Key Points
Question
Is concern about increasing discrimination in society associated with behavioral health outcomes among adolescents?
Findings
In this cohort survey of 2572 adolescents, self-reported level of concern about increasing societal discrimination was associated with higher frequency of substance use, a greater number of different substances used, and 11% higher odds of depression and 12% greater odds of attention-deficit/hyperactivity disorder symptoms.
Meaning
Public health and policy interventions may be warranted to address the potential adverse effect of increasing public expressions of discrimination on adolescent behavioral health.
This cohort survey assesses whether self-reported concern about societal discrimination and the magnitude of increased concern are associated with behavioral health outcomes among adolescents.
Abstract
Importance
Public expressions of discrimination may generate stress and behavioral health problems, particularly in racial/ethnic minority or socioeconomically disadvantaged youths.
Objectives
To determine whether concern about increasing discrimination in society reported among adolescents during 2016 and the magnitude of increase in concern from 2016 to 2017 were associated with behavioral health outcomes by 2017 and to examine racial/ethnic or socioeconomic differences in associations.
Design, Setting, and Participants
This prospective cohort survey collected data at baseline from January 2 through September 28, 2016 (11th grade), and at follow-up from January 1 through August 10, 2017 (12th grade), at 10 high schools in Los Angeles, California, recruited through convenience sampling. A total of 2572 students completed both surveys.
Exposures
Reported concern, worry, or stress regarding “increasing hostility and discrimination of people because of their race, ethnicity, sexual orientation/identity, immigrant status, religion, or disability status in society” were scored as “not at all” (0) to “extremely” (4). Mean ratings were calculated in a 3-item composite (range, 0-4).
Main Outcomes and Measures
Self-reported days of cigarette, alcohol, or marijuana use in the past month (range, 0-30 days), number of substances used in the past 6 months (range, 0-27), mild to moderate depression (yes or no), and attention-deficit/hyperactivity disorder (ADHD) (yes or no) at follow-up.
Results
The sample of 2572 students (54.4% female; mean [SD] baseline age, 17.1 [0.4] years; 1969 [87.7%] had at least 1 parent with high school diploma) included 2530 with race/ethnicity data (1198 [47.4%] Hispanic; 482 [19.0%] Asian; 104 [4.1%] African American; 155 [6.1%] multiracial; 419 [16.6%] white; 172 [6.8%] other). Appreciable numbers of students reported feeling very or extremely concerned (baseline, 1047 [41.5%]; follow-up, 1028 [44.6%]), worried (baseline, 743 [29.7%]; follow-up, 795 [34.7%]), or stressed (baseline, 345 [13.9%]; follow-up, 353 [15.5%]) about increasing societal discrimination. Each 1-SD increase on the societal discrimination concern composite in 2016 was associated with more days of past-month cigarette (incidence rate ratio [IRR], 1.77; 95% CI, 1.42-2.20; P < .001), marijuana (IRR, 1.13; 95% CI, 1.01-1.26; P = .03), and alcohol (IRR, 1.11; 95% CI, 1.02-1.21; P = .01) use, more substances used (IRR, 1.07; 95% CI, 1.01-1.17; P = .04), and greater odds of depression (odds ratio [OR], 1.11; 95% CI, 1.01-1.23; P = .04) and ADHD (OR, 1.12; 95% CI, 1.01-1.26; P = .04) symptoms in 2017. The magnitude of increase in societal discrimination concern from 2016 to 2017 was also associated with several behavioral health problems in 2017; some associations were amplified among teenagers who were African American (IRR for cigarette smoking, 2.97; 95% CI, 1.45-6.09) or Hispanic (IRR for cigarette smoking, 1.30; 95% CI, 1.09-1.54) or had parents with less educational attainment (IRR for alcohol use, 1.41 [95% CI, 1.14-1.74]; OR for ADHD, 1.81 [95% CI, 1.13-2.89]).
Conclusions and Relevance
Concern over societal discrimination was common among youths in Los Angeles in 2016 and was associated with behavioral health problems 1 year later. Adolescents’ behavioral responses to recent societal expressions of discrimination may warrant public health attention.
Introduction
Public expressions of resentment, discrimination, and hostility toward minority and disadvantaged populations have become increasingly prominent.1 Several events leading up to 2016 exemplify such trends, including highly publicized incidents of police violence toward racial/ethnic minorities, backlash against same-sex marriage legislation, and the largest number of hate crimes against American Muslims since the period immediately following September 11, 2001.2,3,4 The social climate intensified during 2016 and 2017, when the Trump presidential campaign and administration released several statements and social policy proposals perceived by many as discriminatory. Because polarizing societal events have historically been linked with stress and behavioral health problems,5,6,7 the ramifications of recent discrimination-associated societal events may be a public health concern, particularly for vulnerable populations, such as adolescents.
Whether the extent of concern adolescents attribute to increasing discrimination in society is of an appreciable level to heighten risk of behavioral health problems is unknown. Concern over societal discrimination could cause distress, impair concentration, and lead to hopelessness about the future among teenagers on the cusp of adulthood, especially among racial/ethnic minority and socioeconomically disadvantaged youths who may be worried about being directly targeted by discrimination. Distress, concentration impairment, and hopelessness increase the incidence, persistence, and exacerbation of behavioral health problems that are prevalent in late adolescence, including substance use, depression, and attention-deficit/hyperactivity disorder (ADHD).8,9,10,11,12,13
If concern over societal discrimination is common among adolescents and associated with adverse behavioral health outcomes, preventive measures to protect the current generation of youth exposed to public expressions of hostility and discrimination toward minority populations may be warranted. This study investigated whether concern over increasing discrimination in society reported among 11th grade students in Los Angeles, California, during 2016 and the magnitude of increase in concern from 2016 to 2017 were associated with behavioral health outcomes by 2017 and whether associations were amplified among youth from racial/ethnic minority groups or youth with less educated parents.
