Abstract
Introduction
According to the World Health Organization (WHO), burns result in the loss of approximately 18 million disability adjusted life years (DALYs) and more than 250,000 deaths each year, more than 90% of which are in low- and middle-income countries (LMICs). The epidemiology of these injuries, especially in the WHO-defined African Region, has yet to be adequately defined.
Methods
We performed a systematic review of the literature regarding the epidemiology of thermal, chemical, and electrical burns in the WHO-defined African Region. All articles indexed in PubMed, EMBASE, Web of Science, Global Health, and the Cochrane Library databases as of October 2015 were included.
Results
The search resulted in 12,568 potential abstracts. Through multiple rounds of screening using criteria determined a priori, 81 manuscripts with hospital-based epidemiology as well as eleven manuscripts that included population-based epidemiology were identified. Although the studies varied in methodology, several trends were noted: young children appear to be at most risk; most individuals were burned at home; and hot liquids and flame are the most common aetiologies.
Discussion
While more population-based research is essential to identifying specific risk factors for targeted prevention strategies, our review identifies consistent trends for initial efforts at eliminating these often devastating and avoidable injuries.
Abstract
Introduction
Selon l'Organisation mondiale de la Santé (OMS), les brûlures résultent sur la perte d'environ 18 millions d'années de vie corrigées du facteur d'invalidité (AVCI) et sur plus de 250 000 décès chaque année, plus de 90% se produisant dans les pays à revenu faible et intermédiaire (PRFI). L'épidémiologie de ces blessures, notamment dans la région africaine de l'OMS, reste encore à définir adéquatement.
Méthodes
Nous avons procédé à une revue systématique de la documentation relative à l'épidémiologie des brûlures thermiques, chimiques et électriques dans la région africaine de l'OMS. Tous les articles indexés dans les bases de données de PubMed, EMBASE, Web of Science, Global Health et de la Cochrane Library à compter d'octobre 2015 ont été inclus.
Résultats
La recherche a produit 12 568 résumés potentiels. Par le biais de plusieurs séries de tri à l'aide de critères déterminés a priori, 81 manuscripts fournissant une épidémiologie dans le cadre hospitalier ainsi que 11 manuscripts incluant une épidémiologie basée sur la population ont été identifiés. Bien que les études variaient dans leur méthodologie, plusieurs tendances ont été observées: les jeunes enfants semblent constituer la population la plus à risque; la plupart des individus étaient brûlés à la maison; et les liquides chauds et les flammes constituent les étiologies les plus courantes.
Discussion
Si des études davantage basées sur la population sont essentielles pour identifier les facteurs de risque spécifiques en vue de stratégies de prévention ciblées, notre revue identifie des tendances constantes pour les efforts initiaux visant à éliminer ces blessures souvent dévastatrices et évitables.
African relevance
-
•
The WHO-defined African Region carries the greatest burden of disease with regard to burn injuries.
-
•
Little is known about the epidemiology of burn injuries in the African Region.
-
•
To date, no systematic review has been performed on the epidemiology of burns in the African Region.
Introduction
The World Health Organization (WHO) broadly defines a burn as an injury caused by heat (hot objects, gases, or flames), chemicals, electricity and lightning, friction, or radiation [1]. Annually, burns result in more than 7.1 million injuries, the loss of almost 18 million disability adjusted life years (DALYs) and more than 250,000 deaths worldwide. More than 90% of the burden of burn injury is borne by low- and middle-income countries (LMICs). The three WHO regions with the greatest burden of injury are the Eastern Mediterranean Region, the South East Asian Region, and the African Region, with the African Region bearing nearly two-thirds of the total burden [2]. To date, systematic reviews on the epidemiology of burn injuries have been conducted in the first two regions [3], [4], but only limited information has been gathered regarding the epidemiology of burn injury in the WHO-defined African Region [5], [6].
Several global systematic reviews of burn injuries that include the WHO-defined African Region have been completed to date, but they have often identified different epidemiological patterns and contradictory risk factors [7], [8], [9], [10], [11], [12]. For example, a review of childhood injuries in low-income countries by Bartlett in 2002 highlights burn injuries as occurring most often at home in children under four years of age, especially during cooler months in countries with seasonal variations. Bartlett also reports scalds of the upper extremities as the most common injuries and emphasizes the dangers of children’s access to appliances in the home [7]. Ahuja and Bhattacharya, however, note that perhaps children, as well as the elderly, are at less risk for burn injuries likely as a result of the joint family unit and the potential for redundant supervision. They highlight women aged 16–35 as being the most susceptible to burn injuries as a result of their use of loose clothing and their predominant roles in cooking for the family. They also emphasize flame as a common cause for injuries [8].
Furthermore, these global reviews as well as other reviews focused on more specific types of burns [13], [14], [15], [16], [17], [18], [19], [20], [21], [22], [23], [24], [25], [26], [27], have several limitations. Most are not comprehensive, few are systematic, many include high-income countries (HICs) or highlight other injury mechanisms along with burn injuries, and none have specifically focused on the WHO-defined African Region. Additionally, most include hospital-based (patients presenting to or admitted to clinics or hospitals), and not population-based, data. As Dissanaike and Rahimi mention, studies heavily based in data acquired from healthcare facilities often grossly underestimate the incidence of burn injuries as injuries that do not meet admission criteria are often not identified. Furthermore, epidemiological data from these studies is often biased as there are many factors in LMICs that determine whether or not individuals can or do seek medical care for serious injuries and medical conditions [11].
However, although limited, these reviews do help to identify epidemiological factors that are potentially important in the study of burn injuries. These factors include age, sex, socioeconomic status (SES), type of fuel and lighting sources used in the home, education, occupation, number of people in the home, potential for supervision (in paediatric burns), seasonal and temporal variation, high risk locations for burn injury (e.g. specific rooms in the home), mechanism of burn injury, extent of burn injury including total body surface area (TBSA) and burn depth, and other potential risk factors (e.g. medical co-morbidities, flammable clothing, cultural practices).
A detailed understanding of epidemiology is essential in order to take steps to prevent injuries. According to Peck et al., epidemiology and surveillance, are the key first steps in injury prevention [28]. With this goal in mind, in this paper we systematically review the epidemiological studies of burns in the WHO-defined African Region in order to more specifically and comprehensively describe these preventable injuries in the region with the greatest burden of injury.
