Key Points
Question
What is the variation in survival after out-of-hospital cardiac arrest between emergency medical services (EMS) agencies?
Findings
In this cohort study, among 43 656 adults treated for out-of-hospital cardiac arrest by any of 112 EMS agencies, there was a median difference of 56% in the odds of survival to hospital discharge for similar participants between any 2 randomly selected EMS agencies, after adjusting for known measured sources of variability and clustering of patients within agencies.
Meaning
This study suggests there is substantial unexplained variation in survival after out-of-hospital cardiac arrest across treating EMS agencies in North America, despite controlling for documented patient and agency characteristics.
This cohort study at 10 sites in the United States and Canada quantifies variation in patient outcomes across emergency medical service agencies after out-of-hospital cardiac arrest.
Abstract
Importance
Emergency medical services (EMS) deliver essential initial care for patients with out-of-hospital cardiac arrest (OHCA), but the extent to which patient outcomes vary between different EMS agencies is not fully understood.
Objective
To quantify variation in patient outcomes after OHCA across EMS agencies.
Design, Setting, and Participants
This observational cohort study was conducted in the Resuscitation Outcomes Consortium (ROC) Epistry, a prospective multicenter OHCA registry at 10 sites in North America. Any adult with OHCA treated by an EMS from April 2011 through June 2015 was included. Data analysis occurred from May 2017 to March 2018.
Exposure
Treating EMS agency.
Main Outcomes and Measures
The primary outcome was survival to hospital discharge. Secondary outcomes were return of spontaneous circulation at emergency department arrival and favorable functional outcome at hospital discharge (defined as a modified Rankin scale score ≤3). Multivariable hierarchical logistic regression models were used to adjust confounders and clustering of patients within EMS agencies, and calculated median odds ratios (MORs) were used to quantify the extent of residual variation in outcomes between EMS agencies.
Results
We identified 43 656 patients with OHCA treated by 112 EMS agencies. At EMS agency level, we observed large variations in survival to hospital discharge (range, 0%-28.9%; unadjusted MOR, 1.43 [95% CI, 1.34-1.54]), return of spontaneous circulation on emergency department arrival (range, 9.0%-57.1%; unadjusted MOR, 1.53 [95% CI, 1.43-1.65]), and favorable functional outcome (range, 0%-20.4%; unadjusted MOR, 1.54 [95% CI, 1.40-1.73]). This variation persisted despite adjustment for patient-level and EMS agency–level factors known to be associated with outcomes (adjusted MOR for survival 1.56 [95% CI 1.44-1.73]; adjusted MOR for return of spontaneous circulation at emergency department arrival, 1.50 [95% CI, 1.41-1.62]; adjusted MOR for functionally favorable survival, 1.53 [95% CI, 1.37-1.78]). After restricting analysis to those who survived more than 60 minutes after hospital arrival and including hospital treatment characteristics, the variation persisted (adjusted MOR for survival, 1.49 [95% CI, 1.36-1.69]; adjusted MOR for functionally favorable survival, 1.34 [95% CI, 1.20-1.59]).
Conclusions and Relevance
We found substantial variations in patient outcomes after OHCA between a large group of EMS agencies in North America that were not explained by documented patient-level and EMS agency–level variables.
Introduction
Out-of-hospital cardiac arrest (OHCA) is a major public health problem worldwide.1 In North America, survival after OHCA greatly varies across geographic regions.2,3,4 Although some factors (eg, layperson cardiopulmonary resuscitation [CPR] and location of arrest) are contributing to the geographic variation in survival after OHCA,5 reasons for this variation have not been fully investigated. Understanding the relative contributing factors to this variation may reveal modifiable targets for interventions to refine performance and improve patient outcomes after OHCA.
Emergency medical services (EMS) play a critical role in OHCA management as a part of the chain of survival and may explain some of the variation in outcomes after OHCA.6 The National Academy of Medicine recently recommended enhancing the capabilities and performance of EMS systems as one step to improve cardiac arrest survival.7,8 However, the extent to which EMS agency factors contribute to the variation in outcomes after OHCA is unclear. Differences between EMS agencies are often attributed to differences in the population served,9 geographical challenges to response time,10 or practice patterns, such as the initiation of resuscitation attempts in patients with EMS-assessed OHCA.11 Previous studies comparing outcomes across EMS agencies have lacked sufficient power to separate the EMS factors from differences in patient demographics, cardiac arrest characteristics, and hospital care.12
To address this knowledge gap, we quantified the variation in patient outcomes after OHCA between EMS agencies in a large cohort with detailed patient-level and EMS agency–level data. We tested the hypothesis that variation in outcomes among those treated by differing EMS agencies would persist after adjusting for known confounders and clustering of patients within agencies.
Methods
Study Design and Setting
The Resuscitation Outcomes Consortium (ROC) was a clinical research network that conducted trials in OHCA and trauma at 10 regional coordinating sites across North America, their affiliated EMS agencies, and participating hospitals.13,14 We performed a secondary analysis of data collected from April 2011 through June 2015 in the ROC Epistry–Cardiac Arrest, a database of prospectively identified consecutive patients with OHCA, which we have previously described in detail.13,14
Investigators acquired data under a waiver of informed consent for a minimal risk intervention with institutional review board approval at each coordinating site. The ROC data coordinating center created the final database from deidentified data transmitted from participating sites. The institutional review board at the University of Pittsburgh approved this secondary analysis of deidentified data.
Study Participants
We included adults (≥18 years old) with EMS-treated nontraumatic OHCA, defined as initiation of resuscitation attempts with shock delivery by an external defibrillator (by a layperson or EMS personnel) or chest compressions by EMS personnel. We excluded patients in whom resuscitations were terminated in the prehospital setting because of confirmation of a preexisting written do not resuscitate orders, patients initially treated by EMS agencies that did not participate in ROC, patients treated by EMS agencies that treated 10 or fewer OHCA cases annually, cases with missing data for the primary outcome, and cases with an unidentifiable primary EMS agency.
