Abstract
Introduction
Emergency centres (EC) in low- and middle-income countries often have limited diagnostic imaging capabilities. Point-of-care ultrasound (POCUS) is used in high-income countries to diagnose and guide treatment of life-threatening conditions. This study aims to identify high impact POCUS scans most relevant to practice in an Ethiopian EC.
Methods
A prospective observational study where patients presenting to Tikur Anbessa Specialized Hospital EC in Addis Ababa were eligible for inclusion. Physicians referred patients with a clinical indication for POCUS from a pre-determined 15-scan list. Scans were performed and interpreted, at the bedside, by qualified emergency physicians with POCUS training.
Results
A convenience sample of 118 patients with clinical indications for POCUS was enrolled. The mean age was 35 years and 42% were female. In total, 338 scans were performed for 145 indications in 118 patients. The most common scans performed were pericardial (n = 78; 23%), abdominal free fluid (n = 73; 22%), pleural effusion/haemothorax (n = 51; 15%), inferior vena cava (n = 43; 13%), pneumothorax (n = 38; 11%), and global cardiac activity (n = 25; 7%). One hundred and twelve (95%) POCUS scans provided clinically useful information. In 53 (45%) patients, ultrasound findings changed patient management plans by altering the working diagnosis (n = 32; 27%), resulting in a new treatment intervention (n = 28; 24%), resulting in a procedure/surgical intervention (n = 17; 14%) leading to consultation with a specialist (n = 16; 14%), and/or changing a disposition decision (n = 9; 8%).
Discussion
In this urban, low-resource, academic EC in Ethiopia, POCUS provided clinically relevant information for patient management, particularly for polytrauma, undifferentiated shock and undifferentiated dyspnea. Results have subsequently been used to develop a locally relevant emergency department ultrasound curriculum for Ethiopia’s first emergency medicine residency program.
Keywords: Emergency, Ultrasound, Point-of-care, Low-resource, Emergency medicine, Curriculum
African relevance
-
•
Point-of-care ultrasound (POCUS) is a highly effective tool used to diagnose and guide treatment of emergency patients.
-
•
POCUS is highly relevant to low resource settings since it requires less financial and human resources than other diagnostic imaging tests and can be provided at no cost to patients.
-
•
Training in POCUS in Africa needs to be specific to the needs of local emergency physicians.
Introduction
Emergency centre (EC) point-of-care ultrasound (POCUS) is a highly effective clinical tool in the hands of qualified emergency physicians [1], [2], [3], [4], [5], [6], [7], [8]. In high-resource settings, emergency medicine residents often require ultrasound skills prior to graduation from their residency programs and these skills are acquired through a combination of didactic and practical bedside teaching, with direct supervision by qualified physicians in the EC [5].
In low-resource settings, interest in POCUS training is increasing [9]. As an imaging modality, POCUS is a valuable tool for making timely diagnoses in acute illness, as well as guiding resuscitation and invasive emergency procedures [8], [10], [11]. Ultrasound machines are portable, allowing for continuous monitoring of critically ill patients since scans can be performed directly at the bedside [9], [12], [13]. Furthermore, POCUS is highly relevant to low-resource settings as it can be provided at no cost to the patient, and requires much less financial and human resources than comparable tests such as computerized tomography (CT) scans and X-rays [9], [12], [13]. While POCUS has key features supporting its uptake in low-resource settings, training for emergency residents requires its own curriculum. This should be relevant to the clinical setting, the patient population and the needs of local emergency physicians.
Tikur Anbessa Specialized Hospital (TASH) is a tertiary care referral center in Addis Ababa, Ethiopia. It is Ethiopia’s largest public hospital, a trauma referral centre and the site of the country’s first emergency medicine residency training program, run by Addis Ababa University since 2010. The burden of trauma and acute illness is high in the TASH-EC, and rapid diagnosis and treatment of severely injured or ill patients is often required. However, in-hospital access to formal radiologic studies is limited and critically ill patients are often referred off-site for private imaging if they can afford it. This delays time to diagnosis and increases the risk of adverse outcomes during transport.
The goal of this study was to first determine which POCUS scans are most frequently requested in the TASH-EC. Second, we evaluated the clinical impact of POCUS on patient care by calculating how often the requested scans changed initial patient management plans. We utilized the findings of this study to develop and implement a context relevant POCUS curriculum for the emergency medicine residency program at Addis Ababa University.
