Abstract
Introduction
Ninety percent of all injury-related deaths occur in low- and middle-income countries. The WHO recommends short, resource-specific trauma courses for healthcare providers. Studies show that teaching trauma courses to medical students in developed countries leads to significant increases in knowledge and skill. High costs hinder widespread and sustained teaching of these courses in low-income countries.
Methods
A two-day trauma course was designed for students at Moi College of Health Sciences in Eldoret, Kenya. Participants underwent pre- and post-course written and simulation testing and rated their confidence in 21 clinical scenarios and 15 procedures pre- and post-course using a five point Likert scale. A subset of the students was re-evaluated nine months post-course. Using the paired t-test, mean written, simulation and confidence scores were compared pre-course, immediately post-course and nine months post-course.
Results
Twenty-two students were enrolled. Written test score means were 61.5% pre-course and 76.9% post-course, mean difference 15.5% (p < 0.001). Simulation test score means were 36.7% pre-course and 82.2% post-course, mean difference 45.5% (p < 0.001). Aggregate confidence scores were 3.21 pre-course and 4.72 post-course (scale 1–5). Ten out of 22 (45.5%) students were re-evaluated nine months post-course. Results showed written test score mean of 75%, simulation score mean of 61.7%, and aggregate confidence score of 4.59 (scale 1–5). Mean differences between immediate post- and nine months post-course were 1.6% (p = 0.75) and 8.7% (p = 0.10) for the written and simulation tests, respectively.
Conclusion
Senior Kenyan medical students demonstrated statistically significant increases in knowledge, skills and confidence after participating in a novel student trauma course. Nine months post-course, improvements in knowledge skills and confidence were sustained.
African relevance
-
•
In many African countries, WHO-recommended short trauma courses are not uniformly taught
-
•
Teaching a trauma course as a capstone for healthcare professional students ensures sustainability
Introduction
Injury accounts for more than five million deaths globally, approximately equal to deaths from HIV, malaria and TB combined [1]. Ninety percent of injury-related deaths occur in low and middle-income countries such as Kenya. In an observational study of public emergency centres in Kenya in 2011, trauma was the second most common presenting complaint [2]. Similarly, a descriptive study of the emergency centre at a national referral hospital showed that injury was the top presenting complaint [3]. Despite this, Kenya has no organised system of trauma care and clinicians lack specific training on the systematic management of the acutely injured patient.
In its guidelines for essential trauma care, the World Health Organization (WHO) recommends short, resource specific trauma courses for providers working in low-income countries [4]. The Advanced Trauma Life Support (ATLS) is a well-known short trauma course developed and administered by the American College of Surgeons [5], [6]. The course has been shown to improve provider knowledge and to confer long-lasting skills on the organised and priority-based approach to the injured patient [7]. Studies show that teaching ATLS to medical students leads to significant increases in knowledge and skill and is well received [8], [9], [10]. However, high start-up costs and ongoing faculty and resource investment hinder the widespread teaching of ATLS in low-income countries. Several modified ATLS courses that have been developed as alternatives have contributed to significant knowledge and skill acquisition, improved confidence, and enhanced team dynamics in trauma management [11], [12], [13]. Furthermore, systematic reviews have shown that such short trauma courses contribute to significant reduction in mortality [14]. These courses are traditionally taught as Continuous Medical Education (CME) to heterogeneous groups of clinicians, are sporadically offered, and have been difficult to sustain. None of these courses have been implemented and evaluated at the medical school level in Kenya.
Accordingly, we sought to develop and evaluate a novel, low cost, emergency trauma course based on ATLS principles but adapted to the needs of medical students and resources available in Kenya. We selected Kenya as an ideal site for this study as Moi University School of Medicine was supportive of developing greater curriculum in trauma care and the need for such clinical expertise is substantial. In our analysis, we examined the impact of this course on medical students’ knowledge, skill, and confidence in managing acutely injured patients presenting to an emergency centre setting.
