This case series study assesses a statistical prediction algorithm with the aim of efficiently diagnosing and treating patients with dizziness.
Key Points
Question
What is the clinical effectiveness of the linear predictor model calculated from a statistical algorithm for diagnosing benign paroxysmal positional vertigo in an outpatient, clinical setting?
Findings
In this case series study, 106 of 200 patient visits had the required information to calculate the linear predictor value. Patients with benign paroxysmal positional vertigo had a significantly different linear predictor result compared with those with all other vestibular disorders.
Meaning
The statistical algorithm may serve as a useful tool in the diagnosis of benign paroxysmal positional vertigo as a source of dizziness in the outpatient, clinical setting.
Abstract
Importance
Benign paroxysmal positional vertigo (BPPV) is an otologic pathologic condition defined as a sensation of spinning triggered by changes in head position relative to gravity and caused by an entrapment of fragmented endolymph debris most commonly in the posterior semicircular canal. Confirmation of diagnosis requires experience with procedures that are poorly known by those other than practitioners with advanced otologic training. The complexity in the diagnosis of BPPV inspired the design of a questionnaire-based algorithm that would be useful for determining a vestibular diagnosis and treatment options.
Objective
To assess a statistical algorithm for the diagnosis of BPPV in a busy tertiary care setting, with the long-term goal of implementing a clinical pathway to efficiently diagnose and treat patients with dizziness.
Design, Setting, and Participants
In this retrospective case series, 200 patients who visited the Department of Otolaryngology–Head and Neck Surgery at Johns Hopkins University School of Medicine for their initial vertigo symptoms from September 1, 2016, to December 31, 2016, were assessed.
Interventions
Use of a validated patient questionnaire as a tool to differentiate patients with dizziness in an electronic medical record review.
Main Outcomes and Measures
Linear predictor (LP) value based on the questionnaire for the diagnosis of BPPV.
Results
Of the 200 patient visits reviewed (132 [66%] female), 106 (53.0%; 68 [64%] female) had the information necessary to calculate the LP value and had a confirmed final diagnosis. On the basis of an LP value of 0.2 or greater, the sensitivity for a diagnosis of BPPV was 0.75 and the specificity was 1.0. The positive predictive value was 1.0, whereas the negative predictive value was 0.96. Patients with BPPV had a statistically significantly different LP value (odds ratio, 5.92; 95% CI, 2.73-12.83) than did patients without BPPV.
Conclusions and Relevance
The findings of this study suggest that the algorithm is efficient for the diagnosis of BPPV in a clinical care setting.
Introduction
Benign paroxysmal positional vertigo (BPPV) is an otologic pathologic condition defined as a sensation of spinning triggered by changes in head position relative to gravity and caused by an entrapment of fragmented endolymph debris most commonly in the posterior semicircular canal.1,2,3 A population-based study4 of BPPV reported a lifetime prevalence of 2.4%, a 1-year prevalence of 1.6%, and a 1-year incidence of 0.6%. The symptoms of BPPV can include brief episodes of spinning vertigo triggered by changes in head position; however, other vestibular disorders may have overlapping symptoms. To date, there is no accepted validated questionnaire for the diagnosis of BPPV. To help differentiate causes of vertigo and expedite diagnosis, Friedland et al5 designed a statistical algorithm using preencounter intake data for predicting vestibular diagnoses such as BPPV. This questionnaire solicits information such as the nature of and triggers for dizziness and frequency and duration of episodes. The authors found correlations between the results from the questionnaire and the final diagnosis.5 This questionnaire has not been assessed in populations outside the author's institution. Our goal was to assess the statistical algorithm by Friedland et al5 in a busy tertiary care setting, with the long-term goal of implementing a clinical pathway to efficiently diagnose and treat patients with dizziness.
Methods
We retrospectively reviewed the medical records of the last 200 patients who had new patient visits for vertigo from September 1, 2016, to December 31, 2016, at the Department of Otolaryngology–Head and Neck Surgery at Johns Hopkins University School of Medicine, Baltimore, Maryland. Patients are scheduled for a new patient visit for vertigo if they contact the call center and request to be seen for vertigo or dizziness. Patients can be scheduled after obtaining a referral from a primary care physician or specialist or by self-referral. Once scheduled, patients are seen by 1 of 7 otologists, neurotologists, or neurotology fellows. The patient may undergo vestibular testing, such as electronystagmography, before evaluation by a practitioner. Scanned questionnaires, notes, and discrete data, such as visit diagnoses, are entered into an electronic medical record (EMR). This study was approved by the Johns Hopkins Hospital Institutional Review Board.
