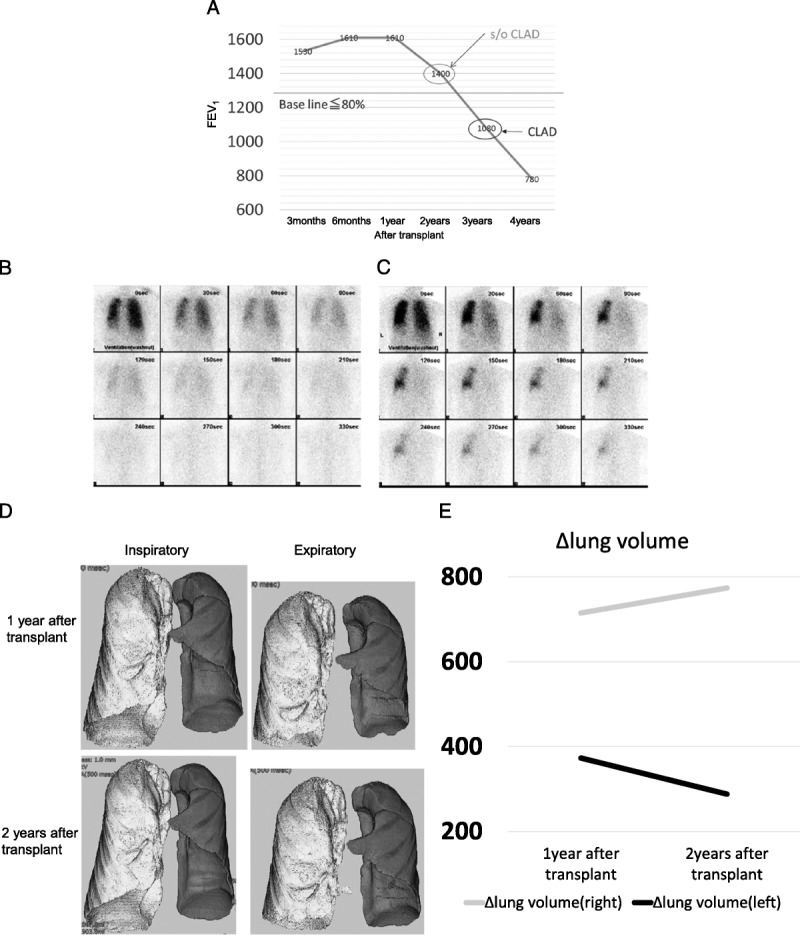
Representative case of unilateral CLAD. A, Posttransplant course of FEV1. B, 133Xe ventilation scintigraphy 1 year after transplant. C, 133Xe ventilation scintigraphy 2 years after transplant. D, I/E CT volumetry at 1 year and 2 years after transplantation. E, Δlung volume 1 year and 2 years after transplant.
DISCUSSION
This study compared the result from I/E CT volumetry, PFTs, and 133Xe ventilation scintigraphy in patients who underwent bilateral LDLLT and the usefulness of I/E CT volumetry for diagnosis of unilateral CLAD. The results showed that I/E CT volumetry on both sides had a strong positive correlation with FVC and FEV1. The MTT of 133Xe ventilation scintigraphy (MTT) was useful for diagnosis of BOS and Δlung volume of unilateral lungs had a weak correlation with MTT. Decline in Δlung volume of bilateral lungs from baseline in CLAD patients was significantly larger than that in non-CLAD patients. Furthermore, Δlung volume of unilateral lungs was able to detect unilateral change in CLAD patients.
A previous study has shown the usefulness of inspiratory CT volumetry in CLAD patients to differentiate RAS from BOS patients because inspiratory lung volume had a strong positive correlation with total lung capacity.17 In this study, by adding expiratory CT to inspiratory CT, it is possible to estimate FVC and FEV1 from Δlung volume of bilateral lungs, and it can be used for diagnosis of CLAD. It has been reported that expiratory CT can detect air trapping which is frequently observed in obstructive change.18-21 Therefore, I/E CT volumetry was able to detect not only restrictive change but also obstructive change. In BOS patients, inspiratory lung volume was gradually increased, and expiratory lung volume was also increased by emphysematous change. In RAS patients, both inspiratory lung volume and expiratory lung volume were gradually decreased because of fibrotic change, and dynamic compliance of the lungs were decreased. This is the difference between BOS and RAS.
We recommend that 20% of Δlung volume loss should be considered CLAD because we clinically diagnosed CLAD using FEV1 by 20% or more from the baseline. Furthermore, in ROC curve analysis for differentiating between CLAD and non-CLAD group using Δlung volume onset or latest/ baseline, the cutoff value that maximizes AUC was 0.80 with high specificity (98%), but not so high sensitivity (73%). In this study and setting, 2 of 9 unilateral CLAD cases could be early diagnosed by I/E CT volumetry.