Methods
The study was carried out at Moi University College of Health Sciences, which is affiliated with Moi Teaching and Referral Hospital (MTRH), a public tertiary referral hospital in Eldoret, Kenya. Moi University College of Health Sciences and MTRH are part of the Academic Model Providing Access to Healthcare (AMPATH), a consortium of North American academic health centres involved in research and health care in Kenya. The study was approved by the Miriam Hospital/Brown University Institutional Review Board, and the Institutional Research and Ethics Committee at MTRH.
Prior to the course, a needs assessment was carried out. Medical education in Kenya begins after high school, and is structured as three years pre-clinical work, 4th year core clinical rotations (Surgery, Medicine, Paediatrics, Obstetrics/Gynaecology), 5th year elective rotations and 6th/final year repeat core clinical rotations with a senior student role. After graduation, the new physicians are sent to district hospitals all over the country as interns serving in surgical, medicine, paediatric and obstetric/gynaecology departments. After internship, a small subset of trainees elect to pursue further post-graduate Master’s training while the majority work as general practitioners. A structured questionnaire was used to evaluate whether final-year medical students were interested in a trauma course and what topics they considered relevant. We also surveyed key faculty members who are involved in trauma care and medical student education at Moi University College of Health Sciences. Additionally, we assessed the equipment and facilities available at Moi Teaching and Referral Hospital based on the WHO Guidelines for Essential Trauma Care.
Results from the needs assessment were used to modify course material developed by the Brown University Division of Global Emergency Medicine to the Kenyan context. These materials included didactic lectures created using ATLS guidelines, skill stations, radiology stations, simulations, and teamwork exercises. Similar material has been used to pilot and implement three short trauma courses elsewhere [15], [16]. The course was further adapted for medical students by reducing the amount of time spent on didactic material, introducing radiology stations, dedicating more time to skill stations, teamwork and simulation exercises. Low-cost, locally sourced materials were used to create a chest tube and cricothyroidotomy model as previously reported by Pringle et al. [15]. A standardised and systematic approach to the injured patient, as stipulated through ATLS principles, was emphasised throughout the course. The material was reviewed and approved by attending physicians from the Brown University Division of Global Emergency Medicine and key faculty members from Moi University College of Health Sciences. Table 1 shows the course timetable with details on the didactic material, procedure labs and radiology stations.
Table 1.
Course timetable.
| Day 1 | Day 2 | ||
|---|---|---|---|
| 8.00–8.30 a | Intro to course, intro to simulation | 8.00–9.30 a | Procedure labs (Airway, IV placement, tube thoracostomy, E-FAST) |
| 8.30–10.30 a | Written and simulation pre-test | 9.30–10.00 a | Extremity trauma |
| 10.30–11.30 a | Primary survey + interventions + shock | 10.00–10.30 a | Burns |
| 11.30 a–12.00 p | Secondary survey | 10.30–12.00 p | Radiology stations (Chest X-ray, cervical spine X-ray, head CT, pelvis X-ray, extremity X-rays) |
| 12.00–1.00 p | Lunch | 12.00–1.00 p | Lunch |
| 1.00–2.00 p | Primary + secondary survey practice | 1.00–1.30 p | Trauma in extremes of age |
| 2.00–2.30 p | Head + Face trauma | 1.30–2.00 p | Trauma in pregnancy |
| 2.30–3.00 p | Cervical spine trauma | 2.00–2.30 p | Kenya-specific cases |
| 3.00–3.30 p | Chest trauma | 2.30–3.00 p | Triage and transfer |
| 3.30–4.00 p | Abdomen + pelvis trauma | 3.00 p-4.30 p | Written and simulation post test |
| 4.00–5.00 p | Teamwork exercises | 4.30–5.30 p | Simulation review, debrief, graduation |
| Adjourn | |||
E-FAST, Extended Focused Assessment with Sonography for Trauma.
