Abstract
Introduction
Emergency Medical Services are ideally placed to provide relief of acute pain and discomfort. The objectives of this study were to describe pre-hospital pain management practices by Emergency Medical Services in the Western Cape, South Africa.
Methods
A retrospective, descriptive survey was undertaken of analgesic drug administration by advanced life support paramedics. Patient care records generated in the City of Cape Town during an 11-month period containing administrations of morphine, ketamine, nitrates and 50% nitrous oxide/oxygen were randomly sampled. Variables studied were drug dose, dose frequency, and route of administration, patient age, gender, disorder and call type as well as qualification and experience level of the provider.
Results
A total of 530 patient care records were included (n = 530). Morphine was administered in 371 (70%, 95% CI 66–74) cases, nitrates in 197 (37%, 95% CI 33–41) and ketamine in 9 (1.7%, 95% CI 1–3) cases. A total of 5 mg or less of morphine was administered in 278 (75%, 95% CI 70–79) cases, with the median dose being 4 mg (IQR 3–6). Single doses were administered to 268 (72.2%, 95% CI 67–77) morphine administrations, five (56%, 95% CI 21–86) ketamine administrations and 161 (82%, 95% CI 76–87) of nitrate administrations. Chest pain was the reason for pain management in 226 (43%) cases. Advanced Life Support Providers had a median experience level of two years (IQR 2–4).
Discussion
Pre-hospital acute pain management in the Western Cape does not appear to conform to best practice as Advanced Life Support providers in the Western Cape use low doses of morphine. Chest pain is an important reason for drug administration in acute pre-hospital pain. Multimodal analgesia is not a feature of care in this pre-hospital service. The development of a Clinical Practice Guideline for and training in pre-hospital pain should be viewed as imperative.
Abstract
Introduction
Les services d'aide médicale d'urgence sont dans une position idéale pour atténuer les douleurs aigues et la gêne. Les objectifs de cette étude étaient de décrire la gestion préhospitalière de la douleur par les services d'aide médicale d'urgence dans la province du Cap occidental, en Afrique du Sud.
Méthodes
Une étude rétrospective et descriptive a été réalisée sur l'administration d'analgésiques par des auxiliaires médicaux spécialisés en réanimation. Les dossiers médicaux des patients générés dans la ville du Cap sur une période de 11 mois indiquant l'administration de morphine, de kétamine, de nitrates et d'un mélange de protoxyde d'azote/oxygène à 50 % ont été échantillonnés de manière aléatoire. Les variables étudiées étaient la dose de médicament, la fréquence d'administration des doses et la voix d'administration, l'âge du patient, son sexe, le trouble dont il souffre et le type d'appel, ainsi que les qualifications et le niveau d'expérience de l'administrateur.
Résultats
Au total, 530 dossiers médicaux de patients ont été inclus (n = 530). De la morphine a été administrée dans 371 (70 %, IC 95% 66–74) cas, du protoxyde d'azote dans 197 (37 %, IC 95 % 33–41) cas et de la kétamine dans 9 (1,7 %, IC 95 % 1–3) cas. Un total de 5 mg de morphine ou moins a été administré dans 278 (75 %, IC 95 % 70–79) cas, la dose moyenne étant de 5 mg (IIQ 3–6). Des doses uniques ont été administrées pour 268 (72,2 %, IC 95 %, 67–77) administrations de morphine, cinq (56 %, IC 95 % 21–86) administrations de kétamine et 161 (82 %, IC 95 % 76–87) administrations de protoxyde d'azote. Les douleurs thoraciques étaient la raison de l'administration d'analgésiques dans 226 (43 %) cas. Les auxiliaires médicaux spécialisés en réanimation disposaient d'un niveau d'expérience moyen de deux ans (IIQ 2–4).
Discussion
La gestion préhospitalière de la douleur aiguë dans la province du Cap occidental ne semble pas se conformer aux meilleures pratiques, car les auxiliaires médicaux spécialisés en réanimation utilisent de faibles doses de morphine. Les douleurs thoraciques constituent une raison importante de l'administration d'analgésiques pour le traitement préhospitalier de la douleur aiguë. L'analgésie multimodale n'est pas une caractéristique des soins dans ce service préhospitalier. Le développement de Directives pratiques cliniques pour la formation à la gestion préhospitalière de la douleur devrait être considéré comme un impératif.
African relevance
-
•
Advanced life support providers are responsible for advanced pre-hospital pain management in this setting.
-
•
There does not appear to be a decisive, pre-hospital pain management strategy locally, to support quality out of hospital care.
-
•
Chest pain is the single largest pain disorder managed by advanced life support providers in the local urban setting.