Methods
Participants and Procedures
Data were drawn from a prospective cohort survey of behavioral health, which enrolled students from urban and suburban public high schools in Los Angeles County in 2013.14 Approximately 40 public high schools in the Los Angeles metropolitan region were contacted about participating in this study because of their diverse demographic characteristics and proximity to the study institution. Ten schools agreed to participate (school characteristics in context of Los Angeles city public schools appear in eTable 1 in the Supplement). All 9th grade students in standard educational programming within these schools in 2013 who provided assent and who had written or verbal parental consent were eligible to join the cohort. The institutional review board of the University of Southern California approved the study.
Paper-and-pencil surveys were administered semiannually in classrooms from 9th through 12th grade. Students not in class during data collections completed abbreviated surveys by telephone, Internet, or mail that included only behavioral health measures. The measure involving concern over societal discrimination was included in the full-length baseline survey from January 2 through September 28, 2016 (11th grade), and the 12-month follow-up survey from January 1 through August 10, 2017 (12th grade).
Measures
Societal Discrimination Concern
In 3 separate items, students rated their level of concern, worry, or stress regarding “increasing hostility and discrimination of people because of their race, ethnicity, sexual orientation/identity, immigrant status, religion, or disability status in society” (scored 0 for “not at all”; 1 for “slightly”; 2 for “somewhat”; 3 for “very”; and 4 for “extremely”). We calculated the mean of the 3 ratings to quantify the overall magnitude of societal discrimination concern (range, 0-4) in a composite index that had high internal consistency at baseline (Cronbach α = 0.88) and follow-up (Cronbach α = 0.90). Difference scores were also computed (follow-up – baseline) to operationalize the change in societal discrimination concern level from 2016 to 2017.
Substance Use
Cigarette, marijuana, and alcohol use were measured using well-validated items15,16 instructing students to select the number of days they used each substance in the past 30 days. Past 6-month use (yes or /no) of 27 different substances (eg, cigarettes, alcohol, marijuana, prescription painkillers, inhalants, ecstasy, or cocaine) were summed to create a cumulative substance use index (range, 0-27).
Mental Health
Students were administered the Center for Epidemiologic Studies Depression Scale17 appropriate for adolescent use,18 which collects past-week frequency ratings of experiencing 20 depressive symptoms (eg, sadness, sleep and appetite problems, or psychomotor slowing) on a scale of 0 to 3 (0 indicates 0 days; 3, 5-7 days). Sum scores were used to classify whether students met or exceeded the recommended screening cutoff indicative of mild to moderate depressive symptoms (score, ≥16).17 The 18-item Current Symptoms Scale–Self Report Form,19 which screens for Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition) (DSM-IV)-defined ADHD, was administered. Respondents indicated the past 6-month frequency of experiencing inattention (ie, difficulty organizing and completing tasks) and hyperactivity and/or impulsivity (ie, difficulties remaining still or with task persistence) ADHD symptoms. Consistent with DSM-IV criteria,19,20 adolescents who reported experiencing at least 6 inattention or at least 6 hyperactivity and/or impulsivity symptoms often or very often were classified positive for ADHD symptoms.
Covariates and Descriptive Measures
Covariates to address the potential confounding influence of sociodemographic variation included age, sex, race/ethnicity, and highest parental educational level, which were assessed with investigator-defined, forced-choice items (response categories are given in Table 1). Additional measures include perceived frequency of personal discrimination using the Everyday Discrimination Scale,21 reported birth country of students and their parents (United States vs other), and acculturation using the Short Acculturation Scale for Hispanic Youth22 that assesses the extent of use of non-English languages across settings (eg, at home, with friends) (sum of 1 [only another language] to 5 [only English] for 4 items; Cronbach α = 0.82).
Table 1. Sample Characteristics and Societal Discrimination Concern Composite Scores by Sociodemographic Groupa.
| Baseline Variable | Responseb | Baselinec | Changed | ||
|---|---|---|---|---|---|
| Composite Score, Mean (SD) | P Valuee | Composite Score, Mean (SD) | P Valuee | ||
| Sex, No. (%) | |||||
| Female | 1400/2572 (54.4) | 1.82 (1.20) | <.001 | 0.11 (1.27) | .05 |
| Male | 1172/2572 (45.6) | 1.24 (1.14) | 0.01 (1.24) | ||
| Age, y, No. (%) | |||||
| 16 | 1063/2518 (42.2) | 1.57 (1.19) | .17 | 0.11 (1.25) | .16 |
| 17 | 1388/2518 (55.1) | 1.56 (1.20) | 0.03 (1.27) | ||
| 18 | 67/2518 (2.7) | 1.38 (1.37) | 0.27 (1.29) | ||
| Race/ethnicity, No. (%) | |||||
| Hispanic | 1198/2530 (47.4) | 1.53 (1.21) | .01 | 0.14 (1.28) | .001 |
| Asian | 482/2530 (19.0) | 1.72 (1.15) | −0.09 (1.16) | ||
| African American | 104/2530 (4.1) | 1.54 (1.24) | 0.34 (1.04) | ||
| White | 419/2530 (16.6) | 1.42 (0.06) | 0.11 (1.07) | ||
| Multiracial | 155/2530 (6.1) | 1.66 (1.23) | −0.14 (1.17) | ||
| Otherf | 172/2530 (6.8) | 1.56 (1.21) | 0.03 (1.25) | ||
| Highest parental educational level, No. (%)g | |||||
| 8th Grade or less | 80/2244 (3.6) | 1.72 (1.13) | .66 | 0.17 (1.20) | .84 |
| Some high school | 195/2244 (8.7) | 1.67 (1.28) | 0.06 (1.34) | ||
| High school graduate | 348/2244 (15.5) | 1.53 (1.21) | 0.08 (1.34) | ||
| Some college | 430/2244 (19.2) | 1.56 (1.21) | 0.12 (1.30) | ||
| College graduate | 743/2244 (33.1) | 1.54 (1.18) | 0.03 (1.22) | ||
| Graduate degree | 448/2244 (20.0) | 1.58 (1.21) | 0.12 (1.22) | ||
| Everyday Discrimination Scale score, mean (SD)h | 8.52 (8.15) | NA | NA | NA | NA |
| Short Acculturation Scale for Youth, mean (SD)h | 16.70 (2.89) | NA | NA | NA | NA |
| Born outside United States, No. (%)h | |||||
| Student | 262 (10.5) | NA | NA | NA | NA |
| Mother | 1383 (56.3) | NA | NA | NA | NA |
| Father | 1417 (58.8) | NA | NA | NA | NA |
Abbreviation: NA, not applicable.