We conducted a pre- and post-longitudinal study of participants in the short course, which was implemented from March 28–29, 2015. Participants were surveyed for their knowledge, skill, and confidence at the start of the course and after completing the course. All medical students who had completed or were currently in their surgical rotations were eligible to participate in the course and the study. After informed consent, all 22 eligible medical students agreed to participate for an inclusion rate of 100%. Nine months later in January 2016, all students who had participated in the initial course were invited back for re-evaluation testing. Ten out of 22 students (45.5%) were available to participate in the written, simulation and confidence re-testing.
We evaluated participants’ knowledge, skills, and confidence as outcomes. To assess knowledge, we used two sets of 23 Multiple Choice Questions (MCQs, sample test Appendix A) that evaluated knowledge about emergent trauma care: Test A and Test B. The two tests were unique but were matched in the trauma care concepts tested. In the pre-intervention period, participants were randomly assigned to either Test A or Test B. In the post-intervention period, those previously assigned to Test A were assigned to Test B and vice versa, to avoid bias from previous exposure to knowledge items. Knowledge was rated as acceptable for those with scores of 60% correct or greater, as per earlier studies [12]. To assess skills, we used four simulation cases: 1) closed head injury requiring intubation, 2) blunt abdominal trauma in a pregnant woman, 3) gunshot wound to the right chest and 4) blunt abdominal trauma from a motorcycle accident. At the pre-intervention period, participants were randomly assigned to either simulation cases 1 and 2 or to simulation cases 3 and 4. In the post-intervention period, those previously assigned to simulation cases 1 and 2 were assigned to simulation cases 3 and 4 and vice versa, to avoid bias from previous exposure to the cases. The students underwent simulation testing in pairs. Each pair underwent two simulation cases pre- and post-course. Every student assumed a leadership role once in a pre-course case and once on a post-course case. Three assessors were involved in each simulation case: one acted as the injured patient, the second acted the role of a nurse, and the third assessor observed and scored the students’ performances. An assessment tool was used to test the performance of the primary and secondary survey and key associated critical actions (Appendix B). This tool was adapted from the Trauma Team Training (TTT) program [13]. Scores were awarded based on the core approach to all injured patients, and case-specific critical actions. The tool was also used to score team organisation and dynamics. Score differences between the pre- and post-course simulation performance were used as the primary outcome for skill acquisition. Lastly, we evaluated self-confidence in performing key procedures using a course questionnaire comprised of 36 items rated with a 5-point Likert scale (Appendix C). Twenty-one of these items covered clinical scenarios and 15 were related to life-saving procedures. Increased scores indicated greater self-confidence in performing necessary procedures. The MCQ tests, simulation assessment tool and the confidence evaluation questionnaire were piloted in prior short trauma courses [15], [16]. At the nine-month re-evaluation, a convenience sample of students took a new MCQ test (Test C) and a new simulation case. Self-confidence was evaluated using the same set of 36 items used in prior testing.
The demographic features of the participating medical students and their knowledge, skills, and self-confidence in pre-intervention, post-intervention and nine-month post-intervention periods were evaluated using standard descriptive statistics. The statistical significance of changes in knowledge and skills was assessed using the paired t-test. A confidence level of alpha <0.05 was employed. Analyses were carried out using Microsoft Excel 2011 and SAS 9.3 (SAS Institute Inc. Cary, NC, USA).
Results
Twenty-two final-year medical students participated in the course. Thirteen (59%) were male. Mean age was 27.4 years. One of the students had clinical experience prior to medical school, and one other student had taken a modified ATLS course prior to the student trauma course.