There were some cases in which FEV1 was decreased, but Δlung volume was not decreased. Among them, the MTT was not extended in this study. It seemed that detection of obstructive changes without air trapping was difficult with I/E CT volumetry. However, air trapping is a characteristic finding in BOS patients, and the ability to detect air trapping is one of the reasons for high specificity of diagnosis. It is likely that ventilation scintigraphy, with its ability to be evaluated by integrating multiple breaths, might have higher sensitivity to detect obstructive change than I/E CT volumetry, but we can no longer use it.
The I/E CT volumetry data were also affected by other lung diseases. For example, there was a case who had pneumonia and decreased Δlung volume in this study. After the treatment of pneumonia, Δlung volume was improved but not as much as before and lung injury (scarring) on pneumonia was remained in this case.
ΔLung volume can be measured not only in both lungs but also in localized areas, such as 1 lung or 1 lobe, and it is possible to estimate the regional lung function and to detect unilateral CLAD. This is the advantage of using I/E CT volumetry. We think these results are applicable on single lung transplantation, and we plan to collect the data in cadaveric single lung transplantation patients.
Previously, it was difficult to evaluate the respiratory function of lung regions, but I/E CT volumetry allows us to analyze the regional lung function. Evaluation of lung function using imaging modality is expected to progress further in the future.11 Specifically, evaluation of the total respiratory phase with 4DCT and evaluation of airflow in xenon contrast CT may be useful as well.22
Several limitations of this study should be acknowledged. First, it is difficult to stop breathing in patients whose respiratory function is significantly low, and it is uncertain whether the inspiratory phase or the expiratory phase at the time of each scan. However, since I/E CT is aimed at early detection of CLAD, it is probable that patients with worse lung function have already been diagnosed and treated, and it will not fit for this study purpose.
Second, inspiratory CT and expiratory CT imaging double the usual exposure dose. However, ultralow dose CT has become available for CT volumetry, and the exposure dose is expected to be further reduced with the development of technology in the future.23,24
Third, some patients with pulmonary complication other than CLAD (eg, pneumonia) decreased Δlung volume. However, we were able to use CT imaging by I/E CT and diagnose it appropriately.
In conclusion, our findings suggest that I/E CT volumetry is able to predict the unilateral pulmonary function in patients with LDLLT. I/E CT volumetry is useful for assessment of CLAD in which change occurs only unilaterally. In this study, we examined patients who underwent bilateral LDLLT. It may be useful also in single lung transplantation from cadaveric donors.
Footnotes
Published online 12 October, 2018.
The authors declare no funding or conflicts of interests.
M.S. participated in the study design, data acquisition and analysis, article composition and revision. T.F.C.Y. participated in the study design, data analysis, and article composition. Y.N. participated in the study design, data acquisition, and article revision. H.K. participated in the data acquisition and article revision. J.T. participated in the data acquisition. S.U. participated in the data acquisition. H.Y. participated in the data acquisition and article revision. F.G. participated in the data acquisition and article revision. R.O. participated in the study conception, data acquisition, and article revision. A.K. participated in the study design and data acquisition. M.H. participated in the article revision. H.M. participated in the article revision. A.A. participated in the study conception and article revision. H.D. participated in the study conception and design, article revision.
