Key Points
Question
What is the state of hospice care in older patients hospitalized with heart failure?
Findings
In this cohort analysis of 121 990 Medicare beneficiaries in the American Heart Association Get With The Guidelines–Heart Failure registry, hospice discharges increased from 2% in 2005 to 5% in 2014. Patients discharged to hospice had a median survival of 11 days, and 4% of patients discharged to hospice were readmitted to the hospital; nonwhite race and younger age were the strongest predictors of hospital readmission.
Meaning
Hospice use remains infrequent in patients with heart failure, and those patients are referred late.
This cohort analysis of Medicare beneficiaries in the American Heart Association Get With The Guidelines–Heart Failure registry assesses rates of discharge to hospice, readmission after hospice, and survival in hospice in patients following hospital discharge.
Abstract
Importance
While 1 in 10 older patients hospitalized with heart failure (HF) die within 30 days, end-of-life care for this population is not well described.
Objective
To assess rates of discharge to hospice, readmission after hospice, and survival in hospice in patients following hospital discharge.
Design, Setting, and Participants
In this observational cohort analysis of patients in the multicenter American Heart Association Get With The Guidelines (GWTG)–HF registry linked to Medicare fee-for-service claims data, we analyzed patients 65 years and older discharged alive from the hospital between 2005 and 2014. We compared 4588 patients discharged to hospice with 4357 patients with advanced HF (ejection fraction ≤25% and any of the following: inpatient inotrope use, serum sodium level ≤130 mEq/L, blood urea nitrogen level ≥45 mg/dL [to convert to micromoles per liter, multiply by 0.357], systolic blood pressure ≤90 mm Hg, or comfort measures during hospitalization) not discharged to hospice and with 113 045 other patients with HF in the GWTG-HF registry. Data were analyzed from October 2017 to June 2018.
Main Outcomes and Measures
Discharge to hospice, rehospitalization, and mortality.
Results
Of the 4588 patients discharged to hospice, 2556 (55.7%) were female and 4047 (88.2%) were white, and they had a median (interquartile range) age of 86 (80-90) years. Hospice accounted for 4588 of 121 990 discharges (3.8%), of which 2424 (52.8%) were discharges to home hospice and 2164 (47.2%) were to a hospice facility. Hospice discharges increased from 2.0% (109 of 5528) in 2005 to 4.9% (968 of 19 590) in 2014. Patients discharged to hospice were older, white, and more symptomatic compared with patients with advanced HF (n = 4357) and other patients in the GWTG-HF registry (n = 113 045). The median (interquartile range) postdischarge survival time in patients discharged to hospice was 11 (3-63) days compared with 318 (78-1105) days in patients with advanced HF and 754 (221-1868) days in other patients in the GWTG-HF registry. A total of 739 patients (34.1%) discharged to hospice facilities died in less than 72 hours, while 295 (12.2%) discharged to home hospice died in less than 72 hours; 690 patients (15.0%) discharged from hospice lived for 6 months or more. Among hospitals with more than 25 hospice discharges, the median (interquartile range) hospice discharge rate was 3.5% (2.0%-5.7%). Readmission at 30 days was lower in patients discharged to hospice (189 [4.1%]) compared with patients with advanced HF (1185 [27.2%]) and others in the GWTG-HF registry (25 022 [22.2%]). Nonwhite race and younger age were the strongest predictors of readmission from hospice.
Conclusions and Relevance
Hospice use has grown to about 4.9% of Medicare HF hospital discharges, with significant hospital-level variation. Almost a quarter of patients discharged to hospice die within 3 days of discharge, and about 4.1% of patients are readmitted to the hospital within 30 days.
Introduction
Patients with heart failure (HF) report a high symptom burden, and despite therapeutic advances, the median survival among Medicare beneficiaries hospitalized with HF is only 2.1 years.1,2 Therefore, many patients with HF may benefit from palliative care and hospice.
Hospice, a Medicare benefit, is a form of palliative care for patients with an expected survival of less than 6 months. While the number of patients with HF dying in hospice is increasing, patients with cardiovascular disease have been identified as having the greatest unmet need for palliative care.3,4,5 Therefore, we used the American Heart Association Get With The Guidelines (GWTG)–HF hospital inpatient registry linked to Medicare claims data to assess trends, care patterns, and outcomes of patients with HF discharged to hospice.
Methods
The data for this analysis were obtained from the GWTG-HF registry linked to Medicare claims. The GWTG-HF program is a national registry that enrolls consecutive patients admitted to the hospital with worsening HF or if they develop HF symptoms during a hospitalization for which HF is the primary diagnosis at discharge.6 All participating institutions secured institutional review board approval as necessary. Because data were used primarily at the local sites for quality improvement, a waiver of informed consent was granted under the common rule. Quintiles (Cambridge, Massachusetts) served as the registry coordinating center, and the Duke Clinical Research Institute (Durham, North Carolina) was the data analysis center. Institutional review board approval was granted to analyze the aggregate, deidentified data.
Patients
We included all 121 990 index HF hospitalizations in the GWTG-HF registry between January 1, 2005, and December 31, 2014, of patients 65 years and older linked with US Centers for Medicare and Medicaid inpatient claims eligible for Part A and B fee-for-service during the discharge month.7 If a patient had multiple hospitalizations, the first HF hospitalization identified during the study period was used as the index HF hospitalization. Medicare files included all fee-for-service Medicare beneficiaries with follow-up through the end of December 2015. We excluded 8330 patients with missing discharge disposition, who died in-hospital, who transferred to another short-term hospital, who left against medical advice, and/or with missing socioeconomic information.
Patients were listed as being discharged to home hospice care (n = 2424) or to a medical hospice facility (n = 2164). We compared these patients with 4357 patients with advanced HF (ejection fraction ≤25% and any of the following: inpatient inotrope use, serum sodium level ≤130 mEq/L, blood urea nitrogen level ≥45 mg/dL [to convert to micromoles per liter, multiply by 0.357], systolic blood pressure ≤90 mm Hg, or comfort measures during hospitalization) not discharged to hospice and 113 045 other patients with HF in the GWTG-HF registry.
Outcomes
The primary outcomes of interest were all-cause mortality, all-cause readmission, and a composite of mortality/readmission at 30 days, 6 months, and 1 year after index discharge. All-cause mortality was determined based on death dates in the Medicare denominator files, and readmissions were defined as any new nonelective inpatient claim (excluding the index hospitalization claim), transfers to or from another hospital, and admissions for rehabilitation.
