This cohort study investigated whether IgE-mediated allergy is associated with a lower risk for complicated appendicitis among children undergoing appendectomy for acute appendicitis.
Key Points
Question
Do children with IgE-mediated allergy have a lower risk of complicated appendicitis?
Findings
In this cohort study of 605 children undergoing appendectomy, those with IgE-mediated allergy had a 3 times lower risk of complicated appendicitis compared with those without allergy.
Meaning
These findings present previously unknown risk factors for complicated appendicitis and shed light on pathogenesis and clinical detection of adverse outcomes.
Abstract
Importance
Childhood appendicitis is commonly complicated by gangrene and perforation, yet the causes of complicated appendicitis and how to avoid it remain unknown.
Objective
To investigate whether children with IgE-mediated allergy have a lower risk of complicated appendicitis.
Design, Setting, and Participants
This retrospective cohort study included all consecutive patients younger than 15 years (hereinafter referred to as children) who underwent appendectomy for acute appendicitis at a tertiary pediatric surgery center in Sweden between January 1, 2007, through July 31, 2017. Children were stratified between those with and without IgE-mediated allergies.
Main Outcome and Measures
Risk of complicated appendicitis with gangrene or perforation, with occurrence of IgE-mediated allergy as an independent variable and adjusted for age, sex, primary health care contacts, seasonal antigenic exposure, allergy medications, appendicolith, and duration of symptoms.
Results
Of 605 included children (63.0% boys; median age, 10 years; interquartile range, 7-12 years), 102 (16.9%) had IgE-mediated allergy and 503 (83.1%) had no allergy. Complicated appendicitis occurred in 20 children with IgE-mediated allergy (19.6%) compared with 236 with no allergy (46.9%; adjusted odds ratio, 0.33; 95% CI, 0.18-0.59). No significant allergy effect modification by sex, seasonal antigenic exposure, or allergy medication was found. Children with IgE-mediated allergy had a shorter hospital stay (median, 2 days for both groups; interquartile range, 1-2 days vs 1-5 days; P = .004).
Conclusions and Relevance
In this study, children with IgE-mediated allergy had a lower risk of complicated appendicitis. The findings suggest that immunologic disposition modifies the clinical pattern of appendiceal disease. This theory introduces novel opportunities for understanding of the pathogenesis and clinical decision making for one of childhood’s most common surgical emergencies.
Introduction
The incidence of appendicitis peaks in childhood,1 and appendectomy is the most common abdominal emergency operation performed worldwide.2 At a minimum, every third child with appendicitis develops complicated disease with gangrene or perforation,1 and the morbidity and avoidable societal costs are high.3,4 The pathogenesis remains unclear, and we lack proper understanding of risk factors, urgency, and reliable predictors associated with spontaneous resolution and adverse outcome. Furthermore, no means of prevention exists.
From previous work, clinical risk factors such as age and sex4,5,6,7 and the presence of an appendicolith8 have been identified to influence the development of complicated appendicitis. In a cultural context, insurance status9 and health care connectivity before presentation10 have been associated with severity of the disease.
The view of appendicitis as a progressive inflammatory disease always ending with perforation is increasingly being challenged7,11 and is a current topic of debate.5,6,7,12,13,14,15,16,17,18,19 Studies have implied that complicated and uncomplicated appendicitis represent 2 distinct immunologic entities, with complicated disease being characterized by a dominance of helper T-cell subsets TH1 and TH17, whereas uncomplicated disease has a TH2-dependent immunologic response.12,15,16,20 Evidence further suggests that individual susceptibility to a TH1- or a TH2-dominated response,21,22 and in the case of appendicitis, complicated appendicitis has been shown to be associated with a higher subsequent risk of TH1-dominated Crohn disease23 and a lower risk of TH2-dominated ulcerative colitis.24,25 Given the evidently strong link between the TH2 response and IgE-mediated (type 1) allergy, one may hypothesize that children with allergy would have a lower risk of complicated disease. However, no study has yet explored the possible connection between common allergy and adverse appendicitis outcome.