Methods
We conducted a prospective case series of TASH-EC patients with a clinical indication for POCUS. The TASH-EC sees the whole spectrum of emergency medical and surgical complaints in patients 13 years and older, including referrals from peripheral centres. The only patients that are not routinely seen are pregnant patients, as they are triaged directly to the labour and delivery ward. The estimated monthly census for the TASH-EC is 1500 visits, of which approximately 35% of patient visits are trauma related.
A list of 15 POCUS scans (Table 1) relevant to the Ethiopian EC was developed by an expert panel which consisted of the following physicians: three emergency physicians with global health experience, two POCUS fellowship-trained emergency physicians, and one board certified radiologist with experience performing and interpreting ultrasound scans in low-resource settings. This list of scans was distributed to all resident physicians working in the TASH-EC in order to identify those patients with a clinical indication for POCUS.
Table 1.
POCUS scan list.
| Intra-abdominal free fluid |
| Pericardial effusion or tamponade |
| Cardiac function (global left ventricular function, b-line profile, right ventricular assessment) |
| Haemothorax/pleural effusion |
| Pneumothorax |
| First trimester pregnancy (rule-in intra-uterine pregnancy) |
| Third trimester pregnancy (fetal heart rate, fetal position, placenta previa) |
| Inferior vena cava for volume status (>50% collapsibility) |
| Deep vein thrombosis |
| Soft tissue/musculoskeletal assessment (long bone fractures, abscess, joint effusion) |
| Gallbladder |
| Aorta |
| Renal/bladder (urinary retention, hydronephrosis) |
| Bowel for evidence of bowel obstruction |
| Ultrasound guided procedures (vascular access, pericardiocentesis, paracentesis, thoracentesis, abscess drainage, arthrocentesis). |
Patients presenting to the EC during two separate four-week study periods in 2012 were eligible for inclusion. Inclusion criteria required that the patient have an indication for one or more of the POCUS scans listed in Table 1. Clinical indications included trauma, dyspnea, shock (hypotension), cardiac arrest, vascular assessment for deep vein thrombosis (DVT) and abdominal aortic aneurysm (AAA), renal/bladder, abdominal pain, pregnancy, musculoskeletal/soft tissue complaints and procedural. For example, the treating physician might want to rule-out intra-abdominal haemorrhage and pneumothorax in a poly-trauma patient. In another case, the physician might want to know if a patient with undifferentiated dyspnea has a pericardial or pleural effusion. Patients were excluded if they did not have a clinical indication for POCUS. Examples include obviously displaced extremity fracture, isolated head injuries, mental health concerns or stroke. Patients were also excluded if the diagnosis was obvious without ultrasound, such as patients with cellulitis, lacerations or gastrointestinal bleeding. A portable ultrasound machine, Sonosite MicroMaxx (on loan) or Full Digital Laptop Ultrasound Scanner RUS-9000F (owned by the TASH-EC), equipped with a 3.5 MHz curved array probe, was kept in the EC at all times. A SeeMore USB ultrasound system equipped with a GP3.5/5.0 MHz abdominal probe and SP7.5/24.0 MHz high frequency probe was available for the last two weeks of the study. This machine was donated to the EC on completion of the study.
Ethiopian emergency medicine resident physicians responsible for the care of EC patients were provided with the POCUS scan list (Table 1) and were instructed to refer patients for one or more POCUS scans when there was a clinical indication. All scans were performed and interpreted in real-time at the patient’s bedside by one of the study physicians. Ethiopian emergency medicine residents caring for patients also had the opportunity to repeat the ultrasound scan under supervision to facilitate their training in POCUS.
The five study physicians performing and interpreting POCUS scans were Canadian consultant level emergency physicians, certified in emergency ultrasound as per the criteria established by the Canadian Emergency Ultrasound Society. Specifically, the minimum qualification for physicians performing and interpreting POCUS scans was the Emergency Department Echo (EDE) 1 certification and prior completion of the EDE2 course [14]. EDE1 certification involves 50 supervised scans in four POCUS areas: subxiphoid view of the heart, abdominal free fluid assessment, aortic assessment for aneurysm and assessment for intrauterine pregnancy in the first trimester. Certification also requires a written, visual and practical examination. The EDE2 course teaches advanced POCUS scans. The list includes but is not limited to advanced cardiac assessment, lung assessment, gallbladder, DVT, vascular access, procedure guidance, inferior vena cava (IVC), musculoskeletal POCUS and others [14]. One of the study physicians was fellowship-trained in POCUS.
