Severe hypoglycemia (SH) is believed to be responsible for 4% to 10% of deaths in individuals with type 1 diabetes (T1D).1 Treatment recommendations for people with SH and impaired awareness of hypoglycemia (IAH) incorporate a tiered, 4-stage algorithm that includes educational, technological, and transplantation interventions.2 However, applicability of islet transplantation is restricted by limited supply of donor organs, need for immunosuppression, and strict eligibility criteria. This is the first report of mortality in people referred to a national islet transplantation program, whether or not they received a transplant.
All referrals between 2005 and 2016 to Australian islet transplant centers (St Vincent's Hospital, Melbourne; Westmead Hospital, Sydney; Royal Adelaide Hospital, Adelaide) were retrospectively reviewed. Major inclusion criteria for islet transplantation include: age, 18 to 65 years; T1D, longer than 5 years; recurrent SH; IAH; failed intensive insulin therapy. Exclusion criteria include: creatinine clearance less than 75 mL/min per 1.73 m2; proteinuria greater than 300 mg/d; weight greater than 80 kg; active psychiatric illness; pregnancy.3
Of 321 people (66% female) referred for islet transplantation, 40 received 1 or more transplant, 15 were on the active waiting list, and 266 were considered unsuitable for transplant (Table 1). There were a total of 11 deaths, resulting in an overall mortality rate of 3.4%. Table 2 shows characteristics of the deceased individuals. Most were women with long-duration T1D and suboptimal glycemic control, using multiple daily injections. Use of continuous subcutaneous insulin infusion (CSII) is limited in Australia; however, the transplant program mandates that CSII is considered and/or trialed before proceeding to transplant. There were no differences in baseline demographics or diabetes-related characteristics between the deceased and transplant group (data not shown).
TABLE 1.
Mortality rates in people referred for islet transplantation
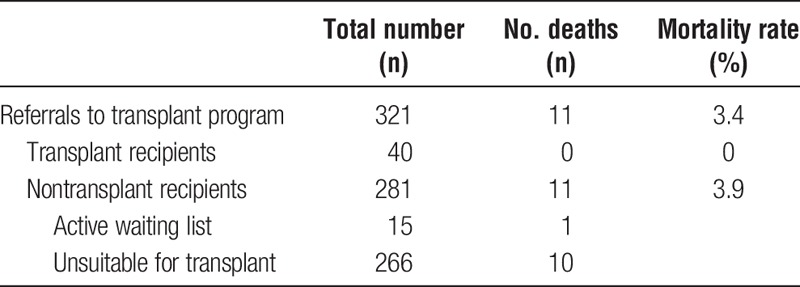
TABLE 2.
Characteristics of deceased individuals referred for islet transplantation (n = 11)
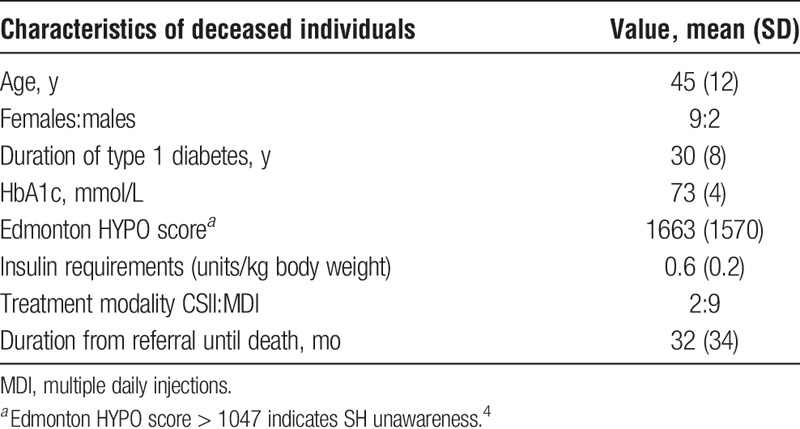
Ten of 11 deceased individuals were unsuitable for transplantation due to renal impairment (stage 3 chronic kidney disease) (3), mental illness (3), previous renal transplant (1), gastroparesis (1), active smoking (1), and acute myeloid leukemia (1). Only 1 person was on the active waiting list and died after presumed deliberate insulin overdose, despite undergoing formal assessment for psychiatric illness. Eight of 11 deaths were hypoglycemia-related: 3 from deliberate insulin overdose in individuals with known depression; 3 from “dead-in-bed” syndrome; 1 from myocardial infarction following hypoglycemia; and 1 after an unintentional insulin overdose. There was 1 death due to diabetic ketoacidosis. The 2 nondiabetes-related deaths were due to septic shock after bowel perforation and acute myeloid leukemia.