Methods
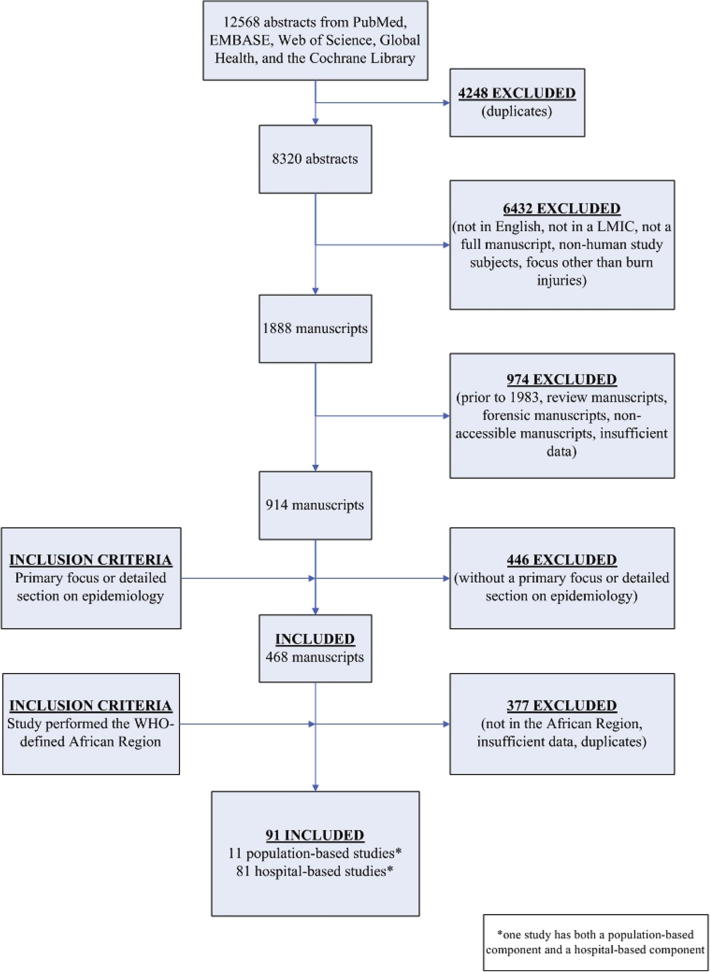
We performed a systematic review of the literature indexed in PubMed, EMBASE, Web of Science, Global Health, and the Cochrane Library databases as of October 2015. Abstracts were limited to human studies in English. The initial search had a broader scope of burn injuries in LMICs and returned 12568 abstracts, 4248 which were duplicates that were excluded prior to review. On primary review of the remaining 8320 abstracts, 6432 were excluded by two reviewers (with conflicts resolved by a third) using the following a priori exclusion criteria: non-human study subjects, language other than English, not a full manuscript (e.g. only an abstract, poster presentation, lecture, letter, or short communication), not conducted in a LMIC – as defined by the World Bank classification of countries as of June 1, 2013 [29], and a manuscript without a focus on thermal, electrical, or chemical burns, or with a focus only on burn injuries involving radiation injuries, sunburns, sulphur mustard/other chemical warfare agents/paraquat, or mass casualty incidents (MCIs). The remaining 1888 manuscripts were screened by two reviewers, using the following a priori exclusion criteria: full manuscripts not accessible, manuscripts with epidemiology of only the deceased/forensic manuscripts, manuscripts prior to 1983, other systematic reviews, and finally those without sufficient epidemiological or preventative data (i.e. ten or fewer subjects, limited detailed data). The remaining 914 manuscripts were screened with the following a priori inclusion criteria: having a primary focus on or detailed section (must include original data with or without statistical analysis – e.g. percentages, averages) on epidemiology. This resulted in 468 manuscripts. These manuscripts were then separated into regions to determine those conducted in the WHO-defined African Region resulting in 91 manuscripts – ten population-based studies, 80 hospital-based studies, and one manuscript including both a population- and a hospital-based component to the study (Fig. 1).
Fig. 1.
Flowchart of the systematic review process.
All screening and data extraction was completed using Microsoft Excel. Ethics approval was not required by the study facility because this study reviewed existing literature.
Results
Population-based studies
The search resulted in eleven population-based studies: two from Ethiopia, five from Ghana, and one each from Kenya, Sierra Leone, South Africa, and Tanzania. These studies are listed in Table 1 [30], [31], [32], [33], [34], [35], [36], [37], [38], [39], [40]. A summary of the major findings from these studies is reported in Table 2.
Table 1.
Population-based studies by country, first author, journal, and year.
| Country | First Author | Journal | Year |
|---|---|---|---|
| Ethiopia | Nega | Ethiopian Journal of Health Development | 2002 |
| Ethiopia | Courtright | Journal of Epidemiology and Community Health | 1993 |
| Ghana | Forjuoh | Burns | 1995 |
| Ghana | Forjuoh | Journal of Epidemiology and Community Health | 1995 |
| Ghana | Forjuoh | Child Abuse and Neglect | 1995 |
| Ghana | Forjuoh | Burns | 1996 |
| Kenya | Wong | Burns | 2014 |
| Sierra Leone | Wong | Burns | 2014 |
| South Africa | Barnes | African Safety Promotion | 2004 |
| Tanzania | Roman | International Journal of Injury Control and Safety Promotion | 2012 |
Table 2.
Summary of findings in the population-based studies by epidemiological factor.
| Epidemiological Factor | Critical Finding |
|---|---|
| Age | Children (up to five years old) |
| Sex | Male children; female adults |
| Most Common Type of Injury | Scalds |
| Areas Affected | Extremities |
| Location of Injury | Home |
| Socio-economic Factors | No clear trend in place of residence (rural vs. urban), occupation, education or literacy, income, number of children/adults in family/per room, birth order, size of kitchen, housing quality index, hours spent away by the mother |
| Risk Factors |
|
|
The majority of the studies note that children are most at risk for burn injuries [30], [31], [32], [33], [34], [37], [39], [40]. Most studies highlight younger males and older females as most at risk for burn injuries [30], [31], [32], [33], [34], [37], [39], although some showed no clear differences between the sexes [38], [40]. Scald and contact injuries appear to be the most common [30], [31], [32], [33], [34], [38] often as a result of bathing or cooking, however flame injuries as well as electrical and chemical burns are common in some areas [40]. In the studies describing the location of the burn injuries, the extremities – particularly the upper extremities – are the most common locations for suffering burn injuries, especially in scald and contact burns. The lower extremities are more commonly affected in flame injuries [33], [34], [38], [40]. Many studies highlight the home, particularly the kitchen, as the most common location of sustaining burn injuries [30], [31], [32], [33], [34].
It is unclear how the number of persons per household and the composition of those persons contribute to risk of burn injury. Some studies suggest that having four or more persons per room along with having five or fewer adults in the household results in increased risk [31], [39]. Furthermore, one study suggested that burn injuries are more common in high income households among employed parents [31]. This may be due to less supervision (parents out of the house working) or due to having more appliances in the home. Other studies, however, found no significant differences in risk of burn injuries in relation to hours spent away by the mother or number of children in the house [33], [38]. Additionally, although two studies suggest an increased risk among rural households [33], [34], other studies found no association between place of residence (rural vs. urban), as well as occupation, income, education or literacy, size of kitchen, or housing quality index [38], [39], [40].
In one study, significant risk factors for burn injury include impairment (odds ratio 6.6), burn in a sibling (odds ratio 1.7), sibling death from burn (odds ratio 4.4), and storage of flammable substance in the home (odds ratio 1.5) [34]. Non-significant risk factors include type of appliance/fuel, duration of daily burning (if flame used), and birth order [39], [40]. Children playing and adults cooking are the most common scenarios resulting in burn injuries, and at-risk times include just after morning or evening meals [30], [31], [32], [33], [34].
Two sub-populations are also highlighted in additional studies – those with intentional burn injuries and children with a history of more than one burn injury. In the former population, the majority of victims are 24–35 months old, male, and living in rural areas. The majority involve 1–2% TBSA and the trunk/back rather than the extremities. Intentional injuries more often occur outside the home and are more likely to be caused by flame [35]. In the latter group, there is no difference in demographics between repeat victims and those with history of a single burn injury with the following exceptions: those injured more than once more often suffer scald and flame burns and there are more double parent households and more households with televisions among those with more than one injury, and, among children with a single injury, there are more households with stored flammable substances and more mothers away more than eight hours [36].
