Abstract
We describe a community-engaged approach with Medicaid Home and Community-Based Services (HCBS) home care aide (HCA), client, and physical therapist stakeholders to develop a mobile application (app) exercise intervention through focus groups and interviews. Participants desired a short exercise program with modification capabilities, goal setting, and mechanisms to track progress. Concerns regarding participation were training needs and feasibility within usual care services. Technological preferences were for simple, easy-to-use, and engaging content. The app was piloted with HCA-client dyads (n=5) to refine the intervention and evaluate content. Engaging stakeholders in intervention development provides valuable user-feedback on both desired exercise program contents and mobile technology preferences for HCBS recipients.
Keywords: home and community-based care, exercise, mobile applications, home care aides, older adults
Background
It is widely recognized that resistance exercise has significant health benefits for older adults ("American College of Sports Medicine Position Stand. Exercise and physical activity for older adults," 1998). Despite the associated positive health outcomes, less than 15% of older adults meet the American College of Sports Medicine (ACSM) recommendation of twice-weekly resistance exercise participation (Kraschnewski et al., 2014). Participation is further reduced in females and those with advanced age, disability, greater medication use, increased number of chronic conditions, and lower socioeconomic status (Struck & Ross, 2006), (Picorelli, Pereira, Pereira, Felicio, & Sherrington, 2014). These same factors are predictors of those who receive Medicaid Home and Community-Based services (HCBS) (Danilovich, Corcos, Marquez, Eisenstein, & Hughes, 2015), (Health and Medicine Policy Research Group, 2009).
Nationwide, roughly one million older adults use HCBS as an alternative to nursing home placement (Miller & Kirk, 2016). These low-income older adults have substantial physical and/or cognitive deficits commonly requiring the assistance of a home care aide (HCA), a formal caregiver who provides assistance with non-medical tasks such as activities of daily living (ADLs), housekeeping, and errands. Despite the widely-known benefits of exercise ("American College of Sports Medicine Position Stand. Exercise and physical activity for older adults," 1998), this intervention is not commonly included within the HCBS line of services. Further, the physical and cognitive deficits that make clients in need of HCBS are the very same deficits that pose substantial barriers to accessing community-based exercise interventions (Bethancourt, 2014). Thus, to increase participation in exercise among this vulnerable population, alternative in-home exercise strategies require investigation.
One strategy to increase resistance exercise participation among HCBS clients would be to embed this intervention within existing services. Having HCAs lead and supervise exercise during usual care services has been shown to increse accessibility and promote safety and adherence. Danilovich et al., investigated the implementation of the Strong for Life intervention led by HCAs (2016) while Park and Chodzko-Zajko studied the Healthy Moves for Aging Well prorgram (2014). Both studies showed HCAs could be trained to lead an exercise intervention and implement it successfully during usual care hours. Importantly, intervention satisfaction was high in both studies and 100% of clients and HCAs stated that exercise programs should be offered for all Medicaid HCBS clients (Danilovich, Hughes, Corcos, Marquez, & Eisenstein, 2016). However, Strong for Life was not originally intended for older adults receiving HCBS and Healthy Moves for Aging Well does not follow the ACSM recommendations for resistance exercise intensity. Strong for Life is administered following a DVD supplemented by a paper manual with exercise pictures. One limitation to thjs approaches is the lack of DVD players among HCBS clients and the limitations of paper handouts in explicitly showing real-time exercise technique and modifications (Danilovich, Hughes, Corcos, Marquez, & Eisenstein, 2016). Thus, the development of a mobile app with video instruction may be more beneficial to supplement in-person exercise instruction by detailing modifications and facilitating program sustainability by providing a mechanism for clients to access exercise with or without their HCA present.
While a number of mobile app exercise programs exist, to our knowledge, none have targeted frail older adults receiving Medicaid HCBS, nor engaged these important stakeholders in the development process. Given the low rates of exercise participation among older adults, we hypothesized that engaging these stakeholders in exercise program development would result in a program that integrated the preferences of Medicaid HCBS clients, along with best-practice recommendations from physical therapists to improve exercise participation rates and adherence. Once definitive exercise content was determined, we hypothesized that including stakeholders in the development of the mobile app technology used to access the exercise program would provide critical information to facilitate acceptability and usability of mobile technologies. This article describes the engagement of HCAs, older adult HCBS clients, and physical therapists in the design, development, and pilot testing of a mobile exercise app to: 1) determine preferred exercise content, 2) identify desired mobile app features, and 3) ascertain exercise training needs.