Written test mean score for 22 students was 61.5% pre-course and 76.9% immediately post-course and mean difference between pre- and immediate post-testing was 15.5% (p = 0.0001). Simulation test score means improved from 36.7% pre-course to 82.2% post-course, with a mean difference of 45.5%. (p = 0.0001). Nine months post course, ten out of 22 students (45.5%) were re-evaluated. Within this subset, the written test score mean was 62% pre-course, 73% immediately post-course, and 75% nine months post-course. Mean difference between pre- and immediate post-course written testing was 12% (p = 0.0104), between immediate post-course and 9 month post-course was 1.6% (p = 0.74) and between pre-course and 9 month post testing was 13.6% (p = 0.0089). Within the same subset, simulation test scores were 32.6% pre-course, 70% immediately post-course and 61.7% nine months post-course. Mean difference between pre- and immediate post-simulation testing was 37.8% (p = <0.0001), between immediate post-testing and 9 month post-testing was 8.7% (p = 0.1009) and between pre-course and 9 month post-course was 29.1% (p = 0.0005).
Mean confidence scores increased pre- to post-course on all 36 measures evaluated: 21 clinical scenarios and 15 procedures. For all 22 students, aggregate mean scores increased from 3.21 pre-course to 4.72 post-course (scale 1–5). For the 21 clinical scenarios only, mean confidence scores increased from 3.34 pre-course to 4.74 post-course. The clinical scenarios with the greatest improvements were evaluation of neck and back pain and evaluation of pelvic instability. For the 15 life-saving procedures, mean confidence scores increased from 3.01 pre-course to 4.69 post-course. The greatest improvements were observed in the performance of the Focused Assessment with Sonography for Trauma (FAST) exam and cricothyroidotomy.
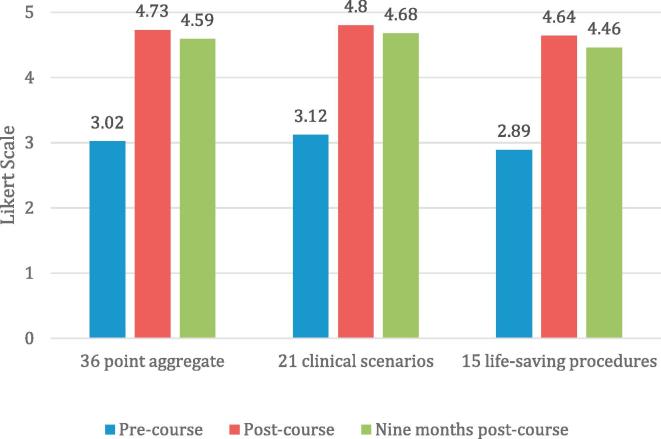
Nine months post course, ten out of 22 students (45.5%) underwent confidence-re-evaluation. Within this subset, aggregate mean confidence scores were 3.02 pre-course, 4.73 immediately post-course and 4.59 nine months post-course (scale 1–5). For the 21 clinical scenarios only, confidence scores were 3.12 pre-course, 4.8 immediately post-course and 4.68 nine months post-course (scale 1–5). For the 15 life-saving procedures, confidence scores were 2.89 pre-course, 4.64 immediately post-course and 4.46 nine months post-course (scale 1–5). Fig. 1 shows the changes in confidence scores in the re-evaluation subset as described.
Fig. 1.
Mean confidence scores in the re-evaluation subset.
Discussion
Our results indicate that a novel student trauma course resulted in significant improvements in knowledge, skills and confidence in trauma management for graduating students at a Kenyan medical school. There were statistically significant increases in knowledge as measured by written test scores and skills as measured by simulation test scores pre- and post-course. There was also a significant improvement in self-reported confidence on all 36 items evaluated, including 21 clinical scenarios and 15 life-saving procedures pre- and post-course.
Ten out of 22 students were re-evaluated nine months post-course. This subset was representative of the primary group as evidenced by the fact that their mean written test, simulation and confidence scores were not significantly different from the primary group. Within this subset, we observed a statistically significant increase in written test scores pre- and post-course that was sustained nine months post course. Simulation test scores were also significantly improved pre- to post-course, and this improvement was sustained nine months later. There was a significant improvement in self-reported confidence scores on all the 36 items tested pre- to post-course. A slight decrease in self-reported confidence was noted nine months later. This trend persisted when the confidence evaluation was broken down to 21 clinical scenarios and 15 life-saving procedures. However, nine-month post-course confidence scores were still significantly better than pre-course scores.