Calculated as the mean of concern, worry, and stress ratings (0 indicates not at all; 1, slightly; 2, somewhat; 3, very; and 4, extremely).
Denominators vary owing to nonmissing data. Percentages have been rounded and may not total 100.
Scores range from 0 to 4.
Calculated as change from baseline to 12-month follow-up. Scores range from −4 to 4.
Calculated using analysis of variance omnibus test of differences in baseline or change in societal discrimination concern composite index by sociodemographic variable.
Includes Native American or Alaskan, Native Hawaiian or Pacific Islander, and other races.
In addition to 22 students who did not respond to the survey question, 302 who marked “don’t know” are not included in the denominator.
Available (nonmissing) data range from 2409 to 2560 students.
Statistical Analysis
Negative binomial regression models23 were used to obtain incidence rate ratios (IRRs) and 95% CIs for associations of the (1) baseline societal discrimination concern composite score and (2) change in societal discrimination concern score from baseline to follow-up, with substance use outcomes at follow-up. Logistic regression was used to obtain odds ratios (ORs) and 95% CIs for associations of the baseline and change in societal discrimination concern score with ADHD and depression symptoms. For each outcome, separate models were tested for the societal discrimination concern baseline and change scores. Models were adjusted for the respective behavioral health outcome at baseline and sociodemographic covariates. To facilitate interpretation of ORs and IRRs, the societal discrimination concern composite was standardized (mean [SD], 0 [1]) for regression modeling. The χ2 difference test of goodness of fit from multigroup analysis24 was used to determine whether associations estimated in regression models differed by race/ethnicity or highest parental educational level (ie, high school graduate or higher degree vs no high school diploma). We used Mplus, version 7 (Muthen & Muthen)25 with complex analysis to account for nesting by school. The 2572 participants with data on baseline societal discrimination concern and at least 1 behavioral health outcome constituted the analytic sample. Additional missing data were managed with full-information maximum-likelihood estimation (eTable 2 in the Supplement provides numbers of participants with available data for key variables). Statistical significance was set at P < .05 (2 tailed). Benjamini-Hochberg corrections for multiple testing26 were applied for primary tests of association of baseline societal discrimination concern with outcomes. Other (secondary) tests were uncorrected. Findings from sensitivity analyses are summarized below and detailed in eMethods in the Supplement.
Results
Study Sample
Among eligible 9th grade students (N = 4100), 3396 enrolled in the cohort in 2013. Societal discrimination concern data were collected from 2735 students in 2016 (baseline), of whom 2572 (94.0%) completed follow-up (2017) (1400 female [54.4%] and 1172 male [45.6%]; mean [SD] age, 17.1 [0.4] years). eFigure 1 in the Supplement provides participant accrual details.
Descriptive Results
The sample was heterogeneous with regard to sex and parental educational level and had a plurality of Hispanic students, with an appreciable representation of students of Asian, African American, multiracial, and white race/ethnicity (Table 1). Of students with parental education data, 1969 (87.7%) reported having at least 1 parent with a high school diploma. The mean (SD) level of acculturation was moderate relative to standardized reference samples of Hispanic youth (16.70 [2.89]).22 Although most students were born in the United States, a substantial proportion of students’ parents were born outside the country (1383 mothers [56.3%] and 1417 fathers [58.8%]). Responses on the Everyday Discrimination Scale (mean [SD], 8.52 [8.15]) indicate considerable interindividual variability in the frequency of personal discrimination in the sample.
Descriptive data on depression, ADHD, and substance use at baseline and follow-up are reported in Table 2 and are commensurate with estimates in other population-based adolescent studies.27 From baseline to follow-up, increases were observed in the number of past-month days of cigarette (baseline vs follow-up mean [SD], 0.27 [2.36] vs 0.41 [2.73]), marijuana (mean [SD], 1.26 [4.55] vs 1.89 [5.76]), and alcohol (mean [SD], 0.85 [2.57] vs 1.16 [2.76]) use and number of past 6-month substances used (mean [SD], 1.57 [3.07] vs 2.01 [3.30]), whereas the prevalence of ADHD (baseline vs follow-up, 188 [7.4%] vs 174 [7.4%]) and depression symptoms (1004 [39.3%] vs 1033 [40.7%]) did not change.
Table 2. Descriptive Statistics of Societal Discrimination Concern Measure and Behavioral Health Outcomes.
