Abstract
Background:
Trends in U.S. premature mortality rates have diverged among demographic groups.
Methods:
Death certificate data for the U.S. population ages 25–64 years,1990–2016, were obtained from the Centers for Disease Control and Prevention. Age-standardized premature mortality rates (ASRs) and corresponding annual percent changes (APCs) for 2017–2030 by sex and race/ethnicity were estimated using age-period-cohort forecasting models. Absolute death counts were estimated using corresponding population projections.
Findings:
During 2017–2030, all-cause death rates are projected to increase among white women and American Indian/Alaska Natives (AIANs), resulting in 239,700 excess deaths, an 10.1% increase. Mortality declines in other groups will result in 945,900 fewer deaths (13.7% reduction). Cancer death rates are generally projected to decline, with the largest declines among black women (APC=−2∙05%/year to ASR=77∙1/100,000 in 2030) and men (−2∙64%/year; 81∙6/100,000). Heart disease death rates are projected to increase in AIAN women (+0∙52%/year; 62∙8/100,000) and men (+1∙41%/year; 175∙9/100,000) and decline in other groups. Accidental death rates are projected to increase in all groups other than API women and most rapidly among white women (+3∙71%/year; 60∙5/100,000) and men (+2∙09%/year; 101∙9/100,000), and AIAN men (+3∙08%/year; 298∙7/100,000). Suicide rates are projected to increase for all groups, and chronic liver disease/cirrhosis death rates for all but black men. A 2%/year reduction in projected accidental death rates would eliminate an estimated 178,700 deaths during 2017–2030.
Interpretation:
To reduce future premature mortality, effective interventions are needed to address rapidly rising death rates due to accidents, suicides and chronic liver disease/cirrhosis.
Introduction
Since 1980, death rates have decreased and life expectancy has increased globally, except for nations suffering natural disasters, violence and war.3 Though life expectancy has been projected to continue to increase across high-income countries, gains for the US are anticipated to be amongst the smallest.4 In fact, the overall U.S. death rates increased from 2014 to 2015.5
Though increases in total U.S. mortality trends are recent,5,6 pronounced heterogeneity in death rates has been documented across age and racial/ethnic groups for the last two decades.7 Premature mortality rates among Hispanic, non-Hispanic black/African American (i.e., black) and Asian/Pacific Islander (API) men and women declined steadily during the 21st century.7,8 In contrast, notable increases have occurred among young and middle-age non-Hispanic white (i.e., white) and American Indian/Alaska Natives (AIANs) during the same time period,7,8 driven largely by increases in accidental deaths, suicide and chronic liver disease/cirrhosis deaths.7,8
Increases in accidental deaths are driven by unintentional drug poisonings, as motor vehicle accident deaths have declined.7 Opioid overdoses are a major contributor to the increases in drug poisonings, including prescription opioids, heroin and fentanyl.9 Despite recent policies implemented to curb the opioid epidemic, the number of people in the U.S. addicted to prescription pain killers continues to increase, heroin use is climbing, and drug overdoses, particularly due to fentanyl, continue to rise.10–12
In contrast to prior studies that have addressed observed trends in mortality rates, this study focuses on projecting premature mortality (here defined as deaths of individuals aged 25–64) trends through 2030 using age-period-cohort models. These projections highlight future trajectories of premature mortality rates if current trends continue, by sex, race/ethnicity, age, and major causes of premature death. In addition, we estimated the total number of deaths projected to occur, the projected number of potential years of life lost due to premature mortality (YPLL), and the impact of reducing projected accidental death rates by 2% per year. Projecting future premature mortality is essential for planning clinical and public health services, to curb rapidly rising causes of death and to sustain progress in declining causes of death.
Methods
Data sources
U.S. mortality data for 1990–2015 were based on underlying cause of death and demographic information extracted from all death certificates from the entire population of U.S. residents, as provided by the Centers for Disease Control and Prevention National Center for Health Statistics and extracted using SEER*Stat in single-year increments of age and year at death.13 US mortality for 2016 for non-AIAN groups was obtained from CDC Wonder14. Death certificate data is provided by states to NCHS. This analysis focused on all-cause premature mortality (deaths among 25–64-year-olds, as defined in prior studies7,15), and the commonest causes of premature death (cancer, heart disease, accidents, suicide, chronic liver disease/cirrhosis)7 among white, black, Hispanic, API and AIAN men and women (ICD code groupings and racial/ethnic classification details in Supplemental Methods. Accidental and suicide deaths were mutually exclusive). AIAN estimates were restricted to counties in Contract Health Services Delivery Areas (CHSDA counties);16 2016 data were not available for AIANs as CDC WONDER does not provide a restriction to these counties. Estimates and projections of yearly U.S. population by age, sex, and race/ethnicity were obtained from the Census Bureau.17 Institutional Review Board approval was unnecessary for this study as all data are de-identified and publicly available.
Statistical Methods
Age-period-cohort methods18,19 were used to model observed all-cause and cause-specific mortality rates during 1990–2016 (1990–2015 for AIANs) by sex and race/ethnicity, and to forecast 2017–2030 rates. These dynamic models are appropriate as there have been notable age and birth-cohort trends in U.S. premature mortality rates.7 We estimate age- and period-specific rates through a log-linear Poisson model as a product of three factors: a longitudinal mortality rate for a reference birth cohort, a rate-ratio relative to this cohort, and an age-invariant period adjustment. Although age, period, and cohort are nonidentifiable, this model estimates identifiable and interpretable parameters. Our forecast projects rates for future periods using these multiplicative factors as estimated using the observed data; rates in future periods are estimated as the product of the longitudinal mortality rate, the cohort rate-ratio (CRR), and a second-order period effect. For partially-observed birth cohorts, we use the estimated CRR, and ratios for unobserved cohorts are projected using the last segment of a JoinPoint piecewise linear model fit to the logarithm of the observed CRR curve20. All estimates were age-standardized to the 2000 US population in 5-year age-groups, and annual-percent-changes in observed and forecasted rates were calculated. Full detail on model parametrization and assumptions, selection and validation, and rate summary calculations is available in the Appendix. We also conducted a sensitivity analysis projecting future mortality rates from the cross-sectional mortality rate and a JoinPoint of the (log) period rate-ratio curve.