Introduction
Acute pain is frequently encountered by Emergency Medical Services (EMS) [1], [2], [3], [4], [5], positioning EMS well for expeditious relief of pain. Unfortunately, pre-hospital management of acute pain is often ineffective, rates of analgesia use are frequently low and oligoanalgesia is common [6], [7], [8], [9]. Pre-hospital pain management is influenced by patient characteristics such as gender [6], age [10], [11], and race [12]. Additional factors which show an association with quality of pain management are rates of pain scale documentation [13], [14], the experience of acute care providers [8], on-scene times [6], [9] and pain severity [10]. The pre-hospital environment is dynamic and complex and may render some interventions difficult, impossible or undesirable. Pain management may be seen as secondary to stabilization and rescue of patients [15].
The Health Professions Council of South Africa (HPCSA), which prescribes the South African EMS scope of practice and protocols nationally, has not published explicit acute pain management guidelines and South African pre-hospital practice in respect of acute pain management is unknown. With as many as seven different EMS qualifications active in South Africa, the potential for practice variation is significant. Local descriptive research is thus important. This study aimed to describe pre-hospital pharmacological analgesia practices in the City of Cape Town. Specific objectives were to describe the age and gender profile of patients, the injury types for which analgesics were administered, the qualifications and experience levels of administering providers, along with the type, dosage, dosage frequency and route of administration of analgesic drugs, and the frequency of objective pain assessment.
Methods
The study was a retrospective, descriptive survey of patient care records reporting analgesic drug administration by advanced life support paramedics. Currently, five of the seven qualifications active in the South African EMS are viewed by the HPCSA as being advanced level qualifications. For convenience sake persons of all advanced qualifications were collectively termed Advanced Life Support (ALS) Providers (qualifications are listed in the results).
Data was collected in the City of Cape Town, from the Medical Emergency Transport and Rescue Organisation (METRO), the EMS service of the Provincial Government of the Western Cape. During the data collection period, the city had a population of 3,740,026 people in an area of 2206 square kilometres. During the study period of August 2013 to July 2014, METRO provided services to a substantial number of patients, of which 347,844 were primary responses and 174,843 were inter-facility transfers. Ethics approval for this study was granted by the Human Research Ethics Committee of the University of Cape Town (HREC Ref: 318/2014).
Patient care records were included if administrations of 50% nitrous oxide/oxygen gas (Entonox®), nitrates, morphine or ketamine were recorded in the context of acute pain. While nitrates are not classified as analgesic agents, they do reduce the intensity of chest pain [16], and were included in both cardiac-specific guidelines [17] and South African EMS protocols [18] for use in the context of cardiac related chest discomfort. The same guidelines also advise that morphine is only used if nitrates do not reduce pain intensity, and as such, the use of nitrates can be expected in the context of chest pain and would influence morphine use. For these reasons, we felt it appropriate to include nitrates in a study of pre-hospital acute pain. Only adults (>18 years) were included in the study as paediatric data required a separate and more complex ethics process for which, at the time, specific regulations had not been published. It was thus decided to omit paediatric data from the study. The presence of pain was determined if a pain score was present, the word “pain” or an equivalent such as “tenderness” appeared on the patient care record or if a condition clearly requiring pain intervention was present.
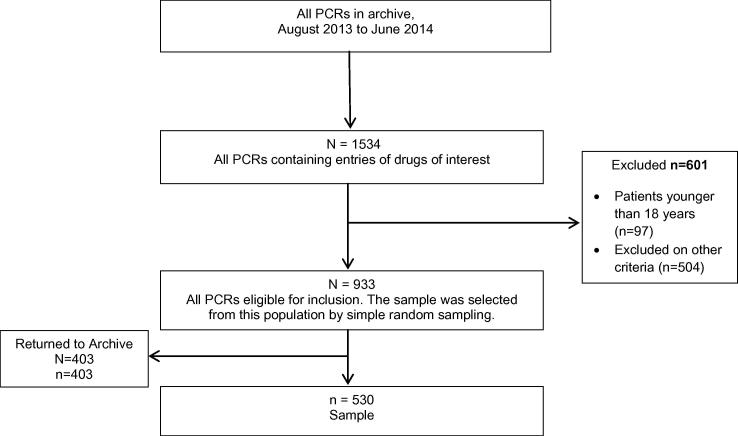
Intubated patients were excluded, as morphine and ketamine may be used for induction and sedation in these patients, and the drugs might have been administered for this purpose rather than analgesia. Unconscious patients were excluded, as objective self-reported pain assessment is not possible in these cases. If clear drug dosage information was missing, or if it could not be determined that the ALS provider had made the decision to administer the drug, the patient care record was excluded. Trained research assistants screened all patient care records generated by ALS providers between August 2013 to July 2014 containing an entry of Entonox®, nitrates, morphine or ketamine. The frequency of drug administrations per month for METRO was not known and data from the month of July 2013 was used as a pilot to inform parameters for a sample size calculation as well as to pilot the data collection tool. The sample size was calculated to determine the proportion of cases where morphine was administered within a certain precision range. Assuming a sample proportion of 50% (proportion of cases where morphine was administered), we calculated a sample size of 530 to detect a CI precision of 8.5%. A total of 1534 patient care records were found containing administrations of the drugs of interest and the primary researcher read each one to determine eligibility for inclusion. Of these, 601 were excluded based on criteria. The remaining 933 patient care records in the sample frame were allocated a sequential number and computer generated simple random sampling was used to select 530 patient care record to form the sample (Fig. 1).