The study population represents a convenience sample. Study physicians were available for up to eight hours per day, four to five days per week during the study period. They did have other teaching commitments so could not be available at all times. The TASH-EC does not keep medical records of patient visits, and although we attempted to enrol all patients with a clinical indication for POCUS when an ultrasound-certified physician was in the department, we were not able to determine how many patients were missed. For each patient scanned, the treating physician completed a standardized data collection form including patient demographics, clinical details, indications for ultrasound, ultrasound scans performed, ultrasound findings, and the pre- and post-ultrasound diagnosis and management plan. The pre-ultrasound working diagnosis and management plan was recorded prior to the POCUS examination. Data was entered into an Excel Spreadsheet (Version 14.6.1, Redmond, WA). Basic descriptive statistics including proportions were calculated using Excel. Data was analysed to determine whether ultrasound findings changed initial patient management plans. POCUS was considered to have changed patient management plans if it changed the pre-ultrasound working diagnosis, resulted in a new treatment intervention, led to consultation with a specialist, led to a procedure/surgery and/or changed a disposition decision.
Informed consent was obtained from all included patients. If the patient was unable to give consent, it was obtained from a substitute decision maker. When a substitute decision maker was unavailable, consent was obtained retrospectively from the patient as soon as they were able to provide consent. Ethical review and approval was provided by Addis Ababa University (Addis Ababa, Ethiopia) and the University Health Network Research Ethics Board (Toronto, Canada).
Results
One-hundred and eighteen patients were enrolled in the study. The mean age was 35 years (ranging from 13 to 78 years) and 42% were female. In total, 338 scans were performed for 145 indications in 118 patients. More than one indication for POCUS was documented for 31 patients. Of the 145 total clinical indications documented, the most common clinical indication for POCUS in the EC was assessment of trauma (n = 51; 35%), followed by assessment of medical shock/hypotension (n = 29; 20%) and undifferentiated dyspnea (n = 24; 17%). POCUS scans were requested and performed at a lesser frequency for other clinical indications listed in Table 2.
Table 2.
POCUS scans requested by clinical indication (total number of indications N = 145).
| Ultrasound Indication | N = 145 | % |
|---|---|---|
| Trauma | 51 | 35 |
| Medical Shock/Hypotension | 29 | 20 |
| Dyspnea | 24 | 17 |
| Abdominal Pain | 11 | 8 |
| Procedure Guidance | 9 | 6 |
| Musculoskeletal | 6 | 4 |
| Pregnancy | 4 | 3 |
| Leg Swelling | 4 | 3 |
| Renal/Bladder | 3 | 2 |
| Cardiac Arrest | 2 | 1 |
| Abdominal Aortic Aneurysm | 2 | 1 |
Of the 338 scan types performed, the most common POCUS scans performed in the study were as follows: pericardium for effusion or tamponade (n = 78; 23%), intra-abdominal free fluid (n = 73: 22%), pleural effusion/haemothorax (n = 51; 15%), IVC assessment (n = 43; 13%), pneumothorax (n = 38; 11%), and the assessment of cardiac function (n = 25; 7%). See Table 3 for frequency of all scan types requested.
Table 3.
POCUS scans requested by scan type (total number of scans N = 338).
| Ultrasound Scan | N = 338 | % |
|---|---|---|
| Pericardial Effusion | 78 | 23 |
| Intra-abdominal Free Fluid | 73 | 22 |
| Pleural effusion/haemothorax | 51 | 15 |
| Inferior Vena Cava | 43 | 13 |
| Pneumothorax | 38 | 11 |
| Cardiac Function | 25 | 7 |
| Procedural | 8 | 2 |
| Musculoskeletal/Soft Tissue | 6 | 2 |
| Deep Vein Thrombosis | 4 | 1 |
| Renal/Bladder | 4 | 1 |
| Pregnancy (First and Third Trimester) | 3 | 1 |
| Other (Aorta, Gallbladder, Bowel) | 5 | 2 |
The number of scans and indications exceeds the number of patients because often, several scans were requested for the same patient. For example, poly-trauma patients were often scanned to assess for intra-abdominal free fluid, haemopericardium, pneumothorax and haemothorax. Medical patients in shock often had several scans including pericardium, global cardiac activity, lung scans, an assessment of IVC collapsibility and DVT search.