Projected numbers of premature deaths (i.e., mortality burden) were calculated by multiplying mortality rates in 2017–2030 by corresponding age- and year-specific U.S. Census population projections. We defined the number of projected excess or averted deaths as the number of deaths projected to occur during 2017–2030 minus the number of deaths that would have occurred if rates remained stable at the most recently observed levels (AIANs: 2015, others: 2016), the latter estimated by multiplying 2015/16 rates by population size projections during 2017–2030, stratified by age, sex and race/ethnicity. We also estimated years of potential life lost (YPLL), a complementary estimate of premature mortality that weights younger deaths more heavily, by multiplying age-specific mortality burden by the difference between age 65 and the age-at-death. Finally, to estimate the impact of a hypothetical public health intervention that could reduce accidental deaths, we reduced the projected 2018–2030 accidental death rates by 2%/year (reduction of 26% by 2030). Analyses were conducted with MATLAB version R2017a;21 code is available from the authors upon request.
Role of the Funding Source
The funder reviewed the final version of the manuscript but had no role in the design, conduct, or reporting of this study. AFB had full access to all data and final responsibility to submit for publication.
Results
All-Cause Death Rates
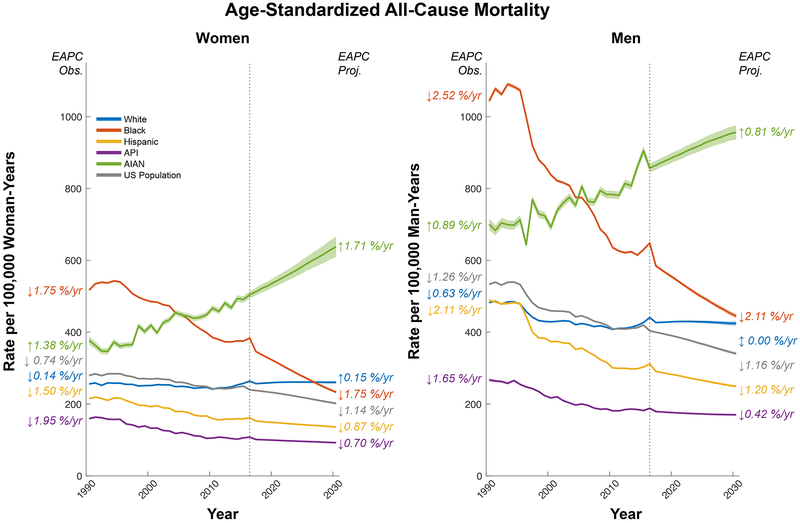
During 2017–2030, U.S. premature death rates are projected to decrease among women (2016: 249∙9/100,000; 2030: 201∙8/100,000) and men (419∙6/100,000; 340∙3/100,000); however, notable racial/ethnic differences in mortality trends are expected (Figure-1, Table-S1). During 1990–2016, all-cause premature death rates declined among black, Hispanic and API women and men. These declines are projected to continue to decrease through 2030. The largest declines (1∙2–3∙0%/year) are projected to occur in black women (ASRs: 2016: 383∙7/100,000; 2030: 232∙9/100,000), black men (647∙8/100,000; 444∙7/100,000) and Hispanic men (311∙6/100,000; 249∙4/100,000). By these estimates, APIs are projected to have the lowest death rates across the time period (2030: women: 92∙6/100,000, men: 170∙2/100,000). Among black men, the projected 2030 death rate among 45–54-year-olds (434∙3/100,000) will fall nearly to the death rate in 25–34-year-olds in 1990 (422∙2/100,000; Table-S2). Compared to the mortality burden estimated with 2016 rates, projected rates will result in 445,100 fewer deaths among blacks, 296,300 among Hispanics, and 48,400 among APIs during 2015–2030 (Table-1, Figure-S5).
Figure 1).
Observed and projected age-standardized all-cause mortality rates for ages 25 – 64 among Whites (blue), Blacks (red), Hispanics (gold), Asians and Pacific Islanders (API, purple), American Indians and Alaskan Natives (AIAN, green), and the US population as a whole (US Population, grey). Left panel displays rates for women, right panel displays rates for men. Observed rates are shown for 1990–2015 for AIANs and the US Population, and 1990–2016 for all other groups, and projected rates to 2030. Vertical dotted reference at 2016 marks end of observation period. Annotations indicate estimated annual percent change (EAPC) during the observed and projected time periods.
Table 1).