Fig. 1.
The process of sampling the patient care reports. PCR, patient care record.
Information on total dosage of the drug, the number of administrations per case, gender and age of patients, type of case (primary response or inter-facility transfer) and qualification of ALS provider was collected. Pain intensity scores, by Numerical Rating Scale (NRS), were recorded only as being present or absent. Experience levels of ALS providers were estimated by cross-referencing the professional registration number, detailed on the patient care record, with registration information available on the iRegister of the HPCSA [19]. As ALS providers often contributed to more than one entry in the analysis, assigning unique study numbers ensured consistent data on Providers, qualifications and experience levels. Data was captured in a separate password protected spreadsheet (Microsoft Excel, Microsoft Corporation, Redmond, WA) and stored securely.
Continuous data was described using means and standard deviations or medians and interquartile ranges, depending on the distribution of data. Normality of data was tested qualitatively (graphs) and quantitatively. Categorical data was described using proportions and 95% confidence intervals. Chi-square tests were used to test associations between categorical data. Hypotheses with continuous data were tested with t-tests or ANOVA. Spearman’s rank was used to determine significant correlations. P-values of 0.05 were considered statistically significant. Where appropriate, non-parametric tests were used. Data was analysed using Statistica version 12 (2014).
Results
A total of 530 patient care records were included, representing drug administrations by 117 individual Providers. The mean age of the population was 46.8 years (SD 18.2) and 324 (61.4%) were male. Trauma accounted for 262 (49.4%, 95% CI 45–54) cases and non-traumatic acute pain for the remainder. Table 1 summarises the injury and disorder types in which pain was being treated. ALS provider qualifications are summarised in Table 2. Case type and pain assessment proportions are described in Table 3.
Table 1.
Proportion of injuries by type.
| Type of Injury | n (%) | 95% CI |
|---|---|---|
| Soft Tissue (including Burns) | 74 (14) | 11–17 |
| Fractures, Amputations, Dislocations | 132 (25) | 21–29 |
| Stab and Gunshot Wounds | 52 (10) | 7–13 |
| Chest Pain | 226 (42) | 38–47 |
| Non-Traumatic Pain (including Back Pain) | 42 (8) | 6–11 |
| No diagnosis noted | 4 (1) | 0–2 |
Table 2.
Provider qualifications.
| Provider Qualification | In Advanced Qualification | In EMS | |
|---|---|---|---|
| n (%) | Median (IQR) in years1 | Median (IQR) in years1 | |
| Critical Care Assistant | 46 (39) | 3 (2–5) | 10 (6–12) |
| Emergency Care Technician | 21 (18) | 1 (1–2) | 7 (6–12) |
| National Diploma: Emergency Medical Care | 34 (29) | 3 (2–3.75) | 3.5 (2–7) |
| Bachelor of Technology: Emergency Medical Care | 16 (14) | 2.5 (2–4) | 5 (3.75–10.25) |
| Total | 117 (100) | 2 (2–4) | 7 (4–11) |
IQR, interquartile range.
Represents full years, or part thereof. Inferred level of experience by qualification of the practitioner (measured by date of registration with the HPCSA). A fifth qualification, Bachelor Emergency Medical Care, was not represented in the sample.
Table 3.
Type of case and frequency of pain assessment.
| n (%) | 95% CI | |
|---|---|---|
| Primary Response | 469 (88) | 85–9 |
| Inter-facility Transfer | 61 (12) | 9–15 |
| Cases with Recorded Pain Assessment (NRS) | 111 (21) | 18–25 |
| Cases with Second Pain Assessment (NRS) | 34 (6) | 4–9 |
NRS, numerical rating scale.
No administration of Entonox® was found. Morphine was administered in 371 (70%, 95% CI 66–74) cases, nitrates in 197 (37%, 95% CI 33–41) and ketamine in nine (1.7% 95% CI 1–3) cases. Descriptive statistics for drug administrations are recorded in Table 4. All intravenous (IV) drug administrations were in the form of boluses and no evidence of ALS provider-initiated infusions was found. The median total dose of morphine was 4 mg (IQR 3–6) and of ketamine was 50 mg (IQR 50–100). Of the morphine administrations, a total of 5 mg or less was administered in 278 (75%, 95% CI 70–79) cases. A single dose of morphine was administered in 268 (72.2%, 95% CI, 67–77) cases, two doses in 86 (23%, 95% CI, 19–28) and three doses in 18 (5%, 95% CI 3–8) cases. Additional doses raised the total mean morphine dose to 6 mg for two doses and 8 mg for three doses (p < 0.01).
