Abstract
Introduction
There is little research on emergency care delivery in low- and middle-income countries (LMICs). To facilitate future research, we aimed to assess the set of key metrics currently used by researchers in these settings and to propose a set of standard metrics to facilitate future research.
Methods
Systematic literature review of 43,109 published reports on general emergency care from 139 LMICs. Studies describing care for subsets of emergency conditions, subsets of populations, and data aggregated across multiple facilities were excluded. All facility- and patient-level statistics reported in these studies were recorded and the most commonly used metrics were identified.
Results
We identified 195 studies on emergency care delivery in LMICs. There was little uniformity in either patient- or facility-level metrics reported. Patient demographics were inconsistently reported: only 33% noted average age and 63% the gender breakdown. The upper age boundary used for paediatric data varied widely, from 5 to 20 years of age. Emergency centre capacity was reported using a variety of metrics including annual patient volume (n = 175, 90%); bed count (n = 60, 31%), number of rooms (n = 48, 25%); frequently none of these metrics were reported (n = 16, 8%). Many characteristics essential to describe capabilities and performance of emergency care were not reported, including use and type of triage; level of provider training; admission rate; time to evaluation; and length of EC stay.
Conclusion
We found considerable heterogeneity in reporting practices for studies of emergency care in LMICs. Standardised metrics could facilitate future analysis and interpretation of such studies, and expand the ability to generalise and compare findings across emergency care settings.
Keywords: Emergency medicine, Systems development, Low- and middle-income countries
Abstract
Introduction
Peu d’études ont été réalisées sur la fourniture de soins d’urgence dans les pays à faible et moyen revenus (PFMR). Pour faciliter les futures études, nous avons cherché à évaluer l’ensemble de mesures clés actuellement utilisées par les chercheurs dans ces contextes, et à proposer un ensemble de mesures standard afin de faciliter les futures études.
Méthodes
Une analyse bibliographique systématique de 43 109 rapports publiés sur les soins d’urgence généraux provenant de 139 PFMR a été réalisée. Les études décrivant les soins pour des sous-ensembles de conditions urgentes, des sous-ensembles de populations, et des données agrégées issues de plusieurs structures ont été exclues. Toutes les statistiques au niveau des structures et des patients rapportées dans ces études ont été enregistrées et les mesures les plus couramment utilisées ont été identifiées.
Résultats
Nous avons identifié 195 études sur la fourniture de soins d’urgence dans les PFMR. Une faible uniformité a été observée dans les mesures rapportées, que ce soit au niveau des patients ou des structures. Les données démographiques relatives aux patients ont été rapportées de manière irrégulière: seulement 33% indiquaient l’âge moyen et 63% la répartition hommes/femmes. La limite d’âge supérieure utilisée pour les données pédiatriques variait dans une large mesure, allant de 5 à 20 ans. La capacité des centres d’urgence a été rapportée en utilisant un vaste éventail de mesures et notamment le volume annuel de patients (n = 175, 90%); nombre de lits (n = 60, 31%), nombre de chambres (n = 48, 25%); souvent, aucune de ces mesures n’était rapportée (n = 16, 8%). De nombreuses caractéristiques essentielles pour décrire les capacités et la performance des soins d’urgence n’étaient pas rapportées, et notamment l’utilisation des méthodes de triage et leur type, le niveau de formation des prestataires, le taux d’admission, le temps écoulé avant qu’une évaluation soit faite et la durée du séjour aux urgences.
Conclusion
Nous avons observé une hétérogénéité considérable dans les pratiques de compte-rendu relatives aux études portant sur les soins d’urgence dans les PMFR. Des mesures standardisées pourraient faciliter l’analyse et l’interprétation futures de telles études, et améliorer la capacité à généraliser et à comparer les conclusions entre les différents contextes de soins d’urgence.
African relevance
-
•
Emergency systems development is a foundational part of developing emergency care in Africa.
-
•
Emergency care research in Africa is small in comparison to the rest of the world.
-
•
Defining key metrics used concurrently throughout African emergency care research is important to facilitate future research.