Methods
Design
The FRAIL: Functional Resistance Activities to Impact Frailty study is a randomized controlled trial (clinicaltrials.gov identifier NCT02942992) testing the effectiveness of a resistance exercise intervention delivered by HCAs to older adult Medicaid HCBS clients to reduce frailty (Danilovich, Diaz, Ciolinio, & Corcos, 2017). In the development phase of the FRAIL study, we employed a participatory action research design to co-develop the exercise intervention and mobile app through focus groups and semi-structured interviews with stakeholders. We then evaluated the acceptability and usability of the mobile intervention following a two-week pilot test. Intervention development occurred in three stages: 1) a qualitative stage focused on developing exercise program content, 2) a qualitative stage focused on developing the mobile app, and 3) a two-week pilot usability test of the app prototype with evaluation through client semi-structured interviews and HCA completion of the IBM Post-Study System Usability Questionnaire. The Northwestern University Institutional Review Board approved this study.
Recruitment
We recruited five HCAs to participate as stakeholders in our intervention development through presentations at a Medicaid HCBS provider company in-service. The primary goal in focus groups was to work with a specific goal towards developing an exercise intervention. We selected a sample size of five HCA-client dyads (10 total participants) to be within size recommendations for focus groups (Carlson and Glenton, 2011) and sized to facilitate completion of the working tasks associated with our stakeholder group. Further, our sample size met the minimum recommendations for mobile application usability testing (Virzi, 1992). Eligible HCAs were primarily English speaking and had one client each who would also enroll in this research study. Eligible clients were English speaking and 60 years of age and older. Criteria for HCBS enrollment in Illinois is net assets less than $17,500 and have an assessed need for nursing facility placement (Health and Medicine Policy Research Group, 2009). We enrolled the first five HCAs who expressed interested in the study who had an eligible client enroll in the study to become enrolled HCA-client dyads. We then recruited five different HCA-client dyads to participate in our pilot-testing stage. Of the ten HCAs and ten clients who participated in all phases in this development study, 100% of HCAs were African-American women, 90% of clients were African-American, and 20% of clients were male. All participants remained engaged throughout the length of the project and we had no study attrition. Four physical therapists with expertise in resistance exercise, geriatrics, and community-engaged research served as clinician stakeholders.
Stakeholder engagement process for exercise program content and mobile app features
Data collection occurred from July 2016 to March 2017 with HCA focus groups held in July and November, client semi-structured interviews conducted in August and September, physical therapist input gathered in January, training and a two-week pilot of the intervention with five HCA-client dyads for usability testing in February, and evaluation of the beta test using the IBMs Post-Study System Usability Questionnaire (Lewis, 1992) in March 2017. The IBM Post-Study System Usability Questionnaire usability survey consists of 14 items on a 5-point Likert scale ranging from 1 (not at all) to 5 (very) or 1 (strongly disagree) to 5 (strongly agree). All HCAs attended focus groups at Northwestern, were compensated for their time, and discussions were approximately two hours long. Client interviews lasted approximately 45 minutes, were conducted in-home, and clients were compensated for their time. A public health researcher trained in qualitative research methodology moderated all focus groups and semi-structured interviews, which were audio-recorded. Focus group and semi-structured interview questions used an inductive exploratory approach to investigate exercise and mobile app preferences. In the first focus group, we described the research study, explained the HCA and client stakeholder role, defined frailty and resistance exercise, discussed basic motivational theories, and brainstormed ideas for exercise approaches to fit in with usual care visits. We provided education on ACSM recommendations for exercise and discussed HCA and client preferred frequency, intensity, time and type of exercises. The second focus group focused on HCA training needs to implement exercise including motivational strategies, exercise progression, and research strategies to measure fidelity and adherence. All client interviews were conducted between the first and second HCA focus group. Client interviews explored exercise preferences, and barriers and facilitators to exercise. Physical therapist stakeholders reviewed focus group and client interview themes and provided solutions to integrate HCA and client preferences into an exercise intervention.