Total number of projected deaths between 2017 and 2030 among individuals aged 25–64 at the most recent observed rate (2016 for AIANs, 2017 for all other groups) and at the model-projected rate, with excess or reduction in deaths in the projection relative to the observed rate. Counts are given by sex, race, and cause of death, estimates rounded to the nearest 100 deaths and 1%.
| Women | Men | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| White | Black | Hispanic | Asian/ Pacific Islander |
American Indian/ Alaska Native |
Total | White | Black | Hispanic | Asian/ Pacific Islander |
American Indian/ Alaska Native |
Total | ||
| 2017–2030 Deaths at Most Recent Observed Rate | Accidents | 262500 | 46500 | 36400 | 5900 | 7000 | 603600 | 603600 | 123100 | 135600 | 15000 | 16700 | 894000 |
| Suicides | 82200 | 5100 | 8100 | 3700 | 1400 | 247100 | 247100 | 21000 | 35100 | 9700 | 4300 | 317200 | |
| Cancer | 733600 | 197400 | 132700 | 51900 | 9000 | 846000 | 846000 | 200700 | 142700 | 47500 | 10200 | 1247100 | |
| Heart Disease | 325500 | 143600 | 47900 | 11000 | 6000 | 778600 | 778600 | 248100 | 132100 | 34300 | 13800 | 1206900 | |
| Chronic Liver Disease/Cirrhosis | 80600 | 11700 | 18600 | 1300 | 6100 | 150700 | 150700 | 20100 | 55900 | 4000 | 8800 | 239500 | |
| All | 2287600 | 704500 | 388700 | 106100 | 47300 | 3745100 | 3745100 | 1048900 | 767000 | 159800 | 83000 | 5803800 | |
| 2017–2030 Deaths at Projected Rates | Accidents | 337400 | 37900 | 34500 | 4400 | 8200 | 639500 | 639500 | 79900 | 100600 | 11400 | 15100 | 846500 |
| Suicides | 88100 | 4400 | 7900 | 4000 | 2100 | 259400 | 259400 | 16900 | 29900 | 9200 | 4500 | 319900 | |
| Cancer | 657700 | 165300 | 116700 | 41100 | 9800 | 760000 | 760000 | 145300 | 128600 | 39400 | 12100 | 1085400 | |
| Heart Disease | 349100 | 124800 | 42300 | 9100 | 8400 | 719700 | 719700 | 204200 | 114300 | 31400 | 15100 | 1084700 | |
| Chronic Liver Disease/Cirrhosis | 90400 | 6400 | 15700 | 1300 | 7400 | 140500 | 140500 | 8500 | 38700 | 3500 | 9900 | 201100 | |
| All | 2508700 | 574000 | 328400 | 85700 | 64100 | 3589000 | 3589000 | 734300 | 531000 | 131800 | 84800 | 5070900 | |
| Deaths Averted or in Excess: 2017–2030 (Percentage difference from observed-rate projection) | Accidents | 74900 (↑29%) |
−8600 (↓18%) |
−1900 (↓5%) |
−1500 (↓25%) |
1200 (↑17%) |
64100 (↑18%) |
35900 (↑6%) |
−43200 (↓35%) |
−35000 (↓26%) |
−3600 (↓24%) |
−1600 (↓10%) |
−47500 (↓5%) |
| Suicides | 5900 (↑7%) |
−700 (↓14%) |
−200 (↓2%) |
300 (↑8%) |
700 (↑50%) |
6000 (↑6%) |
12300 (↑5%) |
−4100 (↓20%) |
−5200 (↓15%) |
−500 (↓5%) |
200 (↑5%) |
2700 (↑1%) |
|
| Cancer | −75900 (↓10%) |
−32100 (↓16%) |
−16000 (↓12%) |
−10800 (↓21%) |
800 (↑9%) |
−134000 (↓12%) |
−86000 (↓10%) |
−55400 (↓28%) |
−14100 (↓10%) |
−8100 (↓17%) |
1900 (↑19%) |
−161700 (↓13%) |
|
| Heart Disease | 23600 (↑7%) |
−18800 (↓13%) |
−5600 (↓12%) |
−1900 (↓17%) |
2400 (↑40%) |
−300 (↓0%) |
−58900 (↓8%) |
−43900 (↓18%) |
−17800 (↓13%) |
−2900 (↓8%) |
1300 (↑9%) |
−122200 (↓10%) |
|
| Chronic Liver Disease/Cirrhosis | 9800 (↑12%) |
−5300 (↓45%) |
−2900 (↓16%) |
0 | 1300 (↑21%) |
2900 (↑2%) |
−10200 (↓7%) |
−11600 (↓58%) |
−17200 (↓31%) |
−500 (↓13%) |
1100 (↑13%) |
−38400 (↓16%) |
|
| All | 221100 (↑10%) |
−130500 (↓19%) |
−60300 (↓16%) |
−20400 (↓19%) |
16800 (↑36%) |
26700 (↑1%) |
−156100 (↓4%) |
−314600 (↓30%) |
−236000 (↓31%) |
−28000 (↓18%) |
1800 (↑2%) |
−732900 (↓13%) |
|
Overall, premature mortality rates among whites declined during 1990–2016, and are projected to remain stable through 2030 (women: 2016: 263∙8/100,000; 2030: 260∙4/100,000. men: 2016: 440∙5/100,000; 2030: 424∙4/100,000, Figure-1; Table-S1). Trends within age-groups are projected to continue to diverge, increasing among 25–44-year-olds and mostly decreasing among 45–64-year-olds (Figure-S1/S2, Table-S2), resulting in a net 156,100 fewer and 221,100 excess deaths during 2017–2030 among white men and women, respectively, through 2030, compared to 2016 rates (Table-1, Figure-S5). In addition, premature mortality rates for white women are projected to exceed those of black women starting in 2027, and mortality rates for white and black men will be close to convergence in 2030 (Figures 1, S1).