The pre- to post-course increases in written test and simulation scores observed are similar to studies in which the standard ATLS course was introduced to senior medical students in North America [7], [8], [9], [17]. The nine-month post-course knowledge and skill retention corroborates prior work that has demonstrated that the skills in the organised and prioritised care of injured patients gained from the standard ATLS course can last for up to eight years [7]. However, the high costs and significant faculty investment required to teach the standard ATLS course to medical students led us to design a modified ATLS course adapted to the context and resources found in Kenyan public hospitals. This course made use of low-cost simulation and skill stations that were employed successfully in Nicaragua by Pringle, et al. [15]. Additional modifications included allocating less time to didactic material since the students had received prior instruction during their surgical rotation.
As our results show, mean pre-course written test score was 61.5%, which was above the passing grade of 60%. More emphasis was placed on skill stations and simulations. Study results support this approach since pre-course simulation scores were low and the students demonstrated lack of an organised and structured approach to the simulated injured patient. Post-course a much greater improvement was observed in simulation test scores compared to written test scores: Mean improvement of 45.5% and 15.5%, respectively. Thus simulation stood out as a key tool for the effective teaching of a student trauma course in a developing country. The use of low cost, locally sourced, easily obtainable materials further facilitated this methodology.
It is notable that nine months post-course, there was no statistically significant decay in skills as measured through simulation. A systematic review of trauma and resuscitation courses shows declines in simulation and skills testing that are documented as early as three months post-course [18]. This finding is significant since the students get minimal exposure to acutely injured patients, and did not receive any refresher training prior to the 9-month re-evaluation. This result points to the strength of the methodology that was focused on, and repeatedly emphasised the organised and systematic approach to the injured patient using simulation. Further studies will be carried out to determine the persistence of this finding within a greater sample of students.
A slight decline was observed when comparing immediate post-course and nine-month post-course confidence scores, although the 9-month post-course scores were still significantly improved compared to pre-course testing. Self-reported confidence scores are a measure of self-efficacy, thus our results indicate that our students experienced a minimal decline in self-efficacy. Several factors may have contributed to this finding. Our student participants are not routinely exposed to acutely injured patients in the Emergency Centre or to the hands-on simulation environment. This likely contributed to the very low pre-course confidence scores and the significant immediate post-exposure improvement. After the course, the students returned to their routine education that involves limited exposure to acutely injured patients and limited exposure to simulation. This contributed to the slight decrease in their confidence and self-efficacy.
The decision to anchor the trauma course in a medical school was based on several factors. First, since Emergency Medicine is not a formally recognised specialty, Kenyan medical students lack structured instruction and exposure to injured patients in the Emergency Centre. This limits their skill and confidence in taking care of acutely injured patients in spite of their demonstrated adequate knowledge base. Upon graduation, these new physicians practice relatively independently as interns in district hospitals. There are few opportunities for additional post-graduate training. Therefore the final year of medical training presents an opportunity to integrate a trauma course that uses simulation to challenge students to translate their knowledge into hands-on skills and to increase their confidence and self-efficacy in taking care of injured patients.
The second reason to introduce a trauma course into the medical school curriculum is to ensure its sustainability. Despite their demonstrated success, modified ATLS courses that are taught as continuing medical education (CME) in Kenya have been sporadic and not sustainable. The goal is to incorporate this course as a capstone within the surgical curriculum. At Moi University College of Health Sciences, students have a one-week clerkship known as ‘The management of the severely injured patient and mass casualty management’ during their surgical rotation in the 4th and 6th year. This trauma course will be integrated into this one-week clerkship for 6th year students. This will not only contribute to sustainability but also ensure that the course is uniformly taught.