To test this hypothesis and to shed new light on risk factors for complicated appendicitis, a cohort of consecutive children who underwent surgery for appendicitis was evaluated for association between allergy and appendicitis severity. The purpose of this study was to investigate whether IgE-mediated allergy is associated with a lower adjusted risk of complicated outcome.
Methods
Study Design and Setting
We conducted a retrospective cohort study of all children who underwent surgery for acute appendicitis at the tertiary pediatric surgery center of Skåne University Hospital, Lund, Sweden, from January 1, 2007, through July 31, 2017. The study was approved by the regional ethical review board, which deemed that patient consent was not required.
Inclusion and Exclusion Criteria
All children younger than 15 years (hereinafter referred to as children) with an intraoperative diagnosis of acute appendicitis were eligible for inclusion. Children with negative appendectomy findings after histopathologic analysis were excluded.
Outcomes
Primary outcome was complicated or uncomplicated appendicitis. Appendicitis was characterized as complicated (gangrenous, perforated, or abscess) or uncomplicated (phlegmonous) based on histopathologic and intraoperative findings. Gangrenous appendicitis was defined from the intraoperative findings and from histopathologic analysis as full-thickness necrosis of the appendix wall. Perforated appendicitis was defined as a visual hole in the appendix or gross contamination in the abdomen during appendectomy. Appendectomy was defined according to the Nordic Medico-Statistical Committee procedure codes JEA00, JEA01, and JEA10.26 Secondary outcomes were length of hospital stay, defined as days at the ward after surgery, and rate of reoperation, defined as any abdominal procedure requiring general anesthesia within 30 days of the appendectomy.
Primary Exposure
Primary exposure was occurrence of any prior IgE-mediated allergy. Information about allergies was collected from multiple sources, including the surgical and anesthesia records and the regionwide medical history files. The admitting surgeon and nurse, the ward nurse, and the anesthesiologist and anesthesia nurse routinely inquired about the presence of allergy. Allergens were reported in detail and categorized as fur or mite allergy, pollen allergy, egg or milk protein allergy, or antibiotic allergy.
Potential Confounders
Potential confounders were age, sex, duration of symptoms, presence of an appendicolith, number of primary care visits within the 12 months before the appendectomy, seasonal antigenic exposure, and ongoing use of allergy medication. Duration of symptoms was measured from reported onset of symptoms to first visit at the pediatric emergency department. Detection of an appendicolith was obtained from preoperative ultrasonographic or computed tomographic study or by the intraoperative findings. Season of appendectomy was categorized according to the following allergy seasons relevant for the region: spring (March-May), summer (June-August), autumn (September-November), and winter (December-February). Ongoing use of allergy medication was defined as use of any medication prescribed for IgE-mediated allergy at the time of appendectomy.
Statistical Analysis
Categorical variables were reported as frequencies and percentages, with differences between groups assessed using the Fisher exact test. Continuous variables were assessed for normal distribution and were presented as medians with an interquartile range (IQR), with differences assessed using the Mann-Whitney test for nonnormal distributed data. Associations of independent variables on the primary outcome were presented as odds ratios (ORs) with 95% CI, using logistic regression. Variables with a significant association with outcome in the unadjusted analysis were included in the multivariable logistic regression model for adjusted ORs of main effects. The final model also remained intact when using backward and forward selection, with significance levels set at P < .05. Effect modification by age, seasonal antigenic exposure, and current allergy medication was assessed by the inclusion of interaction terms, and overall effect modification was assessed with the Wald test. Robustness to unmeasured confounding in the multivariable logistic regression model was quantified by an E value for effect estimate and 95% CI.27 All statistical analyses were performed in Stata/SE version 14.1 for Windows (StataCorp LP).