| Variable | Survey, No. (%)a | P Value | |
|---|---|---|---|
| Baseline | Follow-up | ||
| 3-Item composite score, mean (SD)b | 1.56 (1.21) | 1.71 (1.24) | <.001c |
| Item Responses | |||
| Concerned | |||
| Not at all | 581 (23.0) | 467 (20.3) | .009d |
| Slightly | 294 (11.7) | 252 (10.9) | |
| Somewhat | 601 (23.8) | 555 (24.1) | |
| Very | 554 (22.0) | 558 (24.2) | |
| Extremely | 493 (19.5) | 470 (20.4) | |
| Worried | |||
| Not at all | 685 (27.4) | 579 (25.3) | .003d |
| Slightly | 434 (17.3) | 388 (17.0) | |
| Somewhat | 640 (25.6) | 527 (23.0) | |
| Very | 411 (16.4) | 459 (20.1) | |
| Extremely | 332 (13.3) | 336 (14.7) | |
| Stressed | |||
| Not at all | 1174 (47.2) | 1016 (44.7) | .005d |
| Slightly | 549 (22.1) | 484 (21.3) | |
| Somewhat | 419 (16.8) | 419 (18.4) | |
| Very | 160 (6.4) | 168 (7.4) | |
| Extremely | 185 (7.4) | 185 (8.1) | |
| Behavioral Health Outcomes | |||
| Cigarette use in the past 30 d | |||
| Mean (SD) d | 0.27 (2.36) | 0.41 (2.73) | NA |
| 0 d | 2474 (96.8) | 2415 (95.1) | <.001d |
| 1-2 d | 44 (1.7) | 53 (2.1) | |
| 3-5 d | 15 (0.6) | 23 (0.9) | |
| ≥6 d | 24 (0.9) | 48 (1.9) | |
| Marijuana use in the past 30 d | |||
| Mean (SD) d | 1.26 (4.55) | 1.89 (5.76) | NA |
| 0 d | 2180 (85.2) | 2002 (79.1) | <.001d |
| 1-2 d | 135 (5.3) | 218 (8.6) | |
| 3-5 d | 94 (3.7) | 99 (3.9) | |
| ≥6 d | 150 (5.9) | 211 (8.3) | |
| Alcohol use in the past 30 d | |||
| Mean (SD) d | 0.85 (2.57) | 1.16 (2.76) | NA |
| 0 d | 2007 (78.5) | 1753 (70.0) | <.001d |
| 1-2 d | 350 (13.7) | 507 (20.2) | |
| 3-5 d | 114 (4.5) | 139 (5.5) | |
| ≥6 d | 86 (3.4) | 107 (4.3) | |
| No. of substances used in past 6 moe | |||
| Mean (SD) | 1.57 (3.07) | 2.01 (3.30) | NA |
| 0 | 1506 (58.7) | 1285 (50.4) | <.001d |
| 1 | 341 (13.3) | 401 (15.7) | |
| 2 | 179 (7.0) | 156 (6.1) | |
| 3-5 | 320 (12.5) | 402 (15.8) | |
| ≥6 | 220 (8.6) | 308 (12.1) | |
| Depression symptomsf | 1004 (39.3) | 1033 (40.7) | .59h |
| ADHD symptomsg | 188 (7.4) | 174 (7.4) | .99h |
Abbreviations: ADHD, attention-deficit/hyperactivity disorder; NA, not applicable.
Available (nonmissing) data for variable and categorical variable denominator for within-column percentages can be found in eTable 1 in the Supplement. Unless otherwise specified, values represent No. (%). Percentages have been rounded and may not total 100.
Calculated as the mean of concern, worry, and stress ratings (0 indicates not at all; 1, slightly; 2, somewhat; 3, very; and 4, extremely).
Calculated using the paired-sample t test for mean differences between baseline and follow-up.
Calculated using the Wilcoxon matched-pair signed rank test for change in rank order between baseline and follow-up.
Answers range from 0 to 27 substances.
Measured using the Center for Epidemiologic Studies Depression Scale total score of at least 16, indicating mild to moderate levels of depressive symptoms.
Measured using the Current Symptoms Scale–Self Report Form for Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition)–defined ADHD diagnostic threshold.
Calculated using the McNemar test for change in prevalence between baseline and follow-up.
Characterization of Students’ Level of Societal Discrimination Concern
Sizeable proportions of the overall sample reported feeling very or extremely concerned (baseline, 1047 [41.5%]; follow-up, 1028 [44.6%]), worried (baseline, 743 [29.7%]; follow-up, 795 [34.7%]), or stressed (baseline, 345 [13.9%]; follow-up, 353 [15.5%]) about increasing societal discrimination; each rating increased from baseline to follow-up (Table 2). Overall concern quantified by the 3-item composite varied substantially across students and increased from baseline (mean [SD], 1.56 [1.21]) to follow-up (mean [SD], 1.71 [1.24]).
The baseline societal discrimination concern composite score and change from baseline to follow-up by race/ethnicity are reported in Table 1 and eFigure 2 in the Supplement. Societal discrimination concern composite scores did not differ by parental educational level and were modestly correlated with Everyday Discrimination Scale scores at baseline (Pearson r = 0.14; P < .001).
Associations of Societal Discrimination Concern With Behavioral Health in the Overall Sample
Primary Tests of Baseline Societal Discrimination Concern
Regression models adjusted for sociodemographic covariates and the respective outcome at baseline showed that the baseline societal discrimination concern composite score was associated with greater odds or frequency of behavioral health problems at follow-up for each outcome (Table 3 and eTable 3 in the Supplement). For example, each 1-SD increase in baseline societal discrimination concern was associated with 77% more days of past-month cigarette smoking (IRR, 1.77; 95% CI, 1.42-2.20; P < .001) and 12% greater odds of ADHD symptoms (OR, 1.12; 95% CI, 1.01-1.26; P = .04) at follow-up.
Table 3. Associations of Societal Discrimination Concern Composite Scores With Behavioral Health Outcomes.
| Outcome at Follow-up | Regressora | |||
|---|---|---|---|---|
| Baseline Scoreb | Change in Score, Baseline to Follow-upc | |||
| Estimate of Association | P Value | Estimate of Association | P Value | |
| Past-month days of cigarette use, IRR (95% CI)d | 1.77 (1.42-2.20) | <.001e | 1.18 (1.03-1.42) | .02 |
| Past-month days of marijuana use, IRR (95% CI)d | 1.13 (1.01-1.26) | .03e | 1.10 (1.01-1.21) | .04 |
| Past-month days of alcohol use, IRR (95% CI)d | 1.11 (1.02-1.21) | .01e | 1.00 (0.93-1.10) | .85 |
| Number of substances used in past 6 mo, IRR (95% CI)d | 1.07 (1.01-1.17) | .04e | 1.06 (1.01-1.13) | .04 |
| Depression symptoms, OR (95% CI)f,g | 1.11 (1.01-1.23) | .04e | 1.01 (0.92-1.10) | .87 |
| ADHD symptoms, OR (95% CI)f,h | 1.12 (1.01-1.26) | .04e | 1.06 (0.88-1.29) | .54 |
Abbreviations: ADHD, attention-deficit/hyperactivity disorder; IRR, incidence rate ratio; OR, odds ratio.