Secondary outcomes/end points that we analyzed included demographic, biologic, hospital, and sociological factors, and we assessed if they were associated with discharge to hospice. We assessed the outcomes of patients admitted to the hospital by final disposition, eg, death, discharge to hospice, or discharge without hospice plan. Left ventricular assist device placement or heart transplantation was assessed by International Classification of Diseases, Ninth Revision and International Statistical Classification of Diseases and Related Health Problems, Tenth Revision procedure codes. When assessing trends in hospice discharges, hospital characteristics were excluded given differences in hospital characteristics that enrolled earlier in the GWTG-HF registry. Symptom severity at discharge was assessed using review of patient clinical documentation at discharge.
Statistical Analysis
Patient demographic characteristics, medical history, admission data, and hospital characteristics were collected for patients with HF discharged to hospice, patients with advanced HF, and other patients with HF in the GWTG-HF registry. Proportions and medians with interquartile ranges (IQRs) are reported for categorical and continuous variables, respectively. The Pearson χ2 test was used to compare binary or nominal categorical variables, and Kruskal-Wallis tests were used to compare continuous or ordinal categorical variables. Percent standardized differences (standardized differences × 100) were calculated.
Cumulative incidences were described for all follow-up outcomes in all patient groups. Cumulative incidence for readmission outcomes accounted for the competing risk of mortality. Log-rank test was used to assess the difference in mortality. Gray test was used to assess differences in readmission outcomes. We examined the unadjusted and adjusted associations of follow-up outcomes with patient groups using Cox proportional hazards models on the subdistribution hazards. Fine and Gray methods account for the competing risks of deaths. Robust sandwich variance estimators were used in the model to account for correlation among patients from the same hospital. The following covariates were used for adjustment in this analysis: demographic characteristics (age, sex, and race/ethnicity), medical history (anemia, ischemic etiology, cerebrovascular accident/transient ischemic attack, diabetes, hyperlipidemia, hypertension, chronic obstructive pulmonary disease or asthma, peripheral vascular disease, renal insufficiency, and smoking) examination and laboratory findings (left ventricular ejection fraction, heart rate, systolic blood pressure, body mass index, serum creatinine level, serum sodium level, and blood urea nitrogen level), hospital characteristics (geographic region, teaching status, number of beds, and rural location), and other factors (year and quarter of index admission, median home value, median household income, high school education, and college education). We repeated this analysis comparing patients discharged to home hospice vs a hospice facility. When identifying factors associated with higher risk of readmission in patients discharged to hospice, we reported hazard ratio (HR) estimates and P values for each covariate from the adjusted model on all-cause readmission. We used the Cochran-Armitage trend test to analyze trend in hospice rate in patients with HF by year.
Medical history missing was imputed to no. For all other covariates with missingness, multiple imputation with 25 imputed data sets was used. All P values were 2-tailed, and a P value less than .05 was considered statistically significant. All analyses were performed using SAS software version 9.4 (SAS Institute).
Results
Study Cohort
The initial population of patients hospitalized with HF who were discharged alive between January 1, 2005, and December 31, 2014, was 391 977 patients from 477 sites. Of these, 121 990 patients (31.1%) from 438 sites (91.8%) were included in the analysis (eFigure in the Supplement).
Baseline Characteristics
Overall
Of the study cohort, 4588 (3.8%) were discharged to hospice, 4357 (3.6%) had advanced HF, and 113 045 (92.7%) were other patients with HF in the GWTG-HF registry (Table 1). Missing rates of key variables are provided in eTable 1 in the Supplement. Patients discharged to hospice were older, were more likely to be white, had higher education, and had worse HF severity than patients with advanced HF or other patients in the GWTG-HF registry. Patients discharged to hospice had a higher prevalence of atrial fibrillation, chronic obstructive pulmonary disease, cerebrovascular accident/transient ischemic attack, anemia, depression, and valvular heart disease and a lower prevalence of diabetes, hyperlipidemia, chronic dialysis use, and smoking than patients with advanced HF and other patients in the GWTG-HF registry. At discharge, patients in hospice were much more likely to have worse or unchanged symptoms compared with patients with advanced HF or other patients in the GWTG-HF registry (737 [35.2%] vs 72 [2.2%] vs 577 [1.1%]).
Table 1. Characteristics of Patients With Heart Failure (HF) Discharged to Hospice, Patients With Advanced HF, and Other Patients With HF in the Get With The Guidelines–HF Registry.
| Variable | % | P Value | ||
|---|---|---|---|---|
| Hospice (n = 4588) | Advanced HF (n = 4357)a | Other HF (n = 113 045) | ||
| Demographic Characteristics | ||||
| Age, median (IQR), y | 86 (80-90) | 78 (72-84) | 81 (74-87) | <.001 |
| Female | 2555 (55.7) | 1458 (33.5) | 62 404 (55.2) | <.001 |
| Race | <.001 | |||