Hospital-based studies
The majority of the studies (81) found in this review are based on epidemiological data on patients presenting to or admitted to health care facilities (Table 3, Table 4) [42], [43], [44], [45], [46], [47], [48], [49], [50], [51], [52], [53], [54], [55], [56], [57], [58], [59], [60], [61], [62], [63], [64], [65], [66], [67], [68], [69], [70], [71], [72], [73], [74], [75], [76], [77], [78], [79], [80], [81], [82], [83], [84], [85], [86], [87], [88], [89], [90], [91], [92], [93], [94], [95], [96], [97], [98], [99], [100], [101], [102], [103], [104], [105], [106], [107]. While comparisons are limited by differences in admission criteria and in descriptions of burn injuries and of paediatric populations, these data provide information about which patients with burn injuries present for medical care.
Table 3.
Summary of findings in the hospital-based studies by epidemiological factor.
| Epidemiological Factor | Critical Finding |
|---|---|
| Age | Children (up to 15 years of age) |
| Sex | Trend toward male children, female adults |
| Most Common Type of Injury | Scald (children), flame (adults) |
| Areas Affected | Upper extremities, trunk |
| Extent of Injury | Most ⩽20%; partial thickness |
| Location of Injury | Home (kitchen) |
| Socio-economic Factors |
|
| |
| Other Common Themes |
|
| |
| |
|
Table 4.
Summary of findings by studies on special cases of burn injury.
| Type of Injury | Critical Findings |
|---|---|
| Stove Burns |
|
| |
| |
| Bed Net Burns |
|
| |
| |
| Intentional and Unintentional Chemical Burns |
|
| |
| |
| Intentional Burns |
|
| |
| |
| |
| Electrical Burns |
|
| |
| |
| Occupational Burns |
|
| |
|
SES, socio-economic status; TBSA, total body surface area.
Studies show that children up to the age of 15 years are most at risk, with those less than five at highest risk [31], [42], [43], [44], [45], [46], [47], [48], [49], [50], [51], [52], [53], [54], [55], [56], [57], [58], [59], [60], [61], [62], [63], [64], [65], [66], [67], [68], [69], [70], [71], [72], [73], [74], [75], [76], [77], [78], [79], [80], [81], [82], [83], [84], [85], [86], [87], [88], [89], [90], [91], [92], [93], [94], [95], [96], [97], [98], [99]. Male children and female adults (usually between 20 and 30 years of age) are at risk in studies of children and of all age groups [31], [42], [43], [44], [45], [46], [47], [48], [49], [50], [51], [52], [53], [55], [56], [57], [58], [59], [60], [61], [62], [64], [65], [66], [67], [68], [69], [70], [71], [73], [74], [75], [77], [78], [79], [80], [81], [82], [83], [84], [85], [86], [87], [89], [90], [91], [92], [96], [98]. Among studies with adults only, men are found to be more at risk especially between 20 and 30 years of age [100], [102], [103], [105], [106]. Scald injuries (usually in children) and flame injuries (usually in adults) are the most common types of injuries [41], [42], [43], [44], [45], [46], [47], [48], [49], [50], [51], [52], [53], [54], [55], [56], [57], [58], [59], [60], [61], [62], [63], [64], [65], [66], [67], [68], [69], [70], [71], [72], [73], [74], [75], [76], [77], [78], [79], [80], [81], [82], [83], [84], [85], [86], [87], [88], [89], [90], [91], [92], [93], [94], [95], [96], [97], [98], [99], [101], [102], [103], [104], [105], [106], [107]. The most common areas affected are the extremities followed by the trunk [41], [52], [53], [54], [55], [56], [57], [58], [59], [60], [61], [67], [68], [69], [70], [71], [72], [73], [75], [76], [77], [78], [79], [80], [81], [82], [83], [84], [85], [86], [87], [88], [89], [90], [91], [92], [93], [94], [95], [96], [97], [98], [99], [102], [103], [104], [105], [106]. Most injuries are partial thickness with ⩽20% total body surface area (TBSA). Burn severity in terms of TBSA tend to increase with age [42], [43], [44], [45], [46], [62], [63], [64], [65], [66], [67]. Most burn injuries are sustained in the home, particularly the kitchen [42], [43], [44], [45], [46], [67], [72], [87], [88], [89], [90], [91], [92], [93], [94], [95], [96], [97], [98].
Several studies note specific socio-economic factors common to admitted patients. Limited education, unemployment, having more than six persons in the home and/or single room house, being from a rural area, and/or having a ‘low income’ are common among admitted patients [67], [71], [74], [75], [76], [77], [78], [79], [80], [81], [82], [83], [84], [85], [86], [87], [88], [89], [90], [91], [92], [93], [94], [95], [96], [97], [98], [99].
Chemical and electrical burns as well as intentional burns do occur and are among those admitted [41], [42], [43], [44], [52], [53], [54], [55], [56], [57], [58], [59], [60], [61], [62], [63], [64], [65], [66], [69], [70], [75], [76], [77], [78], [79], [80], [81], [82], [83], [84], [85], [86], [87], [88], [89], [90], [91], [92], [93], [94], [95], [96], [97], [98], [100], [102], [103], [104], [105], [106], [107]. Many burn injuries occur during the cool/dry/windy months [52], [53], [54], [55], [56], [57], [58], [59], [60], [61], [62], [63], [64], [65], [66], [68], [75], [76], [77], [78], [79], [80], [81], [82], [83], [84], [85], [86], [100]. Epilepsy is a common contributing factor to burn injuries [47], [50], [62], [63], [64], [65], [66], [68], [74], [100], [107].
Special cases
There are several studies involving specific burn types. They involve chemical and electrical burns, ingestions, intentional burns, burns from bed nets, burns from stove explosions, and occupational injuries and span six countries: Ghana, Kenya, Nigeria, South Africa, Uganda, and Zimbabwe (Table 4).
Ombati et al. describe risk factors for kerosene stove explosion burns in Kenya. They report women of low SES between the ages of 20 and 39 as those most commonly injured by stove explosions with the majority being injured during cooking or refilling of the stoves [108].
Kalanzi et al. report on burn injuries from bed nets presenting to Mulago National Referral Hospital in Uganda. A bed net burn is one that occurs as a result of when a net that is hung to protect an individual from mosquitoes when he or she is sleeping catches fire as a result of coming into contact with hot objects or flames that are kept in and around the sleeping area for warmth and/or light. Bed net burns are particularly serious as the individual is most often asleep under the net at the time of the injury. Most of those admitted to the hospital with these injuries are one year old or less, are male, and suffer >20% TBSA [109].
Several studies report intentional chemical injuries. The majority of the incidents are a result of domestic disputes, robbery, or assault involving injuries to the head and neck, particularly the eyes, with the majority of those assaulted being male and 30–40 years of age [110], [111], [112]. Thomas et al. and Adedeji et al. describe injuries caused by chemical ingestions. The majority of those admitted are men with a mean age of 23 years. Many are of low SES. Some note accidental ingestions – mostly of acids; most however are intentional ingestions of alkalis in suicide attempts [113], [114].
Datubo-Brown describes the characteristics of intentional burns that present to Port Harcourt Teaching Hospital in Nigeria. The majority of those affected are male and are a result of attempts to treat another ailment. The rest are inflicted as punishment or in the course of attempted robbery. The most common aetiology is flame, followed by chemicals and hot liquids [115].