Introduction
Emergency medicine plays an integral role in many health systems around the world, primarily in high-income countries.1, 2, 3, 4, 5, 6, 7 There is mounting evidence that high-quality emergency care has the potential to address a significant proportion of the global burden of disease, as advocates have called for the development of emergency care in low- and middle-income countries (LMICs).8, 9, 10, 11, 12, 13, 14, 15, 16 Recent outbreaks of pandemic infectious diseases such as MERS-CoV in the Middle East and Asia, and Ebola in West Africa highlighted the need for equipped emergency care facilities, staffed with trained personnel to stem the tide of such outbreaks and to form the front lines in the treatment of more common but increasingly important conditions such as non-communicable disease (NCDs) and injuries in LMICs.17
Despite the compelling need for more data on emergency care in LMICs, research in this area has been largely neglected. A 2015 systematic review of emergency facilities in LMICs found no published reports on emergency care in over half of LMICs.18 Where data were available, the review found that only a small set of metrics on emergency care delivery was reported consistently across facilities, and that researchers frequently used a wide array of ill-defined measures to describe EC characteristics and performance. This inconsistency has complicated inter-facility data comparison and study replication.16, 19 More data are needed to understand current capabilities, expose deficits, and ultimately improve emergency care delivery in these resource-constrained settings.10, 16, 18, 19, 20
In this study, we identify a set of key metrics commonly used by researchers to describe emergency care in LMICs and propose a standard set of data elements that would be practical to collect. A consensus on basic terminology and methodology has advanced the field of emergency medicine in high-income countries, and a clearly defined core set of metrics for describing emergency care in LMICs would similarly not only advance local emergency care research and quality improvement, but also allow for more effective cross pollination and systems development.
Methods
We conducted a systematic review (PROSPERO registry: CRD42014007617) to identify published reports describing general emergency care delivered to an undifferentiated patient population in all 139 LMICs. For each LMIC, we searched PubMed, CINAHL, and all World Health Organization (WHO) regional indices using “[country name] + emerg∗” as the search term. We performed a similar search on Google Scholar, but limited the search to within article titles given the large number of results. We also manually screened select non-indexed journals known to frequently publish research on emergency care. Reference lists of all studies included were further screened manually.
Results were screened by title and abstract, and selected for inclusion if they described facility-based emergency care provided to all patients, regardless of disease category or chief complaint. Articles published after 1989 in all languages were included provided an English or French abstract was available. We excluded studies focussed only on specific emergent conditions (e.g., stroke only), subsets of the general emergency patient population (e.g., women only), or data aggregated from multiple departments or facilities, unless they provided general emergency facility statistics or data on the burden of diseases.
We evaluated the reporting frequency of data elements commonly found in published emergency care literature originating from LMICs. We created a database that continually expanded with new data fields as the systematic review progressed and new reported metrics were encountered. At the conclusion of the review, we selected publications that provided comprehensive descriptions of their facilities and patients, and used them as models to structure our recommendations for future research.