Results of regression models are adjusted for parental educational level, youth age, sex, and race/ethnicity at baseline and the respective behavioral health variable at baseline; separate models were tested for each combination of regressor and outcome. The regressor is standardized (mean, 0; SD, 1) such that ORs and IRRs can be interpreted as the difference in odds or frequency rate of outcome with 1-SD difference in the regressor.
Calculated as the mean of concern, worry, and stress ratings (0 indicates not at all; 1, slightly; 2, somewhat; 3, very; and 4, extremely).
Calculated as the change score (baseline to 12-month follow-up).
Calculated from negative binomial regression models of association with past 30-day cigarette, marijuana, or alcohol use (range, 0-30 days) or number of substances used in the past 6 months (range, 0-27) at follow-up.
Statistically significant after Benjamini-Hochberg corrections for multiple testing to control false discovery rate at .05 (based on 2-tailed corrected P value).
Calculated from binary logistic regression of association with depression and ADHD symptom status at follow-up.
Measured using positive (vs negative) screen for mild to moderate depressive symptoms or higher on the Center for Epidemiologic Studies Depression Scale.
Measured using positive (vs negative) screen for ADHD symptoms using the Current Symptoms Scale–Self Report Form for DSM-IV–defined ADHD diagnostic threshold.
Change in Societal Discrimination Concern From Baseline to Follow-up
The magnitude of change in societal discrimination concern composite score from baseline to follow-up was positively associated with cigarette smoking, marijuana use, and the number of substances used at follow-up after adjusting for sociodemographic factors and the respective baseline substance use variable (Table 3). For example, each 1-SD increase in the societal discrimination concern composite scores from baseline to follow-up was associated with 18% more days of cigarette smoking in the past month at follow-up (IRR, 1.18; 95% CI, 1.03-1.42; P = .02). Change in societal discrimination concern was not associated with alcohol use, depression, or ADHD at follow-up in the overall sample.
Differences in Associations of Societal Discrimination Concern With Behavioral Health by Race/Ethnicity and Parental Educational Level
Associations of baseline societal discrimination concern composite score with behavioral health outcomes did not significantly differ by parental educational level or race/ethnicity. The association of change in societal discrimination concern from baseline to follow-up with past-month marijuana use days at follow-up significantly differed between students with parent(s) who completed high school (IRR, 1.05; 95% CI, 0.98-1.14) vs those did not (IRR, 1.33; 95% CI, 1.08-1.65; difference in associations by parental education, P = .04). Among youths whose parent(s) did not complete high school, the estimated mean past-month days of marijuana use from these regression models was successively higher across students who, for example, reported no change (1.37 days; 95% CI, 1.18-1.51), a 2-point increase (eg, from slightly to very concerned; 2.17 days; 95% CI, 1.76-2.64), and a 4-point increase (eg, from not at all to extremely concerned; 3.36 days; 95% CI, 2.37-4.72) in the societal discrimination concern score from baseline to follow-up (Figure 1A). Among youths whose parent(s) completed high school, the estimated mean days of past-month marijuana use days at follow-up differed less substantially across youths who reported no change (1.05 days; 95% CI, 0.91-1.21), a 2-point increase (1.22 days; 95% CI, 0.95-1.52), and a 4-point increase (1.39 days; 95% CI, 0.91-2.10) on the societal discrimination composite. Associations of societal discrimination concern change scores with past 30-day alcohol use and ADHD were significantly stronger in youths whose parent(s) did not complete high school (IRR for alcohol use, 1.41 [95% CI, 1.14-1.74]; OR for ADHD, 1.81 [95% CI, 1.13-2.89]) than in youths whose parents completed high school (IRR for alcohol use, 0.95 [95% CI, 0.89-1.02; difference in associations by parental education, P = .02]; OR for ADHD, 0.98 [95% CI, 0.81-1.20; difference in associations by parental education, P = .03]) (Figure 1B and C).
Figure 1. Behavioral Health Outcomes as Function of Change in Societal Discrimination Concern From 2016 to 2017, by Parental Educational Level.
Graphs depict the estimated outcome value at follow-up as a function of magnitude of change from baseline to follow-up on the societal discrimination composite score (mean rating of concern, worry, and stress on scales ranging from 0 to 4, with 4 indicating extremely) derived from regression models in subsamples stratified by parental educational level. Marijuana (A) and alcohol use (B) are measured in the past 30 days; attention-deficit/hyperactivity disorder (ADHD) (C), as estimated prevalence of screening positive for ADHD symptoms on the Current Symptoms Scale–Self Report Form for Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition)–defined ADHD. The solid lines indicate estimated alcohol or marijuana use frequency level or ADHD prevalence; shaded areas, 95% CI.
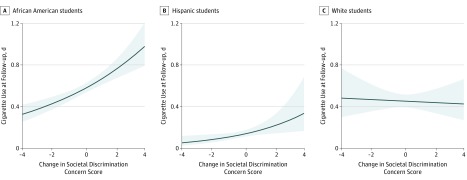
The association of change in societal discrimination concern from baseline to follow-up with past-month smoking days at follow-up differed by race/ethnicity (Figure 2). Each 1-SD increase in societal discrimination concern from baseline to follow-up was associated with significantly more past-month smoking days at follow-up in African American (IRR, 2.97; 95% CI, 1.45-6.09) and Hispanic (IRR, 1.30; 95% CI, 1.09-1.54) youth, whereas in other racial/ethnic groups, associations were nonsignificant (IRR, ≤1.23; P > .13) (difference in associations by race/ethnicity, P = .04). Associations of societal discrimination concern composite change score with other outcomes did not differ by parental educational level or race/ethnicity.