| White | 3957 (88.1) | 3414 (79.7) | 90 541 (81.8) | |
| Black | 263 (5.9) | 493 (11.5) | 10 785 (9.7) | |
| Hispanic (any race) | 137 (3.1) | 193 (4.5) | 4941 (4.5) | |
| Asian | 44 (1.0) | 60 (1.4) | 1419 (1.3) | |
| Other (includes UTD) | 88 (2.0) | 123 (2.9) | 3032 (2.7) | |
| Insurance | <.001 | |||
| No insurance/ND/UTD | 10 (0.3) | 10 (0.3) | 304 (0.3) | |
| Medicare | 2756 (76.3) | 2914 (73.3) | 70 374 (75.9) | |
| Medicaid | 161 (4.5) | 204 (5.1) | 5258 (5.7) | |
| Other | 684 (18.9) | 848 (21.3) | 16 750 (18.1) | |
| Median household income, median (IQR), × $1000 in 2015 US $ | 51.4 (45.4-60.7) | 51.2 (44.6-60.7) | 51.9 (45.6-60.8) | .002 |
| High school degree, median (IQR), % | 88.1 (85.0-90.8) | 87.3 (83.5–90.0) | 87.4 (83.9-90.4) | <.001 |
| Unemployment rate, median (IQR), % | 7.0 (5.8-8.2) | 7.1 (5.9-8.6) | 7.1 (5.9-8.3) | .001 |
| EF, median (IQR), % | 40 (25-56) | 20 (15-25) | 49 (33-60) | <.001 |
| Medical History | ||||
| Atrial flutter/fibrillation | 1974 (46.0) | 1739 (41.0) | 43 627 (41.6) | <.001 |
| COPD or asthma | 1311 (30.5) | 1140 (26.9) | 30 665 (29.2) | .001 |
| Diabetes | 1420 (33.1) | 1806 (42.6) | 41 284 (39.3) | <.001 |
| Hyperlipidemia | 1865 (43.5) | 2102 (49.5) | 52 131 (49.7) | <.001 |
| Hypertension | 3136 (73.1) | 2915 (68.7) | 82 124 (78.3) | <.001 |
| Peripheral vascular disease | 586 (13.7) | 661 (15.6) | 13 620 (13.0) | <.001 |
| CAD | 2184 (50.9) | 2569 (60.5) | 53 357 (50.8) | <.001 |
| Prior MI | 815 (19.0) | 1132 (26.7) | 18 768 (17.9) | <.001 |
| CVA/TIA | 797 (18.6) | 633 (14.9) | 17 292 (16.5) | <.001 |
| ICD only | 308 (7.2) | 988 (23.3) | 6473 (6.2) | <.001 |
| HF | 2916 (67.9) | 2841 (67.0) | 61 598 (58.7) | <.001 |
| Anemia | 1074 (25.0) | 810 (19.1) | 20 544 (19.6) | <.001 |
| Pacemaker | 682 (15.9) | 775 (18.3) | 15 778 (15.0) | <.001 |
| Dialysis, chronic | 75 (1.7) | 130 (3.1) | 3163 (3.0) | <.001 |
| Renal insufficiency, chronic (serum creatinine level >2.0 mg/dL) | 1209 (28.2) | 1350 (31.8) | 20 948 (20.0) | <.001 |
| Depression | 545 (12.7) | 383 (9.0) | 11 304 (10.8) | <.001 |
| Valvular heart disease | 1042 (24.3) | 806 (19.0) | 17 485 (16.7) | <.001 |
| Smoking | 230 (5.4) | 409 (9.4) | 9587 (8.6) | <.001 |
| Symptoms | ||||
| Admission symptoms | ||||
| Chest pain | 227 (10.9) | 443 (13.4) | 9085 (16.2) | <.001 |
| Decreased appetite/early satiety | 186 (8.9) | 240 (7.2) | 2187 (3.9) | <.001 |
| Dizziness/lightheadedness/syncope | 125 (6.0) | 234 (7.1) | 3268 (5.8) | .01 |
| Dyspnea at rest | 1135 (54.6) | 1535 (46.3) | 26 935 (47.9) | <.001 |
| Dyspnea on exertion | 1169 (56.2) | 2179 (65.8) | 34 928 (62.2) | <.001 |
| Fatigue | 534 (25.7) | 920 (27.8) | 11 219 (20.0) | <.001 |
| Orthopnea | 411 (19.8) | 901 (27.2) | 13 130 (23.4) | <.001 |
| PND | 164 (7.9) | 404 (12.2) | 5337 (9.5) | <.001 |
| Admission symptoms missing | 2508 (54.7) | 1045 (24.0) | 56 860 (50.3) | <.001 |
| Discharge symptoms | <.001 | |||
| Unable to determine | 256 (12.2) | 286 (8.7) | 4630 (8.4) | |
| Better, asymptomatic | 277 (13.2) | 1467 (44.9) | 27 612 (50.4) | |
| Better, symptomatic | 822 (39.3) | 1444 (44.2) | 21 991 (40.1) | |
| Unchanged | 365 (17.4) | 60 (1.8) | 481 (0.9) | |
| Worse | 372 (17.8) | 12 (0.4) | 96 (0.2) | |
| No parental therapy | 651 (20.9) | 1062 (26.6) | 27 179 (34.2) | <.001 |
| No in-hospital procedures | 2560 (88.6) | 2577 (66.9) | 59 575 (79.3) | <.001 |
| Advanced care | ||||
| Advanced care plan/surrogate decision maker | 1657 (75.6) | 785 (61.5) | 29 353 (66.0) | <.001 |
| Advance directive executed | 106 (71.1) | 139 (40.6) | 4919 (40.1) | <.001 |
| HF reporting: advanced care plan | 2373 (51.7) | 1532 (35.2) | 51 101 (45.2) | <.001 |
| Hospital characteristics | ||||
| Rural location | 215 (4.8) | 246 (6.0) | 6288 (5.9) | .01 |
| Teaching status | 3117 (69.3) | 3166 (73.8) | 78 314 (70.6) | <.001 |
| Heart transplant hospital | 325 (9.8) | 449 (16.1) | 7153 (9.6) | <.001 |
Abbreviations: CAD, coronary artery disease; COPD, chronic obstructive pulmonary disease; CVA/TIA, cerebrovascular accident/transient ischemic attack; EF, ejection fraction; ICD, implantable cardioverter defibrillator; IQR, interquartile range; MI, myocardial infarction; ND, not determined; PND; paroxysmal nocturnal dyspnea; UTD, unable to determine.
Patients with advanced HF were defined as ejection fraction of 25% or less and any of the following: inpatient inotrope use, serum sodium level of 130 mEq/L or less, blood urea nitrogen level of 45 mg/dL or more [to convert to micromoles per liter, multiply by 0.357], systolic blood pressure of 90 mm Hg or less, or comfort measures during hospitalization.
Overall, there were 6350 patients (5.2%) in our study cohort who received comfort measures only at any point during the hospitalization and survived to discharge, 3192 (50.3%) of whom were discharged to hospice. Most of the 4588 patients discharged to hospice received comfort measures (n = 3192 [69.6%]), followed by patients with advanced HF (n = 578 [13.3%]) and other patients in the GWTG-HF registry (n = 2580 [2.3%]). The median (IQR) length of stay for both patients discharged to hospice and patients with advanced HF was 6 (3-9) days and for other patients in the GWTG-HF registry was 4 (3-6) days. Patients discharged to hospice were much less likely to be discharged with prescriptions for HF and cardiovascular medications than other groups, although a substantial proportion were discharged with prescriptions for medications unlikely to provide them symptomatic benefit, such as aspirin (501 [38.8%]) and lipid-lowering therapies (328 [27.1%]) (eTable 2 in the Supplement).