Results
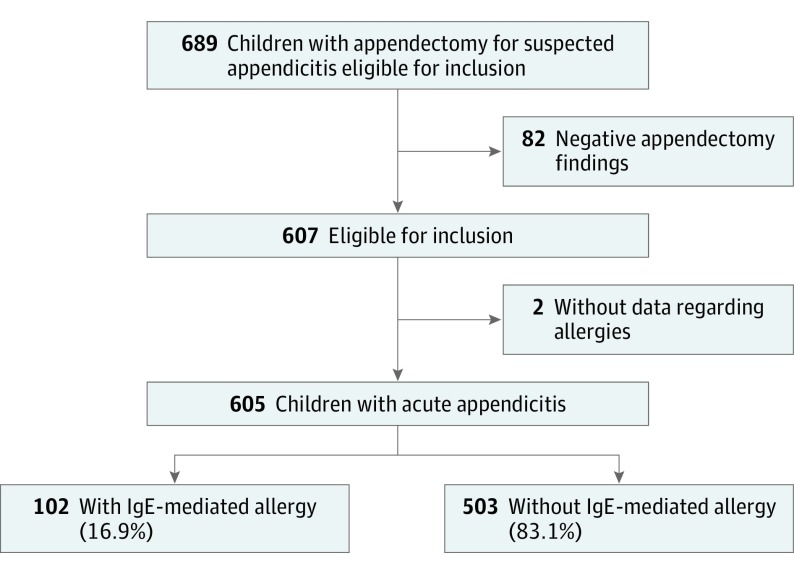
During the study period, a total of 605 children (381 boys [63.0%] and 224 girls [37.0%]; median age, 10 years; IQR, 7-12 years) underwent appendectomy with a primary diagnosis of acute appendicitis, of whom 102 (16.9%) had IgE-mediated allergy and 503 (83.1%) had no allergy (Figure 1). Children with allergy were significantly older (median age, 11 years [IQR, 9-13 years] vs 10 years [IQR, 7-12 years]; P = .002), but no differences in sex distribution, duration of symptoms, presence of an appendicolith, number of primary care visits within the last 12 months, or season of appendectomy were noted (Table 1).
Figure 1. Flow Diagram of the Study Population.
Children younger than 15 years undergoing surgery for suspected acute appendicitis were included in the study.
Table 1. Occurrence of IgE-Mediated Allergy Among 605 Children Undergoing Surgery for Appendicitis.
| Characteristic | Patient Group | P Value | |
|---|---|---|---|
| Allergy (n = 102) | No Allergy (n = 503) | ||
| Age, median (IQR), y | 11 (9-13) | 10 (7-12) | .002a |
| Sex, No. (%) | |||
| Boys | 66 (64.7) | 315 (62.6) | .74b |
| Girls | 36 (35.3) | 188 (37.4) | |
| Duration of symptoms, median (IQR), d | 1 (<1 to 1) | 1 (<1 to 2) | .06a |
| Appendicolith present, No. (%) | 10 (9.8) | 88 (17.5) | .06b |
| No. of primary care visits within last 12 mo, median (IQR)c | 0.5 (0-1) | 0 (0-2) | .61a |
| Season, No. (%) | |||
| Spring | 32 (31.4) | 143 (28.4) | .59b |
| Summer | 25 (24.5) | 103 (20.5) | |
| Autumn | 23 (22.5) | 123 (24.5) | |
| Winter | 22 (21.6) | 134 (26.6) | |
Abbreviation: IQR, interquartile range.
Calculated using the Mann-Whitney test.
Calculated using the Fisher exact test.
Data were available for 95 patients (2015-2016).
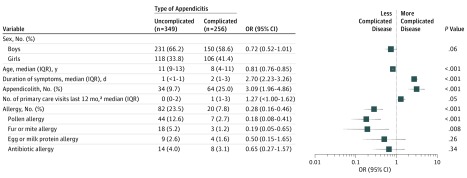
Complicated appendicitis occurred in 20 children with IgE-mediated allergy (19.6%) compared with 236 children with no allergy (46.9%). Younger age (OR, 0.81; 95% CI, 0.76-0.85; P < .001), longer duration of symptoms (OR, 2.70; 95% CI, 2.23-3.26; P < .001), and presence of appendicolith (OR. 3.09; 95% CI, 1.96-4.86; P < .001) were all associated with a higher unadjusted risk of complicated appendicitis (Figure 2).
Figure 2. Unadjusted Independent Variables of Complicated Disease Among 605 Children Undergoing Surgery for Acute Appendicitis.