Data Analysis
All focus groups and interviews were audio-recorded, transcribed verbatim, and analyzed by a member of the research team (MD) to categorize feedback into themes. Although focus group discussions and semi-structured interviews used an exploratory approach, the goal was to develop a specific product, and as such, data analysis was steered by content to reach that objective. Participants answered specific questions and as such, data analysis focused on understanding the group preferences for content. Thematic analysis focused on: 1) preference for exercise content, 2) preferences for mobile technology, 3) required training needs, and 4) anticipated barriers and facilitators for exercise adherence. Usability survey questions were analyzed using Excel version 14.3.0 to provide frequencies and percentages of responses by survey item.
Results
Stage One: Exercise Content Preferences
We identified four themes regarding HCAs’ preferences for intervention content: 1) exercise and motivation training needs, 2) exercise simplicity with individualization capability, 3) short intervention duration, and 4) variety while maintaining routine. The focus groups revealed that some HCAs exercised regularly, while others were sedentary and requested more exercise instruction training before implementing the exercise intervention with their clients. The HCAs anticipated clients may defer exercise some days because of pain, being “unmotivated”, or depressed and wanted to learn motivational techniques to encourage participation. The concept of a behavioral contract was suggested by one HCA; “we are used to doing paperwork and having the client sign that we were there. We could have the client sign almost like a contract that they are doing this (the exercise program) with us together.” All HCAs thought that simple, easy-to-follow exercises would be most desired by their clients, but noted that some clients had medical conditions such as stroke or dementia that would necessitate exercise modifications. Learning to modify exercises was identified as an essential training element. A 20-30 minute program timeframe was noted to be feasible within usual care visits. All HCAs were uncertain of how to select the starting resistance level for their clients and wanted training to make this determination or be told where to begin. Finally, HCAs were concerned that clients would get “bored” over the six-month intervention and requested some variability in exercise content to keep the program engaging, while maintaining a familiar routine. One HCA suggested, “having a sitting program and a standing program would give variety…especially on those days she don’t feel like standing.” Further, the selection of a mobile tablet exercise program was reinforced by HCAs who noted that “not all clients have DVDs and not everybody has phones with apps”.
Client exercise preferences focused on three themes: 1) the need to address activities of daily living (ADLs), 2) short duration, and 3) concerns over the impact on the HCA-client relationship. Clients identified a range of ADLs with which they had difficulty (e.g., sit to stand, getting out of bed, going up stairs) and would like to improve upon. They did not want interventions that would be greater than 30 minutes. To encourage participation, clients suggested not describing the intervention as ‘exercise’, ‘fitness’, or ‘health’ as those terms sounded “too comprehensive and medical” and “something hard that I don’t want to do.” We incorporated this feedback by naming this an “activity program” that focused on functional activities. Clients expressed several concerns over HCAs delivering an exercise intervention and the adequacy of HCA training. One client noted that exercise was something that “my doctor would tell me to do” and clients didn’t view their HCA as a health care team member. The clients dependency upon the HCA for errands and housekeeping caused some concern that adding exercise would take away from their usual care services. This information was incorporated into recruitment materials for the randomized controlled trial of the intervention that stressed the short nature of the intervention that supplemented and did not reduce usual care hours. Both clients and HCAs advocated a behavioral contract prior to beginning exercise to increase intervention adherence. Both clients and HCAs also were familiar with resistance bands for exercise and supported using this form of resistance during exercise.
Stage Two: Mobile Application Preferences
Due to the researcher-proposed six-month intervention duration, HCAs suggested embedding a mechanism to track client functional progress in the app, as this would facilitate intervention adherence. Clients overwhelmingly did not want to complete exercises in time with the video, but rather wanted videos to demonstrate a few repetitions of the exercise so that each person could “go at your own speed.” Further, clients desired methods to individualize app content including selecting whether to complete exercises in sitting or standing, turning music on or off, and receiving motivational prompts that rewarded intervention success. Both clients and HCAs thought having a new tablet would be an incentive to participate, but were also concerned that the device could potentially be stolen.