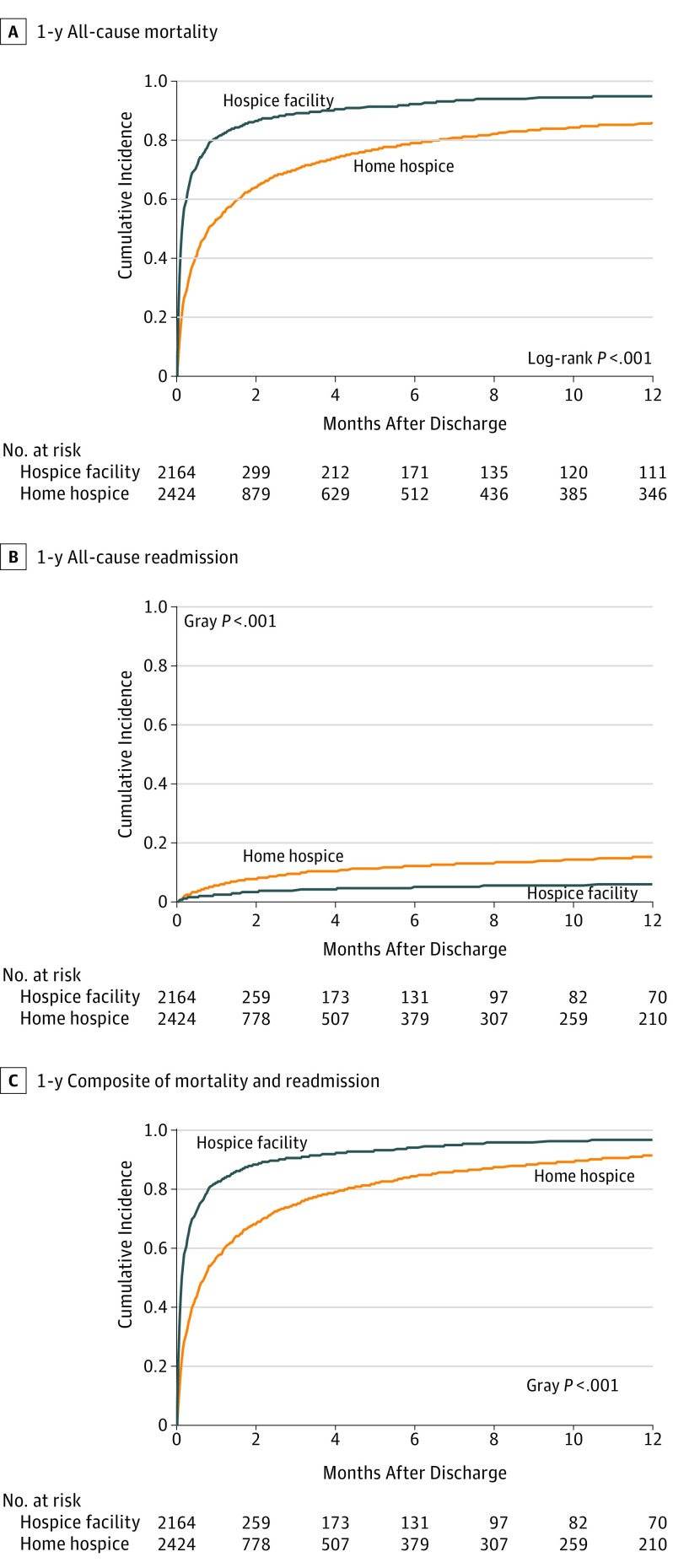
Home Hospice vs Hospice Facility
Of patients discharged to hospice, 2424 (52.8%) were discharged to home hospice and 2164 (47.2%) were discharged to a hospice facility. Compared with patients discharged to home hospice, patients discharged to hospice facilities were more likely to be older (median [IQR] age, 87 [81-91] years vs 85 [79-90] years), female (1263 [58.4%] vs 1292 [53.3%]), white (1906 [89.7%] vs 2051 [86.7%]), college educated (median [IQR], 28.8% [23.2%-34.0%] vs 27.4% [19.8%-33.4%]), have higher median (IQR) home value in 2015 US dollars ($163 500 [131 900-240 100] vs $161 300 [124 500-232 500]), have HF with preserved ejection fraction (924 [46.7%] vs 873 [39.3%]), and have worse or unchanged symptoms at discharge (462 [47.0%] vs 275 [24.8%]) and were less likely to be discharged from a rural (67 [3.2%] vs 148 [6.3%]) or teaching (1435 [67.5%] vs 1682 [71.0%]) hospital (eTable 3 in the Supplement).
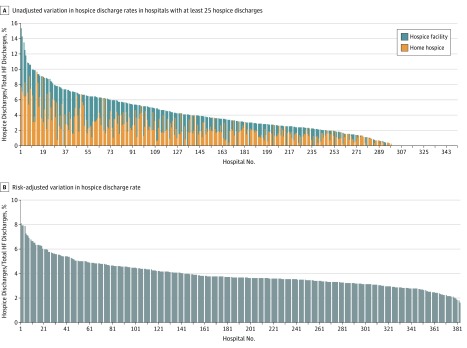
Trends and Hospital-Level Variation in Hospice Discharge Rate
The hospice discharge rate in our study population increased from 2.0% (109 of 5528) in 2005 to 4.9% (968 of 19 590) in 2014 (P value for trend < .001) (eTable 4 in the Supplement). Significant hospital-level variation in hospice discharge rate was noted. The median (IQR) hospice discharge rate among all sites was 3.0% (0.7%-5.5%) and among sites with at least 25 patients in the study population was 3.5% (2.0%-5.7%) (Figure 1A). After risk adjustment, the median (IQR) hospice discharge rate was 3.6% (3.2%-4.5%) (Figure 1B). Patients discharged to hospice were more likely to receive care in hospitals in the western and southern regions and less likely to be in the northeast region and in rural and teaching hospitals (Table 1). Patients with HF discharged to hospice in 2012 to 2014 (n = 2607) compared with patients discharged in 2009 to 2011 (n = 1282) and 2005 to 2008 (n = 699) were older (86 years vs 85 years vs 85 years), more likely to have a high school degree (89.0% vs 87.4% vs 85.3%), HF with preserved ejection fraction (1060 [44.1%] vs 486 [41.3%] vs 251 [40.4%]), and greater burden of comorbidities (eTable 5 in the Supplement).
Figure 1. Variation in Hospice Discharge Rate Among Hospitals.
A, Hospice discharge rates from sites with 25 or more hospice discharges were included, leaving 350 sites and 120 923 patients. B, Only sites missing hospital characteristic data were excluded, leaving 383 sites and 111 584 patients.