Study Variables
We present study variables in eFigure 1 in Supplement 1. Patient-level variables included in risk-adjusted models are (1) patient demographics: age (continuous) and sex (male or female); (2) cardiac arrest event characteristics: year of arrest (2011 through 2015),15 initial rhythm (shockable, pulseless electrical activity, or asystole), location of arrest (a public or private location), witness to collapse (a bystander, EMS personnel, or no witness); (3) layperson interventions: initiation of layperson CPR and public automated external defibrillator (AED) use (no layperson intervention, layperson CPR only, layperson CPR, and public AED use); (4) EMS interventions: number of treating EMS personnel within 15 minutes after an emergency (911) call (categorized as fewer than 6 or more than 6 persons),16 EMS response time (defined as interval from the emergency call to first EMS vehicle arrival on scene, measured as a continuous variable), prehospital epinephrine administration (presence or absence), attempted prehospital advanced airway placement with a tracheal intubation or supraglottic device (yes or no), median chest compression rate per minute (<100, 100-120, or >120), median chest compression fraction (<0.8 or ≥0.8); and (5) postresuscitation treatments: percutaneous coronary intervention (PCI) within 24 hours following hospital arrival (presence or absence) and induced targeted temperature management (TTM; presence or absence). We defined induced TTM as any active attempt to monitor and maintain core body temperature at or less than 36°C.17 We included PCI and TTM variables only in the subgroup analysis of EMS-treated patients who survived longer than 60 minutes after hospital arrival and whose survival and functional outcomes were potentially affected by subsequent hospital care.17
The EMS agency–level variables of the primary EMS agency responsible for resuscitation included EMS crew composition characteristic (advanced life support [ALS], basic life support [BLS], or a combination of both BLS and ALS), the proportion of patients who received any resuscitation attempt among EMS-assessed OHCA at each agency (a continuous variable),11 an ALS-BLS tiered system (yes or no), and area of EMS coverage (rural, suburban, or urban). We defined area of EMS coverage as rural (0-99 residents/km2 or 0-278 residents/mi2), suburban (100-400 residents/km2 or 279-1108 residents/mi2), and urban (>400 residents/km2 or >1108 residents/mi2).14 We assigned 1 primary EMS agency to each OHCA case. If a single patient was treated by multiple agencies (eg, an ALS-BLS tiered system), we assigned the primary EMS agency as per eFigure 2 in Supplement 1: (1) the ALS agency was the primary agency if the ALS agency arrived at the scene earlier than the BLS agency, (2) the ALS agency was the primary agency if the BLS agency arrived at the scene earlier than the ALS agency but ALS intervention was provided within 6 minutes of BLS agency arrival, and (3) the BLS agency was the primary agency if the BLS agency arrived at the scene earlier than the ALS agency, and no ALS intervention was provided within 6 minutes from BLS agency arrival. We defined ALS interventions as the delivery of an advanced airway (endotracheal tube or supraglottic airway), manual defibrillation, or intravenous drug therapy.18 We chose a 6-minute threshold to represent 3 optimal BLS CPR cycles (2 minutes of CPR followed by a pulse check and defibrillation as appropriate) and transition from BLS to ALS care.19 These covariates were chosen a priori based on their known associations with survival from prior studies of OHCA, biologic plausibility, and adequate ascertainment.11,15,16,17,18,19,20,21,22,23
Outcome Measure
The primary outcome was survival to hospital discharge. Although return of spontaneous circulation (ROSC) at emergency department arrival may be an important benchmark of prehospital care, we elected to use survival to hospital discharge as our primary outcome, because this allowed us to investigate several determinants of the patient-centered outcome in the chain of survival. Secondary outcomes were favorable functional outcome at hospital discharge, defined as modified Rankin scale score of 3 or less, and ROSC at emergency department arrival.
Statistical Analysis
We first described the unadjusted rate of survival to hospital discharge after OHCA within each EMS agency. We ranked and grouped EMS agencies into quartiles according to their unadjusted survival rates and reported differences in patient-level and EMS agency–level factors by quartiles. We described the variability in favorable functional outcome at hospital discharge and ROSC at emergency department arrival between EMS agencies.
We then cumulatively constructed a series of multivariable hierarchical logistic regression models predicting survival to hospital discharge, functional outcome at hospital discharge, and ROSC at emergency department arrival, based on previously described patient-level and EMS agency–level variables (eFigure 1 in Supplement 1).24 These models included the full cohort of patients with EMS-treated OHCA and accounted for clustering of patients within each EMS agency. We treated EMS agency as a random effect and nested individual patients within each agency, whereas patient-level and EMS agency–level variables were modeled as fixed effects. From these models, we reported adjusted survival outcome for each agency and calculated median odds ratios (MORs) to quantify the residual variation in outcomes between EMS agencies.3,25 We derived MORs from the variance estimate of the random intercept in the hierarchical regression model.25 Conceptually, the MORs represents the relative odds of outcome for 2 patients with similar characteristics except for treatment by 2 different, randomly selected EMS agencies.25 (For example, an MOR of 2.0 indicates a median 2-fold difference in the odds of outcome for similar individuals treated by 2 different, randomly selected EMS agencies.) We also performed stratified analyses by initial rhythm: those with a shockable rhythm (ventricular fibrillation, pulseless ventricular tachycardia, and shocked by an AED) vs nonshockable rhythm (pulseless electrical activity, asystole, and not shocked by an AED). We only included patients without missing covariates in the multivariable hierarchical models and reported difference in characteristics with standardized mean difference of covariates between patients with and without missing covariates. We considered an absolute standardized mean difference within 0.25 to be a small difference between groups for each covariate.26 For the secondary outcome of favorable functional outcome at hospital discharge, we further excluded patients with missing functional status at hospital discharge and covariates in the models.
Next, as a subgroup analysis, we fitted multivariable hierarchical logistic regression models with patients nested within EMS agency in the subgroup of patients with EMS-treated OHCA who survived more than 60 minutes after hospital arrival for whom subsequent hospital care potentially affected survival and functional outcomes (eFigure 1 in Supplement 1).17,27 The hierarchical models predicted survival to hospital discharge and favorable functional outcome at hospital discharge. These hierarchical models cumulatively adjusted for previously described patient-level and EMS agency–level variables, including postresuscitation treatments (eFigure 1 in Supplement 1). We again calculated MORs to quantify variation in survival and functional outcomes between EMS agencies and repeated stratified analyses by initial rhythm.
Finally, we conducted 3 sensitivity analyses in which we changed model covariates to assess the robustness of the findings. First, we included chest compression depth as a patient-level covariate, as well as previously described covariates in the hierarchical models, with the full cohort of patients with EMS-treated OHCA. We did not include chest compression depth in the primary analysis, because only a subset of defibrillators were able to measure chest compression depth, with the result that the chest compression depth was systematically missing for all cases in some EMS agencies.
Then, for patients treated by multiple EMS agencies, we applied 2 alternative definitions of the primary agency: (1) the first arriving agency as the primary agency and (2) the highest level of agency (ie, ALS agency, where present) as the primary agency. We recalculated MORs for outcomes and repeated the analyses stratified these by initial rhythms.
We used S-Plus version 6.2.1 (TIBCO Software Inc) for data management and Stata version 11 (StataCorp) for our analyses. Data analysis occurred from May 2017 to March 2018.