Figure 2. Cigarette Smoking as Function of Change in Societal Discrimination Concern From 2016 to 2017, by Race/Ethnicity.
Graphs depict the estimated number of days of cigarette use in the past 30 days at follow-up as a function of magnitude of change from baseline to follow-up on the societal discrimination composite score (mean rating of concern, worry, and stress on a scale of 0 to 4, with 4 indicating extremely) used to derive regression models in stratified subsamples of African American (A), Hispanic (B), and white (C) students. The solid lines indicate estimated cigarette use frequency level; shaded areas, 95% CI.
Sensitivity Analyses
Sensitivity analyses showed negligible effects of using alternative methods of addressing missing data or omitting covariates on study findings, modest differences between cohort enrollees included vs excluded in the analytic sample, low likelihood that unmeasured confounding explains the results, and that the association of baseline societal discrimination concern composite scores with 5 of 6 behavioral health outcomes at follow-up did not differ across youth who did and did not report frequently being a direct target of discrimination. Data are given in eMethods and eTables 4 to 7 in the Supplement.
Discussion
Concern, worry, and stress attributed to increasing societal discrimination during the recent sociopolitically charged period was common and associated with adverse behavioral health outcomes in this adolescent cohort. Polarizing societal events before 2016 may have generated concern over societal discrimination reported by students at baseline, including hate crimes, instances of police violence toward racial/ethnic minorities, and hostility toward minorities expressed among public figures in the media.2,3,4 From the spring of 2016 to the spring of 2017—a timespan coinciding with the 2016 presidential campaign and first several months of the Trump presidency—reported concern increased predominantly among Hispanic and African American students. During this period, President Trump pledged to enact new policies that may have heightened concern about intensifying discrimination in society, including proposals to construct a US-Mexico border wall to deter undocumented immigration, repeal the Affordable Care Act that provides health insurance to millions of low-income Americans, and prohibit entry into the United States from several countries with high religious minority populations. Consequently, the adolescents concerned about societal discrimination in early 2016 may have been especially reactive to the events transpiring during the subsequent year, which may, in turn, had implications for their behavioral health.
Several explanations for the associations found in this study may apply. Cross-student differences in willingness to report behavioral health problems and express feelings about the social climate could have affected study results. However, reporting tendencies are implausible explanations of why the change in societal discrimination concern from 2016 to 2017 was associated with certain behavioral health outcomes and why associations were amplified among racial/ethnic minority and socioeconomically disadvantaged youth in several cases. A preexisting liability toward behavioral health problems and sensitivity to environmental stress caused by endogenous (eg, genetics) or exogenous (eg, neighborhood deprivation) factors28,29 could have influenced associations between societal discrimination concern and behavioral health. Shared liability would presumably be reflected, to some extent, by students’ baseline behavioral health and sociodemographic status, and findings with vs without adjusting for these factors did not differ (eTable 4 in the Supplement). Perhaps the measure of youths’ perceptions of discrimination in society is a proxy for discrimination directly experienced, and being the direct target of discrimination, per se, may worsen behavioral health.30 However, the associations predominately generalized across youths who did vs did not report frequently experiencing discrimination (eMethods in the Supplement).
Although inferences regarding whether the demonstrated associations are causal cannot be made from this observational study, perceiving discrimination in society may play a direct role in the behavioral health of youth. Stress in any form may cause depression and interfere with the development of sustained attention, impulse control, and decision-making skills, which in turn may heighten the risk of ADHD and substance use.11,12,13,31,32,33,34 During the age captured in this study (11th to 12th grade), most adolescents began to face impending adult responsibilities, such as independent housing, obtaining full-time employment, financial independence, and embarking on higher education or other forms of career training. Many of these responsibilities are essential to identity formation during this developmental stage and the transition from adolescence to young adulthood.35 Consequently, youth concerned about the social climate may become discouraged about future opportunities for social advancement, less apt to successfully progress toward an adult identity, and more inclined to engage in risky behaviors they otherwise would not have, including substance use.8,9
In the overall sample, youth who became more concerned over societal discrimination during this period accelerated their cigarette and marijuana use frequency by follow-up. The reason why this association was specific to these 2 substances and did not extend to alcohol or to depression or ADHD symptoms is unknown and warrants further inquiry. The association between change in societal discrimination concern and several behavioral health outcomes was heightened among African American, Hispanic, or socioeconomically disadvantaged youths. Youths from these populations may believe that the consequences of shifting social trends are more likely to affect their communities. Consequently, the extent to which accelerated societal discrimination concerns translate into behavioral health problems may be more powerful for these youths. The pattern of stronger associations between changes in societal discrimination concerns and study outcomes was particularly pervasive in adolescents with less educated parents, extending across 3 of the 6 behavioral health problems. Compared with [12.3%] other demographic factors, parental educational level and other socioeconomic indicators are especially indicative of social disadvantage.36 Social disadvantage per se may be a key source of vulnerability to behavioral health consequences of societal discrimination concerns.
Limitations
A limitation of this research was the application of an adversity approach to understanding this phenomenon. Resiliency, connectedness, and other potential buffers of the association between societal discrimination concern and behavioral health warrant future study. This investigation could not biochemically verify substance use or obtain clinician diagnoses of depression or ADHD. Although the societal discrimination concern items exhibited high internal reliability in this study, they have not been subject to extensive psychometric evaluation. These items assess concern over increases in societal discrimination, yet some youth may not perceive societal discrimination to be increasing. Whether findings would generalize to other geographic locations or other developmental periods is unknown.