Outcomes
All-Cause Mortality and Survival in Hospice
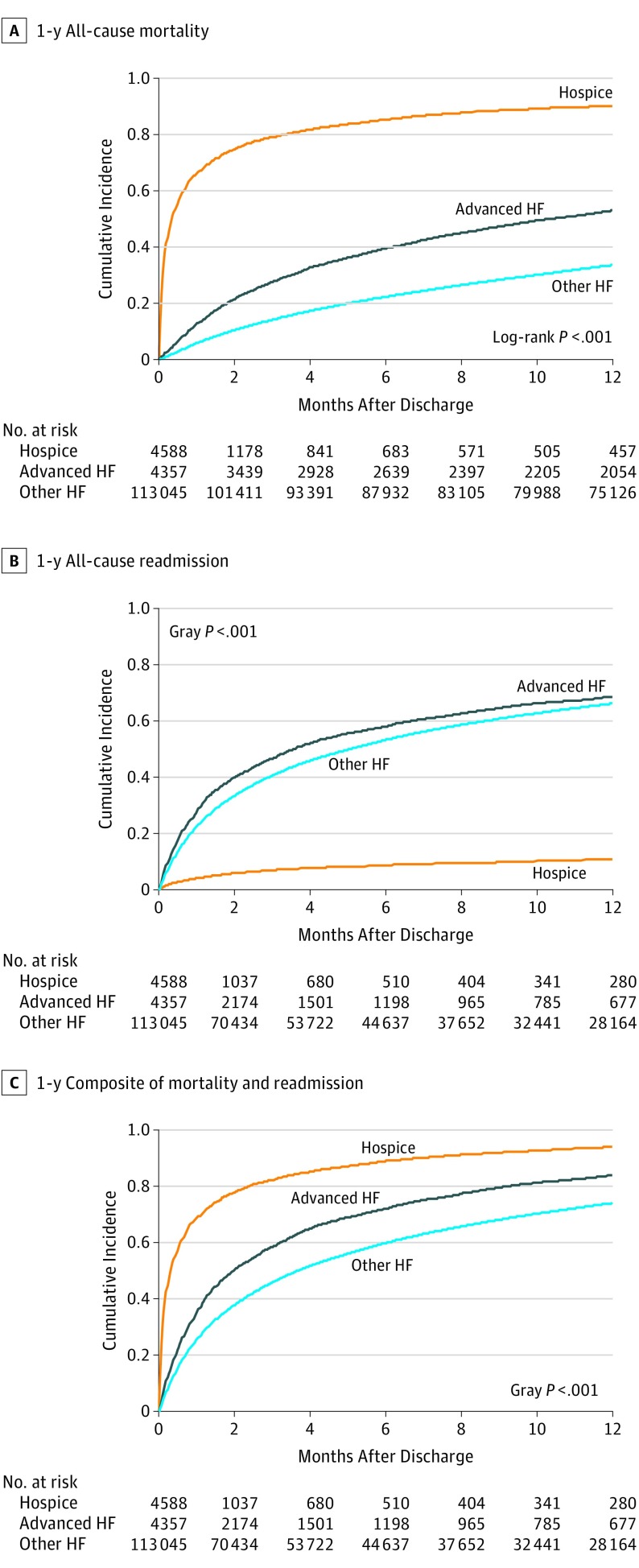
Patients discharged to hospice had higher cumulative incidences of all-cause mortality at 30 days (3026 [66.0%]), 6 months (3901 [85.0%]) and 1 year (4132 [90.1%]) compared with patients with advanced HF (549 [12.6%] at 30 days, 1715 [39.4%] at 6 months, and 2305 [52.9%] at 1 year) and other HF patients (6614 [5.9%] at 30 days, 25 035 [22.1%] at 6 months, and 37 977 [33.6%] at 1 year) (Table 2; Figure 2A). The median (IQR) survival for patients discharged to hospice was 11 (3-63) days compared with 318 (78-1095) days for patients with advanced HF and 754 (221-1784) days for other patients in the GWTG-HF registry. The median (IQR) survival time among patients discharged to hospice facilities was 5 (2-20) days and among patients discharged to home hospice was 25 (6-132) days. Overall, 1034 patients (22.5%) discharged to hospice died in less than 3 days, while 739 (34.1%) discharged to a hospice facility died in less than 3 days. Only 690 patients (15.0%) discharged to hospice lived for 6 months or more. Median survival times in hospice did not change between 2005 and 2014 (eTables 6 and 7 in the Supplement).
Table 2. All-Cause Mortality, All-Cause Readmission, and Composite of Mortality and Readmission Outcomes in Patients With Heart Failure.
| Outcome | Cumulative Incidence | Comparison Groups | Unadjusted Analysis | Adjusted Analysis | |||
|---|---|---|---|---|---|---|---|
| No. (%) | P Valuea | HR (95% CI) | P Valueb | HR (95% CI) | P Valueb | ||
| 30 d | |||||||
| All-cause mortality | <.001 | <.001 | <.001 | ||||
| Hospice | 3026 (66.0) | Hospice vs hospice | 1.00 | NA | 1.00 | NA | |
| Advanced HF | 549 (12.6) | Hospice vs advanced HF | 9.21 (8.32-10.19) | <.001 | 8.63 (7.74-9.62) | <.001 | |
| Other HF | 6614 (5.9) | Hospice vs other HF | 20.48 (19.12-21.94) | <.001 | 13.34 (12.33-14.42) | <.001 | |
| All-cause readmission | <.001 | <.001 | <.001 | ||||
| Hospice | 189 (4.1) | Hospice vs hospice | 1.00 | NA | 1.00 | NA | |
| Advanced HF | 1185 (27.2) | Hospice vs advanced HF | 0.13 (0.11-0.16) | <.001 | 0.15 (0.13-0.18) | <.001 | |
| Other HF | 25 022 (22.2) | Hospice vs other HF | 0.17 (0.15-0.20) | <.001 | 0.15 (0.13-0.18) | <.001 | |
| Composite | <.001 | <.001 | <.001 | ||||
| Hospice | 3143 (68.5) | Hospice vs hospice | 1.00 | NA | 1.00 | NA | |
| Advanced HF | 1498 (34.4) | Hospice vs advanced HF | 3.17 (2.96-3.40) | <.001 | 3.46 (3.21-3.73) | <.001 | |
| Other HF | 28 450 (25.2) | Hospice vs other HF | 4.61 (4.35-4.89) | <.001 | 3.90 (3.66-4.15) | <.001 | |
| 6 mo | |||||||
| All-cause mortality | <.001 | <.001 | <.001 | ||||
| Hospice | 3901 (85.0) | Hospice vs hospice | 1.00 | NA | 1.00 | NA | |
| Advanced HF | 1715 (39.4) | Hospice vs advanced HF | 5.47 (5.06-5.92) | <.001 | 5.15 (4.74-5.59) | <.001 | |
| Other HF | 25 035 (22.2) | Hospice vs other HF | 10.97 (10.32-11.67) | <.001 | 7.10 (6.66-7.56) | <.001 | |
| All-cause readmission | <.001 | <.001 | <.001 | ||||
| Hospice | 401 (8.8) | Hospice vs hospice | 1.00 | NA | 1.00 | NA | |
| Advanced HF | 2498 (57.7) | Hospice vs advanced HF | 0.11 (0.09-0.12) | <.001 | 0.11 (0.10-0.13) | <.001 | |
| Other HF | 59 415 (53.0) | Hospice vs other HF | 0.12 (0.11-0.14) | <.001 | 0.11 (0.10-0.13) | <.001 | |
| Composite | <.001 | <.001 | <.001 | ||||
| Hospice | 4062 (88.7) | Hospice vs hospice | 1.00 | NA | 1.00 | NA | |
| Advanced HF | 3099 (71.6) | Hospice vs advanced HF | 2.33 (2.20-2.47) | <.001 | 2.47 (2.32-2.63) | <.001 | |
| Other HF | 66 724 (59.5) | Hospice vs other HF | 3.30 (3.13-3.48) | <.001 | 2.80 (2.65-2.96) | <.001 | |
| 1 y | |||||||
| All-cause mortality | <.001 | <.001 | <.001 | ||||
| Hospice | 4132 (90.1) | Hospice vs hospice | 1.00 | NA | 1.00 | NA | |
| Advanced HF | 2305 (52.9) | Hospice vs advanced HF | 4.91 (4.55-5.30) | <.001 | 4.60 (4.24-4.98) | <.001 | |
| Other HF | 37 977 (33.6) | Hospice vs other HF | 9.20 (8.64-9.80) | <.001 | 6.13 (5.76-6.53) | <.001 | |
| All-cause readmission | <.001 | <.001 | <.001 | ||||
| Hospice | 497 (10.9) | Hospice vs hospice | 1.00 | NA | 1.00 | NA | |
| Advanced HF | 2948 (68.4) | Hospice vs advanced HF | 0.10 (0.09-0.11) | <.001 | 0.10 (0.09-0.12) | <.001 | |
| Other HF | 73 804 (66.1) | Hospice vs other HF | 0.11 (0.10-0.12) | <.001 | 0.10 (0.09-0.11) | <.001 | |
| Composite | <.001 | <.001 | <.001 | ||||
| Hospice | 4291 (93.8) | Hospice vs hospice | 1.00 | NA | 1.00 | NA | |
| Advanced HF | 3606 (83.7) | Hospice vs advanced HF | 2.20 (2.07-2.33) | <.001 | 2.28 (2.13-2.43) | <.001 | |
| Other HF | 82 568 (74.0) | Hospice vs other HF | 3.06 (2.90-3.23) | <.001 | 2.61 (2.47-2.77) | <.001 | |
Abbreviations: HF, heart failure; HR, hazard ratio; NA, not applicable.