In a study by Godwin and Hudson, men assaulted by their partners are described. The mean age is 37 years. Injuries result from hot water, stove or fish oil, and paraffin and flame in decreasing frequency. The average TBSA is 30% with the head and neck and upper extremities most commonly injured [116].
Mzezewa et al. describe patients admitted for intentional injuries sustained as a result of suicide attempts. The majority of the patients are female and are 22–30 years of age who use paraffin for self-harm, with attempts mostly occurring in the evenings and resulting in an average of 60% TBSA. The most common cause for these actions are relationship difficulties [117].
Two studies report that among electrical injuries, the majority of patients affected are male between 20 and 40 years of age with injuries that occur from high voltages to the upper extremities while at work [118], [119].
Finally, Muguti and Doolabh describe occupational burn injuries sustained by males in Zimbabwe. Of these workers, the majority are skilled workers 30–40 years of age. The mean TBSA is 21% with injuries to the face, hands, and feet in decreasing frequency. The majority are flame burns, followed by scalds, electrical burns, and chemical burns in decreasing frequency [120].
Discussion
Burn injuries are common throughout the world, with the WHO-defined African Region bearing the majority of the burden of the global morbidity and mortality. Unfortunately, little is known about the epidemiology of these injuries in this region. The purpose of this systematic review was to highlight trends from epidemiological studies for the purpose of stimulating further population-based surveillance and of informing preventative efforts. While each country and region are unique, several consistent findings from the eleven population-based studies and the 81 hospital-based studies, representing 13 of the 47 countries in the WHO-defined African Region, are reported in this review.
The findings presented here are similar to those in previous reviews, however, unlike previous studies suggest, there does not seem to be any clear association between certain socio-economic factors such as place of residence, occupation, income, education/literacy, number of children, number of adults, size of kitchen, types of fuels/appliances in the home [5], [6], [7], [8], [9], [10], [11], [12]. This is likely a result of a broader scope of this systematic review as well as the heterogeneous definitions of socioeconomic factors used in the various studies. Finally, it is important to note that electrical and chemical burns, including ingestions, while rare, do occur; intentional burns (either homicidal or suicidal) are a substantial problem in certain areas; and co-morbidities such as epilepsy are likely contributors to burn injuries. These special topics have not always been highlighted in previous reviews.
In hospital-based studies, we see many of the same trends as in the population-based studies, however, there are more findings that are consistent with previous reviews in LMICs as well as in reviews of injuries in HICs, for example, most studies note a male predominance among those admitted [6], [121]. As mentioned, low SES and unemployment are also often reported among families of patients admitted as has also been highlighted in previous studies [5], [6], [7], [8], [9], [10], [11], [12]. Children who are admitted have most commonly suffered a scald; adults most commonly suffered flame burns; most reviews note this, however there is not always the same distribution by age group [5], [6], [7], [8], [9], [10], [11], [12]. The TBSA of those admitted is often 20% or less (often higher in developed countries), perhaps because more severe injuries are more likely to be fatal in LMICs [121]. Special cases of burn injury, such as those caused by epilepsy, intentional burn injuries (including therapeutic burns and assaults), chemical and electrical burns, and injuries occurring at work (especially among men) are often among those admitted as well. The identification of these special burns is not only important for training health care providers in these unique situations (the majority of which are not as common elsewhere with the exception of work- or industry-related burns which are much more common in HICs), but it is also imperative in directing specific and efficient preventative efforts [121], [122], [123].
It is important to remember, however, that these conclusions are made on the basis of both population-based and hospital-based studies with variable methodology and inclusion criteria and are therefore more qualitative than quantitative. There are subtle characteristics of those affected by burn injury as well as risk factors for burn injury that vary among countries and even among communities within countries that are not yet fully characterised in the literature, and thus, by this review. Further limitations of this review include the exclusion of studies not reported in English; the majority of the literature highlighted here is often more than 10–15 years old; the varied definitions of age groups, of burn injuries, and of admission criteria to hospitals and burn units; and the heterogeneity of data in the included studies precludes meta-analysis. Overall, however, this review represents a large sample that is unique among literature reviews on burn injuries, and it provides an extensive overview of the epidemiology in a region that has not been previously well-highlighted.
In areas with limited resources, it is important for each community to identify the population at risk for burn injury and the most unique factors that may contribute to it. As a result, specific, and therefore more effective, preventative programs may be put into effect. It is imperative that future studies, particularly population-based studies in the WHO-defined African Region with consistent definitions of epidemiological factors continue to more comprehensively describe the epidemiology of and to more completely capture the incidence of burn injuries in this heavily burdened area.
Burn injuries are common throughout the world, with the WHO-defined African Region bearing a large burden of injury. Although specific trends have been noted in this review, primary studies are few and are limited by varying definitions of age groups, burn injuries, and hospital or burn unit admission criteria. While the data are limited and would benefit from more study, the consistent epidemiologic trends noted here can inform education and prevention strategies to hopefully begin to reduce the incidence, morbidity, and mortality from burn injuries in the WHO-defined African Region.
Conflicts of interest
Gabrielle Jacquet is an associate editor for the African Journal of Emergency Medicine. Dr Jacquet was not involved in the editing or peer review process for this paper. The authors declare no other conflict of interest.
Authors' contributions
MR, JS, CE, SS, PV, KB, LC and GJ screened the papers. MR, JS, SS, LC extracted the data. MR analyzed the data. MR wrote the paper. All authors revised the manuscript and approved the final version of the manuscript.
Acknowledgements
We thank Kathleen Shea (Department of Emergency Medicine, Boston Medical Center) for obtaining manuscripts and Katie Lobner (Welch Medical Library, Johns Hopkins Medical Institutions) for constructing and conducting the initial search.
Footnotes
Peer review under responsibility of African Federation for Emergency Medicine.
References
- 1.ICD-10: World Health Organization. http://apps.who.int/classifications/icd10/browse/2010/en (accessed March 1, 2015).
- 2.WHO Health Estimates 2014 Summary Tables: Deaths and Global Burden of Disease. http://www.who.int/healthinfo/global_burden_disease/en/ (accessed March 1, 2015).
- 3.Othman N., Kendrick D. Epidemiology of burn injuries in the East Mediterranean Region: a systematic review. BMC Public Health. 2010 doi: 10.1186/1471-2458-10-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Golshan A., Patel C., Hyder A.A. A systematic review of the epidemiology of unintentional burn injuries in South Asia. J Public Health (Bangkok) 2013;35:1–13. doi: 10.1093/pubmed/fds102. [DOI] [PubMed] [Google Scholar]
- 5.Hyder A, Kashyap K, Fishman S, Wali S. Review of childhood burn injuries in sub-Saharan Africa: a forgotten public health challenge. African Saf Promot; 2008.