Patient EMRs were reviewed to obtain the following information: vertigo, length of vertiginous spell (LOVS), and diagnosis. All included data were collected from the history of present illness from the first patient visit with a fellowship-trained neurotologist or otologist. Patients were included only if the history of present illness contained all the information as listed above. The information was entered into the formula identified for the linear predictor (LP) of BPPV as defined in Friedland et al5:
| LP = {[−2.19 + 1.87] × (lying down or rolling over) + [0.92 × (vertigo)] − [0.98 × (LOVS: minutes to hours)] − [1.11 × (LOVS: days)] − [1.84 × (vertigo)] × [(LOVS: days to weeks)]}. |
This was done using a 1 if present for each variable or a 0 if not present. If LOVS was defined as less than 20 minutes, all formulaic LOVS variables were given a value of 0. After the LP value was determined, it was transformed into an estimated probability (Pr) of BPPV with the following formula:
| Pr(BPPV) = exp(LP)/[1 + exp(LP)]. |
Nonparametric regression techniques were used to identify the statistical association between the LP value and vertigo. Simple logistic regression was then used to calculate the effect size of LP value on BPPV against all other patients. Predictive modeling was performed based on the LP cutoff value of 0.2, sensitivity and specificity were calculated, and area under a receiver operating characteristic (ROC) curve was calculated to assess the performance of the model. All statistical analyses in this work were performed using Stata software, version 15 (StataCorp).
Results
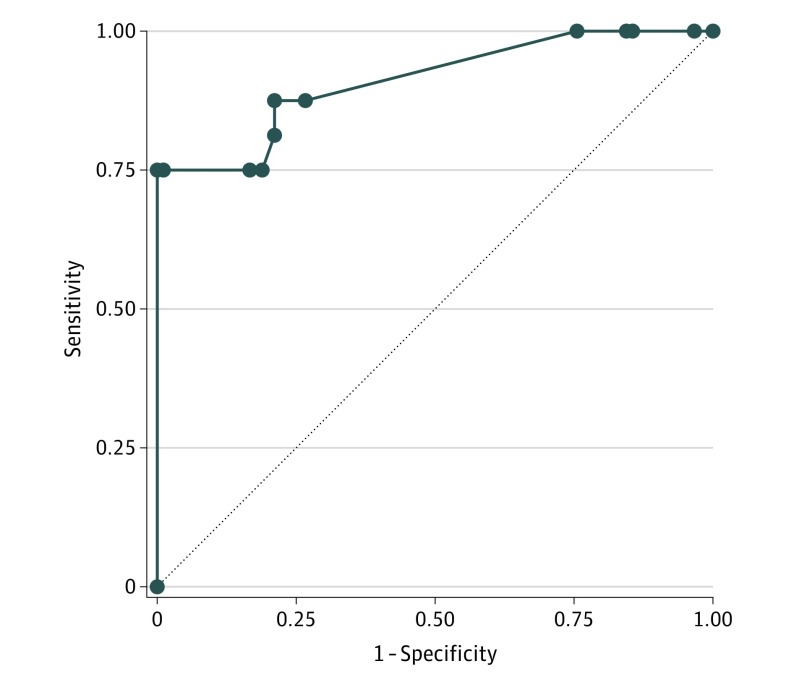
Of the 200 patient visits reviewed (132 [66%] female), 106 (53.0%; 68 [64%] female) had the information necessary to calculate the LP value and had a confirmed final diagnosis. The 94 patients who were not included did not have the information necessary explicitly stated in their EMRs to accurately calculate the LP value. Of these patients, 6 (6.4%) were diagnosed as having BPPV by a neurotologist. Ninety patients who did not meet the algorithm criteria for BPPV had vertigo that did not respond to repositioning maneuvers. Sixteen patients (1.7%) had vertigo that responded to repositioning maneuvers and were diagnosed as having BPPV (12 diagnosed with BPPV by the algorithm and 4 who did not meet the algorithm criteria for BPPV). In univariable analysis, the LP value was noted to be a significant predictor of BPPV (odds ratio, 5.92; 95% CI, 2.73-12.83). The sensitivity and specificity were calculated based on an LP cutoff of 0.2 as in the study by Friedland et al.5 There were 12 true-positive results, 4 false-negative results, 90 true-negative results, and no false-positive results.5 With the use of this criterion, sensitivity for the algorithm was 75% (95% CI, 46%-93%) and specificity was 100% (95% CI, 95%-100%) for predicting a diagnosis of BPPV. The positive predictive value was 100%, and the negative predictive value was 96%. Finally, a ROC curve was created based on the LP cutoff, with excellent predictive probabilities indicated by the area under the ROC curve of 0.91 (Figure).