Incorporation of Stakeholder Feedback into Mobile App
Physical therapist stakeholders were provided themes and quotes from interviews and focus group discussions to provide input on definitive exercise program recommendations and behavioral change strategies. To embed goal setting, physical therapists recommended structuring the intervention around the health action process approach (HAPA) model (Schwarzer, 1999) This model suggests that the adoption of health behaviors is composed of an intention phase and an action phase influenced by beliefs surrounding risk perception, outcome expectancies, planning strategies, and self-efficacy which facilitate movement from intending to exercise to active engagement. Participants who enroll in an exercise study have demonstrated some level of intention to exercise from the act of consenting to the study. Despite good intentions, long-term adherence remains challenging and addressing HAPA components in goal setting may assist intenders to sustain long-term engagement.
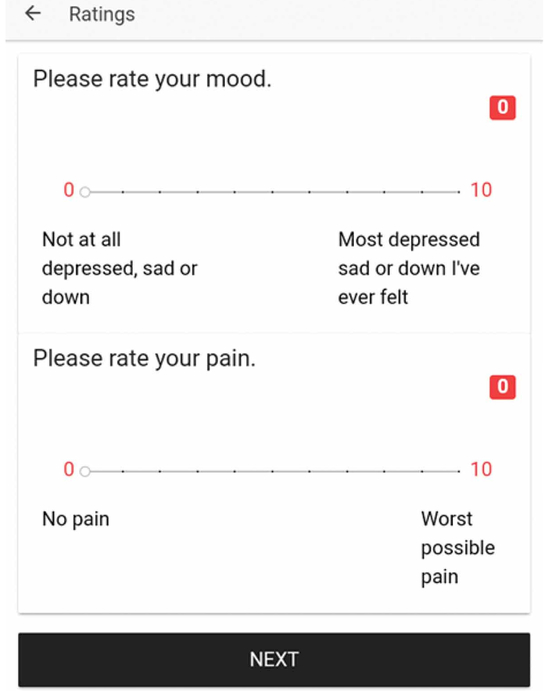
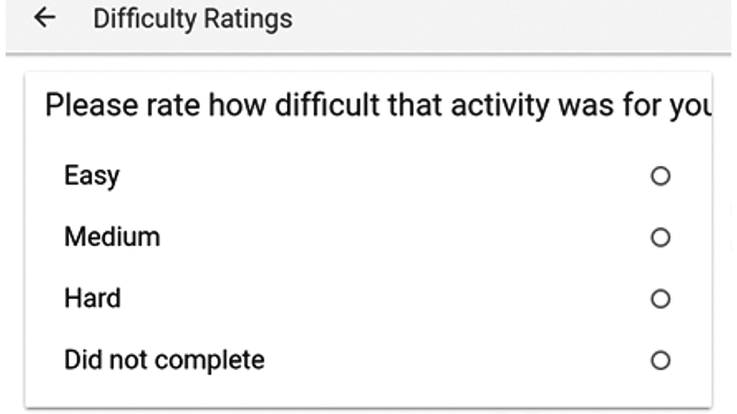
In order to assist HCAs with motivational encouragement, the client user starts each exercise session by ranking his/her pain and mood on an 11-point Likert scale with possible responses from 0 to 10 (Figure 1). Following each exercise, the user rates the difficulty of the exercise (Figure 2). At the completion of the program, the user ranks his/her pain and mood again and the session closes with a congratulatory message. The assessment of pain and mood was to provide HCAs with objective information on how their client is feeling that day as HCAs had identified pain and mood as primary barriers to participation during our focus group development phase. As part of training materials, physical therapist stakeholders developed strategies for HCAs to encourage participation in the face of common barriers such as fatigue and pain. For example, if a client declined participation due to pain, HCAs were trained to educate clients on the role of movement in reducing pain and could use pre- and post-test values from the app to demonstrate inter-session achievements.
Figure 1.
App mood and pain rating
Figure 2.