Univariate logistic regression was used with odds ratios (ORs) and 95% CIs (error bars). IQR indicates interquartile range.
aData were available for 95 patients (2015-2016).
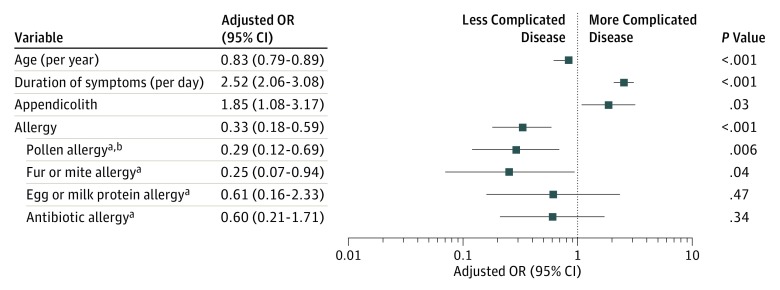
Children with allergy were 3 times less likely to have complicated appendicitis on univariate (OR, 0.28; 95% CI, 0.16-0.46; P < .001) (Figure 2) and multivariable analysis (adjusted OR, 0.33; 95% CI, 0.18-0.59) (Figure 3). The approximate E value for unmeasured confounding was 2.9 for the point estimate and 1.9 to 4.1 for the 95% CI. The lower risk remained in the subgroup analysis of fur or mite allergy (adjusted OR, 0.25; 95% CI, 0.07-0.94; P = .04) and pollen allergy (adjusted OR, 0.29; 95% CI, 0.12-0.69; P = .006), but not for egg or milk protein allergy (adjusted OR, 0.61; 95% CI, 0.16-2.33; P = .47) or antibiotic allergy (adjusted OR, 0.60; 95% CI, 0.21-1.71; P = .34). The presence of allergy was associated with shorter hospital stay (median length of stay, 2 days for both groups; IQR, 1-2 vs 1-5 days; P = .004), but there was no difference in the rate of reoperations (Table 2).
Figure 3. Adjusted Variables for Complicated Disease Among 605 Children Undergoing Surgery for Acute Appendicitis.
Multivariable logistic regression was used with adjusted odds ratios (ORs) and 95% CIs (error bars). The approximate E value for unmeasured confounding was 2.9 for the point estimate and 1.9 to 4.1 for the 95% CI.
aIndicates compared with no allergy.
bIncludes allergies to allergens with cross-reactivity to pollen.
Table 2. Primary and Secondary Outcomes Among 605 Children Undergoing Surgery for Appendicitis.
| Outcome | Patient Group | P Value | |
|---|---|---|---|
| Allergy (n = 102) | No Allergy (n = 503) | ||
| Appendicitis, No. (%) | |||
| Uncomplicated | 82 (80.4) | 267 (53.1) | <.001a |
| Complicated | 20 (19.6) | 236 (46.9) | |
| Reoperation within 30 d, No. (%) | 3 (2.9) | 18 (3.6) | >.99a |
| Length of stay, median (IQR), d | 2 (1-2) | 2 (1-5) | .004b |
Abbreviation: IQR, interquartile range.
Calculated using the Fisher exact test.
Calculated using the Mann-Whitney test.
Sex did not modify the effect of allergy (adjusted OR, 0.89; 95% CI, 0.60-1.33; P = .57) (eFigure 1 in the Supplement). In addition, no effect modification by ongoing allergy medication (Wald test of overall interaction, P = .22) or seasonal antigen exposure (Wald test of overall interaction, P = .83) was noted (eMethods in the Supplement). The number of primary care visits 12 months before appendicitis was not associated with less complicated appendicitis (adjusted OR, 0.98; 95% CI, 0.73-1.31; P = .88) (sensitivity analysis, eFigure 2 in the Supplement). The association between allergy and complicated appendicitis was particularly strong for the subset of patients with histopathologic diagnosis in the sensitivity analysis (univariate OR, 0.19 [95% CI, 0.08-0.43; P < .001]; adjusted OR, 0.23 [95% CI, 0.09-0.56; P = .001]) (eFigures 3A and 4B in the Supplement).