Results
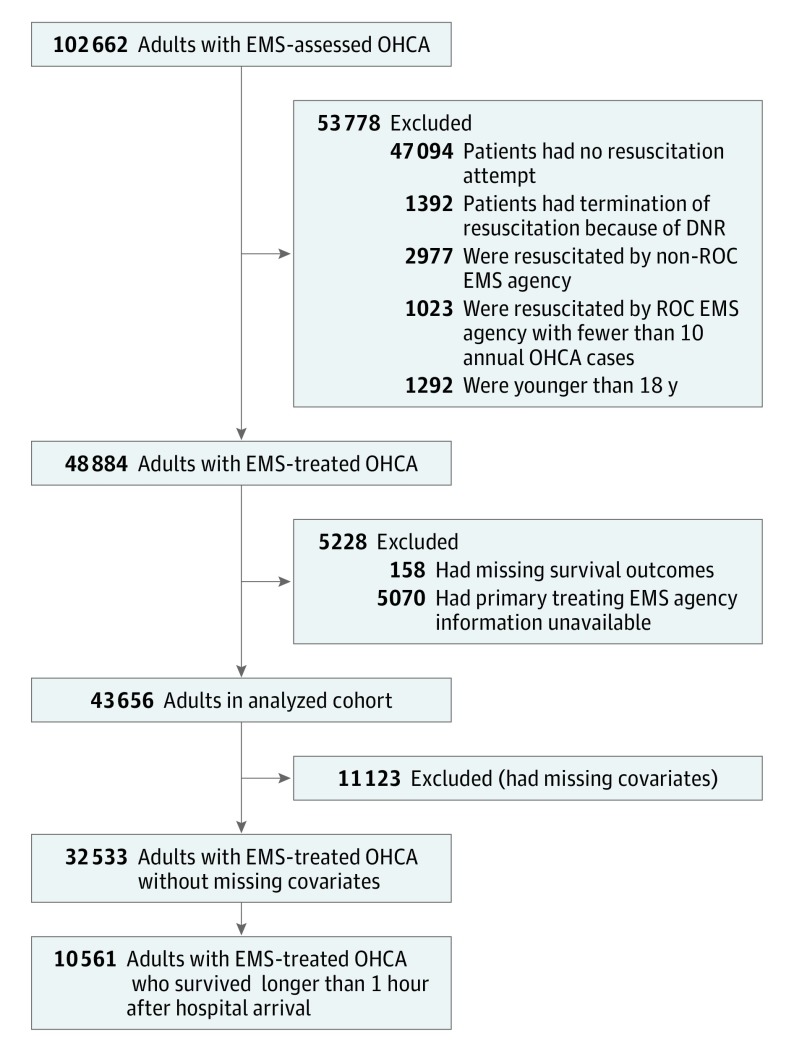
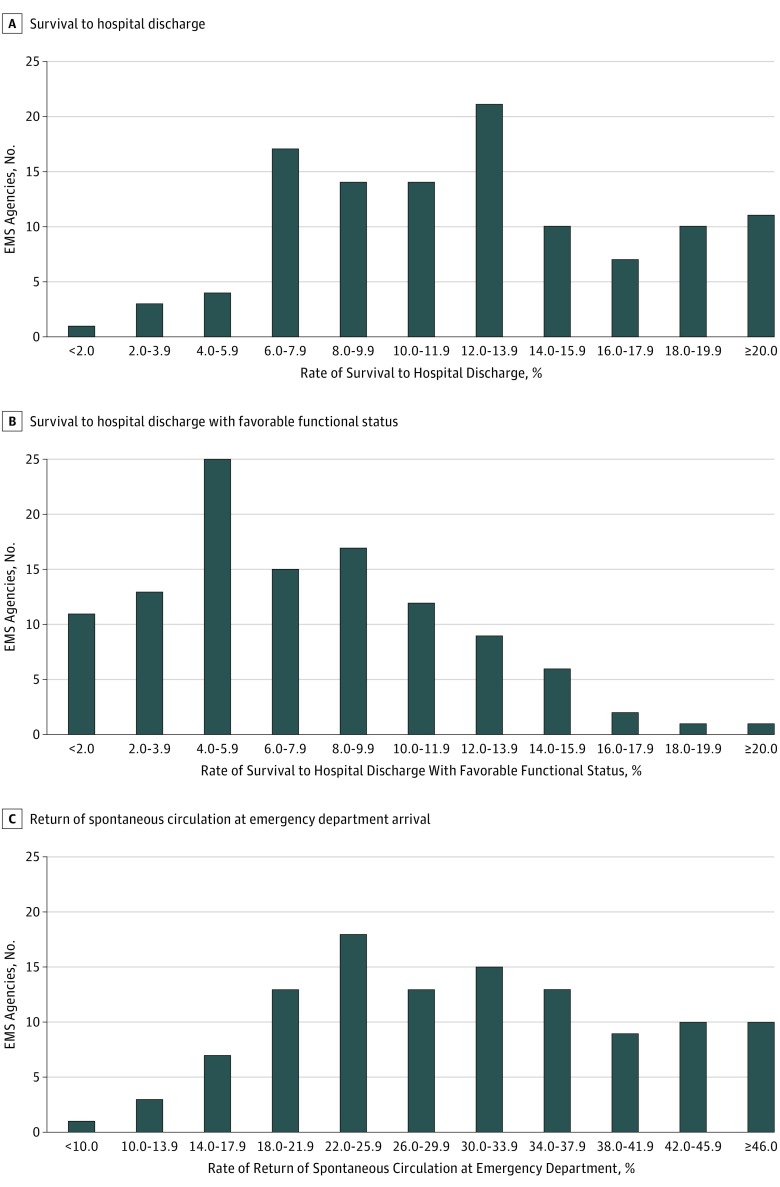
During the study period, participating EMS agencies assessed 102 662 patients with OHCA (Figure 1). Of these, 43 656 were treated by 112 EMS agencies (13 ALS agencies, 52 BLS agencies, and 47 ALS-BLS combined agencies) and included in our primary analysis. For 39 622 patients (90.8%), the first arriving EMS agency was assigned as the primary EMS agency. Survival to hospital discharge occurred in 4912 of 43 656 patients with EMS-treated OHCA (11.3%), and favorable functional outcome at hospital discharge occurred in 1650 of 22 498 patients with EMS-treated OHCA whose functional outcome were available (7.3%). The rate of survival to hospital discharge in each EMS agency ranged from 0% (0 survivors among 36 patients treated by 1 EMS agency) to 28.9% (66 survivors among 228 patients treated by 1 agency; Figure 2A). The rate of favorable functional outcome at hospital discharge ranged from 0% (0 survivors among 87 patients treated by 1 EMS agency) to 20.4% (11 survivors among 54 patients treated by 1 EMS agency; Figure 2B). The rate of ROSC at emergency department arrival ranged from 9.0% (9 survivors among 100 patients treated by 1 EMS agency) to 57.1% (48 survivors among 84 patients treated by 1 EMS agency; Figure 2C). We reported the estimated rate of survival to hospital discharge at each EMS agency after adjustment for patient-level and EMS agency–level variables in eFigure 3 in Supplement 1. A total of 10 561 EMS-treated patients with OHCA survived more than 60 minutes after arrival at 204 hospitals (Figure 1), and these patients constituted a subgroup for whom we also considered the association of postresuscitation management with survival and functional outcomes.
Figure 1. Patient Flow.
DNR indicates do not resuscitate [orders]; EMS, emergency medical services; OHCA, out-of-hospital cardiac arrest; ROC, Resuscitation Outcome Consortium.
Figure 2. Outcome Variations Between Emergency Medical Services (EMS) Agencies.
A, Variations in rate of survival to hospital discharge; B, favorable functional outcome at hospital discharge; and C, return of spontaneous circulation at emergency department arrival.
Table 1 shows characteristics of patient, cardiac arrest event, layperson interventions, EMS interventions, and responding EMS agencies. When categorizing EMS agencies into quartiles based on the rate of patient survival, patients treated by the highest-quartile EMS agencies compared with the lowest-quartile agencies tended to be younger (median [interquartile range (IQR)] age, overall: 66.0 [54.0-79.0] years; lowest quartile: 67.0 [55.0-79.0] years; highest quartile: 65.0 [53.0-77.0] years), be male (overall: 27 524 [63.0%]; lowest quartile: 7379 [60.1%]; highest-quartile: 4444 [65.0%]), have shockable initial heart rhythms (overall: 9717 [22.3%]; lowest quartile: 2317 [18.9%]; highest quartile: 1821 [26.6%]), collapse in a public location (overall: 6235 [14.3%]; lowest quartile: 1502 (12.2%]; highest quartile: 1163 [17.0%]), have a witnessed collapse (overall: 21 347 [48.9%]; lowest quartile: 5731 [46.7%]; highest quartile: 3469 [50.7%]), and receive layperson interventions (overall: 18 762 [43.0%]; lowest quartile: 4716 [38.4%]; highest quartile: 3716 [54.3%]; Table 1). Patients treated by the EMS agencies with survival rates in the highest quartile more often had treatment by more than 6 responding EMS personnel (overall: 12 511 [28.7%]; lowest quartile: 1947 [15.9%]; highest quartile: 4114 [60.1%]), a shorter time interval from an emergency telephone call to EMS defibrillation (overall median [IQR], 12.2 [9.1-20.1] minutes; lowest quartile: 13.0 [9.4-22.1] minutes; highest quartile: 11.0 [8.4-19.0] minutes), advanced airways attempted (overall: 34 392 [78.8%]; lowest quartile: 9576 [78.0%]; highest quartile: 5972 [87.3%]), and treatment by an ALS-BLS tiered system (overall: 25 642 [58.7%]; lowest quartile: 4466 [36.4%]; highest quartile: 5194 [75.9%]; Table 1). Percentages were similar among patients who survived more than 60 minutes after hospital arrival (eTable 1 in Supplement 1).