App rating of exercise difficulty
To address the preference for a familiar exercise routine with some variety, physical therapist stakeholders recommended a periodization resistance training approach for the overall exercise content. Periodization training is a resistance training method in which intensity and volume parameters vary to maximize strength outcomes by including recovery periods designed to facilitate improve neuromuscular performance. Further, periodization training allows for specific targeting of muscular training goals such as endurance, power, and strength during each period; all important components for comprehensive muscle performance in older adults (Signorile, Carmel, Lai, & Roos, 2005).
The exercise program has been described in detail elsewhere (Danilovich et al., 2017), but is a six-month program incorporating resistance bands, eight exercise, and utilizes four phases for muscle adaptation, strength, power, and endurance with a two-week active recovery phase in between each phase. To address preferences for a familiar exercise routine and exercises that addressed client-identified functional deficits, physical therapist stakeholders recommended these exercises which remain the same in each training phase: biceps curls, tricep press, chest press, lateral row, squats, heel raises, sidestepping, and mini-lunges. Active recovery phases consist of five minutes of walking at a self-selected fast speed, one minute of sit to stand exercises, and one-minute repetitions of balance activities including standing with feet together, semi-tandem, tandem, and one-legged. One minute dynamic balance tasks consist of lateral weight shifts and single steps in multiple directions.
Mobile app development process
Once all stakeholders provided input on exercise content and technological preferences, we partnered with the Northwestern University Center for Behavioral Intervention Technologies (CBITs) to develop the mobile app. As HCBS was a population unfamiliar to the CBITs programmers, we shared themes from our qualitiative development phase, as well as population demographics of HCBS users. In the Chicagoland area, HCBS clients are approximately 58% African-American and 24% White and 30% have moderate to severe cognitive impairment (Health and Medicine Policy Research Group, 2009). Clients have pronounced physical limitations and 99% are limited in completing instrumental activities of daily living such as housework, meal preparation, laundy, and activities outside of the home. Our previous work with this population found that 40% of HCAs did not have a high school diploma indicating the low levels of formal education among these formal caregivers (Danilovich, 2016). Based on this demographic profile, our knowledge of client and HCA abilities, and the preferences of clients and HCAs, we worked with the mobile app developers to purposefully create a very simplistic app that would be straightforward for naïve technology users and those without high levels of education.
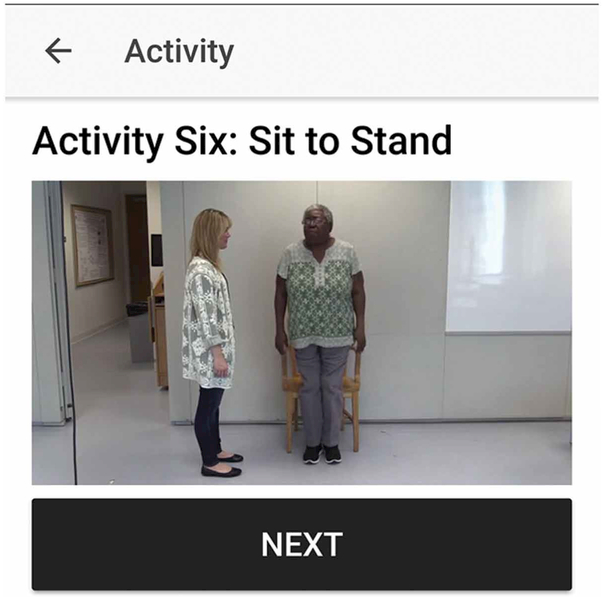
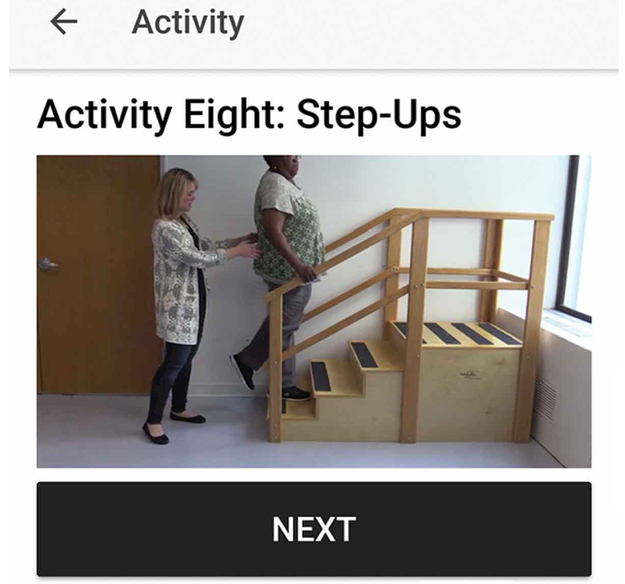
We selected an RCA Voyager 7inch tablet with 16GB of memory due to it being a low cost device with basic application capabilities using the Android® (Google, Mountain View, CA) 6.0 Marshmallow system. We selected an Android® system since it would allow us to use Google Play to download the app onto each tablet which is a more user-friendly platform to use than the Apple App Store. We filmed videos of each exercise in both standing and sitting with one of the HCAs from our pilot study. Screenshots of two of the exercises are shown in Figure 3 and 4. Users are presented with a video of the exercise, complete the number of repetitions prescribed for that phase of training, and select next when done. This structure incorporates client preferences for completing exercise at their own pace rather than in time with an exercise video. These videos were uploaded to the HockeyApp® platform to build the app which was then downloaded directly onto the mobile tablets so that users would not require internet access to load the app. When the app is connected to the internet, all app data can be downloaded into a researcher dashboard allowing the research team to view data on each participant including the length of time the app was open for each exercise session, client ratings of difficulty of each exercise per session, and individual session pre- and post-mood and pain ratings.