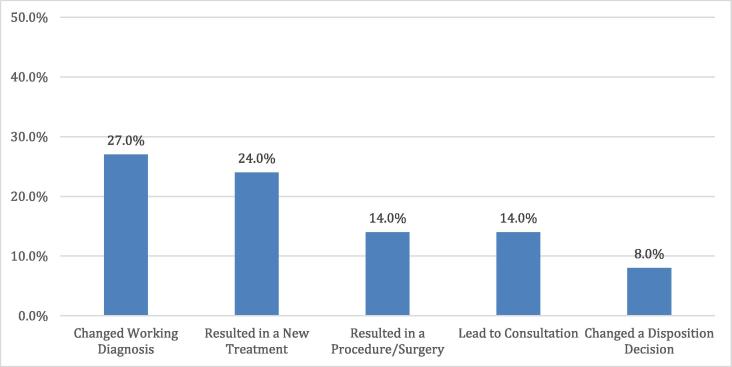
Overall, POCUS was found to provide clinically useful information in 95% of patients (95% CI: 90–98). In 45% of patients (95% CI: 36–54), the ultrasound scan changed initial pre-ultrasound patient management plans by changing the working diagnosis (27%; 95% CI: 20–36), resulting in a new treatment intervention (24%; 95% CI: 17–32), resulting in a procedure/surgical intervention (14%; 95% CI: 9–22), leading to consultation with a specialist (14%; 95% CI: 8–21), and/or changing a disposition decision (8%; 95% CI: 4–14) (Fig. 1).
Fig. 1.
Changes in patient management based on ultrasound findings.
Scans that did not change management still provided clinically useful information in an additional 50% of patients (95% CI: 41–59) by narrowing the differential diagnosis, excluding a life-threatening diagnosis, or providing diagnostic certainty. Five percent of ultrasounds (95% CI: 2–10) did not contribute to patient care. This was either due to an indeterminate scan or occurred when the pre-ultrasound diagnosis and plan was clear prior to the ultrasound examination.
The following are some examples to illustrate how POCUS changed management:
-
•
Case 1: A 31-year old male fell from scaffolding, resulting in a head injury with altered mental status. He was not able to tell the treating physician where he was having pain. POCUS revealed a haemo-pneumothorax that was not clinically suspected. Based on this, a chest tube was inserted for treatment, confirming the POCUS findings.
-
•
Case 2: A 35-year old female presented to the EC following a motor vehicle accident, with chest and pelvic pain. Chest X-ray showed right sided rib fractures and pelvic X-ray showed a pubic ramus fracture. The initial management plan was for discharge home. POCUS revealed a right sided pneumothorax that was not evident on chest X-ray. The management plan was changed and the patient was admitted to the EC for 24 h of oxygen therapy, monitoring and repeat chest X-ray to ensure that the pneumothorax was not expanding.
-
•
Case 3: A 52-year old male presented with generalized weakness, hypotension and a pulsatile abdominal mass felt on physical examination. A working diagnosis of AAA rupture with hypovolemic shock was entertained and surgical consultation was planned. POCUS revealed that the maximal diameter of the abdominal aorta was 2 cm, excluding an AAA. The IVC completely collapsed with respiration. The patient was just very thin leading to a palpable but not aneurysmal aorta. Following POCUS, other causes of hypovolemic shock were investigated.
-
•
Case 4: A 24-year old male was referred from a rural centre with a one-week history of abdominal pain and vomiting, which progressed despite antibiotic treatment to persistent fever, altered mental status and hypotension unresponsive to fluids. On presentation to the TASH-EC, the working diagnosis was septic shock secondary to an intra-abdominal cause (perforated viscus, cholangitis or pancreatitis), although no imaging or blood-work was available. POCUS revealed a large circumferential pericardial effusion with sonographic signs of tamponade and a full, non-collapsible IVC. A diagnosis of cardiac tamponade was not previously considered. Subsequently, an ultrasound-guided pericardiocentesis was performed and frankly purulent material was aspirated, leading to a final diagnosis of purulent pericarditis.