Figure. Best Subsets Model.
The receiver operating characteristic (ROC) curve demonstrates excellent discrimination (area under the ROC curve, 0.91).
Discussion
In this assessment of the algorithm by Friedland et al,5 we tested the formula for predicting a diagnosis of BPPV from the histories obtained by the practicing physicians in our otologic clinics. We found that this algorithm was a useful aid for determining a diagnosis of BPPV. We classified patients as having symptoms for seconds to minutes if they reported a duration of symptoms less than 20 minutes and classified patients as having symptoms for minutes to hours if they reported symptoms that lasted 20 minutes or longer.5 We obtained this cutoff of 20 minutes from the study by Zhao et al6 because greater than 20 minutes was seen as a negative predictor for a diagnosis of BPPV.
The LP value of the model for BPPV was significant, with excellent predictive properties as demonstrated on cross-validation. This finding provides justification that the algorithm by Friedland et al5 predicts a diagnosis of BPPV. One patient had 2 diagnoses, one of which was BPPV. The LP value for this patient was not captured by our estimated probability cutoff and contributed to the false-negative results. In a study by Taura et al,7 up to one-third of patients with Ménière’s disease also had BPPV. Concomitant vertiginous diagnoses may complicate use of this formula. In contrast, we had no false-positive results, demonstrating that patients are likely to have an eventual diagnosis of BPPV if indicated by this formula. In a study that assessed the risk of BPPV in patients with vestibular migraine, Chu et al8 discovered that patients with migraine had a 2.03-fold increased risk of developing BPPV compared with corresponding age- and sex-matched control individuals.
Limitations
Our study is limited by the retrospective nature of this review. It was difficult to differentiate between vertigo episodes that lasted seconds to minutes from those that lasted minutes to hours because this was not always accurately recorded. Our study used physician records and not a questionnaire completed by the patient, which may have made duration data of symptoms more reliable. Therefore, we were limited to only 106 of 200 patients. Patients may interpret duration of symptoms on a questionnaire to imply length of illness; however, neurotologists would more likely correctly record the duration of actual symptoms. These limitations could account for the relatively high sensitivity and specificity of this study compared with the model by Friedland et al.5 In addition, there was only enough information to accurately calculate the LP value and compare diagnoses in half of the patients. The prevalence of BPPV in this study (8%) was lower than that in other reported series of patients who presented to clinics with dizziness and had BPPV.9,10,11 This lower prevalence may be attributable to the referral pattern for our institution as opposed to a true prevalence in the community.
Another explanation for the low prevalence of BPPV observed in this study is the duration that patients waited to see an otolaryngologist for evaluation of dizziness symptoms.12,13 The mean length of time that patients wait to see a dizziness specialist at Johns Hopkins University School of Medicine is 3 months. This finding suggests that patients who attend their appointments in our clinic to have their dizziness evaluated and are diagnosed with BPPV may have experienced symptoms for several months, during which they could have benefited from treatment with particle repositioning maneuvers. This finding motivates clinical pathways aimed at directing patients to appropriate treatment in a more timely manner.