At the conclusion of our review, we presented our findings at the African Federation of Emergency Medicine consensus conferences, Addis Ababa 2014 and Cape Town 2015. Small group discussion amongst attendees provided invaluable insight into some of the local determinants and limitations to data collection and publication in certain settings. We incorporated lessons learnt from the group discussions on how to improve data standards into our recommendations. We highlight specific information to be recorded and reported by individual emergency facilities, to enable reliable inter-facility data comparisons and expose areas for improvement in specific locales.
Results
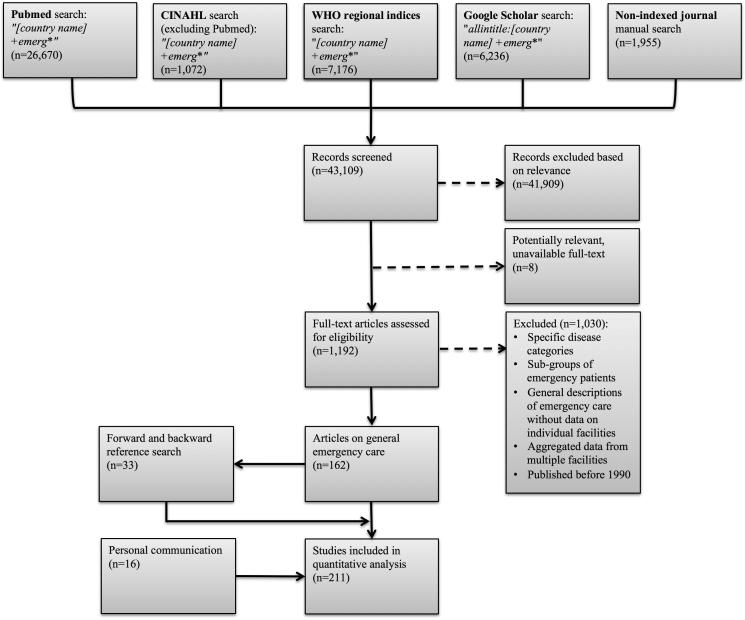
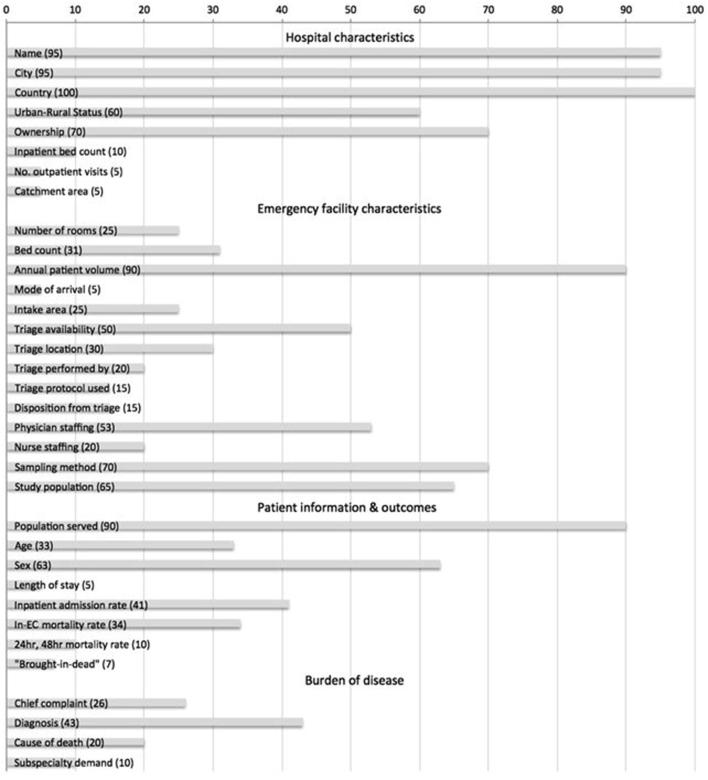
Fig. 1 shows the search strategy used to screen 43,109 published reports with 195 studies meeting our inclusion criteria. This resulted in descriptions of 192 unique facilities in 139 LMICs, as shown geographically in the map in Fig. 2. Fig. 3 presents the proportion of these publications that reported the data elements of interest.
Figure 1.
The flow diagram shows the results of the database and journal searches, acquisition of unpublished data, and application of exclusion criteria.
Figure 2.
Number of publications, geocoded to location of facilities described (Lighter colour indicates more publications. High income countries were removed from the map to show only LMICs.
Figure 3.
Proportion (%) of publications reporting data.
As a whole, hospital characteristics were nearly universally reported, with the exception of whether it was located in an urban or rural setting. As a result, researchers curious as to the kinds of patients the facility served or its geographic access would have to use mapping software (e.g., Google Maps) to find an approximate location for the facility. Similarly, indicators of overall hospital size and patient capacity, such as the number of inpatient beds, were infrequently reported; however, could be found occasionally on the hospital webpage, if one existed. The physical layout of the emergency centre itself, including the number of emergency centre beds, was documented more often. The annual patient volume in the emergency centre was the most commonly reported marker for facility size, but the simultaneous reporting of the catchment area for the hospital or the number of outpatient visits per year was rare.
Although half of the studies referenced the availability of triage, further details on the processes for stratification of patient acuity were not routinely provided. For example, only 20% described the level of training of the healthcare provider performing the triage assessment and even less frequently the protocol used, if any. The level of training for the physicians staffing the EC was reported in only half of the publications, and less so for nurse staffing.
Approximately one-fifth of publications were general facility descriptions, without individual emergency facility patient sampling. When patient-level data for those study subjects presenting for emergency care were utilised, 27% were prospective observational or cross-sectional studies and 73% retrospective studies. Continuous sampling was the most commonly used method to gather data on study subjects. But overall, when employing other sampling methods, there was lack of clarity and detail in the study methods to explain the procedures used to ensure adequate selection of a representative study sample.
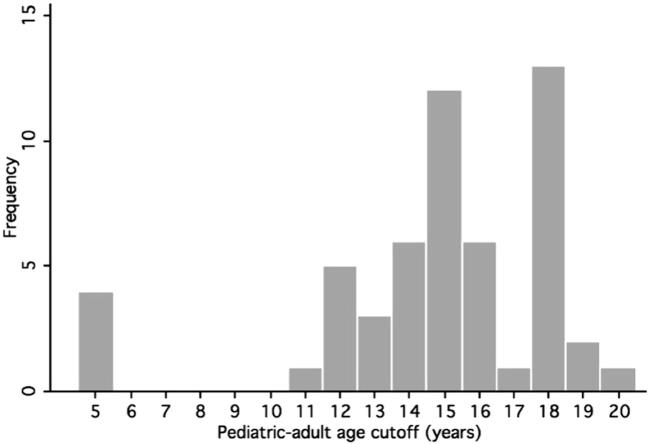
The emergency patient population was defined as paediatric, adult, or general in 90% of reports, 33% reported median or average age for patients, and 63% the proportion of either sex. Fig. 4 shows the frequency of chosen paediatric to adult age cut-offs used by facilities in our review. While the median age was 15 (IQR 14–18), the range was wide from 5 (4 studies in 3 countries)21, 22, 23, 24 to 20 years of age (1 study in 1 country).25
Figure 4.