Projected rates in AIAN women (2015: 491∙4/100,000; 2030: 637∙8/100,000) and men (2015: 904∙9/100,000; 2030: 955∙8/100,000) will continue increasing in all age-groups (Figure-1, Table-S1), resulting in a projected 18,600 excess deaths (Table-1, Figure-S5). Projected death rates among 25–34-year-old AIAN women in 2030 (319∙0/100,000) will exceed those of 35–44-year-olds in 1990 (210∙9/100,000; Figure-S2, Table-S2). In 2030, AIAN women (637∙8/100,000) and men (955∙8/100,000) are projected to have the highest mortality rates (7 and 6-fold higher than projected for API women and men, respectively; Table-S1).
Cause-specific premature mortality projections
During 2017–2030, projected accidental death rates among women will increase among whites and AIANs, remain stable among Hispanics and blacks, and decline among APIs. Among men, accidental death rates are projected to increase most significantly in whites (Figure-2, Table-S1). In 2030, AIAN women (ASR=97∙5/100,000), and AIAN men (ASR=298∙7/100,000) are projected to have the highest accidental death rates, followed by whites (women: 60∙5/100,000, men: 101∙9/100,000; Table-S3). The most rapid projected increases (70–80% by 2030) will occur among 25–44-year-old whites, and 55–64-year-old AIAN women (Table-S3). Rising accidental death rates in some groups are projected to result in a total of 1∙27 million accidental deaths during 2017–2030, compared to 1∙25 million accidental deaths over the same time period if rates remain stable (1.3% increase) (Table-1, Figure-S5).
Figure 2).
Observed and projected age-standardized cause-specific mortality rates for ages 25 – 64 for Whites (blue), Blacks (red), Hispanics (gold), Asians and Pacific Islanders (API, purple), and American Indians and Alaskan Natives (AIAN, green). Top panels display rates for women, bottom panels display rates for men. From left to right, panels display cause-specific rates for accidental death, suicide, cancer, heart disease, and liver disease. The y-axis limits vary by column; to ease comparisons across causes, common y-axis reference points every 50 deaths per 100,000 person-years are denoted by dashed horizontal reference lines. Annotations indicate estimated annual percent change (EAPC) during the observed and projected time periods, for selected causes and racial groups.
Projected suicide rates will increase in all racial/ethnic groups, with the most pronounced increases in white women (2016: 11∙7/100,000; 2030: 23∙8/100,000), AIAN women (2015: 20∙6/100,000; 2030: 27∙7/100,000), and white men (2016: 34∙8/100,000; 2030: 53∙6/100,000; Figure-2, Table-S1). A projected 426,400 suicides are expected during 2017–2030, compared to 417,700 if rates remain stable (2.1% increase) (Table-1, Figure-S5).
Chronic liver disease/cirrhosis remains a significant cause of death for AIANs, and projected mortality rates will increase among women (2015: 72∙3/100,000; 2030: 163∙4/100,000) and men (2015: 105∙6/100,000; 2030: 197∙2/100,000; Figure-2, Table-S1). In addition, projections show chronic liver disease/cirrhosis mortality rising in both sexes for almost all other racial/ethnic groups, with the most rapid increases noted in younger age-groups (Table-S5). Black men are the only group with a projected rate reduction (2016: 12∙4/100,000; 2030: 11∙8/100,000; Figure-2, Table-S1). Due to diverging trends by age, we project a net decrease in the chronic liver disease/cirrhosis mortality burden expected during 2017–2030 from 357,800 deaths if 2015/2016 rates remain stable to 322,300 deaths under projected rates (9.9% decrease) (Table-1, Figure-S5).
Projected cancer death rates will decline among white, black, Hispanic, and API women and men (Figure-2, Table-S1). The most profound decreases were forecast among black women (2016: 104∙5/100,000; 2030: 77∙1/100,000) and men (2016: 116∙8/100,000; 2030: 81∙6/100,000). In contrast, cancer death rates are projected to decline less among AIAN women (2015: 89∙3/100,000; 2030: 70∙4/100,000) and men (2015: 107∙4/100,000; 2030: 92∙9/100,000). Declining cancer rates during 2017–2030 are projected to result in fewer deaths (2∙07 million) than expected if rates remain stable (12.5% decrease) (2∙37 million; Table-1, Figure-S5).
Projected heart disease death rates show overall decreases for white men, and black, API, and Hispanic women and men during 2017–30 (Figure-2, Table-S1). However, heart disease death rates are projected to decrease only slightly in white women (2016: 35∙6/100,000; 2030: 31∙1/100,000) and AIAN women (2015: 64∙4/100,000; 2030: 62∙8/100,000) and increase in AIAN men (2015: 150∙9/100,000; 2030: 175∙9/100,000) across age-groups. During 2017–2030, 1∙62 million premature heart diseases deaths are expected to occur based on projected rates, compared to the 1∙74 million deaths estimated with stable rates (7% decrease) (Table-1, Figure-S5).
Years of Potential Life Lost
In 2030, projected accidental deaths will account for the largest proportion of YPLL among white women (26%) and men (35%), AIAN women (16%) and men (24%), and Hispanic men (31%), projected cancer deaths among black (25%), Hispanic (32%), API women (43%), and API men (23%), and projected heart disease deaths among black men (23%) (Figures 3, S6, Table-S9).
Figure 3).
Observed and projected proportion of total annual person-years of life lost to age 65 due to accidental death (orange), suicide (light green), cancer (dark green), heart disease (blue), and liver disease (purple). Top panels display mortality for women, bottom panels display mortality for men. From left to right, panels display mortality proportions for Whites, Blacks, Hispanics, Asians and Pacific Islanders (API), and American Indians and Alaska Natives (AIAN).
Sensitivity Analysis on Recent Period Trends
Substantial period increases in accidental and all-cause mortality during 2014–2016, across ages and racial groups. As a sensitivity analysis, we projected based primarily on these recent period trends (Figure-S13), which predict substantial increases in the corresponding mortality rates.