- 6.Nthumba P. Burns in sub-Saharan Africa: a review. Burns. 2016;42:258–266. doi: 10.1016/j.burns.2015.04.006. [DOI] [PubMed] [Google Scholar]
- 7.Bartlett S. The problem of children’s injuries in low-income countries: a review. Health Policy Plan. 2002;17:1–13. doi: 10.1093/heapol/17.1.1. [DOI] [PubMed] [Google Scholar]
- 8.Ahuja R., Bhattacharya S. ABC of burns: burns in the developing world and burn disasters. BMJ. 2004;329:447–449. doi: 10.1136/bmj.329.7463.447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Forjuoh S.N. Burns in low- and middle-income countries: a review of available literature on descriptive epidemiology, risk factors, treatment, and prevention. Burns. 2006;32:529–537. doi: 10.1016/j.burns.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 10.Atiyeh B., Masellis A., Conte C. Optimizing burn treatment in developing low-and middle-income countries with limited health care resources (part 1) Ann Burns Fire Disasters. 2009;22:121–125. [PMC free article] [PubMed] [Google Scholar]
- 11.Dissanaike S., Rahimi M. Epidemiology of burn injuries: highlighting cultural and socio-demographic aspects. Int Rev Psychiatry. 2009;21:505–511. doi: 10.3109/09540260903340865. [DOI] [PubMed] [Google Scholar]
- 12.Peck M.D. Epidemiology of burns throughout the world. Part I: distribution and risk factors. Burns. 2011;37:1087–1100. doi: 10.1016/j.burns.2011.06.005. [DOI] [PubMed] [Google Scholar]
- 13.Laloë V. Patterns of deliberate self-burning in various parts of the world. A review. Burns. 2004;30:207–215. doi: 10.1016/j.burns.2003.10.018. [DOI] [PubMed] [Google Scholar]
- 14.Mannan A., Ghani S., Clarke A., Butler P.E.M. Cases of chemical assault worldwide: a literature review. Burns. 2007;33:149–154. doi: 10.1016/j.burns.2006.05.002. [DOI] [PubMed] [Google Scholar]
- 15.Milton R., Mathieu L., Hall A.H., Maibach H.I. Chemical assault and skin/eye burns: two representative cases, report from the Acid Survivors Foundation, and literature review. Burns. 2010;36:924–932. doi: 10.1016/j.burns.2009.10.020. [DOI] [PubMed] [Google Scholar]
- 16.Peck M.D. Epidemiology of burns throughout the world part II: intentional burns in adults. Burns. 2012;38:630–637. doi: 10.1016/j.burns.2011.12.028. [DOI] [PubMed] [Google Scholar]
- 17.Peck MD, Kruger GE, Merwe AE Van Der, Godakumbura W, Ahuja RB. Burns and fires from non-electric domestic appliances in low and middle income countries Part I. The scope of the problem 2008;34:303–11. [DOI] [PubMed]
- 18.Sadeghi-Bazargani H., Mohammadi R. Epidemiology of burns in Iran during the last decade (2000–2010): review of literature and methodological considerations. Burns. 2012;38:319–329. doi: 10.1016/j.burns.2011.09.025. [DOI] [PubMed] [Google Scholar]
- 19.Thanni L. Epidemiology of injuries in Nigeria – a systematic review of mortality and aetiology. Prehosp Disaster Med. 2011;26:293–298. doi: 10.1017/S1049023X11006546. [DOI] [PubMed] [Google Scholar]
- 20.Peltzer K. Injury and social determinants among in-school adolescents in six African countries. Inj Prev. 2008;14:381–388. doi: 10.1136/ip.2008.018598. [DOI] [PubMed] [Google Scholar]
- 21.Lau Y.S. An insight into burns in a developing country: a Sri Lankan experience. Public Health. 2006;120:958–965. doi: 10.1016/j.puhe.2006.05.016. [DOI] [PubMed] [Google Scholar]
- 22.Oladele AO, Olabanji JK. Burns in Nigeria: a Review 2013;23:120–7. [PMC free article] [PubMed]
- 23.Outwater A.H., Ismail H., Mgalilwa L., Justin Temu M., Mbembati N.A. Burns in Tanzania: morbidity and mortality, causes and risk factors: a review. Int J Burns Trauma. 2013;3:18–29. [PMC free article] [PubMed] [Google Scholar]
- 24.Kai-Yang L., Zhao-Fan X., Luo-Man Z., Yi-Tao J., Tao T., Wei W. Epidemiology of paediatric burns requiring hospitalization in China: a literature review of retrospective studies. Pediatrics. 2008;122:132–142. doi: 10.1542/peds.2007-1567. [DOI] [PubMed] [Google Scholar]
- 25.Hyder A.A., Sugerman D.E., Puvanachandra P., Razzak J., El- H., Isaza A. Bulletin of the World Health Organization Global childhood unintentional injury surveillance in four cities in developing countries: a pilot study. Bull World Health Organ. 2009 doi: 10.2471/BLT.08.055798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mutto M., Lett R., Lawoko S., Nansamba C., Svanstrom L. Intentional injuries among Ugandan youth: a trauma registry analysis. Inj Prev. 2010;16:333–336. doi: 10.1136/ip.2008.020495. [DOI] [PubMed] [Google Scholar]
- 27.Dale E.L., Mueller M.A., Wang L, Fogerty MD, Guy JS, Nthumba PM. Epidemiology of operative burns at Kijabe Hospital from, To 2010: pilot study of a web-based tool for creation of the Kenya Burn Repository. Burns. 2006;2013(39):788–795. doi: 10.1016/j.burns.2012.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Peck M.D., Kruger G.E., van der Merwe A.E., Godakumbura W., Oen I.M.M., Swart D. Burns and injuries from non-electric-appliance fires in low- and middle-income countries Part II. A strategy for intervention using the Haddon Matrix. Burns. 2008;34:312–319. doi: 10.1016/j.burns.2007.08.009. [DOI] [PubMed] [Google Scholar]
- 29.World Bank Classification of Countries. http://data.worldbank.org/about/country-classifications/country-and-lending-groups (accessed June 1, 2013).
- 30.Nega KE, Lindtjørn B. Epidemiology of burn injuries in Mekele Town, Northern Ethiopia: a community based study. Ethiop J Heal Dev 2002;16.