Table 4.
Characteristics of drug administrations.
| Morphine n (%) | Ketamine n (%) | Nitrates* n (%) | |
|---|---|---|---|
| Proportion of Cases | 371 (70) | 9 (1.7) | 197 (37) |
| Only Drug Administered | 322 (87) | 6 (67) | 148 (75) |
| Intravenous Route | 366 (99) | 9 (100) | – |
| Single Dose | 268 (72) | 5 (56) | 161 (81) |
Describes both Isosorbide Dinitrate tablets (5 mg) and Glyceryl Trinitrate spray (0.4 mg).
Morphine was administered intramuscularly in six (1.4%, 95% CI 1–3) cases, while the sublingual route was used for all nitrate administrations. Morphine was co-administered with nitrates in 47 (24%, 95% CI 18–30) cases and with ketamine in three (33%, 95% CI 7–70) cases.
For the different qualifications, the mean total dosages of morphine were 4.4 mg for Critical Care Assistants (95% CI, 3.9–4.8), 4.8 mg for Emergency Care Technicians (95% CI, 4.2–5.3), 5 mg for National Diplomas (95% CI, 4.6–5.5) and 5.4 mg for Emergency Care Practitioners (95% CI, 4.7–6.1. These differing dosages were statistically significant (p = 0.03).
Discussion
This study is the first to describe operational pre-hospital pain management practices in the Western Cape. Best practice is considered to be the administration of pain medications based on a self-reported objective pain score such as the NRS [20], [21] as subjective and clinical pain assessments have been found to be unreliable and underestimate pain intensity [22], [23], [24], [25]. Higher rates of objective pain assessment are associated with higher rates of analgesia use [13]. We found the use of an objective pain score in approximately a fifth of cases and poor follow-up assessment. This rate is consistent with some international findings [3], though others show much higher rates of assessment [2], [9].
Effective morphine doses are difficult to define. Some texts advocate small boluses in an individual titration based manner [26] and others an initial weight based dose of 0.1 mg/kg [27], which has also been shown to be ineffective for pain control in the Emergency Centre (EC) 30 min after administration [28]. Research evaluating pre-hospital pain management report total morphine doses of between 5 mg [9] and 13.5 mg ± 3 mg [4] with varying levels of pain reduction. While a dose of 0.15 mg/kg provided statistically superior pain reductions compared to doses of 0.1 mg/kg, it was not necessarily clinically superior in reducing pain intensity at 30 and 60 min [29]. A pre-hospital randomised controlled trial comparing a 0.05 mg/kg bolus and subsequent 0.025 mg/kg titrations with 0.1 mg/kg boluses and 0.05 mg/kg titrations found both regimens provide similar pain reduction at 30 min, with the higher dose provided significantly better pain reduction at 10 min [30] which is more desirable in the pre-hospital context. At a median of 4 mg, the total morphine dose in our study is low, even with the uncertainty surrounding effective doses. Considering the low proportion of objective pain assessments, specifically reassessment after the intervention, pain management in this setting does not conform to best practice and is possibly ineffective.
Most morphine doses were administered as a single bolus, without concomitant administration of another drug. Our study supports the finding that South African ALS providers are familiar with weight-based dosing, but most would never exceed 5 mg as an initial bolus and they would definitely never exceed a total of 10 mg, citing fear of adverse events [31]. Fear of adverse events are a common reason for withholding analgesia or using lower doses [31], [32], even though they occur infrequently and are mostly mild [33].
Our study does not shed light on how ALS providers decide on the dose of morphine to administer. A titration based strategy seems unlikely as it is reasonable to expect multiple boluses together with multiple pain assessments in such an approach. Our findings do not definitively indicate that pain assessments were not taking place. Scoring systems require cognition, hearing and numeracy on the part of the patient, which we could not determine from the patient care records. Pain may have been assessed and not recorded, or an adjective type scale may have been used rather than the NRS, as the word “pain”, or pain equivalent words were frequently found on patient care records. Whether these constitute assessment or are merely case notes is unknown. ALS providers have indicated that they base pain assessment not just on a pain score but on clinical presentation, disorder type and clinical experience [31], [32], [34].
Providers' experience levels have been associated with differences in prescribing patterns in the EC [35] and lower experience levels have been associated with oligoanalgesia [8]. The median experience level of ALS provider was 2 years, within a narrow range, and this is possibly too low to definitively determine the influence of experience on practice. Statistically significant differences in morphine doses were found between the qualifications, but the range of these differences is within one milligramme, and the clinical significance is probably negligible. As the different qualifications do not seem to differ in approach to dosing in pain management, critical evaluation of education and training and the development of contextualised pre-hospital Clinical Practice Guidelines (CPGs) are imperatives [36].