Conclusions
This study suggests that the formula devised by Friedland et al5 can identify BPPV in most patients with dizziness with a simple algorithmic tool, which may be especially helpful in the clinical setting to direct patients to an appropriate physician. Our results may more closely mirror how well a physician could stratify BPPV compared with data from a patient-derived questionnaire and, thus, prove to be a good predictor of BPPV. In addition, defining duration of symptoms to fit into the algorithm can be challenging. We used a predetermined cutoff of 20 minutes; however, a more accurate definition may be available.
References
- 1.Kim JS, Zee DS. Clinical practice: benign paroxysmal positional vertigo. N Engl J Med. 2014;370(12):1138-1147. doi: 10.1056/NEJMcp1309481 [DOI] [PubMed] [Google Scholar]
- 2.Bhattacharyya N, Gubbels SP, Schwartz SR, et al. Clinical Practice Guideline: Benign Paroxysmal Positional Vertigo (Update) Executive Summary. Otolaryngol Head Neck Surg. 2017;156(3):403-416. doi: 10.1177/0194599816689660 [DOI] [PubMed] [Google Scholar]
- 3.Giommetti G, Lapenna R, Panichi R, et al. Residual dizziness after successful repositioning maneuver for idiopathic benign paroxysmal positional vertigo: a review. Audiol Res. 2017;7(1):178. doi: 10.4081/audiores.2017.178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.von Brevern M, Radtke A, Lezius F, et al. Epidemiology of benign paroxysmal positional vertigo: a population based study. J Neurol Neurosurg Psychiatry. 2007;78(7):710-715. doi: 10.1136/jnnp.2006.100420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Friedland DR, Tarima S, Erbe C, Miles A. Development of a statistical model for the prediction of common vestibular diagnoses. JAMA Otolaryngol Head Neck Surg. 2016;142(4):351-356. doi: 10.1001/jamaoto.2015.3663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhao JG, Piccirillo JF, Spitznagel EL Jr, Kallogjeri D, Goebel JA. Predictive capability of historical data for diagnosis of dizziness. Otol Neurotol. 2011;32(2):284-290. doi: 10.1097/MAO.0b013e318204aad3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Taura A, Funabiki K, Ohgita H, et al. One-third of vertiginous episodes during the follow-up period are caused by benign paroxysmal positional vertigo in patients with Meniere’s disease. Acta Otolaryngol. 2014;134(11):1140-1145. doi: 10.3109/00016489.2014.936624 [DOI] [PubMed] [Google Scholar]
- 8.Chu C-H, Liu C-J, Lin L-Y, Chen T-J, Wang S-J. Migraine is associated with an increased risk for benign paroxysmal positional vertigo: a nationwide population-based study. J Headache Pain. 2015;16:62. doi: 10.1186/s10194-015-0547-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tungvachirakul V, Lisnichuk H, O’Leary SJ. Epidemiology of vestibular vertigo in a neuro-otology clinic population in Thailand. J Laryngol Otol. 2014;128(suppl 2):S31-S38. doi: 10.1017/S0022215113003484 [DOI] [PubMed] [Google Scholar]
- 10.Lüscher M, Theilgaard S, Edholm B. Prevalence and characteristics of diagnostic groups amongst 1034 patients seen in ENT practices for dizziness. J Laryngol Otol. 2014;128(2):128-133. doi: 10.1017/S0022215114000188 [DOI] [PubMed] [Google Scholar]
- 11.Muelleman T, Shew M, Subbarayan R, et al. Epidemiology of dizzy patient population in a neurotology clinic and predictors of peripheral etiology. Otol Neurotol. 2017;38(6):870-875. doi: 10.1097/MAO.0000000000001429 [DOI] [PubMed] [Google Scholar]
- 12.Asawavichianginda S, Isipradit P, Snidvongs K, Supiyaphun P. Canalith repositioning for benign paroxysmal positional vertigo: a randomized, controlled trial. Ear Nose Throat J. 2000;79(9):732-734, 736-737. [PubMed] [Google Scholar]
- 13.Sekine K, Imai T, Sato G, Ito M, Takeda N. Natural history of benign paroxysmal positional vertigo and efficacy of Epley and Lempert maneuvers. Otolaryngol Head Neck Surg. 2006;135(4):529-533. doi: 10.1016/j.otohns.2005.09.021 [DOI] [PubMed] [Google Scholar]