Impact of Accidental Death Reductions
Public health interventions leading to an overall 2%/year reduction in projected accidental deaths would have the largest effect in whites, resulting in 131,500 fewer accidental deaths during 2017–2030 (Figure 4). An additional 19,900 accidental deaths among blacks, 20,300 among Hispanics, 2,800 among APIs and 4,200 among AIANs would also be averted. Reductions in accidental death rates would also eliminate the projected increase in all-cause mortality among AIAN men and 25–44-year-old white women and men, but not AIAN women, where other causes of death contribute significantly.
Figure 4).
Observed and projected 1990 – 2030 age-standardized cause-specific mortality rates for persons ages 25 – 64, for Whites (blue), Blacks (red), Hispanics (gold), Asians and Pacific Islanders (API, purple), and American Indians and Alaskan Natives (AIAN, green) aged. Top panels display rates for women, bottom panels display rates for men. Dashed curves show estimates based on optimistic projections (2%/yr reduction in future mortality due to accidental death); solid curves show estimates based on base-case projections. Left panels show estimates for accidental death, right panels show estimates for all causes combined.
Discussion
According to our projections extrapolated from observed age and birth-cohort trends in mortality, the unexpected divergence of premature death rate trajectories by race/ethnicity and sex will become more prominent in the coming decade. Projected increases in premature death rates among white women and AIANs are estimated to cause an additional 239,700 premature deaths during 2017–2030 relative to expected deaths if rates remain constant at 2015/16 levels – an increase of 10%. In contrast, continued declines in white men and black, Hispanic and API men and women are expected to result in 945,900 fewer premature deaths during the same time period - a reduction of 14%. The largest increases in projected death rates are due to accidental deaths;7 cancer death rates will have the largest declines.
If current trends continue, rising accidental death rates in whites and AIAN women will cause 112,000 additional premature deaths during 2017–2030. These increases are driven by opioid and other drug poisonings, as deaths due to motor vehicle accidents have declined steadily over time.7 Large increases in rates of drug poisoning mortality from 2014–2016 add further urgency. Immediate intervention is needed to prevent these dire increases. Federal legislation on addiction was signed into law in July 2016, focusing on prevention, education, treatment and recovery.22 Our analyses show that if newly introduced or expanded and sustainable public health interventions could successfully reduce accident-related mortality by 2%/year, 178,700 deaths would be averted during 2017–2030, and the projected increase in all-cause mortality rates among AIANs and young whites would be eliminated.
Suicide and chronic liver disease/cirrhosis deaths are also projected to increase through 2030 in some racial/ethnic groups. Suicide increases are unlikely to be driven by miscoded opioid overdoses, as only 4% of suicides in 2014 were opioid-related.24 Chronic liver disease/cirrhosis mortality has multiple causes, predominantly non-alcoholic fatty liver disease, alcoholic liver disease and hepatitis C virus, which may be attributable to risk factors such as obesity, alcohol use and injection drug use.25 As ≥70% of cirrhosis deaths among 25–44-year-olds are due to alcohol,26 recent increases in alcohol use/abuse may have contributed.27 If these increases continue unabated, an additional 19,100 suicides and 11,200 chronic liver disease/cirrhosis deaths will occur among whites and AIANs during 2017–2030 over what is expected based on 2015/16 rates.
We predict decades-long progress in preventing cancer and heart disease deaths will continue in most groups,6 with 295,700 fewer deaths during 2017–2030 relative to 2015/16 rates. Declines in cancer mortality have largely been attributable to decreases in cigarette smoking, increases in cancer screening, reduced surgical mortality and advances in therapy.28 Declines in heart disease mortality have largely been attributed to decreases in risk factors and advances in medical and surgical treatment.29–31 It is plausible that premature cancer and heart disease mortality will continue to improve given sustained declines in smoking, cholesterol and hypertension,30,32 and presumed future advances in medical care and treatment. However, premature heart disease death rates are projected to increase in white and AIAN women and young white, Hispanic, and API men, potentially due to increases in obesity and diabetes.28,31 Additionally, prescription opioids increase risk of non-overdose-related cardiovascular disease death.33
We have projected that, circa 2027, premature mortality rates among white women will be higher than black women and close to convergence for white and black men in 2030, a combination of increases in death rates among whites and continuing declines among blacks. Importantly, declines in HIV deaths, a cause of death not specifically examined here, have had a large impact on premature mortality rates among blacks.7 Nonetheless, substantial health disparities will remain between blacks and other race/ethnicities. Projected 2030 all-cause death rates will be 2–3 times higher in blacks than Hispanics and APIs. Further, projected cancer and heart disease death rates among blacks will remain higher than whites, reflecting differences in both disease incidence and survival. Blacks have a higher burden of chronic disease risk factors (e.g., obesity, diabetes),34,35 unequal access to preventive interventions (e.g., statins, cancer screening) and differences in treatment receipt and timeliness.28,31,36,37 Our analysis forecasts rates for ages 25–64, and does not project future racial/ethnic health disparities among those younger or older. Increased efforts targeted toward black communities to address chronic disease risk factors, as well as increases in access to affordable healthcare, are needed to address these disparities.