Table 1. Patient, Cardiac Arrest Event, Layperson and EMS Interventions, and EMS Agency Characteristics, Stratified by Quartiles of Survival at EMS Agency.
| Characteristic | No. (%) | ||||
|---|---|---|---|---|---|
| Total | EMS Agencies With Survival Rates in Lowest Quartilea | EMS Agencies With Survival Rates in Second-Lowest Quartilea | EMS Agencies With Survival Rates in Second-Highest Quartilea | EMS Agencies With Survival Rates in Highest Quartilea | |
| Patients | 43 656 | 12 272 (28.1) | 17 842 (40.9) | 6701 (15.3) | 6841 (15.7) |
| EMS agencies | 112 (100) | 28 (25.0) | 28 (25.0) | 28 (25.0) | 28 (25.0) |
| Patient demographics | |||||
| Age, median (IQR), y | 66.0 (54.0-79.0) | 67.0 (55.0-79.0) | 67.0 (55.0-80.0) | 67.0 (54.0-79.0) | 65.0 (53.0-77.0) |
| Sex | |||||
| Male | 27 524 (63.0) | 7379 (60.1) | 11 339 (63.6) | 4362 (65.1) | 4444 (65.0) |
| Unknown | 18 (0.0) | 1 (0.0) | 8 (0.0) | 5 (0.1) | 4 (0.1) |
| Cardiac arrest event characteristics | |||||
| Year of arrest | |||||
| 2011 | 4508 (10.3) | 1192 (9.7) | 1927 (10.8) | 682 (10.2) | 707 (10.3) |
| 2012 | 10 118 (23.2) | 2562 (20.9) | 4222 (23.7) | 1672 (25.0) | 1662 (24.3) |
| 2013 | 11 242 (25.8) | 3156 (25.7) | 4617 (25.9) | 1744 (26.0) | 1725 (25.2) |
| 2014 | 11 903 (27.3) | 3630 (29.6) | 4693 (26.3) | 1706 (25.5) | 1874 (27.4) |
| 2015 | 5885 (13.5) | 1732 (14.1) | 2383 (13.4) | 897 (13.4) | 873 (12.8) |
| Initial rhythm | |||||
| Shockable | 9717 (22.3) | 2317 (18.9) | 3942 (22.1) | 1637 (24.4) | 1821 (26.6) |
| Nonshockable | 33 084 (75.8) | 9730 (79.3) | 13 581 (76.1) | 4908 (73.2) | 4865 (71.1) |
| Unknown | 855 (1.9) | 225 (1.8) | 319 (1.8) | 156 (2.3) | 155 (2.2) |
| Location | |||||
| Public | 6235 (14.3) | 1502 (12.2) | 2588 (14.5) | 982 (14.7) | 1163 (17.0) |
| Home | 31 846 (72.9) | 8641 (70.4) | 13 438 (75.3) | 4987 (74.4) | 4780 (69.9) |
| Other | 5475 (12.5) | 2096 (17.1) | 1760 (9.9) | 724 (10.8) | 895 (13.1) |
| Unknown | 100 (0.2) | 33 (0.3) | 56 (0.3) | 8 (0.1) | 3 (0.0) |
| Witnessed collapse | |||||
| Bystander | 15 949 (36.5) | 4217 (34.4) | 6477 (36.3) | 2644 (39.5) | 2611 (38.2) |
| EMS | 5398 (12.4) | 1514 (12.3) | 2228 (12.5) | 798 (11.9) | 858 (12.5) |
| None | 21 270 (48.7) | 6212 (50.6) | 8617 (48.3) | 3140 (46.9) | 3301 (48.3) |
| Unknown | 1039 (2.4) | 329 (2.7) | 520 (2.9) | 119 (1.8) | 71 (1.0) |
| Layperson interventions | |||||
| None | 24 042 (55.1) | 7318 (59.6) | 10 160 (56.9) | 3573 (53.3) | 2991 (43.7) |
| Layperson CPR only | 16 831 (38.6) | 4187 (34.1) | 6685 (37.5) | 2659 (39.7) | 3300 (48.2) |
| Layperson CPR and public access AED use | 1931 (4.4) | 529 (4.3) | 652 (3.7) | 334 (5.0) | 416 (6.1) |
| Unknown | 852 (2.0) | 238 (1.9) | 345 (1.9) | 135 (2.0) | 134 (2.0) |
| EMS interventions | |||||
| No. of treating EMS personnel within 15 min after 911 call | |||||
| Mean (SD) | 5.6 (2.1) | 5.3 (1.8) | 5.5 (2.0) | 5.4 (2.1) | 7.0 (2.3) |
| ≤6 | 31 068 (71.2) | 10 266 (83.7) | 13 342 (74.8) | 4733 (70.6) | 2727 (39.9) |
| >6 | 12 511 (28.7) | 1947 (15.9) | 4482 (25.1) | 1968 (29.4) | 4114 (60.1) |
| Unknown | 77 (0.2) | 59 (0.5) | 18 (0.1) | 0 (0.0) | 0 (0.0) |
| EMS response time (time interval from first telephone call to first EMS arrival) | |||||
| Median (IQR), min | 5.4 (4.2-6.9) | 5.1 (4.0-6.6) | 5.5 (4.2-7.0) | 5.9 (4.7-7.4) | 5.1 (4.0-6.4) |
| Unknown | 521 (1.2) | 279 (2.3) | 187 (1.0) | 45 (0.7) | 10 (0.1) |
| Time interval from first telephone call to defibrillation | |||||
| Median (IQR), min | 12.2 (9.1-20.1) | 13.0 (9.4-22.1) | 12.2 (9.2-19.6) | 12.3 (9.5-19.9) | 11.0 (8.4-19.0) |
| Unknown | 29 466 (67.5) | 8914 (72.6) | 11 915 (66.8) | 4413 (65.9) | 4224 (61.7) |
| Epinephrine administration | |||||
| Yes | 36 907 (84.5) | 10 580 (86.2) | 15 330 (85.9) | 5512 (82.3) | 5485 (80.2) |
| No | 6715 (15.4) | 1679 (13.7) | 2497 (14.0) | 1183 (17.7) | 1356 (19.8) |
| Unknown | 34 (0.1) | 13 (0.1) | 15 (0.1) | 6 (0.1) | 0 (0.0) |
| Attempted advanced airway | |||||
| Yes | 34 392 (78.8) | 9576 (78.0) | 13 614 (76.3) | 5230 (78.0) | 5972 (87.3) |
| No | 9222 (21.1) | 2679 (21.8) | 4211 (23.6) | 1463 (21.8) | 869 (12.7) |
| Unknown | 42 (0.1) | 17 (0.1) | 17 (0.1) | 8 (0.1) | 0 (0.0) |
| Chest compression fraction | |||||
| Median (IQR) | 0.85 (0.77-0.91) | 0.83 (0.74-0.90) | 0.85 (0.76-0.91) | 0.85 (0.77-0.91) | 0.89 (0.81-0.95) |
| Unknown | 8212 (18.8) | 2626 (21.4) | 2986 (16.7) | 1478 (22.1) | 1122 (16.4) |
| Chest compression rate | |||||
| Median (IQR), per minute | 108.5 (102.1-116.4) |
107.9 (101.5-117.3) |
108.0 (102.0-115.5) |
108.9 (102.5-117.1) |
110.1 (104.0-116.7) |
| Unknown | 8387 (19.2) | 2424 (19.8) | 3013 (16.9) | 1449 (21.6) | 1501 (21.9) |
| EMS agency characteristics | |||||
| Crew composition of primary EMS agency | |||||
| BLS | 9848 (22.6) | 2912 (23.7) | 2049 (11.5) | 3211 (47.9) | 1676 (24.5) |
| ALS | 949 (2.2) | 96 (0.8) | 0 (0.0) | 406 (6.1) | 447 (6.5) |
| BLS/ALS | 32 859 (75.3) | 9264 (75.5) | 15 793 (88.5) | 3084 (46.0) | 4718 (69.0) |
| Proportion of patients who received resuscitation attempt among EMS-assessed OHCA in each EMS agency, mean (SD), % | 54.0 (15.5) | 57.8 (18.0) | 50.2 (11.6) | 58.9 (16.9) | 52.5 (15.7) |
| ALS-BLS tiered response system | 25 642 (58.7) | 4466 (36.4) | 11 561 (64.8) | 4421 (66.0) | 5194 (75.9) |
| Area of EMS agency coverage | |||||
| Rural | 1835 (4.2) | 803 (6.5) | 94 (0.5) | 535 (8.0) | 403 (5.9) |
| Suburban | 8329 (19.1) | 288 (2.3) | 3005 (16.8) | 2781 (41.5) | 2255 (33.0) |
| Urban | 33 492 (76.7) | 11 181 (91.1) | 14 743 (82.6) | 3385 (50.5) | 4183 (61.1) |
Abbreviations: AED, automated external defibrillator; ALS, advanced life support; BLS, basic life support; CPR, cardiopulmonary resuscitation; EMS, emergency medical services; IQR, interquartile range.