ALS providers in our study did not use multimodal analgesia. The basis for multimodal analgesia is the synergistic effects of the combination therapy, acting on different sites and pain pathways, which provides more effective analgesia and fewer adverse events as lower doses of each drug are used [37]. Pre-hospital trials have found the combination of morphine and ketamine result in a significant reduction in morphine dose [38] and produce faster and superior pain intensity reduction than morphine alone [39], with an improvement in haemodynamic parameters [40]. In practice, South African ALS providers have very limited pharmacological analgesia options available. Only bachelor’s degree holders were authorised to use ketamine and, anecdotally, Entonox® was not available on the majority of ambulances despite being authorised for use by the HPCSA. This leaves morphine and nitrates as the only options available to most Providers. The reasons for Entonox® being absent are speculative, but might be due to expense, the bulky equipment making it unpopular operationally or concerns over the control of the drug. The high rate of unimodal analgesia in this study might reflect limited drug options rather than decision-making.
The majority of ALS provider-initiated analgesia took place on primary responses, with only a small percentage of inter-facility transfers documenting ALS provider-initiated analgesia. Reasons for this include the following of physician’s orders and continuation of hospital-initiated infusions or assumption that in-hospital analgesia was effective without requiring further adjustment. There is evidence in the literature that provision of analgesia in-hospital is suboptimal [41], [42], [43], [44], [45] and that patients frequently experience high levels of pain during inter-facility transfer [46], [47]. Our study was not designed to detect oligoanalgesia and no conclusions are drawn regarding oligoanalgesia in Western Cape Hospitals, or during transfer.
Prevalence of cardiac chest pain presenting to EMS has been reported to be between 17% [2] and 29% [4]. In our study, ALS providers were likely to administer analgesia in pain of traumatic and medical aetiologies in roughly equal proportions; the finding that chest pain was the reason for drug administration in 43% cases was unexpected. While this data cannot be used to determine disorder prevalence, it does suggest the types of working diagnoses being made during treatment. In this pre-hospital service, 12 lead ECGs were not present on the ambulances during the study period and ALS providers were probably basing management decisions on clinical presentation and a 3 lead ECG tracing. The use of morphine in non-ST-elevation myocardial infarction (NSTEMI) has been associated with harm [48], though it does remain in guidelines [49] as a reasonable intervention. As initiation of chest pain management protocols appears frequent, ongoing training relating to the management of chest pain, and the use of 12 lead ECG is an imperative.
This study only examines cases in which drugs were administered and no conclusions regarding the prevalence of acute pain can be drawn. The injuries and disorders represent the ALS providers’ diagnosis and not definitive diagnoses, as no hospital data was collected. Transport and drug administration times were not collected, and the effect of time on drug analgesia cannot be examined. Time data is subject to inaccuracy, as it is frequently impossible to complete patient care records during the management of the case. Patient care records may be completed once the patient has been handed over and time data may be estimated. Provider experience was inferred from date of registration, and Providers may not have always been active in a clinical environment thus actual clinical experience may have been overestimated. Bachelor’s degree graduates’ levels of experience will have been underestimated, as these Providers would have held an advanced qualification prior to graduation. While we believe the selected variables to have been recorded accurately, allowance must be made for the inaccurate recording of variables, which is recognised as one of several limitations of medical chart reviews [50].
In conclusion, though this study does not provide a definitive answer, pre-hospital pain management in this setting is probably arbitrary and ineffective. There is very little documented evidence of objective pain assessment and morphine doses administered by ALS providers are low. Most drugs are administered as single boluses and multimodal analgesia is not a feature of this EMS, possibly as a result of limited availability of alternate drugs. Experience levels of ALS providers are low, and it is uncertain if qualification type influences pain management in any way. Chest pain is the reason for a significant number of drug administrations in the context of acute pain and management of this disorder requires more attention. While data was collected in a single service, the standardised training, scope of practice and accreditation of ALS providers by a single national body is a reason to believe that similar results may be found in other pre-hospital services in the country. The lack of an official pre-hospital pain management CPG is a glaring omission and may contribute to poor practice. The development of a CPG and ongoing training in pre-hospital acute pain management is an imperative.
Conflicts of interest
Funds were received from the Emergency Care Institute (ECI). The ECI played no role in the conception, design, data collection, analysis or writing of the manuscript. The authors declare no other conflicts of interest.
Dissemination of results
The results were presented to personnel of the ambulance service concerned, at a Continuing Professional Development (CPD) event.
Authors’ contributions
RM conceived and designed the study, supervised collection and recording of the data, and was primarily responsible for analysis, interpretation of data and writing of the manuscript. MM provided input and assistance with statistical consulting, writing of results, preparation of tables and figures and editing the manuscript. WS supervised the original research dissertation on which the manuscript is based and assisted with writing and editing of the manuscript. All authors agreed to the final text.