Log-rank P value is shown for mortality and Gray P value is shown for other outcomes.
The first P value has 3 df and tests if hazards of a given outcome is different in at least 1 pair of groups; other P values test whether hazards in given comparison groups are significantly different. The following covariates were used for adjustment in this analysis: demographic characteristics (age, sex, and race/ethnicity), medical history (anemia, ischemic etiology, cerebrovascular accident/transient ischemic attack, diabetes, hyperlipidemia, hypertension, chronic obstructive pulmonary disease or asthma, peripheral vascular disease, renal insufficiency, and smoking) examination and laboratory findings (left ventricular ejection fraction, heart rate, systolic blood pressure, body mass index, serum creatinine level, serum sodium level, and blood urea nitrogen level), hospital characteristics (geographic region, teaching status, number of beds, and rural location), and other factors (year and quarter of index admission, median home value, median household income, high school education, and college education).
Figure 2. Time-to-Event Comparisons Between Patients Discharged to Hospice, Patients With Advanced Heart Failure, and Other Patients With Heart Failure in the Get With The Guidelines–Heart Failure Registry.
Patients discharged to hospice within a week (n = 1991) compared with patients who died between 7 days and 1 year (n = 2141) and those surviving more than 1 year (n = 456) were more likely to be white (1754 [89.9%] vs 1835 [87.5%] vs 368 [83.3%]) and have atrial fibrillation (900 [48.3%] vs 901 [45.1%] vs 173 [40.1%]), peripheral vascular disease (285 [15.3%] vs 257 [12.9%] vs 44 [10.2%]), renal insufficiency (567 [30.4%] vs 562 [28.2%] vs 80 [18.6%]), lower systolic blood pressure (125 mm Hg vs 128 mm Hg vs 139 mm Hg), lower diastolic blood pressure (68 mm Hg vs 70 mm Hg vs 72 mm Hg), and unchanged to worsening symptoms at discharge (474 [52.4%] vs 239 [24.4%] vs 24 [11.5%]) and were less likely to be female (1070 [53.7%] vs 1195 [55.8%] vs 290 [63.6%]) and discharged on evidence-based HF therapies. They were also more likely to be discharged from an urban hospital (74 [3.8%] vs 110 [5.3%] vs 31 [6.9%]) and transplant-capable hospital (157 [11.1%] vs 140 [9.0%] vs 28 [8.3%]) (eTable 8 in the Supplement). At 1 year after discharge, 67 patients with advanced HF (1.5%) received a left ventricular assist device or heart transplantation compared with 132 other patients in the GWTG-HF registry (0.1%) and 1 patient discharged to hospice (0.02%) (eTable 9 in the Supplement).
All-Cause Readmission
Patients discharged to hospice had much lower cumulative incidences of all-cause readmission (189 [4.1%] at 30 days, 401 [8.7%] at 6 months, and 497 [10.8%] at 1 year) compared with both patients with advanced HF (1185 [27.2%] at 30 days, 2498 [57.3%] at 6 months, and 2948 [67.7%] at 1 year) and other patients in the GWTG-HF registry (25 022 [22.1%] at 30 days, 59 415 [52.6%] at 6 months, and 73 804 [65.3%] at 1 year) (Figure 2B). Patients discharged to hospice also had greater hazards of the composite outcome of all-cause mortality and all-cause readmission in both adjusted and unadjusted analyses compared with patients with advanced HF and other patients in the GWTG-HF registry (Figure 2C). Lastly, patients discharged to home hospice had lower cumulative incidence and hazards of mortality, higher incidence and hazards of readmission, and lower incidence of the composite end point of all-cause mortality and readmission compared with patients discharged to hospice facilities (Figure 3) (eTable 10 in the Supplement).
Figure 3. Time-to-Event Comparisons Between Patients Discharged to Home Hospice and a Hospice Facility.
Characteristics of Patients Readmitted From Hospice
Patients discharged to hospice who were readmitted (497 of 4588) compared with patients with advanced HF (2948 of 4357) and other patients in the GWTG-HF registry (73 804 of 113 045) were older (median [IQR] age, 84 [76-89] years vs 78 [71-83.5] years and 81 [74-87] years), were less likely to have a primary cardiovascular diagnosis (216 [43.5%] vs 1693 [57.4%] vs 35 702 [48.4%]) or have a cardiovascular procedure performed (67 [13.5%] vs 767 [26.0%] vs 16 637 [22.6%]), and were more likely to die during the readmission (59 [12.1%] vs 266 [9.1%] vs 4428 [6.1%]) or discharged back to hospice (131 [26.8%] vs 180 [6.2%] vs 2812 [3.9%]) (eTable 11 in the Supplement). Patients discharged to hospice and readmitted from home hospice were younger than patients readmitted from hospice facilities (median [IQR] age, 83 [75-88] years vs 86 [80-91] years), but no significant differences were noted in other characteristics (eTable 12 in the Supplement). Rates of readmission from hospice did not change through the course of the study (eTable 13 in the Supplement). Factors associated with readmission from hospice were nonwhite race (adjusted HR, 1.59; 95% CI, 1.18-2.17), younger age (adjusted HR per 5 years, 1.18; 95% CI, 1.10-1.27), heart rate (adjusted HR per 5 beats per minute, 0.97; 95% CI, 0.95-1.00), systolic blood pressure (adjusted HR per 5 mm Hg, 1.03; 95% CI, 1.02-1.05), and blood urea nitrogen level (adjusted HR per 5 mg/dL, 0.97; 95% CI, 0.94-1.00) (eTable 14 in the Supplement).