-
•
Case 5: A 16-year old female presented with shortness of breath, hypoxia and hypotension. Her working diagnosis was pneumonia and she was being treated with intravenous ceftriaxone but was too unstable to leave the EC for chest X-ray. Surprisingly, POCUS showed a dilated, poorly contracting right ventricle. Her IVC was dilated and non-collapsible. There was normal bilateral lung sliding with no B-lines, no pleural effusion and no lung hepatisation. POCUS changed the working diagnosis from pneumonia with septic shock to large pulmonary embolism. The patient was anti-coagulated. Her family was able to afford a CT scan and the diagnosis of saddle pulmonary embolism was confirmed on CT chest approximately 48 h later.
-
•
Case 6: A 15-year old male presented with fever and hip pain. The working diagnosis was a septic joint, however multiple attempts at blind aspiration of the hip joint had failed. POCUS confirmed a joint effusion. Ultrasound-guided arthrocentesis was done, resulting in aspiration of 15 cc of purulent material.
Table 4 lists all POCUS scans that were positive for pathology during the study period.
Table 4.
Pathology identified by POCUS (total number of patients N = 118).
| Pathology | N |
|---|---|
| Intra-abdominal free fluid (traumatic) | 11 |
| Haemothorax | 7 |
| Pneumothorax | 9 |
| Intra-abdominal free fluid (non-traumatic) | 10 |
| Pleural Effusion | 13 |
| Ectopic Pregnancy | 1 |
| Fetal Viability in Third Trimester | 3 |
|
(1) |
| Inferior Vena Cava | |
|
10 |
|
6 |
|
9 |
| Cardiac | |
|
5 |
|
2 |
|
2 |
|
6 |
|
1 |
| Pericardial effusion | 8 |
|
(1) |
| Renal | |
|
1 |
|
2 |
| Deep Vein Thrombosis | 2 |
| US Guided procedures | |
|
3 |
|
1 |
|
1 |
|
1 |
|
1 |
| Soft Tissue Abscess | 1 |
| Cholecystitis | 1 |
| Signs of bowel obstruction | 1 |
Discussion
This study adds to a growing body of literature that supports clinician-performed POCUS as a valuable diagnostic and therapeutic tool in resource-limited settings [9], [16], [17], [18]. First, we report that, from the scans done, most were requested to assist in the diagnosis and management of critically ill and injured patients, which reflects the patient population in the TASH-EC [19]. As other low-income countries share an increased burden of trauma and critical illness worldwide, we believe these indications are also highly relevant in similar urban low-resource settings [20], [21]. Second, in the absence of other available modalities (ie. X-ray, CT scan), we report that multiple POCUS scans were requested per patient to assess these critical conditions. For example, many trauma patients received extended Focused Assessment with Sonography in Trauma (FAST) examinations looking for intra-abdominal free fluid, pericardial effusion, pneumothorax and haemothorax (Table 3). Finally, we showed that POCUS had an important role in guiding management for undifferentiated EC patients. This high degree of utility in clinical decision-making reflects the value of POCUS in settings with limited access to formal diagnostic imaging and laboratory testing. Several studies in sub-Saharan Africa have shown similar utility. In Rwanda, where ultrasound was introduced in a rural setting, 43% of management plans were changed by POCUS. In a tertiary care urban center in Liberia, ultrasound changed management plans 62% of the time [16], [17].