Projected premature mortality rates appear particularly grim for AIANs. AIANs who are enrolled in a federally-recognized tribe can access healthcare through the federally-funded Indian Health Service (IHS); thus, policy decisions impacting access and delivery can be measured in the health of the population. For example, policies and funding devoted to specific diabetes programs within the IHS were initiated in 1997, resulting in a 54% decrease in diabetes-related end-stage renal disease during 1996–2013,38 and radically reducing diabetes mortality.39 The projected premature mortality in AIANs will require substantial public health efforts to reverse, with focus on behavioral health and treatment for alcohol and opioid substance use disorder, as well as continued work in preventative healthcare. Currently, there are innovations with telehealth to improve treatment and management of liver disease in tribal areas and training for opioid substance use disorder, but it is too early to assess outcomes.40,41 In addition, the Affordable Care Act expanded Medicaid with increased coverage for AIANs; this has provided IHS with needed revenue for clinical services. Although the impact of this policy change is yet to be observed in the AIAN population health, with one-third of the AIAN population receiving Medicaid coverage, it is expected that there will be measurable health benefits, potentially slowing or reversing mortality trends42,43, although such benefits would be affected by changes in Medicaid funding and coverage.
The main strengths of this analysis are the use of data from all deaths that occurred in the U.S. population during 1990–2015/16, and the use of age-period-cohort forecasting methods that account for different trends across age-groups that are a consequence of birth-cohort effects. While these models fit the observed data well, our projections are dependent on model assumptions, and do not consider the possible effects of already-implemented interventions that have not yet reached full effectiveness, nor of potential future interventions or catastrophes, though they offer a plausible estimate of the future if cohort patterns continue on the same trajectory as observed. Our analysis is limited by its reliance on death certificates for cause of death and race/ethnicity data;44,45 however, the CDC mortality database provides the most comprehensive available information on deaths in the United States. The reported uncertainty in our projections reflects that of our model; additional uncertainty is always inherent in projections due to the potential for unforeseen events. We were unable to obtain 2016 rates on AIANs specific to CHSDA counties through CDC WONDER. Finally, future mortality among Hispanics and APIs may be influenced by future immigration patterns, given the large fractions of foreign-born people (34 and 67%, respectively) in these groups.46
Our methods provide forecasts based on observed long-term cohort trends and second-order period effects. Therefore, our forecasts are less reflective of very recent period changes – for example, rapid accidental mortality increases in whites, blacks, and Hispanics during 2014–2016 (Figure-2). In our primary model, these are included as a higher-order period effect on the observed periods only; this causes a gap from the 2016 observed and 2017 forecast rates (Figures 1,2). It is impossible to know whether these increases represent a temporary perturbation or whether they are a harbinger of large future mortality increases. Our sensitivity analyses include a projection based primarily on period trends, which suggests potentially very large and worrisome future increases in accidental deaths in whites, blacks, and Hispanics. In light of these projections, reports of increasing contamination of cocaine and heroin with fentanyl47,48 are of grave concern, and recent preliminary data indicate that continued short-term increases are likely49. Future descriptive studies tracking trends in accidental deaths over the next several years will be of critical importance.
Based upon recent trends, we have projected substantial increases in death rates among AIANs and younger whites through 2030. These increasing mortality rates are unusual and alarming, given that life expectancy is generally projected to increase worldwide.3 The largest driver of these increases is the ongoing drug epidemic. Interventions aimed at curbing drug overdoses could prevent deaths across all demographic groups, and would have a substantial impact on mitigating expected future mortality. Although, recent increases in accidental mortality deaths from 2014–2016 suggest worsening rather than improving trends. Rapid and effective interventions to address rapidly rising rates of deaths due to drug poisonings, suicide and chronic liver disease/cirrhosis, and sustained prevention and treatment efforts toward continued reductions in cancer and heart disease deaths are urgently needed to prevent future premature deaths.
Supplementary Material
Research in Context
Evidence before this study
Since 1980, mortality rates have decreased and life expectancy has increased across most countries. However, in the U.S. since 2000, increases in premature mortality have been reported in some groups of non-Hispanic whites and American Indians/Alaska Natives, mainly due to rising rates of accidental deaths (primarily drug poisonings), suicides, and chronic liver disease and cirrhosis. This contrasts with continued decreases in mortality in other countries and among US non-Hispanic blacks, Hispanics and Asian/Pacific Islanders. We searched PubMed on May 10, 2018, with MeSH search terms (“Life Expectancy” OR “Mortality, Premature” or “Death Rate”) AND (“Forecasting” or “Projection, Population”) AND “United States”, restricting to articles published since 2010. Of the 31 listed items, 1 contained mortality rate or burden forecasts to at least 20201,2 but did not provide age-specific rate or burden predictions, and focused only on cancer and heart disease mortality in whites and blacks.
Added value of this study
In contrast to prior studies that have focused on observed historical trends in mortality rates, this study focuses on projecting premature mortality trends through 2030 using age-period-cohort models. These projections highlight future increases in premature mortality rates if current trends continue by sex, race/ethnicity, age, and major causes of premature death. In addition, we estimated the total number of deaths projected to occur, and the projected number of potential years of life lost due to premature mortality. We also estimated the impact of a hypothetical public health intervention which would reduce accidental death rates by 2% per year from the base-case projections, on all-cause mortality rates and the total number of projected deaths.
Implications of all the available evidence
Based on our projections that take into account contemporary birth-cohort trends in premature mortality, we expect the observed divergence in mortality trajectories by race and ethnicity to continue. In particular, we expect that mortality rates will continue to increase among American Indians/Alaska Natives and non-Hispanic white women through 2030, and continue to decline among non-Hispanic blacks, Asian/Pacific Islanders, Hispanics, and non-Hispanic white men. The largest increases in premature mortality rates are projected for accidental deaths, and the largest decreases for cancer deaths. Reductions of 2% per year in accidental death rates would avert an expected 178,700 deaths. Unfortunately, however, recent period increases in accidental deaths from 2014–2016 suggest that such reductions in accidental death rates are unlikely, at least over the next few years. Swift and effective interventions are needed to halt the rapid rise of death rates due to drug poisonings, suicide, and chronic liver disease, in addition to sustained prevention and treatment efforts to continue reductions in cancer and heart disease mortality.