- 31.Courtright P., Haile D., Kohls E. The epidemiology of burns in rural Ethiopia. J Epidemiol Community Health. 1993;47:19–22. doi: 10.1136/jech.47.1.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Forjuoh S.N., Keyl P.M., Diener-West M., Smith G.S., Guyer B. Prevalence and age-specific incidence of burns in Ghanaian children. J Trop Pediatr. 1995;41:273–277. doi: 10.1093/tropej/41.5.273. [DOI] [PubMed] [Google Scholar]
- 33.Forjuoh S.N., Guyer B., Smith G.S. Childhood burns in Ghana: epidemiological characteristics and home-based treatment. Burns. 1995;21:24–28. doi: 10.1016/0305-4179(95)90776-v. [DOI] [PubMed] [Google Scholar]
- 34.Forjuoh S.N., Guyer B., Strobino D.M., Keyl P.M., Diener-west M., Smith G.S. Risk factors for childhood burns: a case-control study of Ghanaian children. J Epidemiol Community Health. 1995:189–193. doi: 10.1136/jech.49.2.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Forjuoh S.N. Pattern of intentional burns to children in Ghana. Child Abuse Negl. 1995;19:837–841. doi: 10.1016/0145-2134(95)00041-6. [DOI] [PubMed] [Google Scholar]
- 36.Forjuoh S.N. Burn repetitions in Ghanaian children: prevalence, epidemiological characteristics and socioenvironmental factors. Burns. 1996;22:539–542. doi: 10.1016/0305-4179(96)00034-4. [DOI] [PubMed] [Google Scholar]
- 37.Wong J.M., Nyachieo D.O., Benzekri N.A., Cosmas L., Ondari D., Yekta S. Sustained high incidence of injuries from burns in a densely populated urban slum in Kenya: an emerging public health priority. Burns. 2014;40:1194–1200. doi: 10.1016/j.burns.2013.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wong E.G., Groen R.S., Kamara T.B., Stewart K., Cassidy L.D., Samai M. Burns in Sierra Leone: a population-based assessment. Burns. 2014;40:1748–1753. doi: 10.1016/j.burns.2014.03.007. [DOI] [PubMed] [Google Scholar]
- 39.Barnes B., Moiloa K. Domestic energy use, time activity patterns and risk of burns amongst children less than five years of age in rural South Africa: an exploratory study. Afr Saf Promot. 2004;2:28–34. [Google Scholar]
- 40.Roman I.M., Lewis E.R., Kigwangalla H.A., Wilson M.L. Child burn injury in Dar es Salaam, Tanzania: results from a community survey. Int J Inj Contr Saf Promot. 2012;19:135–139. doi: 10.1080/17457300.2011.628753. [DOI] [PubMed] [Google Scholar]
- 41.Mulat T., Salemark L. Descriptions of patients admitted to a burn unit of Yekatit 12 Hospital, Addis Ababa, Ethiopia. Ethiop Med J. 2006;44:369–375. [PubMed] [Google Scholar]
- 42.Agbenorku P., Edusei A., Ankomah J. Epidemiological study of burns in Komfo Anokye Teaching Hospital, 2006–2009. Burns. 2011;37:1259–1264. doi: 10.1016/j.burns.2011.04.014. [DOI] [PubMed] [Google Scholar]
- 43.Agbenorku P., Akpaloo J., Yalley D., Appiah A. A new era in the management of burns trauma in kumasi, ghana. Ann Burns Fire Disasters. 2010;23:59–66. [PMC free article] [PubMed] [Google Scholar]
- 44.Brusselaers N., Agbenorku P., Hoyte-Williams P.E. Assessment of mortality prediction models in a Ghanaian burn population. Burns. 2013;39:997–1003. doi: 10.1016/j.burns.2012.10.023. [DOI] [PubMed] [Google Scholar]
- 45.Otteni C.R., Saruni S.I., Duron V.P., Hedges J.P., White R.E. Baseline assessment of inpatient burn care at Tenwek Hospital, Bomet, Kenya. World J Surg. 2013;37:1530–1535. doi: 10.1007/s00268-013-2045-2. [DOI] [PubMed] [Google Scholar]
- 46.Ndiritu S., Ngumi Z., Nyaim O. Burns: the epidemiological pattern, risk and safety awareness at Kenyatta National Hospital, Nairobi. East Afr Med J. 2006;83:455–460. doi: 10.4314/eamj.v83i8.9462. [DOI] [PubMed] [Google Scholar]
- 47.Samuel J., Campbell E., Mjuweni S., Muyco A., Cairns B., Charles A. The epidemiology, management, outcomes and areas for improvement of burn care in Central Malawi: an observational study. J Int Med Res. 2011;39:873–879. doi: 10.1177/147323001103900321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gallaher J.R., Mjuweni S., Shah M., Cairns B.A., Charles A.G. Timing of early excision and grafting following burn in sub-Saharan Africa. Burns. 2015;41:1353–1359. doi: 10.1016/j.burns.2015.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tyson A.F., Boschini L.P., Kiser M.M., Samuel J.C., Mjuweni S.N., Cairns B.A. Survival after burn in a sub-Saharan burn unit: challenges and opportunities. Burns. 2013;39:1619–1625. doi: 10.1016/j.burns.2013.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Boschini L.P., Tyson A.F., Samuel J.C., Kendig C.E., Mjuweni S., Varela C. The role of seizure disorders in burn injury and outcome in sub-Saharan Africa. J Burn Care Res. 2014;35:406–412. doi: 10.1097/BCR.0000000000000026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Komolafe O., James J., Makoka M., Kalongeolera L. Epidemiology and mortality of burns at the Queen Elizabeth Central Hospital Blantyre, Malawi. Cent Afr J Med. 2003;49:130–134. [PubMed] [Google Scholar]
- 52.Jiburum B.C. Burn injuries in Enugu. Nigeria. 2005;7:271–273. [Google Scholar]
- 53.Kalayi G. Burn injuries in Zaria: a one year prospective study. East Afr Med J. 1994;71:317–322. [PubMed] [Google Scholar]
- 54.Datubo-Brown D., Kejeh B. Burn injuries in Port Harcourt, Nigeria. Burns. 1989;15:152–154. doi: 10.1016/0305-4179(89)90170-8. [DOI] [PubMed] [Google Scholar]
- 55.Nnabuko R.E.E., Ogbonnaya I.S., Otene C.I., Ogbonna U., Amanari O.C., Opara K.O. Burn injuries in Enugu, Nigeria – aetiology and prevention. A six-year retrospective review, December 2005) Ann Burns Fire Disasters. January 2000;2009(22):40–43. [PMC free article] [PubMed] [Google Scholar]
- 56.Olaitan P., Fadiora S., Agodirin O. Burn injuries in a young Nigerian teaching hospital. Ann Burn Fire Disasters. 2007;20:59–61. [PMC free article] [PubMed] [Google Scholar]
- 57.Onuba O., Udoidiok E. The problems and prevention of burns in developing countries. Burn Incl Therm Inj. 1987;13:382–385. doi: 10.1016/0305-4179(87)90128-8. [DOI] [PubMed] [Google Scholar]
- 58.Adesunkanmi K., Oyelami O. The pattern and outcome of burn injuries at Wesley Guild Hospital, Ilesha, Nigeria: a review of 156 cases. J Trop Med Hyg. 1994;97:108–112. [PubMed] [Google Scholar]
- 59.Kalayi G. Mortality from burns in Zaria: an experience in a developing economy. East Afr Med J. 2006;83:461–464. doi: 10.4314/eamj.v83i8.9459. [DOI] [PubMed] [Google Scholar]
- 60.Grange A.O., Akinsulie A.O., Sowemimo G.O. Flame burns disasters from kerosene appliance explosions in Lagos, Nigeria. Burns Incl Therm Inj. 1988;14:147–150. doi: 10.1016/0305-4179(88)90223-9. [DOI] [PubMed] [Google Scholar]