Footnotes
Peer review under responsibility of African Federation for Emergency Medicine.
References
- 1.Berben S.A., Schoonhoven L., Meijs T.H.J.M. Prevalence and relief of pain in trauma patients in emergency medical services. Clin J Pain. 2011;27(7):587–592. doi: 10.1097/AJP.0b013e3182169036. [DOI] [PubMed] [Google Scholar]
- 2.Jennings P.A., Cameron P., Bernard S. Epidemiology of prehospital pain: an opportunity for improvement. Emerg Med J. 2011;28(6):530–531. doi: 10.1136/emj.2010.098954. [DOI] [PubMed] [Google Scholar]
- 3.Kosiński S., Bryja M., Wojtaszowicz R. Incidence, characteristics and management of pain in one operational area of medical emergency teams. Anaesthesiol Intensive Ther. 2014;46(2):83–87. doi: 10.5603/AIT.2014.0016. [DOI] [PubMed] [Google Scholar]
- 4.Galinski M., Ruscev M., Gonzalez G. Prevalence and management of acute pain in prehospital emergency medicine. Prehosp Emerg Care. 2010;14(3):334–339. doi: 10.3109/10903121003760218. [DOI] [PubMed] [Google Scholar]
- 5.Marinangeli F., Narducci C., Ursini M.L. Acute pain and availability of analgesia in the prehospital emergency setting in Italy: a problem to be solved. Pain Pract. 2009;9(4):282–288. doi: 10.1111/j.1533-2500.2009.00277.x. [DOI] [PubMed] [Google Scholar]
- 6.Michael G.E., Sporer K.A., Youngblood G.M. Women are less likely than men to receive prehospital analgesia for isolated extremity injuries. Am J Emerg Med. 2007;25(8):901–906. doi: 10.1016/j.ajem.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 7.Siriwardena A.N., Shaw D., Bouliotis G. Exploratory cross-sectional study of factors associated with pre-hospital management of pain. J Eval Clin Pract. 2010;16(6):1269–1275. doi: 10.1111/j.1365-2753.2009.01312.x. [DOI] [PubMed] [Google Scholar]
- 8.Albrecht E., Taffe P., Yersin B. Undertreatment of acute pain (oligoanalgesia) and medical practice variation in prehospital analgesia of adult trauma patients: a 10 yr retrospective study. Br J Anaesth. 2013;110(1):96–106. doi: 10.1093/bja/aes355. [DOI] [PubMed] [Google Scholar]
- 9.Bakkelund K.E., Sundland E., Moen S. Undertreatment of pain in the prehospital setting: a comparison between trauma patients and patients with chest pain. Eur J Emerg Med. 2013;20(6):428–430. doi: 10.1097/MEJ.0b013e32835c9fa3. [DOI] [PubMed] [Google Scholar]
- 10.Jennings P.A., Cameron P., Bernard S. Determinants of clinically important pain severity reduction in the prehospital setting. Emerg Med J. 2012;29(4):333–334. doi: 10.1136/emj.2010.107094. [DOI] [PubMed] [Google Scholar]
- 11.Infinger A.E., Studnek J.R. An assessment of pain management among patients presenting to emergency medical services after suffering a fall. Prehosp Disaster Med. 2014;29(4):344–349. doi: 10.1017/S1049023X14000594. [DOI] [PubMed] [Google Scholar]
- 12.Young M.F., Hern H.G., Alter H.J. Racial differences in receiving morphine among prehospital patients with blunt trauma. J Emerg Med. 2013;45(1):46–52. doi: 10.1016/j.jemermed.2012.07.088. [DOI] [PubMed] [Google Scholar]
- 13.Frakes M.A., Lord W.R., Kociszewski C. Factors associated with unoffered trauma analgesia in critical care transport. Am J Emerg Med. 2009;27(1):49–54. doi: 10.1016/j.ajem.2008.01.005. [DOI] [PubMed] [Google Scholar]
- 14.Simpson P.M., Bendall J.C., Tiedemann A. Provision of out-of-hospital analgesia to older fallers with suspected fractures: above par, but opportunities for improvement exist. Acad Emerg Med. 2013;20(8):761–768. doi: 10.1111/acem.12190. [DOI] [PubMed] [Google Scholar]
- 15.van der Velde J., Linehan L., Cusack S. Helicopter Winchmens’ experiences with pain management in challenging environments. Ir Med J. 2013;106(2):42–44. [PubMed] [Google Scholar]
- 16.Engelberg S., Singer A.J., Moldashel J. Effects of prehospital nitroglycerin on hemodynamics and chest pain intensity. Prehosp Emerg Care. 2000;4(4):290–293. doi: 10.1080/10903120090940967. [DOI] [PubMed] [Google Scholar]
- 17.O’Connor E.R., Brady W., Brooks S.C. Part 10: acute coronary syndromes: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122(18):S787–S817. doi: 10.1161/CIRCULATIONAHA.110.971028. [DOI] [PubMed] [Google Scholar]
- 18.Professional Board for Emergency Care Providers . Health Professions Council of South Africa; 2006. Advanced Life Support Practitioner Protocols. [Google Scholar]
- 19.Health Professions Council of South Africa. iRegister [Internet]. 2014 [cited 2014 Nov 30]. Available from: http://isystems.hpcsa.co.za/iregister/.