Acknowledgments
This work was funded by the Intramural Research Program of the US National Cancer Institute.
Funding: National Cancer Institute Intramural Research Program
Figure 4) (Table Panel). Reduction in accidental deaths between 2017 and 2030 due to a 2%/year reduction in projected accidental deaths.
| White | Black | Hispanic | Asian/Pacific Islander | American Indian/Alaska Native | |
|---|---|---|---|---|---|
| Women | 46448 | 5820 | 3278 | 216 | 1100 |
| Men | 85044 | 14043 | 17041 | 2596 | 3106 |
Footnotes
Declaration of Interest
We declare no competing interests.
References
- 1.Weir HK, Anderson RN, Coleman King SM, et al. Heart Disease and Cancer Deaths - Trends and Projections in the United States, 1969–2020. Prev Chronic Dis 2016; 13: E157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bradley CJ, Yabroff KR, Dahman B, Feuer EJ, Mariotto A, Brown ML. Productivity costs of cancer mortality in the United States: 2000–2020. J Natl Cancer Inst 2008; 100(24): 1763–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mortality GBD, Causes of Death C. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016; 388(10053): 1459–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kontis V, Bennett JE, Mathers CD, Li G, Foreman K, Ezzati M. Future life expectancy in 35 industrialised countries: projections with a Bayesian model ensemble. Lancet 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xu J, Murphy SL, Kochanek KD, Arias E. Mortality in the United States, 2015. NCHS Data Brief 2016; (267): 1–8. [PubMed] [Google Scholar]
- 6.Ma J, Ward EM, Siegel RL, Jemal A. Temporal Trends in Mortality in the United States, 1969–2013. JAMA 2015; 314(16): 1731–9. [DOI] [PubMed] [Google Scholar]
- 7.Shiels MS, Chernyavskiy P, Anderson WF, et al. Trends in premature mortality in the USA by sex, race, and ethnicity from 1999 to 2014: an analysis of death certificate data. Lancet 2017; 389(10073): 1043–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Case A, Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc Natl Acad Sci U S A 2015; 112(49): 15078–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rudd RA, Seth P, David F, Scholl L. Increases in Drug and Opioid-Involved Overdose Deaths - United States, 2010–2015. MMWR Morb Mortal Wkly Rep 2016; 65(5051): 1445–52. [DOI] [PubMed] [Google Scholar]
- 10.Han B, Compton WM, Jones CM, Cai R. Nonmedical Prescription Opioid Use and Use Disorders Among Adults Aged 18 Through 64 Years in the United States, 2003–2013. JAMA 2015; 314(14): 1468–78. [DOI] [PubMed] [Google Scholar]
- 11.Martins SS, Sarvet A, Santaella-Tenorio J, Saha T, Grant BF, Hasin DS. Changes in US Lifetime Heroin Use and Heroin Use Disorder: Prevalence From the 2001–2002 to 2012–2013 National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Han B, Compton WM, Blanco C, Crane E, Lee J, Jones CM. Prescription Opioid Use, Misuse, and Use Disorders in U.S. Adults: 2015 National Survey on Drug Use and Health. Ann Intern Med 2017; 167(5): 293–301. [DOI] [PubMed] [Google Scholar]
- 13.National Center for Health Statistics. Mortality - All COD, Total U.S. (1990–2014, Early release with Vintage 2014 Katrina/Rita Population Adjustment) - Linked To County Attributes - Total U.S., 1969–2014 Counties. April 2016 ed.
- 14.Centers for Disease Control and Prevention. CDC WONDER Detailed Cause of Death. 2018. https://wonder.cdc.gov/ucd-icd10.html (accessed 5/7/2018.
- 15.Stein EM, Gennuso KP, Ugboaja DC, Remington PL. The Epidemic of Despair Among White Americans: Trends in the Leading Causes of Premature Death, 1999–2015. Am J Public Health 2017; 107(10): 1541–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jim MA, Arias E, Seneca DS, et al. Racial misclassification of American Indians and Alaska Natives by Indian Health Service Contract Health Service Delivery Area. Am J Public Health 2014; 104 Suppl 3: S295–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bureau USC. 2014 National Population Projections Datasets. 2014. https://www.census.gov/programs-surveys/popproj/data/datasets.html (accessed September 12 2017).
- 18.Anderson WF, Katki HA, Rosenberg PS. Incidence of breast cancer in the United States: current and future trends. J Natl Cancer Inst 2011; 103(18): 1397–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rosenberg PS, Barker KA, Anderson WF. Estrogen Receptor Status and the Future Burden of Invasive and In Situ Breast Cancers in the United States. J Natl Cancer Inst 2015; 107(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med 2000; 19(3): 335–51. [DOI] [PubMed] [Google Scholar]
- 21.MATLAB and Statistics Toolbox Release 2017a. Natick, Massachusetts: The MathWorks, Inc.; 2017. [Google Scholar]
- 22.Comprehensive Addiction and Recovery Act of 2016. 2016. https://www.congress.gov/bill/114th-congress/senate-bill/524/text (accessed 3/26/2018.