Discussion
This study provides an overview of trends and patterns in hospice use for patients with HF in the United States. Only 4.9% of Medicare patients hospitalized with HF were discharged to hospice, and there was significant hospital-level variation in hospice discharge rates. More than one-third of patients were discharged to hospice with unchanged or worsening symptoms compared with only 1% to 2% of other patients in the GWTG-HF registry. The median survival time in hospice was only 11 days, and nearly one-quarter of patients discharged to hospice died less than 3 days of discharge. The median survival time of patients discharged to hospice facilities was even shorter at 5 days. Black race and younger age were the strongest predictors of readmission from hospice. These findings highlight significant areas for potential improvement in the quality of end-of-life care received by patients with HF.
Our study confirms the poor overall survival of older adults discharged after an HF hospitalization.1 A 2012 report8 from GWTG-HF reported on hospice discharges between 2005 and 2010. However, that analysis did not report patient survival, differentiate hospice site, or provide rates or predictors of readmission. A 2017 report9 assessed hospice use in Medicare beneficiaries receiving home health care from 2009 to 2010. This study found a longer median survival in hospice of 15 days. Finally, a study of Medicare beneficiaries in Alabama between 1998 and 200110 showed that very few patients (182 [2%]) had received hospice care.
Randomized trials have shown that patients with HF have better quality of life when receiving palliative care.11,12,13 However, there are limited metrics for assessing quality of care at end of life. One metric, short survival in hospice, has been proposed.14 However, a downtrend in survival in hospice has been noted nationally, driven by the increase in patients with noncancer diagnoses enrolling in hospice.15 Further, diseases such as HF are difficult to prognosticate, and therefore, many patients might be receiving hospice referrals very late in the trajectory of disease.16 This might be one important reason why patients with heart disease continue to be grossly underrepresented in the hospice-enrolled population in the United States compared with patients with other diseases, such as cancer.4 Therefore, early recognition of poor prognosis and palliative consultation could facilitate timely hospice referral.17 In our study, 15% of patients survived more than 6 months, similar to rates for other diseases.18,19 However, about 1 in 10 patients in our study discharged to hospice survived for more than 1 year. It would also be useful to develop tools to predict patients who experience such long survival in hospice.
Disenrollment from hospice is another potential metric of suboptimal end-of-life care.20 Younger age and black race were the most significant predictors of hospital readmission after adjustment for other variables. Disparities in palliative care use have been extensively noted among black patients.21 Furthermore, we found significant variation between hospitals in hospice discharge rate in our study. This finding warrants further investigation to identify factors driving high and low hospice discharge rates in hospitals.
Our study found important differences in patients discharged to home hospice vs those discharged to hospice facilities. Patients discharged to hospice facilities had much shorter survival than patients discharged to home hospice. This suggests that patients discharged to hospice facilities might be sicker. However, patients discharged to hospice facilities had higher income than patients discharged home. Hospice facilities have additional out-of-pocket costs, which might restrict access.
Limitations
Our study has several limitations. We only looked at index hospitalizations to simplify our look at subsequent outcomes, including readmission. Given the observational nature of this study, we cannot make inferences regarding causality when examining outcomes. The GWTG-HF registry is dependent on voluntary participation; thus, there is the potential for selection biases. However, Medicare beneficiaries in the registry have been shown in prior studies to be representative of the overall US Medicare population.22 Finally, 13% of patients with advanced HF and 2% of other patients with HF received comfort measures only during the hospitalization. However, the aim of this study was to better define patterns of hospice use at the end of life for patients with HF. Lastly, GWTG did not gather information about type of hospice care, categorized into routine home care, continuous home care (which can also be provided in a facility), general inpatient care, and inpatient respite care.
Conclusions
In conclusion, hospice care is increasing gradually among patients hospitalized with HF. Once discharged to hospice, few patients are readmitted to the hospital, and most die within 2 weeks of hospice referral. As there is wide hospital-level variation in hospice referral, clinicians may benefit from having access to better tools to assess prognosis in HF such that timely referrals to palliative care and hospice could be made. Better management of symptoms might also lead to improvement in transition to hospice. These findings can inform clinical care, future research, and policy interventions to improve the care patients with HF receive at the end of life.
eFigure. Study population.
eTable 1. Variable missing rates in overall study population.
eTable 2. Admission and discharge therapies of heart failure patients discharged to hospice.
eTable 3. Characteristics of patients discharged to hospice: home vs health care facility.
eTable 4. Trend of hospice rate in study population (121 990 patients from 438 sites).
eTable 5. Characteristics of heart failure patients discharged to hospice over time.
eTable 6. Survival times in heart failure patients.
eTable 7. Trends in observed median survival in hospice.
eTable 8. Characteristics of patients discharged to hospice who survived <7 days, 7 days-1 year, and >1 year.
eTable 9. Left ventricular assist device implantation or heart transplantation at 1 year after index heart failure discharge.
eTable 10. Mortality, readmission, and composite outcomes in heart failure patients discharged to hospice by hospice destination.
eTable 11. Hospital course of patients’ first readmission within 1 year post index heart failure discharge.
eTable 12. Hospital course of patients’ first readmission within 1 year post discharge by hospice destination at index heart failure discharge.
eTable 13. One-year cumulative incidence rate for readmission from hospice by year (4588 patients from 337 sites).
eTable 14. Factors associated with 1-year all-cause readmissions in heart failure patients readmitted from hospice.
References
- 1.Shah KS, Xu H, Matsouaka RA, et al. . Heart failure with preserved, borderline, and reduced ejection fraction: 5-year outcomes. J Am Coll Cardiol. 2017;70(20):2476-2486. doi: 10.1016/j.jacc.2017.08.074 [DOI] [PubMed] [Google Scholar]
- 2.Gupta A, Allen LA, Bhatt DL, et al. . Association of the hospital readmissions reduction program implementation with readmission and mortality outcomes in heart failure. JAMA Cardiol. 2018;3(1):44-53. doi: 10.1001/jamacardio.2017.4265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Worldwide Palliative Care Alliance Global atlas of palliative care at the end of life. http://www.who.int/nmh/Global_Atlas_of_Palliative_Care.pdf. Accessed June 18, 2018.