Conclusions
Recent societal increases in hostility and discrimination directed toward minorities may be a significant source of concern in youth that is associated with adverse behavioral health outcomes, particularly in teenagers of color or from socioeconomically disadvantaged families. Although some of the associations were of small magnitude, even modest increases in the risk of adolescent behavioral health problems may pose important public health consequences given that increasing societal discrimination can be a nationwide (and to some degree international) phenomenon. The behavioral consequences of adolescent exposure to public expressions of discrimination may warrant public health attention.
eTable 1. Characteristics of Participating Schools Compared With Los Angeles County Schools
eTable 2. Available (Nonmissing) Data for Key Variables
eTable 3. Estimates of Association Between Covariates and Behavioral Health Outcomes in the Primary Regression Models
eTable 4. Associations of Reported Concern Over Increasing Discrimination in Society Composite Score With Behavioral Health Outcomes at Follow-up Without Adjustment for Sociodemographic Covariates
eTable 5. Associations of Reported Concern Over Increasing Discrimination in Society Composite Score With Behavioral Health Outcomes at Follow-up Among All Cohort Enrollees Using FIML Estimation to Account for Missing Data
eTable 6. Associations of Reported Concern Over Increasing Discrimination in Society Composite Score With Behavioral Health Outcomes at Follow-up, Including Students Who Completed the Societal Discrimination Concern at Both Time Points Using FIML Estimation to Account for Missing Data
eTable 7. Associations of Reported Concern Over Increasing Discrimination in Society Composite Score With Behavioral Health Outcomes at Follow-up After Listwise Deletion for All Missing Data
eFigure 1. Study Accrual Flowchart
eFigure 2. Associations of Reported Concern Over Increasing Discrimination in Society Composite Score With Behavioral Health Outcomes at Follow-up After Listwise Deletion for All Missing Data
eMethods. Retesting, Missing Data, and Confounding
References
- 1.Williams DR, Medlock MM. Health effects of dramatic societal events: ramifications of the recent presidential election. N Engl J Med. 2017;376(23):2295-2299. doi: 10.1056/NEJMms1702111 [DOI] [PubMed] [Google Scholar]
- 2.Swaine J, Laughland O, Lartey J, McCarthy C Young black men killed by US police at highest rate in year of 1134 deaths. The Guardian December 31, 2015. https://www.theguardian.com/us-news/2015/dec/31/the-counted-police-killings-2015-young-black-men. Accessed December 11, 2017.
- 3.Human Rights Campaign Addressing anti-transgender violence: exploring realities, challenges and solutions for policymakers and community advocates. https://www.hrc.org/resources/addressing-anti-transgender-violence-exploring-realities-challenges-and-sol. 2015. Accessed December 11, 2017.
- 4.Lichtblau E. Hate crimes against American Muslims most since post-9/11 era. New York Times September 17, 2016. https://www.nytimes.com/2016/09/18/us/politics/hate-crimes-american-muslims-rise.html?_r=0. Accessed December 11, 2017.
- 5.Hatzenbuehler ML, Prins SJ, Flake M, et al. Immigration policies and mental health morbidity among Latinos: a state-level analysis. Soc Sci Med. 2017;174:169-178. doi: 10.1016/j.socscimed.2016.11.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Padela AI, Heisler M. The association of perceived abuse and discrimination after September 11, 2001, with psychological distress, level of happiness, and health status among Arab Americans. Am J Public Health. 2010;100(2):284-291. doi: 10.2105/AJPH.2009.164954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Richman LS, Jonassaint C. The effects of race-related stress on cortisol reactivity in the laboratory: implications of the Duke lacrosse scandal. Ann Behav Med. 2008;35(1):105-110. doi: 10.1007/s12160-007-9013-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cho J, Kogan SM. Risk and protective processes predicting rural African American young men’s substance abuse. Am J Community Psychol. 2016;58(3-4):422-433. doi: 10.1002/ajcp.12104 [DOI] [PubMed] [Google Scholar]
- 9.Cho J, Kogan SM. Parent and youth dopamine D4 receptor genotypes moderate multilevel contextual effects on rural African American youth’s risk behavior. Dev Psychopathol. 2016;28(2):433-445. doi: 10.1017/S0954579415000565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hinshaw SP. Attention deficit hyperactivity disorder (ADHD): controversy, developmental mechanisms, and multiple levels of analysis. Annu Rev Clin Psychol. 2018;14:291-316. doi: 10.1146/annurev-clinpsy-050817-084917 [DOI] [PubMed] [Google Scholar]
- 11.van Lieshout M, Luman M, Buitelaar J, Rommelse NN, Oosterlaan J. Does neurocognitive functioning predict future or persistence of ADHD? a systematic review. Clin Psychol Rev. 2013;33(4):539-560. doi: 10.1016/j.cpr.2013.02.003 [DOI] [PubMed] [Google Scholar]
- 12.Hankin BL, Abramson LY, Siler M. A prospective test of the hopelessness theory of depression in adolescence. Cognit Ther Res. 2001;25(5):607-632. doi: 10.1023/A:1005561616506 [DOI] [Google Scholar]
- 13.Sanders-Phillips K, Kliewer W, Tirmazi T, Nebbitt V, Carter T, Key H. Perceived racial discrimination, drug use, and psychological distress in African American youth: a pathway to child health disparities. J Soc Issues. 2014;70(2):279-297. doi: 10.1111/josi.12060 [DOI] [Google Scholar]
- 14.Leventhal AM, Strong DR, Kirkpatrick MG, et al. Association of electronic cigarette use with initiation of combustible tobacco product smoking in early adolescence. JAMA. 2015;314(7):700-707. doi: 10.1001/jama.2015.8950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Eaton DK, Kann L, Kinchen S, et al. ; Centers for Disease Control and Prevention (CDC) . Youth risk behavior surveillance: United States, 2009. MMWR Surveill Summ. 2010;59(5):1-142. [PubMed] [Google Scholar]