Limitations to this study include a small sample size at a single medical school. The sample was limited by the fact that we could only recruit students who were currently in, or who had just completed their surgical clerkship. Few students were able to attend the re-evaluation since it occurred after they had already graduated and left the university. The multiple-choice tests and simulation scoring tool used in our evaluation have not been validated. This factor limits our study, although care was taken to ensure that the written tests evaluated similar concepts, and the simulation tool has been used in several similar studies.
We used simulation scores as a surrogate measure of skill acquisition, but it is impossible to know how this measure translates into clinical practice. In addition, while self-reported confidence scores indicate improved self-efficacy in taking care of injured patients, the impact on clinical care is yet to be evaluated. Future work is required to determine the impact of this course on clinical outcomes.
Conclusion
Senior students at a Kenyan public medical school demonstrated statistically significant improvements in knowledge, skills and confidence in trauma management after participating in a novel, low-cost, student trauma course. This modified trauma course for students produced similar results as standard ATLS taught to medical students in developed countries, but at a cheaper cost. Knowledge and skills were sustained on re-testing nine months later, and a slight decline was observed in self-reported confidence. This course can be integrated as a valuable capstone for all graduating students at medical and health professional schools in low- and middle-income countries with heavy trauma burdens and limited post-graduate training.
Conflicts of interest
The authors report no conflict of interest.
Author contributions
GW conceived original idea, applied for grant funding and coordinated the study. HJ carried out the needs assessment, taught the trauma course, helped in data collection and analysis. JF assisted with course development, taught and supervised the course, assisted with manuscript preparation. RP assisted with course development, taught and supervised the course, assisted with manuscript preparation. AL assisted with course development, taught and supervised the course, assisted with manuscript preparation. JT was the site director in Kenya. Assisted with course development, coordinated and supervised the course, assisted with manuscript development. YW assisted with course development, taught the course and collected data. AK assisted with course development, taught the course and collected data. JC was the faculty site director at Brown University and Kenya. Assisted with IRB development, course development.
Dissemination of results
The findings from this study were shared with the Dean of Moi University College of Health Sciences in Eldoret Kenya, the Chair of the Emergency Department at the Alpert Medical School of Brown University, and the AMPATH team leader in Eldoret, Kenya.
Acknowledgements
We would like to thank Benjamin Wachira, Florian Schmachtenberg, Claire Burgardt, Elizabeth Sutton, Naomi George, and Arabia Molette for their support in this project. Grant funding for the course was provided by the Emergency Medicine Resident’s Association’s Global Health Impact Award and the Framework in Global Health Scholarship from Brown University’s Global Health Initiative. The course was directed by faculty from the Global Emergency Medicine Health Division of the Emergency Department at the Alpert Medical School of Brown University, and faculty from Moi University College of Health Sciences. Janet O’Connell and The Brown-Kenya office provided logistical support and the AMPATH research office reviewed the research proposal. Faculty from the Emergency Medicine Kenya Foundation provided assistance in teaching the course. Elizabeth Bradley provided writing assistance as the instructor of the Global Health Research Colloquium in which the primary author was enrolled at Yale University.
Footnotes
Peer review under responsibility of African Federation for Emergency Medicine.
Supplementary data associated with this article can be found, in the online version, at https://doi.org/10.1016/j.afjem.2017.04.013.