Discussion
This cohort study introduces a strong and previously unknown association between allergy and appendicitis. Children with IgE-mediated allergy had an adjusted risk of developing complicated appendicitis that was 3 times lower than those without IgE-mediated allergy. These findings offer new opportunities to understand the pathogenesis and clinical prediction of adverse appendicitis outcome.
Our results suggest that allergic immune responses modulate the severity of appendicitis, yet we can only speculate about the causal mechanisms. The importance of immune responses in appendicitis has been supported previously by epidemiologic15,16,23,24,25,28 and immunologic12,20 reports. The lower risk of complicated appendicitis among children with allergy could indicate that the less aggressive TH2-mediated immune response to appendicitis12,15,16,20 is associated with a synchronous TH2 shift of allergic comorbidities. Whether this shift represents an underlying genetic predisposition or the likelihood of a benign appendicitis response can be modulated transiently by TH2 shifts induced by certain acute illnesses, environmental factors,29 or even medical therapy will require further investigations. Our findings do not support the theory that seasonal antigenic exposure or allergy treatment influences the association of allergy with complicated appendicitis. Rather, an inherent tendency for certain inflammatory responses may be the underlying explanation for the lower risk of a complicated disease course among these children.
Several clinical risk factors, such as younger age4 and the presence of an appendicolith,8 have been shown to be associated with complicated pediatric appendicitis, but clinicians often lack reliable signals of severity to determine which children would benefit from urgent surgery or conservative treatment. Based on the strong association between allergy and low risk of complicated appendicitis found in this study, we propose that the presence of allergy should be considered for inclusion in future clinical scoring systems for pediatric appendicitis. Also, if noncomplicated appendicitis is driven by a TH2-dependent immunologic response, one could hypothesize that this response would result in a possible elevated activity of eosinophils and basophils and perhaps even preventive or therapeutic opportunities.
Limitations
Our findings must be interpreted in the context of a nonrandomized design. Most known risk factors for complicated appendicitis were adjusted for in the multivariable model and, given the strong association between allergy and uncomplicated appendicitis, an unmeasured confounder would need to be associated with allergy and complicated appendicitis by approximately 2.9-fold for the OR (and approximately 1.9-fold for the 95% CI) above and beyond the measured variables to explain the observed effect of allergy. Socioeconomic variables were not available, and information about primary care visits were introduced in the countywide electronic medical records only from 2015 onward, corresponding to approximately one-sixth of the patients; however, we believe that the inclusion of self-reported duration of symptoms in the multivariable model compensates well for this limitation, especially for the Swedish health care system, where all patients have the right to seek first-line medical care directly in tertiary care hospitals and where practically no financial barriers to surgical care exist. In our study, a direct first-line contact with the emergency departments at the hospital was the preferred contact by most families; approximately 5% of our patients with appendicitis were referred from primary care. Also, the occurrence of IgE-mediated allergy was taken from a patient’s retrospective history, which is subjective and potentially inaccurate; however, we do not expect this limitation to have biased our results systematically. Another weakness is that all children did not have histopathologically confirmed appendicitis; however, according to the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, complicated appendicitis is now a clinical diagnosis not requiring histopathologic confirmation, and when analyzing the subset of patients with a histopathologic diagnosis, the association between allergy and complicated disease became even stronger, despite reduced statistical power. Overall, it should be emphasized that our results hypothesize that allergy in some way influences the severity of appendicitis, and certainly other immunopathologic factors must play a part in pathogenesis. Our findings clearly generate more questions than they resolve, and further studies are warranted.