- 16.Miech RA, Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Secondary School Students. Vol I Ann Arbor: Institute for Social Research, The University of Michigan; 2016. Monitoring the Future national survey results on drug use, 1975-2015. [Google Scholar]
- 17.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385-401. doi: 10.1177/014662167700100306 [DOI] [Google Scholar]
- 18.Radloff LS. The use of the Center for Epidemiologic Studies Depression Scale in adolescents and young adults. J Youth Adolesc. 1991;20(2):149-166. doi: 10.1007/BF01537606 [DOI] [PubMed] [Google Scholar]
- 19.Barkley RA. Attention-Deficit Hyperactivity Disorder: A Clinical Workbook. Silver Spring, MD: Medifocus.com Inc; 1991. [Google Scholar]
- 20.American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- 21.Williams DR, Yan Yu, Jackson JS, Anderson NB. Racial differences in physical and mental health: socio-economic status, stress and discrimination. J Health Psychol. 1997;2(3):335-351. doi: 10.1177/135910539700200305 [DOI] [PubMed] [Google Scholar]
- 22.Barona A, Miller JA. Short Acculturation Scale for Hispanic Youth (SASH-Y): a preliminary report. Hisp J Behav Sci. 1994;16(2):155-162. doi: 10.1177/07399863940162005 [DOI] [Google Scholar]
- 23.Wagner B, Riggs P, Mikulich-Gilbertson S. The importance of distribution-choice in modeling substance use data: a comparison of negative binomial, beta binomial, and zero-inflated distributions. Am J Drug Alcohol Abuse. 2015;41(6):489-497. doi: 10.3109/00952990.2015.1056447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Molina KM, Alegría M, Mahalingam R. A multiple-group path analysis of the role of everyday discrimination on self-rated physical health among Latina/os in the USA. Ann Behav Med. 2013;45(1):33-44. doi: 10.1007/s12160-012-9421-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Muthén LK. Mplus: Statistical Analysis with Latent Variables [computer software]. Version 4.21. University of California, Los Angeles; 2007.
- 26.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Series B Stat Methodol. 1995;57(1):289-300. [Google Scholar]
- 27.Conway KP, Swendsen J, Husky MM, He J-P, Merikangas KR. Association of lifetime mental disorders and subsequent alcohol and illicit drug use: results from the National Comorbidity Survey–Adolescent Supplement. J Am Acad Child Adolesc Psychiatry. 2016;55(4):280-288. doi: 10.1016/j.jaac.2016.01.006 [DOI] [PubMed] [Google Scholar]
- 28.Strachan E, Duncan G, Horn E, Turkheimer E. Neighborhood deprivation and depression in adult twins: genetics and gene × environment interaction. Psychol Med. 2017;47(4):627-638. doi: 10.1017/S0033291716002622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bogdan R, Pizzagalli DA. The heritability of hedonic capacity and perceived stress: a twin study evaluation of candidate depressive phenotypes. Psychol Med. 2009;39(2):211-218. doi: 10.1017/S0033291708003619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Unger JB, Soto DW, Baezconde-Garbanati L. Trajectories of perceived discrimination from adolescence to emerging adulthood and substance use among Hispanic youth in Los Angeles. Addict Behav. 2016;53:108-112. doi: 10.1016/j.addbeh.2015.10.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Charles ST, Piazza JR, Mogle J, Sliwinski MJ, Almeida DM. The wear and tear of daily stressors on mental health. Psychol Sci. 2013;24(5):733-741. doi: 10.1177/0956797612462222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Quinn ME, Joormann J. Control when it counts: change in executive control under stress predicts depression symptoms. Emotion. 2015;15(4):522-530. doi: 10.1037/emo0000089 [DOI] [PubMed] [Google Scholar]
- 33.Sinha R, Jastreboff AM. Stress as a common risk factor for obesity and addiction. Biol Psychiatry. 2013;73(9):827-835. doi: 10.1016/j.biopsych.2013.01.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Duckworth AL, Kim B, Tsukayama E. Life stress impairs self-control in early adolescence. Front Psychol. 2013;3:608. doi: 10.3389/fpsyg.2012.00608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Arnett JJ. Emerging adulthood: a theory of development from the late teens through the twenties. Am Psychol. 2000;55(5):469-480. doi: 10.1037/0003-066X.55.5.469 [DOI] [PubMed] [Google Scholar]
- 36.Bauman LJ, Silver EJ, Stein RE. Cumulative social disadvantage and child health. Pediatrics. 2006;117(4):1321-1328. doi: 10.1542/peds.2005-1647 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Characteristics of Participating Schools Compared With Los Angeles County Schools
eTable 2. Available (Nonmissing) Data for Key Variables
eTable 3. Estimates of Association Between Covariates and Behavioral Health Outcomes in the Primary Regression Models
eTable 4. Associations of Reported Concern Over Increasing Discrimination in Society Composite Score With Behavioral Health Outcomes at Follow-up Without Adjustment for Sociodemographic Covariates
eTable 5. Associations of Reported Concern Over Increasing Discrimination in Society Composite Score With Behavioral Health Outcomes at Follow-up Among All Cohort Enrollees Using FIML Estimation to Account for Missing Data
eTable 6. Associations of Reported Concern Over Increasing Discrimination in Society Composite Score With Behavioral Health Outcomes at Follow-up, Including Students Who Completed the Societal Discrimination Concern at Both Time Points Using FIML Estimation to Account for Missing Data
eTable 7. Associations of Reported Concern Over Increasing Discrimination in Society Composite Score With Behavioral Health Outcomes at Follow-up After Listwise Deletion for All Missing Data
eFigure 1. Study Accrual Flowchart
eFigure 2. Associations of Reported Concern Over Increasing Discrimination in Society Composite Score With Behavioral Health Outcomes at Follow-up After Listwise Deletion for All Missing Data
eMethods. Retesting, Missing Data, and Confounding