Quartiles for survival rates were 0% to 8.46% (lowest); 8.47% to 12.54% (second lowest), 12.55% to 15.84% (second highest), and 15.85% to 28.95% (highest).
After excluding 11 123 patients with missing covariates, we included 32 533 patients in the multivariable hierarchical models that determined the association of survival with hospital discharge (Figure 1). We reported percentage of missing variables and characteristics of patients with and without missing variables in eTable 2 in Supplement 1. Most of the excluded patients were missing the chest compression fraction (n = 8212) and/or the chest compression rate (n = 8387; eTable 2 in Supplement 1). For most patient-level and EMS agency–level variables, characteristics were similar between patients with and without missing data (standardized mean differences within 0.25; eTable 2 in Supplement 1). The unadjusted MOR for survival to hospital discharge in EMS-treated OHCA was 1.43 (95% CI, 1.34-1.54; Table 2). After adjustment for patient-level and EMS agency–level factors, the MOR for survival increased to 1.56 (95% CI, 1.44-1.73; Table 2 and eTable 3 in Supplement 1).
Table 2. Variation in Survival and Functional Outcomes After EMS-Treated Out-of-Hospital Cardiac Arrest Between EMS Agencies.
| Adjustment | Median Odds Ratios for EMS Agency Effect (95% CI) | ||
|---|---|---|---|
| Survival to Hospital Discharge | Favorable Functional Outcome at Discharge | Return of Spontaneous Circulation at Emergency Department Arrival | |
| EMS-Treated Out-of-Hospital Cardiac Arrest | |||
| Patients, No. | 32 533 | 18 442 | 32 528 |
| Adjustments | |||
| Unadjusted | 1.43 (1.34-1.54) | 1.54 (1.40-1.73) | 1.53 (1.43-1.65) |
| 1a | 1.42 (1.33-1.53) | 1.56 (1.42-1.76) | 1.53 (1.43-1.65) |
| 2b | 1.45 (1.35-1.58) | 1.60 (1.44-1.83) | 1.57 (1.47-1.70) |
| 3c | 1.43 (1.34-1.56) | 1.58 (1.42-1.81) | 1.56 (1.46-1.69) |
| 4d | 1.57 (1.45-1.74) | 1.59 (1.41-1.85) | 1.54 (1.44-1.67) |
| 5e | 1.56 (1.44-1.73) | 1.53 (1.37-1.78) | 1.50 (1.41-1.62) |
| EMS-Treated Shockable Out-of-Hospital Cardiac Arrest | |||
| Patients, No. | 7602 | 4421 | 7600 |
| Adjustments | |||
| Unadjusted | 1.39 (1.30-1.52) | 1.51 (1.36-1.72) | 1.55 (1.43-1.70) |
| 1a | 1.41 (1.31-1.55) | 1.56 (1.40-1.79) | 1.56 (1.44-1.73) |
| 2b | 1.43 (1.33-1.58) | 1.54 (1.39-1.77) | 1.59 (1.46-1.76) |
| 3c | 1.39 (1.29-1.54) | 1.50 (1.35-1.72) | 1.57 (1.44-1.73) |
| 4d | 1.53 (1.39-1.73) | 1.57 (1.39-1.85) | 1.63 (1.49-1.83) |
| 5e | 1.53 (1.39-1.73) | 1.48 (1.32-1.75) | 1.58 (1.44-1.76) |
| EMS-Treated Nonshockable Out-of-Hospital Cardiac Arrest | |||
| Patients, No. | 24 931 | 14 021 | 24 928 |
| Adjustments | |||
| Unadjusted | 1.61 (1.45-1.82) | 1.66 (1.42-2.08) | 1.59 (1.48-1.74) |
| 1a | 1.57 (1.42-1.78) | 1.66 (1.42-2.08) | 1.59 (1.48-1.74) |
| 2b | 1.57 (1.42-1.79) | 1.69 (1.44-2.15) | 1.62 (1.50-1.78) |
| 3c | 1.58 (1.43-1.80) | 1.71 (1.45-2.17) | 1.62 (1.50-1.78) |
| 4d | 1.69 (1.51-1.94) | 1.56 (1.31-2.06) | 1.56 (1.45-1.71) |
| 5e | 1.64 (1.47-1.89) | 1.43 (1.21-1.98) | 1.52 (1.41-1.65) |
Abbreviation: EMS, emergency medical services.
Adjustment 1 was for patient demographics: patient age and sex.
Adjustment 2 was for patient demographics, as above, and cardiac arrest event characteristics: year of arrest, initial rhythm, location of arrest, and witnessed collapse.
Adjustment 3 was for patient demographics and cardiac arrest event characteristics, as above, and layperson interventions: layperson cardiopulmonary resuscitation and public access automated external defibrillator use.
Adjustment 4 was for patient demographics, cardiac arrest event characteristics, and layperson interventions, as above, and EMS interventions: number of treating EMS personnel within 15 minutes after emergency telephone call, EMS response time, epinephrine administration, attempted advanced airway, chest compression fraction, and chest compression rate.
Adjustment 5 was for patient demographics, cardiac arrest event characteristics, layperson interventions, and EMS interventions, as above, and EMS agency-level variables: EMS crew composition characteristics, proportion of patients who received any resuscitation attempt among EMS-assessed out-of-hospital cardiac arrest, advanced life support–basic life support tiered system, and area of EMS coverage.
In the subgroup of those who survived more than 60 minutes after hospital arrival, the unadjusted MOR for survival was 1.39 (95% CI, 1.29-1.53; Table 3). After adjustment for patient-level and EMS agency–level variables, including postresuscitation treatments (eg, PCI within 24 hours after hospital arrival and induced TTM), the MOR for survival increased to 1.49 (95% CI, 1.36-1.69).