We acknowledge that this study has the following limitations. First, our results reflect the patient population of TASH-EC, which is a very high acuity and mainly adult population. This may not be the case in other resource-limited settings in sub-Saharan Africa with a higher percentage of obstetric, paediatric and ambulatory patients. Specifically, the low rates of ultrasound use for the management of pregnancy-related emergencies in our study should not be interpreted as more broadly applicable to other settings in sub-Saharan Africa, but rather specific to our hospital where obstetric patients go directly to labour and delivery, bypassing the EC. Several studies support the value of obstetric POCUS in sub-Saharan Africa [16], [17], [18], [22]. Secondly, the study was limited by the availability of a 3.5 MHz transducer. Had a high-frequency probe been more readily available, requests for DVT assessment, ultrasound guided vascular access and other procedures may have been higher. Third, due to the limitations of the practice environment, we were not able to compare POCUS findings against the final diagnosis in some cases. Ultrasound machines did not have recording capabilities and most patients were either too unstable or could not afford formal ultrasound or CT scanning. Furthermore, once the patient left the EC, it was very difficult to track them. Whenever possible we did try and verify POCUS findings. For some patients, POCUS lead to a procedure which confirmed the findings (for example, aspiration of a pleural effusion or insertion of a chest tube). If POCUS lead to a surgical intervention, we confirmed the diagnosis with our surgical colleagues. Occasionally we were able to obtain formal ultrasound or CT scans. We are not aware of any cases where the POCUS diagnosis disagreed with the final diagnosis.
Prior to this study, emergency medicine residents at Addis Ababa University received some limited POCUS training from visiting emergency medicine faculty from the University of Toronto as part of the Toronto Addis Ababa Academic Collaboration in Emergency Medicine (TAAAC-EM) partnership [15]. However, at the time of study, there was no formal POCUS curriculum and no mechanism in place to assess resident competency at the completion of their emergency medicine training.
In conclusion, in this urban academic emergency center setting in Ethiopia, POCUS had a significant impact on diagnosis and management plans for emergency patients, particularly those presenting with polytrauma, undifferentiated shock and dyspnea. The findings of this study contributed to the development and implementation of a formalized context relevant POCUS curriculum for the Emergency Medicine Residency Program at Addis Ababa University. Residents now receive ongoing didactic lectures and practical sessions for an evidence-based set of POCUS indications that reflect local disease patterns and emergency provider needs. We plan to report on the development and impact of this new curriculum in a future publication.
Conflicts of interest
The authors declare no conflicts of interest.
Dissemination of results
The results of this study were shared with staff members at Tikur Anbessa Specialized Hospital emergency centre. The study results were used guide the development and implementation of a POCUS curriculum for the emergency medicine residency program at Addis Ababa University.
Authors’ contributions
MS, ML, FA, RV, CH, JS and AA designed the study. MS, FA, RV, JM, AA and TKcollected the data. MS, ML and SB analyzed and interpreted the data. MS, ML, FA, CH and SB wrote the manuscript. MS, ML, FA, RV, CH, SB, JM, JS and AA contributed to the manuscript editing and revision. MS, ML, FA, RV, CH, SB, JM, JS, AA and TK agreed with manuscript results and conclusions.
Footnotes
Peer review under responsibility of African Federation for Emergency Medicine.
References
- 1.McRae A., Murray H., Edmonds M. Diagnostic accuracy and clinical utility of emergency department targeted ultrasonography in the evaluation of first-trimester pelvic pain and bleeding: a systematic review. CJEM. 2009;11:355–364. doi: 10.1017/s1481803500011416. [DOI] [PubMed] [Google Scholar]
- 2.Melniker L.A., Leibner E., McKenney M.G. Randomized controlled clinical trial of point-of-care, limited ultrasonography for trauma in the emergency department; the first sonography outcomes assessment program trial. Ann Emerg Med. 2006;235:227–235. doi: 10.1016/j.annemergmed.2006.01.008. [DOI] [PubMed] [Google Scholar]