Appendix A. Supplementary data
References
- 1.Lopez A.D., Mathers C.D., Ezzati M. World Bank; Washington (DC): 2006. Global Burden of Disease and Risk Factors. Disease Control Priorities Project. [Google Scholar]
- 2.Wachira B.W., Wallis L.A., Geduld H. An analysis of the clinical practice of emergency medicine in public emergency departments in Kenya. Emerg Med J. 2012;29(6):473–476. doi: 10.1136/emj.2011.113753. [DOI] [PubMed] [Google Scholar]
- 3.House D.R., Nyabera S.L., Yusi K. Descriptive study of an Emergency center in Western Kenya: challenges and opportunities. African Journal of Emergency Medicine. 2014;4(1):19–24. [Google Scholar]
- 4.Mock C., Lormand J.D., Goosen J. World Health Organization; Geneva: 2004. Guidelines for essential trauma care. [Google Scholar]
- 5.American College of Surgeons . American College of Surgeons; Chicago, IL: 2008. Advanced Trauma Life Support for Doctors. [Google Scholar]
- 6.Carmont M. The Advanced Trauma Life Support course: a history of its development and review of related literature. Postgrad Med J. 2005;81(952):87–91. doi: 10.1136/pgmj.2004.021543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mohammad A., Branicki F., Abu-Zidan F.M. Educational and clinical impact of Advanced Trauma Life Support (ATLS) courses: a systematic review. World J Surg. 2014;38(2):322–329. doi: 10.1007/s00268-013-2294-0. [DOI] [PubMed] [Google Scholar]
- 8.Ali J., Howard M. The advanced trauma life support course for senior medical students. Can J Surg. 1992;35(5):541–545. [PubMed] [Google Scholar]
- 9.Ali J., Cohen R., Reznick R. Demonstration of acquisition of trauma management skills by senior medical students completing the ATLS program. J Trauma. 1995;38(5):687–691. doi: 10.1097/00005373-199505000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Ali J., Cohen R.J., Gana T.J. Effect of the Advanced Trauma Life Support program on medical students’ performance in simulated trauma patient management. J Trauma. 1998;44(4):588–591. doi: 10.1097/00005373-199804000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Jana B.A., MacLeod J.B.A., Okech M. Evaluation of trauma and critical care training courses on the knowledge and confidence of participants in Kenya and Zambia. World J Surg. 2011;35(1):9–16. doi: 10.1007/s00268-010-0810-z. [DOI] [PubMed] [Google Scholar]
- 12.Nogaro M.C., Pandit H., Peter N. How useful are Primary Trauma Care courses in sub-Saharan Africa? Injury. 2015;46(7):1293–1298. doi: 10.1016/j.injury.2015.04.010. [DOI] [PubMed] [Google Scholar]
- 13.Bergman S., Deckelbaum D., Lett R. Assessing the impact of the trauma team training program in Tanzania. J Trauma. 2008;65(4):879–883. doi: 10.1097/TA.0b013e318184a9fe. [DOI] [PubMed] [Google Scholar]
- 14.Peter A.M., Alexis A.T., Heather K.C. Resuscitation training in developing countries: a systematic review. Resuscitation. 2010;81(11):1462–1472. doi: 10.1016/j.resuscitation.2010.06.024. [DOI] [PubMed] [Google Scholar]
- 15.Pringle K., Mackey J.M., Modi P. A short trauma course for physicians in a resource-limited setting: is low-cost simulation effective? Injury. 2015;46(9):1796–1800. doi: 10.1016/j.injury.2015.05.021. [DOI] [PubMed] [Google Scholar]
- 16.Janeway H., Modi P., Wanjiku G. Training the trainers in emergency medicine: an advanced trauma training course in Rwanda’s medical simulation center. Pan Afr Med J. 2015;20:242. doi: 10.11604/pamj.2015.20.242.6358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Papp K.K., Miller F.B. A required trauma lecture series for junior medical students. J Trauma. 1995;38(1):2–4. doi: 10.1097/00005373-199501000-00002. [DOI] [PubMed] [Google Scholar]
- 18.Mosley C., Dewhurst C., Molloy S. What is the impact of structured resuscitation training on healthcare practitioners, their clients and the wider service? A BEME systematic review: BEME Guide No. 20 (2012) Med Teach. 2012;34(6):e349–e385. doi: 10.3109/0142159X.2012.681222. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.