- 20.Tselios M., Afilalo C. Pain relief versus patient satisfaction. Ann Emerg Med. 1996;27(4):436–438. doi: 10.1016/s0196-0644(96)70225-1. [DOI] [PubMed] [Google Scholar]
- 21.Maio R.F., Garrison H.G., Spaite D.W., Desmond J.S., Gregor M.A., Stiell I.G. Emergency medical services outcomes project (EMSOP) IV: pain measurement in out-of-hospital outcomes research. Ann Emerg Med. 2002 Aug;40(2):172–179. doi: 10.1067/mem.2002.124756. [DOI] [PubMed] [Google Scholar]
- 22.Luger T.J., Lederer W., Gassner M. IH. Acute pain is underassessed in out-of-hospital emergencies. Acad Emerg Med. 2003;10(6):627–632. doi: 10.1111/j.1553-2712.2003.tb00046.x. [DOI] [PubMed] [Google Scholar]
- 23.Guru V., Dubinsky I. The patient vs. caregiver perception of acute pain in the emergency department. J Emerg Med. 2000;18(1):7–12. doi: 10.1016/s0736-4679(99)00153-5. [DOI] [PubMed] [Google Scholar]
- 24.Lord B., Woollard M. The reliability of vital signs in estimating pain severity among adult patients treated by paramedics. Emerg Med J. 2011;28(2):147–150. doi: 10.1136/emj.2009.079384. [DOI] [PubMed] [Google Scholar]
- 25.Bossart P., Fosnocht D., Swanson E. Changes in heart rate do not correlate with changes in pain intensity in emergency department patients. J Emerg Med. 2007;32(1):19–22. doi: 10.1016/j.jemermed.2006.05.029. [DOI] [PubMed] [Google Scholar]
- 26.Division of Clinical Pharmacology Faculty of Health Sciences University of Cape Town . 9th ed. Health and Medical Publishing Group South African Medical Association; Cape Town: 2010. South African Medicines Formulary. [Google Scholar]
- 27.Ducharme J. Acute pain management in adults. In: Tintinalli J.E., Stapczynski J.S., Ma O.J., Cline D.M., Cydulka R.K., Meckler G.D., editors. Tintinalli’s emergency medicine: a comprehensive study guide. 7th ed. The McGraw-Hill Companies; New York, NY: 2011. [Google Scholar]
- 28.Bijur P.E., Kenny M.K., Gallagher E.J. Intravenous morphine at 0.1 mg/kg is not effective for controlling severe acute pain in the majority of patients. Ann Emerg Med. 2005;46(4):362–367. doi: 10.1016/j.annemergmed.2005.03.010. [DOI] [PubMed] [Google Scholar]
- 29.Birnbaum A., Esses D., Bijur P.E. Randomized double-blind placebo-controlled trial of two intravenous morphine dosages (0.10 mg/kg and 0.15 mg/kg) in emergency department patients with moderate to severe acute pain. Ann Emerg Med. 2007;49(4) doi: 10.1016/j.annemergmed.2006.06.030. [DOI] [PubMed] [Google Scholar]
- 30.Bounes V., Charpentier S., Houze-Cerfon C.-H. Is there an ideal morphine dose for prehospital treatment of severe acute pain? A randomized, double-blind comparison of 2 doses. Am J Emerg Med. 2008;26(2):148–154. doi: 10.1016/j.ajem.2007.04.020. [DOI] [PubMed] [Google Scholar]
- 31.Vincent-Lambert C., De Kock J.M. Use of morphine sulphate by South African paramedics for prehospital pain management. Pain Res Manag. 2015;20(3):141–144. doi: 10.1155/2015/507470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Berben S.A.A., Meijs T.H.J.M., van Grunsven P.M. Facilitators and barriers in pain management for trauma patients in the chain of emergency care. Injury. 2012;43(9):1397–1402. doi: 10.1016/j.injury.2011.01.029. [DOI] [PubMed] [Google Scholar]
- 33.Bounes V., Barniol C., Minville V. Predictors of pain relief and adverse events in patients receiving opioids in a prehospital setting. Am J Emerg Med. 2011;29(5):512–517. doi: 10.1016/j.ajem.2009.12.005. [DOI] [PubMed] [Google Scholar]
- 34.Iqbal M., Spaight P.A., Siriwardena A.N. Patients’ and emergency clinicians’ perceptions of improving pre-hospital pain management: a qualitative study. Emerg Med J. 2013;30(3):e18. doi: 10.1136/emermed-2012-201111. [DOI] [PubMed] [Google Scholar]