- 61.Dongo A.E., Irekpita E.E., Oseghale L.O., Ogbebor C.E., Iyamu C.E., Onuminya J.E. A five-year review of burn injuries in Irrua. BMC Health Serv Res. 2007;7:171. doi: 10.1186/1472-6963-7-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Scheven D., Barker P., Govindasamy J. Burns in rural Kwa-Zulu Natal: Epidemiology and the need for community health education. Burns. 2012;38:1224–1230. doi: 10.1016/j.burns.2012.04.001. [DOI] [PubMed] [Google Scholar]
- 63.Allorto N.L., Oosthuizen G.V., Clarke D.L., Muckart D.J. The spectrum and outcome of burns at a regional hospital in South Africa. Burns. 2009;35:1004–1008. doi: 10.1016/j.burns.2009.01.004. [DOI] [PubMed] [Google Scholar]
- 64.Fiandeiro D, Chb MB, Sa F, Sa DEC, Sa DA, Govindsamy J, et al. Prehospital cooling of severe burns: Experience of the Emergency Department at Edendale Hospital, KwaZulu-Natal, South Africa 2015;105:457–60. [DOI] [PubMed]
- 65.Den Hollander D., Albert M., Strand A., Hardcastle T.C. Epidemiology and referral patterns of burns admitted to the Burns Centre at Inkosi Albert Luthuli Central Hospital, Durban. Burns. 2014;40:1201–1208. doi: 10.1016/j.burns.2013.12.018. [DOI] [PubMed] [Google Scholar]
- 66.Gevaart-Durkin A., Swart D., Chowdhury Z. A study of energy-related injuries from hospital admissions among children and adults in South Africa. Burns. 2014;40:1209–1218. doi: 10.1016/j.burns.2013.12.014. [DOI] [PubMed] [Google Scholar]
- 67.Ringo Y., Chilonga K. Burns at KCMC: epidemiology, presentation, management and treatment outcome. Burns. 2014;40:1024–1029. doi: 10.1016/j.burns.2013.10.019. [DOI] [PubMed] [Google Scholar]
- 68.Edwards D., Heard J., Latenser B., Quinn K.Y., van Bruggen J., Jovic G. Burn injuries in eastern Zambia: impact of multidisciplinary teaching teams. J Burn Care Res. 2009;32:31–38. doi: 10.1097/BCR.0b013e318204b36a. [DOI] [PubMed] [Google Scholar]
- 69.Mzezewa S., Jonsson K., Aberg M., Salemark L. A prospective study on the epidemiology of burns in patients admitted to the Harare burn units. Burns. 1999;25:499–504. doi: 10.1016/s0305-4179(99)00041-8. [DOI] [PubMed] [Google Scholar]
- 70.Muguti G., Doolabh D., Chakanyuka C., Flemin A. A review of burns treated over a one-year period at Mpilo Central Hospital, Zimbabwe. J R Coll Surg Edinb. 1994;39:214–217. [PubMed] [Google Scholar]
- 71.Daniel E., Yoo M. Survey of burn admissions to the Ethio-Swedish Children’s Hospital. Ethiop Med J. 1990;28:163–168. [PubMed] [Google Scholar]
- 72.Mutiso V., Khainga S., Muoki A., Kimeu M. Epidemiology of burns in patients aged 0–13 years at a paediatric hospital in Kenya. East Cent African J Surg. 2014;19:12–22. [PubMed] [Google Scholar]
- 73.Shonubi A. Thermal injuries in under-4-year-old children; the Lesotho experience. Afr J Med Med Sci. 2005;34:77–80. [PubMed] [Google Scholar]
- 74.Karan A., Amado V., Vitorino P., Kulber D., Taela A. Evaluating the socioeconomic and cultural factors associated with paediatric burn injuries in Maputo, Mozambique. Pediatr Surg Int. 2015;31:1035–1040. doi: 10.1007/s00383-015-3761-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Mabogunje O., Khwaja M., Lawrie J. Childhood burns in Zaria, Nigeria. Burns. 1987;13:298–304. doi: 10.1016/0305-4179(87)90050-7. [DOI] [PubMed] [Google Scholar]
- 76.Afiomah U., Oduwole O., Renner J. The impact of housing in paediatric burns cases: a review of health implication of habitat in centre families in Lagos. Nig Q J Hosp Med. 2002;12:52–54. [Google Scholar]
- 77.Okoro P.E., Igwe P.O., Ukachukwu A.K. Childhood burns in south eastern Nigeria. Afr J Paediatr Surg. 2009;6:24–27. doi: 10.4103/0189-6725.48571. [DOI] [PubMed] [Google Scholar]
- 78.Fadeyibi I.O., Mustapha I.A., Ibrahim N.A., Faduyile F.I., Faboya M.O., Jewo P.I. Characteristics of paediatric burns seen at a tertiary centre in a low income country: a five year (2004–2008) study. Burns. 2011;37:528–534. doi: 10.1016/j.burns.2010.09.015. [DOI] [PubMed] [Google Scholar]
- 79.Kalayi G., Muhammad I. Burns in children under 3 years of age: the Zaria experience. Ann Trop Pediatr. 1996;16:243–248. doi: 10.1080/02724936.1996.11747833. [DOI] [PubMed] [Google Scholar]
- 80.Laditan A.A. Accidental scalds and burns in infancy and childhood. J Trop Pediatr. 1987;33:199–202. doi: 10.1093/tropej/33.4.199. [DOI] [PubMed] [Google Scholar]
- 81.Asuquo M.E., Ekpo R., Ngim O. A prospective study of burns trauma in children in the University of Calabar Teaching Hospital, Calabar, south-south Nigeria. Burns. 2009;35:433–436. doi: 10.1016/j.burns.2008.07.007. [DOI] [PubMed] [Google Scholar]
- 82.Onuba O. Pattern of burns injury in Nigerian children. Trop Doct. 1988;18:106–108. doi: 10.1177/004947558801800306. [DOI] [PubMed] [Google Scholar]
- 83.Oludiran O.O., Umebese P.F. Pattern and outcome of children admitted for burns in Benin City, mid-western Nigeria. Indian J Plast Surg. 2009;42:189–193. doi: 10.4103/0970-0358.59279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Ugburo A.O., Fadeyibi I.O., Mofikoya B.O., Akanmu O.N., Temiye E.O., Kanu O.O. Neonatal burns in Lagos, South-Western Nigeria: Epidemiology and outcome of management. Burns. 2013;39:483–492. doi: 10.1016/j.burns.2012.07.025. [DOI] [PubMed] [Google Scholar]
- 85.Iregbulem L.M., Nnabuko B.E. Epidemiology of childhood thermal injuries in Enugu, Nigeria. Burns. 1993;19:223–226. doi: 10.1016/0305-4179(93)90153-y. [DOI] [PubMed] [Google Scholar]
- 86.Olawoye O., Iyun A., Ademola S., Michael A., Oluwatosin O. Demographic characteristics and prognostic indicators of childhood burn in a developing country. Burns. 2014;40:1794–1798. doi: 10.1016/j.burns.2014.04.008. [DOI] [PubMed] [Google Scholar]
- 87.Niekerk A Van, Rode H, Laflamme L. Incidence and patterns of childhood burn injuries in the Western Cape , South Africa 2004;30:341–7. [DOI] [PubMed]
- 88.Teo A., Van As A., Cooper J. A comparison of the epidemiology of paediatric burns in Scotland and South Africa. Burns. 2012;38:802–806. doi: 10.1016/j.burns.2012.04.010. [DOI] [PubMed] [Google Scholar]
- 89.Cahill T.J., Rode H., Millar A.J.W. Ashes to ashes: thermal contact burns in children caused by recreational fires. Burns. 2008;34:1153–1157. doi: 10.1016/j.burns.2008.05.015. [DOI] [PubMed] [Google Scholar]
- 90.Parbhoo A., Louw Q.A., Grimmer-Somers K. A profile of hospital-admitted paediatric burns patients in South Africa. BMC Res Notes. 2010;3:165. doi: 10.1186/1756-0500-3-165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Wesson H.K.H., Bachani A.M., Mtambeka P., Schulman D., Mavengere C., Stevens K. Paediatric burn injuries in South Africa: a 15-year analysis of hospital data. Injury. 2013;44:1477–1482. doi: 10.1016/j.injury.2012.12.017. [DOI] [PubMed] [Google Scholar]