Table 3. Variation in Survival and Functional Outcomes Between EMS Agencies in the Subcohort of EMS-Treated Patients With Out-of-Hospital Cardiac Arrest Who Survived Longer Than 60 Minutes after Hospital Arrival.
| Adjustment | Median Odds Ratios for EMS Agency Effect (95% CI) | |
|---|---|---|
| Survival to Hospital Discharge | Favorable Functional Outcome | |
| EMS-Treated Out-of-Hospital Cardiac Arrest | ||
| Patients, No. | 7976 | 5481 |
| Adjustments | ||
| Unadjusted | 1.39 (1.29-1.53) | 1.55 (1.40-1.77) |
| 1a | 1.38 (1.28-1.52) | 1.56 (1.41-1.79) |
| 2b | 1.37 (1.27-1.52) | 1.48 (1.34-1.71) |
| 3c | 1.36 (1.26-1.51) | 1.47 (1.32-1.70) |
| 4d | 1.53 (1.39-1.73) | 1.46 (1.30-1.72) |
| 5e | 1.49 (1.36-1.68) | 1.35 (1.21-1.60) |
| 6f | 1.49 (1.36-1.69) | 1.34 (1.20-1.59) |
| EMS-Treated Shockable Out-of-Hospital Cardiac Arrest | ||
| Patients, No. | 3522 | 2363 |
| Adjustments | ||
| Unadjusted | 1.32 (1.21-1.50) | 1.43 (1.28-1.66) |
| 1a | 1.29 (1.18-1.48) | 1.44 (1.29-1.68) |
| 2b | 1.27 (1.16-1.47) | 1.39 (1.25-1.63) |
| 3c | 1.24 (1.13-1.45) | 1.36 (1.22-1.60) |
| 4d | 1.39 (1.25-1.63) | 1.40 (1.24-1.69) |
| 5e | 1.36 (1.23-1.59) | 1.27 (1.14-1.58) |
| 6f | 1.35 (1.22-1.58) | 1.26 (1.12-1.58) |
| EMS-Treated Nonshockable Out-of-Hospital Cardiac Arrest | ||
| Patients, No. | 4454 | 3118 |
| Adjustments | ||
| Unadjusted | 1.46 (1.31-1.70) | 1.64 (1.38-2.10) |
| 1a | 1.43 (1.29-1.66) | 1.63 (1.38-2.10) |
| 2b | 1.46 (1.31-1.70) | 1.64 (1.38-2.12) |
| 3c | 1.46 (1.31-1.70) | 1.65 (1.39-2.13) |
| 4d | 1.64 (1.44-1.98) | 1.51 (1.26-2.07) |
| 5e | 1.57 (1.38-1.87) | 1.38 (1.16-2.05) |
| 6f | 1.57 (1.38-1.87) | 1.37 (1.15-2.04) |
Abbreviation: EMS, emergency medical services.
Adjustment 1 was for patient demographics: patient age and sex.
Adjustment 2 was for patient demographics, as above, and cardiac arrest event characteristics: year of arrest, initial rhythm, location of arrest, and witnessed collapse.
Adjustment 3 was for patient demographics and cardiac arrest event characteristics, as above, and layperson interventions: layperson cardiopulmonary resuscitation and public access automated external defibrillator use.
Adjustment 4 was for patient demographics, cardiac arrest event characteristics, and layperson interventions, as above, and EMS interventions: number of treating EMS personnel within 15 minutes after emergency telephone call, EMS response time, epinephrine administration, attempted advanced airway, chest compression fraction, and chest compression rate.
Adjustment 5 was for patient demographics, cardiac arrest event characteristics, layperson interventions, and EMS interventions, as above, and EMS agency-level variables: EMS crew composition characteristics, proportion of patients who received any resuscitation attempt among EMS-assessed OHCA, advanced life support–basic life support tiered system, and area of EMS coverage.
Adjustment 6 was for patient demographics, cardiac arrest event characteristics, layperson interventions, EMS interventions, and EMS agency-level variables, as above, and treatment variables: percutaneous coronary intervention within 24 hours of hospital arrival and induced targeted temperature management.
Differences in MORs for favorable functional outcome at hospital discharge were similar in the total cohort of patients with EMS-treated OHCA and in the subgroup of those who survived more than 60 minutes after hospital arrival (Tables 2 and 3). When stratified by initial rhythm, differences in MORs for survival were greater for patients with nonshockable rhythms than those with shockable rhythms (Tables 2 and 3). In all sensitivity analyses, we found similar MORs (eTables 4, 5, and 6 in Supplement 1).
Discussion
In this analysis of a large prospective registry of patients with OHCA in North America, clinically important patient outcomes (eg, ROSC at ED arrival, survival to hospital discharge, and favorable functional outcome at hospital discharge) substantially differed across EMS agencies, despite adjustment for measured sources of variability. We observed a median difference of 56% in the odds of survival to hospital discharge for any 2 otherwise similar patients who were treated by any 2 randomly selected EMS agencies. We observed similar variation in those surviving to hospital care with adjustment for postresuscitation treatments (eg, PCI within 24 hours after hospital arrival and induced TTM) and in all sensitivity analyses. These data suggest that the between-agency variation resulted from unmeasured patient, EMS agency, hospital, and/or community characteristics, because the variation in outcomes persisted after adjustment for multiple measured factors.
We previously reported2 a 5-fold regional variation in the unadjusted rates of survival to hospital discharge after EMS-treated OHCA (3.0% to 16.3%) and EMS-treated OHCA with ventricular fibrillation (7.7% to 39.9%) across the same geographic sites between 2006 and 2007. Using more recent data between 2011 and 2015, we also found4 persisting regional variations in the unadjusted rates of survival to hospital discharge after EMS-treated OHCA (4.2% to 19.8%) and EMS-treated OHCA with shockable rhythm (11.9% to 47.1%) among the 10 ROC sites. Similarly, analysis of the Cardiac Arrest Registry to Enhance Survival database demonstrated large variation in unadjusted survival to hospital discharge (3.4% to 22.0%) across 132 counties in the United States.3 Across 10 regions in the United Kingdom, the crude survival to hospital discharge after OHCA ranged from 2.2% to 12.0% between ambulance services, and this variation persisted after adjustment for presumed causative mechanisms of illness, witnessed collapse, and initial rhythm.12 Our findings confirm and expand these observations by assessing a critical unit of OHCA management (ie, EMS agency) and including functional outcome and multiple health care settings with a robust statistical approach, accounting for known confounders and clustering of patients within EMS agencies.
The mechanisms of the observed variation in our study are likely multifactorial, including unmeasured patient-level factors (eg, comorbidity9 and first-responder interventions), EMS-level factors (eg, experience and training of EMS personnel),28 hospital-level factors (eg, practice variation in timing of withdrawal of life-sustaining therapy29 and receiving hospital characteristics30), and neighborhood-level factors (eg, racial/ethnic composition).31 We found that in all survival quartiles of EMS agencies, median chest compression fraction exceeded 0.80, and median chest compression rate was between 100 and 120 compressions per minute. Both metrics conform with current evidence-based practice guidelines.19,32 This suggests that most EMS agencies included in this analysis performed guideline-compliant chest compression fraction and chest compression rate, and that outcome differences are explained by other factors. We previously reported that the Utstein elements (age, sex, arrest cause, witness status, location of arrest, bystander CPR, initial rhythm, and EMS response interval) partially predicted the variation in survival after OHCA between the ROC sites.5 In this study, we found significant unexplained variation in outcomes after OHCA between EMS agencies, suggesting opportunities to capture contributing factors to the observed variation.