Conclusions
Among children, IgE-mediated allergy is associated with a reduction in the risk of complicated appendicitis. These findings offer new opportunities to understand the pathogenesis and clinical prediction of pediatric appendicitis.
eFigure 1. Adjusting for Sex in Multivariable Regression Model
eFigure 2. Adjusting for Primary Care Visits in Multivariable Regression Model
eFigure 3. Univariate Odds Ratios
eFigure 4. Adjusted Odds Ratios
eMethods. Evaluation of Heterogeneity
References
- 1.Ponsky TA, Huang ZJ, Kittle K, et al. Hospital- and patient-level characteristics and the risk of appendiceal rupture and negative appendectomy in children. JAMA. 2004;292(16):1977-1982. doi: 10.1001/jama.292.16.1977 [DOI] [PubMed] [Google Scholar]
- 2.Bhangu A; GlobalSurg Collaborative . Mortality of emergency abdominal surgery in high-, middle- and low-income countries. Br J Surg. 2016;103(8):971-988. doi: 10.1002/bjs.10151 [DOI] [PubMed] [Google Scholar]
- 3.Feng C, Anandalwar S, Sidhwa F, et al. Beyond perforation: influence of peritoneal contamination on clinical severity and resource utilization in children with perforated appendicitis. J Pediatr Surg. 2016;51(11):1896-1899. doi: 10.1016/j.jpedsurg.2016.08.002 [DOI] [PubMed] [Google Scholar]
- 4.Glass CC, Rangel SJ. Overview and diagnosis of acute appendicitis in children. Semin Pediatr Surg. 2016;25(4):198-203. doi: 10.1053/j.sempedsurg.2016.05.001 [DOI] [PubMed] [Google Scholar]
- 5.Narsule CK, Kahle EJ, Kim DS, Anderson AC, Luks FI. Effect of delay in presentation on rate of perforation in children with appendicitis. Am J Emerg Med. 2011;29(8):890-893. doi: 10.1016/j.ajem.2010.04.005 [DOI] [PubMed] [Google Scholar]
- 6.Papandria D, Goldstein SD, Rhee D, et al. Risk of perforation increases with delay in recognition and surgery for acute appendicitis. J Surg Res. 2013;184(2):723-729. doi: 10.1016/j.jss.2012.12.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Drake FT, Mottey NE, Farrokhi ET, et al. Time to appendectomy and risk of perforation in acute appendicitis. JAMA Surg. 2014;149(8):837-844. doi: 10.1001/jamasurg.2014.77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alaedeen DI, Cook M, Chwals WJ. Appendiceal fecalith is associated with early perforation in pediatric patients. J Pediatr Surg. 2008;43(5):889-892. doi: 10.1016/j.jpedsurg.2007.12.034 [DOI] [PubMed] [Google Scholar]
- 9.Scott JW, Rose JA, Tsai TC, et al. Impact of ACA insurance coverage expansion on perforated appendix rates among young adults. Med Care. 2016;54(9):818-826. doi: 10.1097/MLR.0000000000000586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baxter KJ, Nguyen HTMH, Wulkan ML, Raval MV. Association of health care utilization with rates of perforated appendicitis in children 18 years or younger. JAMA Surg. Published online January 31, 2018. doi: 10.1001/jamasurg.2017.5316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Serres SK, Cameron DB, Glass CC, et al. Time to appendectomy and risk of complicated appendicitis and adverse outcomes in children. JAMA Pediatr. 2017;171(8):740-746. doi: 10.1001/jamapediatrics.2017.0885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rubér M, Berg A, Ekerfelt C, Olaison G, Andersson RE. Different cytokine profiles in patients with a history of gangrenous or phlegmonous appendicitis. Clin Exp Immunol. 2006;143(1):117-124. doi: 10.1111/j.1365-2249.2005.02957.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Landisch RM, Arca MJ, Oldham KT. Emergent or urgent appendectomy? a changing perspective. JAMA Pediatr. 2017;171(8):727-729. doi: 10.1001/jamapediatrics.2017.1445 [DOI] [PubMed] [Google Scholar]