Suicide constitutes 4.4% of deaths in the general population with T1D younger than 40 years in Australia.5 Severe hypoglycemia and IAH is known to be associated with poorer psychological well-being,6 and the high suicide rate of 27% evident within our cohort demonstrates the need for psychological support and intervention. All patients undergo assessment by a psychiatrist prior to transplantation.
Renal impairment is another common reason that people are not suitable for transplant. Cause of death in these individuals was predominantly hypoglycemia-related. Compromised renal function further increases risk of hypoglycemia as well as mortality, including death from unintentional insulin overdose. Reduced clearance of insulin was possibly a contributing factor to hypoglycemia in these cases.
Our mortality rate may be an underestimate as some deaths may not have been identified. Linkage to the National Death Registry is in progress. It is difficult to compare our mortality rates as there are no specific reports of mortality in the T1D population with SH and IAH, and no reports from other islet transplant programs.
Currently, approximately 80% of islet transplant referrals do not receive transplant for medical or psychosocial reasons in Australia. The Australian islet transplant program is actively promoted using educational means to raise awareness within the endocrine community about the indications for transplant and the population in whom transplantation may be beneficial. Highly specialized multidisciplinary clinics with expertise in managing problematic hypoglycemia should be considered to support these high-risk patients who are not suitable for transplant.
This report affirms that individuals referred for islet transplantation represent a highly vulnerable group of T1D patients, at risk of SH and its sequelae, including death. Those who do not receive transplant have higher mortality rates than transplanted individuals despite concerns of transplant-associated risks relating to the procedure and long-term immunosuppression. According to the Collaborative Islet Transplant Registry, 819 islet transplants have been performed worldwide.7 As our eligibility criteria are similar to other major transplant centers contributing to the Collaborative Islet Transplant Registry, it is possible that over 200 people referred for islet transplantation may have died either before receiving a transplant, or after being assessed and found to be unsuitable. Our national database has now been extended to include all patients referred to the islet transplant program.
ACKNOWLEDGMENTS
The authors would like to acknowledge JDRF, Department of Health and Human Services, and NHMRC who have funded the establishment of the islet transplantation program in Australia.
Footnotes
Published online 23 October, 2018.
M.H.L., G.M.W., R.J.M., K.H., D.J.H., P.A., T.R., P.T.C., T.W.K., and D.G. declare no competing financial interests. P.J.O. consults for CSL, Vitaeris and eGenesis; and has received research grants from CSL.
M.H.L. contributed to the literature review, data interpretation and wrote the article. D.G. conceived the study, analyzed the data and reviewed and edited the article. K.H., P.A., T.R. were involved in data collection and interpretation. G.M.W., R.J.M., D.J.H., P.T.C., T.W.K., P.J.O. contributed to data interpretation, and reviewed and edited the article. D.G. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
REFERENCES
- 1.Seaquist ER, Anderson J, Childs B, et al. Hypoglycemia and diabetes: a report of a workgroup of the American Diabetes Association and the Endocrine Society. Diabetes Care. 2013;36:1384–1395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Choudhary P, Rickels MR, Senior PA, et al. Evidence-informed clinical practice recommendations for treatment of type 1 diabetes complicated by problematic hypoglycemia. Diabetes Care. 2015;38:1016–1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.The Transplant Society of Australia and New Zealand. Clinical guidelines for organ transplantation from deceased donors. 2017 May; version 1.1. Available at: https://www.tsanz.com.au/organallocationguidelines/documents/ClinicalGuidelinesV1.1May2017.pdf. Accessed July 14, 2018.
- 4.Ryan EA, Shandro T, Green K, et al. Assessment of the severity of hypoglycemia and glycemic lability in type 1 diabetic subjects undergoing islet transplantation. Diabetes. 2004;53:955–962. [DOI] [PubMed] [Google Scholar]
- 5.Tu E, Twigg SM, Duflou J, et al. Causes of death in young Australians with type 1 diabetes: a review of coronial postmortem examinations. Med J Aust. 2008;188:699–702. [DOI] [PubMed] [Google Scholar]
- 6.Hendrieckx C, Halliday JA, Bowden JP, et al. Severe hypoglycaemia and its association with psychological well-being in Australian adults with type 1 diabetes attending specialist tertiary clinics. Diabetes Res Clin Pract. 2014;103:430–436. [DOI] [PubMed] [Google Scholar]
- 7.Collaborative Islet Transplant Registry. Ninth annual report. 2016. CITR. Available at: www.citregistry.org. Accessed July 14, 2018.