This study has implications for improvement of OHCA management. First, the analysis indicates that the highest-performing EMS agencies had more layperson interventions and more EMS personnel on scene. These metrics of quality of care may be used by other EMS agencies as targets to improve care and outcomes, although further evaluations of optimal measurement of EMS performance are needed. Second, our findings justify further efforts to identify potentially modifiable factors that may explain this residual variation in outcomes and could be targets of public health interventions. Such factors in EMS might include whether the decision to transport for further care is evidence based (ie, the Termination of Resuscitation Guideline) or left to the discretion of the paramedics or direct medical oversight.33 They may also include other factors in EMS culture and practice, such as EMS team design, team composition and roles, communication and leadership, and training and education. Indeed, recent in-hospital cardiac arrest research found these factors were important elements of resuscitation teams at top-performing hospitals.34 Further efforts are needed to identify features of high-performing EMS agencies in OHCA.
Limitations
Our study has several limitations. First, we cannot determine which unmeasured factors explain the observed differences in outcomes. These unmeasured factors include patient comorbidity,9 first-responder interventions, experience and training of treating EMS personnel,28 postresuscitation practice,29 hospital characteristics,30 and neighborhood factors.31 Second, our inference may not be fully generalizable to other health care settings. Because participating sites did not include all EMS agencies in each region but instead selected EMS agencies based on adherence to performance metrics, ability to conduct trials, or interest in participation in research, we may have underestimated the actual variation between all EMS agencies. Third, excluding patients with missing variables from our hierarchical models may have biased results. Although standardized mean differences of most covariates were within 0.25 between patients with and without missing variables, some covariates had greater than 0.25 comparative mean difference (eTable 2 in Supplement 1). Finally, we assigned 1 primary EMS agency to each OHCA case, even if a case was treated by multiple agencies. It is possible that our assignment of an agency did not reflect the agency that primarily managed the resuscitation. However, sensitivity analyses with 2 alternative definitions of primary EMS agency demonstrated similar results, which shows the findings are robust to different exposure definitions.
Conclusions
In this study of data from 112 EMS agencies in North America, patient outcomes after OHCA varied substantially between EMS agencies, despite adjustment for documented factors associated with outcomes. Further research is required to identify modifiable factors that are contributing to this observed variation to improve patient outcomes after OHCA.
eFigure 1. Multivariable Hierarchical Model with Patient- and EMS Agency-level Covariates
eFigure 2. Assignment of the Primary EMS Agency under Multiple Agencies Involvement
eFigure 3. Variation in Adjusted Rate of Survival to Hospital Discharge with 95% CI between EMS Agencies
eTable 1. Patient, Cardiac Arrest Event, Layperson and EMS Interventions, Post-resuscitation Management, and EMS Agency Characteristics among Those who Survived >60 minutes after Hospital Arrival, Stratified by Quartiles of Survival at EMS agency
eTable 2. Patient Demographics, Cardiac Arrest Event Characteristics, Layperson and EMS Interventions, EMS Agency Characteristics, and Outcome between Cases with and without Missing Variables
eTable 3. Coefficient in the Multivariable Hierarchical Model with Patient-level and EMS Agency-level Variables
eTable 4. Variation in Survival and Functional outcomes between EMS Agencies, including Compression Depth
eTable 5. Variation in Survival and Functional Outcomes after EMS-treated Out-of-Hospital Cardiac Arrest between EMS Agencies, Primary agency=first arriving agency
eTable 6. Variation in Survival and Functional outcomes after EMS-treated Out-of-Hospital Cardiac Arrest between EMS Agencies, Primary agency=highest level agency
Data Sharing Statement.
References
- 1.Benjamin EJ, Blaha MJ, Chiuve SE, et al. AHA Statistical Update. Heart diseases and stroke statistics—2017 update: a report from the American Heart Association. Circulation. 2017;135:e1-e458. doi: 10.1161/CIR.0000000000000485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nichol G, Thomas E, Callaway CW, et al. ; Resuscitation Outcomes Consortium Investigators . Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300(12):1423-1431. doi: 10.1001/jama.300.12.1423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Girotra S, van Diepen S, Nallamothu BK, et al. ; CARES Surveillance Group and the HeartRescue Project . Regional variation in out-of-hospital cardiac arrest survival in the United States. Circulation. 2016;133(22):2159-2168. doi: 10.1161/CIRCULATIONAHA.115.018175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zive DM, Schmicker R, Daya M, et al. Survival and variability over time from out of hospital cardiac arrest across large geographically diverse communities participating in the Resuscitation Outcome Consortium [published online July 24, 2018]. Resuscitation. doi: 10.1016/j.resuscitation.2018.07.023 [DOI] [PubMed] [Google Scholar]
- 5.Rea TD, Cook AJ, Stiell IG, et al. ; Resuscitation Outcomes Consortium Investigators . Predicting survival after out-of-hospital cardiac arrest: role of the Utstein data elements. Ann Emerg Med. 2010;55(3):249-257. doi: 10.1016/j.annemergmed.2009.09.018 [DOI] [PubMed] [Google Scholar]
- 6.Hazinski MF, Nolan JP, Aickin R, et al. Part 1: Executive summary: 2015 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation. 2015;132(16)(suppl 1):S2-S39. doi: 10.1161/CIR.0000000000000270 [DOI] [PubMed] [Google Scholar]
- 7.Institute of Medicine of the National Academies Strategies to Improve Cardiac Arrest Survival: A Time to Act. Washington, DC: National Academies Press; 2015. [PubMed] [Google Scholar]
- 8.Becker LB, Aufderheide TP, Graham R. Strategies to improve survival from cardiac arrest: a report from the Institute of Medicine. JAMA. 2015;314(3):223-224. doi: 10.1001/jama.2015.8454 [DOI] [PubMed] [Google Scholar]
- 9.Carew HT, Zhang W, Rea TD. Chronic health conditions and survival after out-of-hospital ventricular fibrillation cardiac arrest. Heart. 2007;93(6):728-731. doi: 10.1136/hrt.2006.103895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Masterson S, Wright P, O’Donnell C, et al. Urban and rural differences in out-of-hospital cardiac arrest in Ireland. Resuscitation. 2015;91:42-47. doi: 10.1016/j.resuscitation.2015.03.012 [DOI] [PubMed] [Google Scholar]
- 11.Brooks SC, Schmicker RH, Cheskes S, et al. ; Resuscitation Outcomes Consortium Investigators . Variability in the initiation of resuscitation attempts by emergency medical services personnel during out-of-hospital cardiac arrest. Resuscitation. 2017;117:102-108. doi: 10.1016/j.resuscitation.2017.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Perkins GD, Cooke MW. Variability in cardiac arrest survival: the NHS ambulance service quality indicators. Emerg Med J. 2012;29(1):3-5. doi: 10.1136/emermed-2011-200758 [DOI] [PubMed] [Google Scholar]