- 92.Chopra M., Kettle H., Wilkinson D., Stirling S. Paediatric burns in a rural South African district hospital. SAMJ. 1997;87:600–603. [PubMed] [Google Scholar]
- 93.Whitelock-Jones L., Bass D., Millar A., Rode H. Inhalation burns in children. Pediatr Surg Int. 1999;15:50–55. doi: 10.1007/s003830050511. [DOI] [PubMed] [Google Scholar]
- 94.Cox S.G., Rode H., Darani A.N., Fitzpatrick-Swallow V.L. Thermal injury within the first 4 months of life. Burns. 2011;37:828–834. doi: 10.1016/j.burns.2011.02.003. [DOI] [PubMed] [Google Scholar]
- 95.Holmes W.J.M., Keane B., Rode H. The severity of kettle burns and the dangers of the dangling cord. Burns. 2012;38:453–458. doi: 10.1016/j.burns.2011.09.012. [DOI] [PubMed] [Google Scholar]
- 96.Cox S.G., Martinez R., Glick A., Numanoglu A., Rode H. A review of community management of paediatric burns. Burns. 2015;41:1805–1810. doi: 10.1016/j.burns.2015.05.024. [DOI] [PubMed] [Google Scholar]
- 97.Justin-Temu M., Rimoy G., Premji Z., Matemu G. Causes, magnitude and management of burns in under-fives in district hospitals in Dar Es Salaam, Tanzania. East Afr J Public Health. 2008;5:38–42. doi: 10.4314/eajph.v5i1.38975. [DOI] [PubMed] [Google Scholar]
- 98.Chalya P.L., Mabula J.B., Dass R.M., Giiti G., Chandika A.B., Kanumba E.S. Pattern of childhood burn injuries and their management outcome at Bugando Medical Centre in Northwestern Tanzania. BMC Res Notes. 2011;4:485. doi: 10.1186/1756-0500-4-485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Mugala D., Chishala C. Admissions for burns in children at Nchanga South Hospital – Chingola. East Cent African J Surg. 2006;12:40–42. [Google Scholar]
- 100.Mabogunje O.A., Lawrie J.H. Burns in adults in Zaria, Nigeria. Burns Incl Therm Inj. 1988;14:308–312. doi: 10.1016/0305-4179(88)90072-1. [DOI] [PubMed] [Google Scholar]
- 101.Mabogunje O.A. Burn injuries during the puerperium in Zaria, Nigeria. Int J Gynaecol Obstet. 1989;30:133–137. doi: 10.1016/0020-7292(89)90307-x. [DOI] [PubMed] [Google Scholar]
- 102.Eyal A., Kemp M., Luvhengo T. A 10-year audit of burns at Kalafong Hospital. Burns. 2007;33:393–395. doi: 10.1016/j.burns.2006.07.011. [DOI] [PubMed] [Google Scholar]
- 103.Godwin Y., Hudson D., Bloch C. Shack fires: a consequence of urban migration. Burns. 1996;23:151–153. doi: 10.1016/s0305-4179(96)00118-0. [DOI] [PubMed] [Google Scholar]
- 104.Hudson D., Rode H., Bloch C. Primus stove burns in Cape Town: a costly but preventable injury. Burns. 1994;20:251–252. doi: 10.1016/0305-4179(94)90193-7. [DOI] [PubMed] [Google Scholar]
- 105.Maritz D., Wallis L., Van Der Merwe E., Nel D. The aetiology of adult burns in the Western Cape, South Africa. Burns. 2012;38(1):120–127. doi: 10.1016/j.burns.2010.12.007. [DOI] [PubMed] [Google Scholar]
- 106.Godwin Y., Wood S.H. Major burns in Cape Town: a modified burns score for patient triage. Burns. 1998;24:58–63. doi: 10.1016/s0305-4179(97)00053-3. [DOI] [PubMed] [Google Scholar]
- 107.Rode H., Millar A., Cywes S., Bloch C., Boes E., Theron E. Thermal injury in pregnancy - the neglected tragedy. SAMT. 1990;77:346–348. [PubMed] [Google Scholar]
- 108.Ombati A.N., Ndaguatha P.L.W., Wanjeri J.K. Risk factors for kerosene stove explosion burns seen at Kenyatta National Hospital in Kenya. Burns. 2013;39:501–506. doi: 10.1016/j.burns.2012.07.008. [DOI] [PubMed] [Google Scholar]
- 109.Kalanzi E.W., Hara L.M.O., Hara N.N.O., Boyle J.C. Bed net related burns at Mulago National Referral Hospital, Uganda: a case series report. Burns. 2013;40:495–499. doi: 10.1016/j.burns.2013.08.009. [DOI] [PubMed] [Google Scholar]
- 110.Olaitan P.B., Jiburum B.C. Chemical injuries from assaults: an increasing trend in a developing country. Indian J Plast Surg. 2008;41:20–23. doi: 10.4103/0970-0358.41106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Ukponmwan C. Chemical injuries to the eye in Benin City, Nigeria. WAJM. 2000;19:71–76. [PubMed] [Google Scholar]
- 112.Asaria J., Kobusingye O.C., Khingi B.A., Balikuddembe R., Gomez M., Beveridge M. Acid burns from personal assault in Uganda. Burns. 2004;30:78–81. doi: 10.1016/j.burns.2003.08.009. [DOI] [PubMed] [Google Scholar]
- 113.Thomas M.O., Ogunleye E.O., Somefun O. Chemical injuries of the oesophagus: aetiopathological issues in Nigeria. J Cardiothorac Surg. 2009;4:56. doi: 10.1186/1749-8090-4-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Adedeji T., Tobih J., Olaosun A., Sogebi O. Corrosive oesophageal injuries: a preventable menace. PanAfrican Med J. 2013;15:1–5. doi: 10.11604/pamj.2013.15.11.2495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Datubo-Brown D. Deliberate burns in Nigerians. Trop Doct. 1989:137–140. doi: 10.1177/004947558901900315. [DOI] [PubMed] [Google Scholar]
- 116.Godwin Y., Hudson D. The burnt male – intentional assault on the male by his partner. SAJS. 1998;36:140–142. [PubMed] [Google Scholar]
- 117.Mzezewa S., Jonsson K., Aberg M., Salemark L. A prospective study of suicidal burns admitted to the Harare burns unit. Burns. 2000;26:460–464. doi: 10.1016/s0305-4179(00)00019-x. [DOI] [PubMed] [Google Scholar]
- 118.Opara K., Chukwuanukwu T., Ogbonnaya I., Nwadinigwe C. Pattern of severe electrical injuries in a Nigerian regional burn centre. Niger J Clin Pract. 2006;9:124–127. [PubMed] [Google Scholar]
- 119.Agbenorku P, Agbenorku E, Akpaloo J, Obeng G, Agbley D. Electrical burns: the trend and risk factors in the Ghanaian population. Ann Burns Fire Disasters 2014;27. [PMC free article] [PubMed]
- 120.Muguti G., Doolabh D. Occupational burns as seen in a major industrial city in Zimbabwe. Cent Afr J Med. 1994;40:44–46. [PubMed] [Google Scholar]
- 121.Brusselaers N., Monstrey S., Vogelaers D., Hoste E., Blot S. Severe burn injury in Europe: a systematic review of the incidence, etiology, morbidity, and mortality. Crit Care. 2010;14:R188. doi: 10.1186/cc9300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Atiyeh B.S., Costagliola M., Hayek S.N. Burn prevention mechanisms and outcomes: pitfalls, failures and successes. Burns. 2009;35:181–193. doi: 10.1016/j.burns.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 123.Parbhoo A., Louw Q., Grimmer-Somers K. Burn prevention programs for children in developing countries require urgent attention: a targeted literature review. Burns. 2010;36:164–175. doi: 10.1016/j.burns.2009.06.215. [DOI] [PubMed] [Google Scholar]