Figure 3.
Sit to Stand Exercise
Figure 4.
Step-up Exercise
Usability testing
Two physical therapists trained five HCAs to use the exercise app to lead the intervention during a half-day training session. Once trained, HCAs led the intervention with their clients for a two-week usability test. All ten HCAs and clients completed usability evaluations following the pilot test to further refine the mobile intervention. The HCAs completed a modified version of the IBM’s Post-Study System Usability Questionnaire (Lewis, 1992), a usability tool that surveys three domains: system usefulness, information quality, and interface quality. These domains are rated using a Likert Scale and open-ended questions allow for user feedback. Clients completed telephone semi-structured interviews to provide feedback on their experience. Finally, in consultation with the CBITs programmers, the research team reviewed multiple iterations of the app to provide feedback on functionality and aesthetics.
Stage Three: Pilot Test Results
All five HCAs were successfully trained in the intervention and were able to demonstrate competence through correctly answering written questions on resistance band levels, exercise progression, and successfully demonstrating appropriate exercise modifications. Following a two-week trial, we conducted a semi-structured interview with clients and a survey with HCAs to assess app usability. Overall, HCAs were highly satisfied with the app formatting, usability, and noted high levels of confidence to use the exercise app with minimal outside assistance (Table 1). Qualitative feedback from HCAs were that videos should be lighter and easier to view for clients, the videos would be “better if the HCA and client interacted throughout”, response anchors should be added to the Likert scale, and “featuring of clients doing things together – group exercise.” Clients overwhelmingly liked the mobile technology and found it easy to use, with the exception of one client who stated that he did not enjoy answering questions about pain and mood and wanted to “get started and get it (the program) done.”
Table 1:
HCA Results from IBM Post-Study System Usability Questionnaire
| Not at all | Somewhat | Very | |||
|---|---|---|---|---|---|
|
Overall, how helpful was the app in helping you lead the program? |
N=5 (100%) |
||||
| How organized was the app? | N=5 (100%) |
||||
|
How much new information the app provide? |
N=1 (20%) |
N=4 (80%) |
|||
| How easy was the app to use? | N=5 (100%) |
||||
|
How much did you like the format/design of the app? |
N=5 (100%) |
||||
|
How helpful were the features of the app? |
N=5 (100%) |
||||
|
How likely would you be to recommend this app to others? |
N=5 (100%) |
||||
|
Strongly disagree |
Disagree |
Somewhat |
Agree |
Strong agree |
|
| I would use the app frequently | N=1 (20%) |
N=4 (80%) |
|||
| I found the app complicated | N=2 (40%) |
N=2 (40%) |
N=1 (20%) |
||
|
I thought the app was easy to use |
N=1 (20%) |
N=4 (80%) |
|||
|
I think I would need support to use this app |
N=3 (60%) |
N=1 (20%) |
N=1 (20%) |
||
| I felt confident using the app | N=1 (20%) |
N=4 (80%) |
|||
|
Most home care aides would learn to use this app quickly |
N=2 (40%) |
N=3 (60%) |
|||
|
I needed to learn a lot before I could get going with this app |
N=4 (80%) |
N=1 (20%) |
Discussion
This paper presents, to our knowledge, the first work in engaging HCA and HCBS client stakeholders, along with physical therapists, in the development of both an exercise program and a mobile app to guide the intervention. Through co-development with our stakeholders, we identified preferences for exercise, mobile technology, training, and facilitating adherence. Our findings contribute new knowledge into the desired exercise parameters and technological preferences among HCA and HCBS clients, and our high satisfaction ratings in usability surveys suggests the stakeholder-engaged co-development process produces a highly acceptable product. Taken together, we document an extensive process to develop an exercise intervention that matches exercise principles and evidence-based recommendations with HCA and client preferences for exercise.