- 3.Mandavia D.P., Hoffner R.J., Mahaney K. Bedside echocardiography by emergency physicians. Ann Emerg Med. 2001;38:377–382. doi: 10.1067/mem.2001.118224. [DOI] [PubMed] [Google Scholar]
- 4.Kuhn M., Bonnin R.L., Davey M.J. Emergency department ultrasound scanning for abdominal aortic aneurysm: accessible, accurate, and advantageous. Ann Emerg Med. 2000;36:219–223. doi: 10.1067/mem.2000.108616. [DOI] [PubMed] [Google Scholar]
- 5.American College of Emergency Physicians Emergency Ultrasound Guidelines. Ann Emerg Med. 2009;14:550–570. [Google Scholar]
- 6.Blaivas M., Fox J. Outcomes in cardiac patients found to have cardiac standstill on the bedside emergency department echocardiography. Acad Emerg Med. 2001;8:616–621. doi: 10.1111/j.1553-2712.2001.tb00174.x. [DOI] [PubMed] [Google Scholar]
- 7.Pomero F., Dentali F., Borretta V. Accuracy of emergency physician-performed ultrasonography in the diagnosis of deep-vein thrombosis: a systematic review and meta-analysis. Thromb Haemost. 2013;109:137–145. doi: 10.1160/TH12-07-0473. [DOI] [PubMed] [Google Scholar]
- 8.Leung J., Duffy M., Finckh A. Real-time ultrasonographically-guided internal jugular vein catheterization in the emergency department increases success rates and reduces complications: a randomized, prospective study. Ann Emerg Med. 2006;48:540–547. doi: 10.1016/j.annemergmed.2006.01.011. [DOI] [PubMed] [Google Scholar]
- 9.Sippel S., Muruganandan K., Levine A. Review Article. Use of ultrasound in the developing world. International. J Emerg Med. 2011;4:72. doi: 10.1186/1865-1380-4-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Perera P., Mailhot T., Riley D. The RUSH exam: rapid ultrasound in shock in the evaluation of the critically ill. Emerg Med Clin N Am. 2010;28:29–56. doi: 10.1016/j.emc.2009.09.010. [DOI] [PubMed] [Google Scholar]
- 11.Jones A.E., Tayal V.S., Sullivan D.M. Randomized, controlled trial of immediate versus delayed goal directed ultrasound to identify the cause of nontraumatic hypotension in emergency department patients. Crit Care Med. 2004;32:1703–1708. doi: 10.1097/01.ccm.0000133017.34137.82. [DOI] [PubMed] [Google Scholar]
- 12.Mindel S. Role of imager in developing world. Lancet. 1997;349:426–429. doi: 10.1016/S0140-6736(97)03340-0. [DOI] [PubMed] [Google Scholar]
- 13.Future use of new imaging technologies in developing countries. World Health Organ Tech Rep Ser. 1985;723:1–67. Report of a WHO Scientific Group. [PubMed] [Google Scholar]
- 14.The Canadian Emergency Ultrasound Society. www.ceus.ca. Accessed April 22, 2016.
- 15.Maskalyk J., Landes M. The Toronto-Addis Ababa academic collaboration: emergency medicine. Ethiop Med J. 2014;2:45–48. [PubMed] [Google Scholar]
- 16.Kotlyar S., Moore C.L. Assessing the utility of ultrasound in Liberia. J Emerg Trauma Shock. 2008;1:10–14. doi: 10.4103/0974-2700.41785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shah S.P., Epino H., Bukhman G. Impact of the introduction of ultrasound services in a limited resource setting: rural Rwanda 2008. BMC Int Health Hum Rights. 2009;9:4. doi: 10.1186/1472-698X-9-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kimberly H.H., Murray A., Mennicke M. Focused maternal ultrasound by midwives in rural Zambia. Ultrasound Med Biol. 2010;36:1267–1272. doi: 10.1016/j.ultrasmedbio.2010.05.017. [DOI] [PubMed] [Google Scholar]
- 19.Hunchak C, Teklu S, Meaney C, et al. Patterns and predictors of early mortality in the emergency department in Addis Ababa, Ethiopia: A Prospective Study. Oral presentation. Canadian Association of Emergency Physicians (CAEP) Annual Conference, Edmonton, Alberta, Canada 2015.
- 20.Razzak J.A., Kellermann A.L. Emergency medical care in developing countries: is it worthwhile? Bull World Health Organ. 2002;80:900–905. [PMC free article] [PubMed] [Google Scholar]
- 21.Hsia R., Razzak J., Tsai A.C. Placing emergency care on the global agenda. Ann Emerg Med. 2010;56:142–149. doi: 10.1016/j.annemergmed.2010.01.013. [DOI] [PubMed] [Google Scholar]
- 22.Harris R.D., Marks W.M. Compact ultrasound for improving maternal and perinatal care in low-resource settings: review of the potential benefits, implementation challenges, and public health issues. J Ultrasound Med. 2009;28:1067–1076. doi: 10.7863/jum.2009.28.8.1067. [DOI] [PubMed] [Google Scholar]