- 14.Andersson RE. The natural history and traditional management of appendicitis revisited: spontaneous resolution and predominance of prehospital perforations imply that a correct diagnosis is more important than an early diagnosis. World J Surg. 2007;31(1):86-92. doi: 10.1007/s00268-006-0056-y [DOI] [PubMed] [Google Scholar]
- 15.Andersson R, Hugander A, Thulin A, Nyström PO, Olaison G. Indications for operation in suspected appendicitis and incidence of perforation. BMJ. 1994;308(6921):107-110. doi: 10.1136/bmj.308.6921.107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Livingston EH, Woodward WA, Sarosi GA, Haley RW. Disconnect between incidence of nonperforated and perforated appendicitis: implications for pathophysiology and management. Ann Surg. 2007;245(6):886-892. doi: 10.1097/01.sla.0000256391.05233.aa [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cappendijk VC, Hazebroek FW. The impact of diagnostic delay on the course of acute appendicitis. Arch Dis Child. 2000;83(1):64-66. doi: 10.1136/adc.83.1.64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bonadio W, Brazg J, Telt N, et al. Impact of in-hospital timing to appendectomy on perforation rates in children with appendicitis. J Emerg Med. 2015;49(5):597-604. doi: 10.1016/j.jemermed.2015.04.009 [DOI] [PubMed] [Google Scholar]
- 19.Yardeni D, Hirschl RB, Drongowski RA, Teitelbaum DH, Geiger JD, Coran AG. Delayed versus immediate surgery in acute appendicitis: do we need to operate during the night? J Pediatr Surg. 2004;39(3):464-469. doi: 10.1016/j.jpedsurg.2003.11.020 [DOI] [PubMed] [Google Scholar]
- 20.Rubér M, Andersson M, Petersson BF, Olaison G, Andersson RE, Ekerfelt C. Systemic TH17-like cytokine pattern in gangrenous appendicitis but not in phlegmonous appendicitis. Surgery. 2010;147(3):366-372. doi: 10.1016/j.surg.2009.09.039 [DOI] [PubMed] [Google Scholar]
- 21.O’Shea JJ, Ma A, Lipsky P. Cytokines and autoimmunity. Nat Rev Immunol. 2002;2(1):37-45. doi: 10.1038/nri702 [DOI] [PubMed] [Google Scholar]
- 22.Romagnani S. Biology of human TH1 and TH2 cells. J Clin Immunol. 1995;15(3):121-129. doi: 10.1007/BF01543103 [DOI] [PubMed] [Google Scholar]
- 23.Andersson RE, Olaison G, Tysk C, Ekbom A. Appendectomy is followed by increased risk of Crohn’s disease. Gastroenterology. 2003;124(1):40-46. doi: 10.1053/gast.2003.50021 [DOI] [PubMed] [Google Scholar]
- 24.Andersson RE, Lambe M. Incidence of appendicitis during pregnancy. Int J Epidemiol. 2001;30(6):1281-1285. doi: 10.1093/ije/30.6.1281 [DOI] [PubMed] [Google Scholar]
- 25.Frisch M, Pedersen BV, Andersson RE. Appendicitis, mesenteric lymphadenitis, and subsequent risk of ulcerative colitis: cohort studies in Sweden and Denmark. BMJ. 2009;338:b716. doi: 10.1136/bmj.b716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.NOMESCO Classification of Surgical Procedures (NSCP) 1.16. Version 1.16 ed. Copenhagen, Denmark and Oslo, Norway. 2012.
- 27.VanderWeele TJ, Ding P. Sensitivity analysis in observational research: introducing the E-value. Ann Intern Med. 2017;167(4):268-274. doi: 10.7326/M16-2607 [DOI] [PubMed] [Google Scholar]
- 28.Andersson RE, Olaison G, Tysk C, Ekbom A. Appendectomy and protection against ulcerative colitis. N Engl J Med. 2001;344(11):808-814. doi: 10.1056/NEJM200103153441104 [DOI] [PubMed] [Google Scholar]
- 29.Flohr C, Quinnell RJ, Britton J. Do helminth parasites protect against atopy and allergic disease? Clin Exp Allergy. 2009;39(1):20-32. doi: 10.1111/j.1365-2222.2008.03134.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. Adjusting for Sex in Multivariable Regression Model
eFigure 2. Adjusting for Primary Care Visits in Multivariable Regression Model
eFigure 3. Univariate Odds Ratios
eFigure 4. Adjusted Odds Ratios
eMethods. Evaluation of Heterogeneity