- 4.Warraich HJ, Hernandez AF, Allen LA. How medicine has changed the end of life for patients with cardiovascular disease. J Am Coll Cardiol. 2017;70(10):1276-1289. doi: 10.1016/j.jacc.2017.07.735 [DOI] [PubMed] [Google Scholar]
- 5.Mandawat A, Heidenreich PA, Mandawat A, Bhatt DL. Trends in palliative care use in veterans with severe heart failure using a large national cohort. JAMA Cardiol. 2016;1(5):617-619. doi: 10.1001/jamacardio.2016.1687 [DOI] [PubMed] [Google Scholar]
- 6.Smaha LA; American Heart Association . The American Heart Association Get With The Guidelines program. Am Heart J. 2004;148(5, suppl):S46-S48. doi: 10.1016/j.ahj.2004.09.015 [DOI] [PubMed] [Google Scholar]
- 7.Hammill BG, Hernandez AF, Peterson ED, Fonarow GC, Schulman KA, Curtis LH. Linking inpatient clinical registry data to Medicare claims data using indirect identifiers. Am Heart J. 2009;157(6):995-1000. doi: 10.1016/j.ahj.2009.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Whellan DJ, Cox M, Hernandez AF, et al. . Utilization of hospice and predicted mortality risk among older patients hospitalized with heart failure: findings from GWTG-HF. J Card Fail. 2012;18(6):471-477. doi: 10.1016/j.cardfail.2012.02.006 [DOI] [PubMed] [Google Scholar]
- 9.Yim CK, Barrón Y, Moore S, et al. . Hospice enrollment in patients with advanced heart failure decreases acute medical service utilization. Circ Heart Fail. 2017;10(3):e003335. doi: 10.1161/CIRCHEARTFAILURE.116.003335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kheirbek RE, Fletcher RD, Bakitas MA, et al. . Discharge hospice referral and lower 30-day all-cause readmission in Medicare beneficiaries hospitalized for heart failure. Circ Heart Fail. 2015;8(4):733-740. doi: 10.1161/CIRCHEARTFAILURE.115.002153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rogers JG, Patel CB, Mentz RJ, et al. . Palliative care in heart failure: the PAL-HF randomized, controlled clinical trial. J Am Coll Cardiol. 2017;70(3):331-341. doi: 10.1016/j.jacc.2017.05.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sidebottom AC, Jorgenson A, Richards H, Kirven J, Sillah A. Inpatient palliative care for patients with acute heart failure: outcomes from a randomized trial. J Palliat Med. 2015;18(2):134-142. doi: 10.1089/jpm.2014.0192 [DOI] [PubMed] [Google Scholar]
- 13.Brännström M, Boman K. Effects of person-centred and integrated chronic heart failure and palliative home care: PREFER: a randomized controlled study. Eur J Heart Fail. 2014;16(10):1142-1151. doi: 10.1002/ejhf.151 [DOI] [PubMed] [Google Scholar]
- 14.Austin BJ, Fleisher LK Financing end-of-life care: challenges for an aging population. http://www.hcfo.org/files/hcfo/eolcare.pdf. Accessed June 18, 2018.
- 15.Aldridge MD, Canavan M, Cherlin E, Bradley EH. Has hospice use changed? 2000-2010 utilization patterns. Med Care. 2015;53(1):95-101. doi: 10.1097/MLR.0000000000000256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Warraich HJ, Allen LA, Mukamal KJ, Ship A, Kociol RD. Accuracy of physician prognosis in heart failure and lung cancer: comparison between physician estimates and model predicted survival. Palliat Med. 2016;30(7):684-689. doi: 10.1177/0269216315626048 [DOI] [PubMed] [Google Scholar]
- 17.Wang SY, Aldridge MD, Gross CP, Canavan M, Cherlin E, Bradley E. End-of-Life care transition patterns of Medicare beneficiaries. J Am Geriatr Soc. 2017;65(7):1406-1413. doi: 10.1111/jgs.14891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Harris PS, Stalam T, Ache KA, et al. . Can hospices predict which patients will die within six months? J Palliat Med. 2014;17(8):894-898. doi: 10.1089/jpm.2013.0631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rothenberg LR, Doberman D, Simon LE, Gryczynski J, Cordts G. Patients surviving six months in hospice care: who are they? J Palliat Med. 2014;17(8):899-905. doi: 10.1089/jpm.2013.0512 [DOI] [PubMed] [Google Scholar]
- 20.Pathak EB, Wieten S, Djulbegovic B. From hospice to hospital: short-term follow-up study of hospice patient outcomes in a US acute care hospital surveillance system. BMJ Open. 2014;4(7):e005196. doi: 10.1136/bmjopen-2014-005196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schonwetter RS, Clark LD, Leedy SA, Quinn MJ, Azer M, Kim S. Predicting emergency room visits and hospitalizations among hospice patients with cardiac disease. J Palliat Med. 2008;11(8):1142-1150. doi: 10.1089/jpm.2008.0032 [DOI] [PubMed] [Google Scholar]
- 22.Reeves MJ, Fonarow GC, Smith EE, et al. . Representativeness of the Get With The Guidelines-Stroke Registry: comparison of patient and hospital characteristics among Medicare beneficiaries hospitalized with ischemic stroke. Stroke. 2012;43(1):44-49. doi: 10.1161/STROKEAHA.111.626978 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure. Study population.
eTable 1. Variable missing rates in overall study population.
eTable 2. Admission and discharge therapies of heart failure patients discharged to hospice.
eTable 3. Characteristics of patients discharged to hospice: home vs health care facility.
eTable 4. Trend of hospice rate in study population (121 990 patients from 438 sites).
eTable 5. Characteristics of heart failure patients discharged to hospice over time.
eTable 6. Survival times in heart failure patients.
eTable 7. Trends in observed median survival in hospice.
eTable 8. Characteristics of patients discharged to hospice who survived <7 days, 7 days-1 year, and >1 year.
eTable 9. Left ventricular assist device implantation or heart transplantation at 1 year after index heart failure discharge.
eTable 10. Mortality, readmission, and composite outcomes in heart failure patients discharged to hospice by hospice destination.
eTable 11. Hospital course of patients’ first readmission within 1 year post index heart failure discharge.
eTable 12. Hospital course of patients’ first readmission within 1 year post discharge by hospice destination at index heart failure discharge.
eTable 13. One-year cumulative incidence rate for readmission from hospice by year (4588 patients from 337 sites).
eTable 14. Factors associated with 1-year all-cause readmissions in heart failure patients readmitted from hospice.