- 23.Shiels MS, Freedman ND, Thomas D, Berrington de Gonzalez A. Trends in U.S. Drug Overdose Deaths in Non-Hispanic Black, Hispanic, and Non-Hispanic White Persons, 2000–2015. Ann Intern Med 2018; 168(6): 453–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Braden JB, Edlund MJ, Sullivan MD. Suicide Deaths With Opioid Poisoning in the United States: 1999–2014. Am J Public Health 2017; 107(3): 421–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Setiawan VW, Stram DO, Porcel J, Lu SC, Le Marchand L, Noureddin M. Prevalence of chronic liver disease and cirrhosis by underlying cause in understudied ethnic groups: The multiethnic cohort. Hepatology 2016; 64(6): 1969–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yoon Y-HC CM Liver Cirrhosis mortality in the United States: National, state, and regional trends, 2000–2013, 2016.
- 27.Grant BF, Chou SP, Saha TD, et al. Prevalence of 12-Month Alcohol Use, High-Risk Drinking, and DSM-IV Alcohol Use Disorder in the United States, 2001–2002 to 2012–2013: Results From the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry 2017; 74(9): 911–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jemal A, Ward EM, Johnson CJ, et al. Annual Report to the Nation on the Status of Cancer, 1975–2014, Featuring Survival. J Natl Cancer Inst 2017; 109(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ford ES, Ajani UA, Croft JB, et al. Explaining the decrease in U.S. deaths from coronary disease, 1980–2000. N Engl J Med 2007; 356(23): 2388–98. [DOI] [PubMed] [Google Scholar]
- 30.Yang Q, Cogswell ME, Flanders WD, et al. Trends in cardiovascular health metrics and associations with all-cause and CVD mortality among US adults. JAMA 2012; 307(12): 1273–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mensah GA, Wei GS, Sorlie PD, et al. Decline in Cardiovascular Mortality: Possible Causes and Implications. Circ Res 2017; 120(2): 366–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jamal A, King BA, Neff LJ, Whitmill J, Babb SD, Graffunder CM. Current Cigarette Smoking Among Adults - United States, 2005–2015. MMWR Morb Mortal Wkly Rep 2016; 65(44): 1205–11. [DOI] [PubMed] [Google Scholar]
- 33.Ray WA, Chung CP, Murray KT, Hall K, Stein CM. Prescription of Long-Acting Opioids and Mortality in Patients With Chronic Noncancer Pain. JAMA 2016; 315(22): 2415–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ogden CL, Carroll MD, Fryar CD, Flegal KM. Prevalence of Obesity Among Adults and Youth: United States, 2011–2014. NCHS Data Brief 2015; (219): 1–8. [PubMed] [Google Scholar]
- 35.Centers for Disease Control and Prevention NCfHS. Age-Adjusted Rates of Diagnosed Diabetes per 100 Civilian, Non-institutionalized Population, by Race and Sex, United States, 1980–2014. December 1, 2015 2015. https://www.cdc.gov/diabetes/statistics/prev/national/figraceethsex.htm (accessed July 20 2017).
- 36.Gillum RF, Mehari A, Curry B, Obisesan TO. Racial and geographic variation in coronary heart disease mortality trends. BMC Public Health 2012; 12: 410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Singh GK, Jemal A. Socioeconomic and Racial/Ethnic Disparities in Cancer Mortality, Incidence, and Survival in the United States, 1950–2014: Over Six Decades of Changing Patterns and Widening Inequalities. J Environ Public Health 2017; 2017: 2819372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bullock A, Burrows NR, Narva AS, et al. Vital Signs: Decrease in Incidence of Diabetes-Related End-Stage Renal Disease among American Indians/Alaska Natives - United States, 1996–2013. MMWR Morb Mortal Wkly Rep 2017; 66(1): 26–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jiang L, Manson SM, Beals J, et al. Translating the Diabetes Prevention Program into American Indian and Alaska Native communities: results from the Special Diabetes Program for Indians Diabetes Prevention demonstration project. Diabetes Care 2013; 36(7): 2027–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Katzman JG, Fore C, Bhatt S, et al. Evaluation of American Indian Health Service Training in Pain Management and Opioid Substance Use Disorder. Am J Public Health 2016; 106(8): 1427–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Weahkee RM. Statement of the Indian Health Service. Senate Appropriations Subcommittee on Interior, Environment and Related Agencies: Department of Health and Human Services; 2017. [Google Scholar]
- 42.Artiga SD A Medicaid and American Indians and Alaska Natives. Menlo Park, CA, 2016. [Google Scholar]
- 43.Warne DD D; Angus-Hornbuckle C; Shelton BL Impact of ACA repeal on American Indians and Alaska Natives: Robert Wood Johnson Foundation and the Montanta Healthcare foundation, 2017.
- 44.Noymer A, Penner AM, Saperstein A. Cause of death affects racial classification on death certificates. PLoS One 2011; 6(1): e15812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Arias EH M; Hakes JK The validity of race and Hispanic-origin reporting on death certificates in the United States: An update. Hyattsville, Maryland: National Center for Health Statistics, 2016. [PubMed] [Google Scholar]
- 46.Lopez G, Radford J. Facts on U.S. Immigrants, 2015: Statistical portrait of the foreign-born population in the United States. 5/3/2017 2017. http://www.pewhispanic.org/2017/05/03/facts-on-u-s-immigrants-current-data/ (accessed 3/26/2018.
- 47.Centers for Disease Control and Prevention. Fentanyl involved in over half of opioid overdose deaths in 10 states. 2017.
- 48.Bebinger M Fentanyl-Laced Cocaine Becoming A Deadly Problem Among Drug Users. Health Shots: Health News from National Public Radio. 2018 3/29/2018. [Google Scholar]
- 49.Ahmad FB, Bastian B. Quarterly provisional estimates for selected indicators of mortality, 2016-Quarter 4, 2017: National Center for Health Statistics. National Vital Statistics System, Vital Statistics Rapid Release Program, 2018.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.