- 13.Morrison LJ, Nichol G, Rea TD, et al. ; ROC Investigators . Rationale, development and implementation of the Resuscitation Outcomes Consortium Epistry–Cardiac Arrest. Resuscitation. 2008;78(2):161-169. doi: 10.1016/j.resuscitation.2008.02.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Davis DP, Garberson LA, Andrusiek DL, et al. A descriptive analysis of emergency medical services systems participating in the Resuscitation Outcomes Consortium (ROC) network. Prehosp Emerg Care. 2007;11(4):369-382. doi: 10.1080/10903120701537147 [DOI] [PubMed] [Google Scholar]
- 15.Daya MR, Schmicker RH, Zive DM, et al. ; Resuscitation Outcomes Consortium Investigators . Out-of-hospital cardiac arrest survival improving over time: results from the Resuscitation Outcomes Consortium (ROC). Resuscitation. 2015;91:108-115. doi: 10.1016/j.resuscitation.2015.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Warren SA, Prince DK, Huszti E, et al. ; ROC Investigators . Volume versus outcome: more emergency medical services personnel on-scene and increased survival after out-of-hospital cardiac arrest. Resuscitation. 2015;94:40-48. doi: 10.1016/j.resuscitation.2015.02.019 [DOI] [PubMed] [Google Scholar]
- 17.Callaway CW, Schmicker RH, Brown SP, et al. ; ROC Investigators . Early coronary angiography and induced hypothermia are associated with survival and functional recovery after out-of-hospital cardiac arrest. Resuscitation. 2014;85(5):657-663. doi: 10.1016/j.resuscitation.2013.12.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Callaway CW, Soar J, Aibiki M, et al. ; Advanced Life Support Chapter Collaborators . Part 4: advanced life support, 2015 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation. 2015;132(16)(suppl 1):S84-S145. doi: 10.1161/CIR.0000000000000273 [DOI] [PubMed] [Google Scholar]
- 19.Travers AH, Perkins GD, Berg RA, et al. ; Basic Life Support Chapter Collaborators . Part 3: adult basic life support and automated external defibrillation, 2015 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation. 2015;132(16)(suppl 1):S51-S83. doi: 10.1161/CIR.0000000000000272 [DOI] [PubMed] [Google Scholar]
- 20.Sasson C, Rogers MA, Dahl J, Kellermann AL. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010;3(1):63-81. doi: 10.1161/CIRCOUTCOMES.109.889576 [DOI] [PubMed] [Google Scholar]
- 21.Nakahara S, Tomio J, Ichikawa M, et al. Association of bystander interventions with neurologically intact survival among patients with bystander-witnessed out-of-hospital cardiac arrest in Japan. JAMA. 2015;314(3):247-254. doi: 10.1001/jama.2015.8068 [DOI] [PubMed] [Google Scholar]
- 22.Hasselqvist-Ax I, Riva G, Herlitz J, et al. Early cardiopulmonary resuscitation in out-of-hospital cardiac arrest. N Engl J Med. 2015;372(24):2307-2315. doi: 10.1056/NEJMoa1405796 [DOI] [PubMed] [Google Scholar]
- 23.Hallstrom AP, Ornato JP, Weisfeldt M, et al. ; Public Access Defibrillation Trial Investigators . Public-access defibrillation and survival after out-of-hospital cardiac arrest. N Engl J Med. 2004;351(7):637-646. doi: 10.1056/NEJMoa040566 [DOI] [PubMed] [Google Scholar]
- 24.Goldstein H, Browne W, Rasbash J. Multilevel modelling of medical data. Stat Med. 2002;21(21):3291-3315. doi: 10.1002/sim.1264 [DOI] [PubMed] [Google Scholar]
- 25.Merlo J, Chaix B, Ohlsson H, et al. A brief conceptual tutorial of multilevel analysis in social epidemiology: using measures of clustering in multilevel logistic regression to investigate contextual phenomena. J Epidemiol Community Health. 2006;60(4):290-297. doi: 10.1136/jech.2004.029454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stuart EA. Matching methods for causal inference: a review and a look forward. Stat Sci. 2010;25(1):1-21. doi: 10.1214/09-STS313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stub D, Schmicker RH, Anderson ML, et al. ; ROC Investigators . Association between hospital post-resuscitative performance and clinical outcomes after out-of-hospital cardiac arrest. Resuscitation. 2015;92:45-52. doi: 10.1016/j.resuscitation.2015.04.015 [DOI] [PubMed] [Google Scholar]
- 28.Gold LS, Eisenberg MS. The effect of paramedic experience on survival from cardiac arrest. Prehosp Emerg Care. 2009;13(3):341-344. doi: 10.1080/10903120902935389 [DOI] [PubMed] [Google Scholar]
- 29.Elmer J, Torres C, Aufderheide TP, et al. ; Resuscitation Outcomes Consortium . Association of early withdrawal of life-sustaining therapy for perceived neurological prognosis with mortality after cardiac arrest. Resuscitation. 2016;102:127-135. doi: 10.1016/j.resuscitation.2016.01.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Carr BG, Kahn JM, Merchant RM, Kramer AA, Neumar RW. Inter-hospital variability in post-cardiac arrest mortality. Resuscitation. 2009;80(1):30-34. doi: 10.1016/j.resuscitation.2008.09.001 [DOI] [PubMed] [Google Scholar]
- 31.Starks MA, Schmicker RH, Peterson ED, et al. ; Resuscitation Outcomes Consortium (ROC) . Association of neighborhood demographics with out-of-hospital cardiac arrest treatment and outcomes: where you live may matter. JAMA Cardiol. 2017;2(10):1110-1118. doi: 10.1001/jamacardio.2017.2671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Meaney PA, Bobrow BJ, Mancini ME, et al. ; CPR Quality Summit Investigators, the American Heart Association Emergency Cardiovascular Care Committee, and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation . Cardiopulmonary resuscitation quality: [corrected] improving cardiac resuscitation outcomes both inside and outside the hospital: a consensus statement from the American Heart Association. Circulation. 2013;128(4):417-435. doi: 10.1161/CIR.0b013e31829d8654 [DOI] [PubMed] [Google Scholar]
- 33.Morrison LJ, Verbeek PR, Zhan C, Kiss A, Allan KS. Validation of a universal prehospital termination of resuscitation clinical prediction rule for advanced and basic life support providers. Resuscitation. 2009;80(3):324-328. doi: 10.1016/j.resuscitation.2008.11.014 [DOI] [PubMed] [Google Scholar]
- 34.Nallamothu BK, Guetterman TC, Harrod M, et al. How do resuscitation teams at top-performing hospitals for in-hospital cardiac arrest succeed? a qualitative study. Circulation. 2018;138(2):154-163. doi: 10.1161/CIRCULATIONAHA.118.033674 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. Multivariable Hierarchical Model with Patient- and EMS Agency-level Covariates
eFigure 2. Assignment of the Primary EMS Agency under Multiple Agencies Involvement
eFigure 3. Variation in Adjusted Rate of Survival to Hospital Discharge with 95% CI between EMS Agencies
eTable 1. Patient, Cardiac Arrest Event, Layperson and EMS Interventions, Post-resuscitation Management, and EMS Agency Characteristics among Those who Survived >60 minutes after Hospital Arrival, Stratified by Quartiles of Survival at EMS agency
eTable 2. Patient Demographics, Cardiac Arrest Event Characteristics, Layperson and EMS Interventions, EMS Agency Characteristics, and Outcome between Cases with and without Missing Variables
eTable 3. Coefficient in the Multivariable Hierarchical Model with Patient-level and EMS Agency-level Variables
eTable 4. Variation in Survival and Functional outcomes between EMS Agencies, including Compression Depth
eTable 5. Variation in Survival and Functional Outcomes after EMS-treated Out-of-Hospital Cardiac Arrest between EMS Agencies, Primary agency=first arriving agency
eTable 6. Variation in Survival and Functional outcomes after EMS-treated Out-of-Hospital Cardiac Arrest between EMS Agencies, Primary agency=highest level agency
Data Sharing Statement.