- 35.Heins J.K., Heins A., Grammas M. Disparities in analgesia and opioid prescribing practices for patients with musculoskeletal pain in the emergency department. J Emerg Nurs. 2006;32(3):219–224. doi: 10.1016/j.jen.2006.01.010. [DOI] [PubMed] [Google Scholar]
- 36.McCaul M., Grimmer K. Pre-hospital clinical practice guidelines – where are we now? Afr J Emerg Med. 2016:4–6. doi: 10.1016/j.afjem.2016.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kehlet Henrik, Dahl J.B. The value of “multimodal” or “balanced analgesia” in postoperative pain treatment. Anesth Analg. 1993;77(5):1048–1056. doi: 10.1213/00000539-199311000-00030. [DOI] [PubMed] [Google Scholar]
- 38.Galinski M., Dolveck F., Combes X. Management of severe acute pain in emergency settings: ketamine reduces morphine consumption. Am J Emerg Med. 2007;25(4):385–390. doi: 10.1016/j.ajem.2006.11.016. [DOI] [PubMed] [Google Scholar]
- 39.Jennings P.A., Cameron P., Bernard S. Morphine and ketamine is superior to morphine alone for out-of-hospital trauma analgesia: a randomized controlled trial. Ann Emerg Med. 2012;59(6):497–503. doi: 10.1016/j.annemergmed.2011.11.012. [DOI] [PubMed] [Google Scholar]
- 40.Johansson P., Kongstad P., Johansson A. The effect of combined treatment with morphine sulphate and low-dose ketamine in a prehospital setting. Scand J Trauma Resusc Emerg Med. 2009;17(1):61. doi: 10.1186/1757-7241-17-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Berben S.A., Meijs T.H.J.M., van Dongen R.T.M. Pain prevalence and pain relief in trauma patients in the Accident & Emergency department. Injury. 2008;39(5):578–585. doi: 10.1016/j.injury.2007.04.013. [DOI] [PubMed] [Google Scholar]
- 42.Holdgate A., Shepherd S.A., Huckson S. Patterns of analgesia for fractured neck of femur in Australian emergency departments: original research. Emerg Med Australas. 2010;22(1):3–8. doi: 10.1111/j.1742-6723.2009.01246.x. [DOI] [PubMed] [Google Scholar]
- 43.Minick P., Clark P.C., Dalton J.A. Long-bone fracture pain management in the emergency department. J Emerg Nurs. 2012;38(3):211–217. doi: 10.1016/j.jen.2010.11.001. [DOI] [PubMed] [Google Scholar]
- 44.Todd K.H., Ducharme J., Choiniere M. Pain in the emergency department: results of the Pain and Emergency Medicine Initiative (PEMI) multicenter study. J Pain. 2007;8(6):460–466. doi: 10.1016/j.jpain.2006.12.005. [DOI] [PubMed] [Google Scholar]
- 45.Patanwala A.E., Keim S.M., Erstad B.L. Intravenous opioids for severe acute pain in the emergency department. Ann Pharmacother. 2010;44(11):1800–1809. doi: 10.1345/aph.1P438. [DOI] [PubMed] [Google Scholar]
- 46.Frakes M.A., Lord W.R., Kociszewski C. Efficacy of fentanyl analgesia for trauma in critical care transport. Am J Emerg Med. 2006;24(3):286–289. doi: 10.1016/j.ajem.2005.11.021. [DOI] [PubMed] [Google Scholar]
- 47.Buckenmaier C.C., Rupprecht C., McKnight G. Pain following battlefield injury and evacuation: a survey of 110 casualties from the wars in Iraq and Afghanistan. Pain Med. 2009;10(8):1487–1496. doi: 10.1111/j.1526-4637.2009.00731.x. [DOI] [PubMed] [Google Scholar]
- 48.Meine T.J., Roe M.T., Chen A.Y. Association of intravenous morphine use and outcomes in acute coronary syndromes: results from the CRUSADE Quality Improvement Initiative. Am Heart J Durham: Mosby. 2005;149(6):1043–1049. doi: 10.1016/j.ahj.2005.02.010. [DOI] [PubMed] [Google Scholar]
- 49.O’Connor R.E., Al Ali A.S., Brady W.J. Part 9: acute coronary syndromes. Circulation. 2015;132(18 Suppl 2):S483–S500. doi: 10.1161/CIR.0000000000000263. [DOI] [PubMed] [Google Scholar]
- 50.Gilbert E.H., Lowenstein S.R., Koziol-McLain J. Chart reviews in emergency medicine research: where are the methods? Ann Emerg Med. 1996;27(3):305–308. doi: 10.1016/s0196-0644(96)70264-0. [DOI] [PubMed] [Google Scholar]