REFERENCES
- 1.Meyer KC. Lung transplantation. F1000Prime Rep. 2013;5:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yusen RD, Edwards LB, Dipchand AI, et al. The registry of the International Society for Heart and Lung Transplantation: thirty-third adult lung and heart-lung transplant report-2016; focus theme: primary diagnostic indications for transplant. J Heart Lung Transplant. 2016;35:1170–1184. [DOI] [PubMed] [Google Scholar]
- 3.Royer PJ, Olivera-Botello G, Koutsokera A, et al. Chronic lung allograft dysfunction: a systematic review of mechanisms. Transplantation. 2016;100:1803–1814. [DOI] [PubMed] [Google Scholar]
- 4.Verleden GM, Vos R, Vanaudenaerde B, et al. Current views on chronic rejection after lung transplantation. Transpl Int. 2015;28:1131–1139. [DOI] [PubMed] [Google Scholar]
- 5.Weigt SS, Wang X, Palchevskiy V, et al. Gene expression profiling of bronchoalveolar lavage cells preceding a clinical diagnosis of chronic lung allograft dysfunction. PLoS One. 2017;12:e0169894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Miyamoto E, Chen F, Aoyama A, et al. Unilateral chronic lung allograft dysfunction is a characteristic of bilateral living-donor lobar lung transplantation. Eur J Cardiothorac Surg. 2015;48:463–469. [DOI] [PubMed] [Google Scholar]
- 7.Yabuuchi H, Kawanami S, Kamitani T, et al. Prediction of post-operative pulmonary function after lobectomy for primary lung cancer: a comparison among counting method, effective lobar volume, and lobar collapsibility using inspiratory/expiratory CT. Eur J Radiol. 2016;85:1956–1962. [DOI] [PubMed] [Google Scholar]
- 8.Chen F, Fujinaga T, Bando T, et al. Pulmonary function of individual lung lobes after complex living-donor lobar lung transplantation using inspiratory and expiratory three-dimensional computed tomographic volumetry. Interact Cardiovasc Thorac Surg. 2012;15:1077–1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen F, Kubo T, Shoji T, et al. Comparison of pulmonary function test and computed tomography volumetry in living lung donors. J Heart Lung Transplant. 2011;30:572–575. [DOI] [PubMed] [Google Scholar]
- 10.Norberg P, Persson HL, Carlsson GA, et al. Quantitative lung SPECT applied on simulated early COPD and humans with advanced COPD. EJNMMI Res. 2013;3:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kyoyama H, Hirata Y, Kikuchi S, et al. Evaluation of pulmonary function using single-breath-hold dual-energy computed tomography with xenon: results of a preliminary study. Medicine (Baltimore). 2017;96:e5937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen-Yoshikawa TF, Date H. Three-dimensional image in lung transplantation. Gen Thorac Cardiovasc Surg. 2018;66:19–26. [DOI] [PubMed] [Google Scholar]
- 13.Verleden GM, Raghu G, Meyer KC, et al. A new classification system for chronic lung allograft dysfunction. J Heart Lung Transplant. 2014;33:127–133. [DOI] [PubMed] [Google Scholar]
- 14.Oguma T, Niimi A, Hirai T, et al. Assessment of small airways with computed tomography: mosaic attenuation or lung density? Respiration. 2015;89:539–549. [DOI] [PubMed] [Google Scholar]
- 15.Kawase S, Ohno K, Nakamoto Y, et al. Safety management of nuclear medicine personnel with visualization of air dose rate. Radiat Prot Dosimetry. 2015;165:439–442. [DOI] [PubMed] [Google Scholar]
- 16.Shinya T, Sato S, Kato K, et al. Assessment of mean transit time in the engrafted lung with 133Xe lung ventilation scintigraphy improves diagnosis of bronchiolitis obliterans syndrome in living-donor lobar lung transplant recipients. Ann Nucl Med. 2008;22:31–39. [DOI] [PubMed] [Google Scholar]
- 17.Saito T, Horie M, Sato M, et al. Low-dose computed tomography volumetry for subtyping chronic lung allograft dysfunction. J Heart Lung Transplant. 2016;35:59–66. [DOI] [PubMed] [Google Scholar]
- 18.Yamashiro T, Matsuoka S, Bartholmai BJ, et al. Collapsibility of lung volume by paired inspiratory and expiratory CT scans: correlations with lung function and mean lung density. Acad Radiol. 2010;17:489–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mohamed Hoesein FA, de Jong PA. Air trapping on computed tomography: regional versus diffuse. Eur Respir J. 2017;49. [DOI] [PubMed] [Google Scholar]
- 20.Mets OM, Zanen P, Lammers JW, et al. Early identification of small airways disease on lung cancer screening CT: comparison of current air trapping measures. Lung. 2012;190:629–633. [DOI] [PubMed] [Google Scholar]
- 21.Solyanik O, Hollmann P, Dettmer S, et al. Quantification of pathologic air trapping in lung transplant patients using CT density mapping: comparison with other CT air trapping measures. PLoS One. 2015;10:e0139102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jahani N, Choi S, Choi J, et al. Assessment of regional ventilation and deformation using 4D-CT imaging for healthy human lungs during tidal breathing. J Appl Physiol. 2015;119:1064–1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Messerli M, Ottilinger T, Warschkow R, et al. Emphysema quantification and lung volumetry in chest X-ray equivalent ultralow dose CT—intra-individual comparison with standard dose CT. Eur J Radiol. 2017;91:1–9. [DOI] [PubMed] [Google Scholar]
- 24.Hammond E, Sloan C, Newell JD, Jr, et al. Comparison of low- and ultralow-dose computed tomography protocols for quantitative lung and airway assessment. Med Phys. 2017;44:4747–4757. [DOI] [PMC free article] [PubMed] [Google Scholar]