Older adult HCBS client stakeholders desired a short-duration intervention, help with goal setting, and motivation. These findings are congruent with other qualitative work with older adults that finds time is a primary barrier to physical activity, while social support facilitates accomplishing physical activity goals (Gothe & Kendall, 2016). Our incorporation of motivational prompts in the app mirrors the best-practice recommendation to provide users feedback on behavior and motivation in order to promote behavior change (Helbostad et al., 2017). We did not anticipate the strong client concerns about losing HCA care services with the addition of an exercise program or the view of the HCA as a caretaker versus healthcare team member. This is a novel fnding unique to the population of older adults receiving HCBS. These perspectives have important policy ramifications, as well as influencing how research studies are presented to the HCBS population. Reinforcing the addition of a research study to usual care services rather than removing usual care services may assist with recruitment. Further, it appears that providing education on the training and background of individuals assisting in a research study may help older adults mitigate fears about participation.
Pain and depression have been noted as barriers to exercise among the general population of older adults. Our results confirm this barrier is present among more functionally and cognitively impaired older adults receiving Medicaid HCBS. Given the variability in HCA training nationwide and the overall low amounts of training HCAs receive, they likely do not have the skills to motivate older adults to exercise in spite of these barriers. Thus, our approach of having older adults rate these levels prior to exercise participation and training HCAs in simple motivational interviewing techniques to encourage participation depending on the numeric ratings presents a novel mechanism to integrate both exercise programming and behavioral reinforcements into HCA services.
An important strength of this study was the design of both exercise content and the mobile app following an iterative design process among a diverse set of stakeholders. While our stakeholder group of five HCA-client dyads meets the minimum recommendation for a usability evaluation (Virzi, 1992), the small sample size in the pilot test precludes definitive recommendations to be made about exercise app effectiveness. However, all of our participants in our pilot test reported high satisfaction with the app and no difficulties with utilization. We do note that our participants were all urban dwelling, African-American participants and as such, exercise program and mobile app preferences may be varied among different sub-populations. We did not collect quantitative usability survey data from clients. Our objective was to use the mobile app to supplement the HCA exercise instruction, which is why we focused on the HCA’s perceptions of usability versus the client’s.
Results from the ongoing exercise trial will guide the determination of exercise program and app effectiveness. However, this paper contributes important knowledge on a first-of-its-kind process engaging Medicaid HCBS HCA and client stakeholders into the development of an exercise intervention on a mobile app. This exercise program may serve as a model for other agencies within the Medicaid HCBS system to integrate exercise programming within usual care services to bring needed physical activity into the homes of community-limited older adults, while empowering HCAs to expand their training, skills, and service offerings.
Acknowledgments
This project is supported by the Retirement Research Foundation (#2016-042), in part, by the National Institutes of Health's National Center for Advancing Translational Sciences, Grant UL1TR001422, and Performance Health. Content is solely the authors’ responsibility and does not necessarily represent the official views of the NIH.
Contributor Information
Margaret Danilovich, Northwestern University, Feinberg School of Medicine, Department of Physical Therapy and Human Movement Sciences.
Laura Diaz, Northwestern University, Feinberg School of Medicine, Department of Physical Therapy and Human Movement Sciences.
Gustavo Saberbein, Help at Home, Inc.
William Healey, Northwestern University, Feinberg School of Medicine, Department of Physical Therapy and Human Movement Sciences.
Gail Huber, Northwestern University, Feinberg School of Medicine, Department of Physical Therapy and Human Movement Sciences.
Daniel Corcos, Northwestern University, Feinberg School of Medicine, Department of Physical Therapy and Human Movement Science.
References
- American College of Sports Medicine Position Stand. Exercise and physical activity for older adults. (1998). Med Sci Sports Exerc, 30(6), 992–1008. [PubMed] [Google Scholar]
- Bethancourt HJ, Rosenberg DE, Beatty T, & Arterburn DE (2014). Barriers to and Facilitators of Physical Activity Program Use Among Older Adults. Clinical Medicine & Research, 12(1-2), 10–20. 10.3121/cmr.2013.1171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlsen B, & Glenton C (2011). What about N? A methodological study of sample-size reporting in focus group studies. BMC Medical Research Methodology, 11, 26 10.1186/1471-2288-11-26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danilovich MK, Diaz L, Ciolinio JD, & Corcos DM (2017). The FRAIL study: Functional Resistance Activities for Independent Living. Contemp Clin Trials. In press. [DOI] [PMC free article] [PubMed]
- Danilovich MK, Hughes SL, Corcos DM, Marquez DX, & Eisenstein AR (2016). Translating Strong for Life Into the Community Care Program. J Appl Gerontol, Jan 20(553-559). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gothe NP, & Kendall BJ (2016). Barriers, Motivations, and Preferences for Physical Activity Among Female African American Older Adults. Gerontol Geriatr Med, 2, 2333721416677399. doi: 10.1177/2333721416677399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health and Medicine Policy Research Group and UIC Center for Research on Health and Aging: Determination of need, service cost maximum study. Springfield, IL: Illinois Department on Aging, 2009. Retrieved from https://www.illinois.gov/aging/Resources/Documents/DON.pdf. Accessed on February 1, 2015. [Google Scholar]
- Helbostad JL, Vereijken B, Becker C, Todd C, Taraldsen K, Pijnappels M, … Mellone S (2017). Mobile Health Applications to Promote Active and Healthy Ageing. Sensors (Basel), 17(3). doi: 10.3390/s17030622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraschnewski JL, Sciamanna CN, Ciccolo JT, Rovniak LS, Lehman EB, Candotti C, & Ballentine NH (2014). Is exercise used as medicine? Association of meeting strength training guidelines and functional limitations among older US adults. Prev Med, 66, 1–5. doi: 10.1016/j.ypmed.2014.05.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller NA, & Kirk A (2016). Predicting State Investment in Medicaid Home- and Community-Based Services, 2000-2011. J Aging Soc Policy, 28(1), 49–64. doi: 10.1080/08959420.2016.1111729 [DOI] [PubMed] [Google Scholar]
- Park CH, & Chodzko-Zajko W (2014). Feasibility of integrating the "Healthy moves for aging well" program into home care aide services for frail older adults. J Exerc Rehabil, 10(3), 191–197. doi: 10.12965/jer.140116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Picorelli AM, Pereira LS, Pereira DS, Felicio D, & Sherrington C (2014). Adherence to exercise programs for older people is influenced by program characteristics and personal factors: a systematic review. J Physiother, 60(3), 151–156. doi: 10.1016/j.jphys.2014.06.012 [DOI] [PubMed] [Google Scholar]
- Signorile JF, Carmel MP, Lai S, & Roos BA (2005). Early plateaus of power and torque gains during high- and low-speed resistance training of older women. J Appl Physiol (1985), 98(4), 1213–1220. doi: 10.1152/japplphysiol.00742.2004 [DOI] [PubMed] [Google Scholar]
- Struck BD, & Ross KM (2006). Health promotion in older adults. Prescribing exercise for the frail and home bound. Geriatrics, 61(5), 22–27. [PubMed] [Google Scholar]
- Virzi RA Refining the test phase of usability evaluation: how many subjects is enough? Hum Factors, 34(4), 457–468. [Google Scholar]