Distribution of paediatric to adult age cut-offs found in emergency care literature originating from LMICs.
Patient outcomes of emergency care, which would serve as a marker for the standard of acute care delivery at each facility, were poorly reported limiting the reader’s ability to draw accurate conclusions from the published reports. Perhaps the most objective and useful metrics for emergency care- mortality rates at specific time interval, such as 24-h or 48-h mortality- were only available in 10% of publications.
The recording of diagnoses was hallmarked by the same lack of consistency as the data describing emergency care. Only 10% of reports used specific diagnosis coding systems, such as ICD-10 Clinical Classification Software. Frequent misclassification, inconsistent, or double classification of conditions can result in over- or underestimation of key conditions. Table 1 lists examples of inconsistencies in the categorisation of various diagnoses and causes of death. Articles commonly classified localized infections with their respective organ system—but also included a separate infectious disease category, presumably for systemic infections (e.g., meningitis and cerebral malaria categorised with the central nervous system, while malaria, tetanus, septicaemia and enteric fever with “various infections”).26 Similarly, traumatic conditions could be categorised with the organ system affected and with a general trauma category.
Table 1.
Burden of disease reporting inconsistencies.
| Inconsistencies in reporting and categorisation of burden of disease metrics | Examples |
|---|---|
| Diagnosis | |
| Infectious disease | |
| Localized infections included with respective organ system categories | Pneumonia categorised with ‘respiratory disease’ (rather than infectious)27 |
| Infectious disease categorised separately from organ system categories | Malaria and pneumonia categorised with “all infectious complaints”28 |
| Inconsistent reporting of infectious diagnoses within a single study | Infective endocarditis categorised with cardiovascular disease, amoebic liver abscess with gastrointestinal disease, but pneumonia, liver abscess, and amoebic dysentery categorised with infectious disease29 |
| Trauma | |
| Specific traumatic diagnoses reported with respective organ system despite separate trauma category | Abdominal bruising and wounds categorised with abdominal conditions despite an abdomen subcategory for trauma30 |
| Cause of death | |
| Infectious disease | |
| Infectious causes included with respective organ system | Meningitis categorised with neurological disease31 |
| Inconsistent reporting of infectious causes within a single study | Cerebral malaria categorised with neurological disease, but also a separate severe malaria category32 |
| Surgical | |
| Malignancies classified as surgical causes of death | Prostate and breast cancer categorised with surgical causes of death31 |
Discussion
Our review uncovered considerable heterogeneity in reporting practices for studies of emergency care in LMICs. As a result, these research efforts, despite presenting valuable statistics and important healthcare metrics, had limited utility when comparing emergency care delivery and outcomes across different settings and determining trends in time.
Specific deficiencies were identified in data elements that required obtaining data from other departments. For example, inpatient beds (10%) and total outpatient visits per year (5%) were underreported. Metrics obtained directly from within the footprint of the EC were reported more reliably, for example annual EC patient volume (90%) was consistently reported as a measure of EC capacity. Similarly, patient events that occur outside the EC are infrequently reported in publications of emergency care in LMICs. Rates of 48 h mortality (10%) and need for subspecialty care (10%) had low-rates of reporting possibly because they do not occur within the patient’s EC stay, while data such as type of population served (90%) and gender (63%) are both readily obtained during the EC stay itself and thus more frequently reported. It is instructive to note that studies were 3–4× as likely to report important metrics like patient mortality in the EC, compared to reporting that required follow up of patients after disposition to the inpatient service. This may be the result of weaknesses in hospital-wide health information systems in most facilities in LMICs, resulting in inability to consistently capture data on these events as part of the emergency care data recorded. Finally, the rate of patients “brought-in-dead” was only reported 7% of the time—this complicates interpretation of in-EC mortality rates, since some hospitals may report these patients as having died in the EC. This raises questions regarding the consistency of definitions used for these categories and the lack of transparency in the practices regarding reporting mortality statistics in these facilities.
Several important functions of emergency care were also underreported in the studies we reviewed, complicating interpretation of data and its use for future research. First, patient triage is an indispensable first step to high quality emergency care; yet, it was only referenced in approximately one quarter of reports from LMICs. Even fewer publications provided details on triage processes, which are likely to be variable33, 34; indeed, several studies have demonstrated a significant improvement in patient outcomes after the implementation of structured triage.21, 22, 35 Second, the training level for physicians staffing the facility was noted in approximately half of reports. Lack of senior level supervision of physicians in training has been linked to worse patient outcomes,36, 37, 38 Reporting the level of training of physicians and nurses staffing facilities in LMICs is essential to understanding the capabilities to provide various services and for accurately mapping the human resource gaps.39
Other statistics reported in the literature used non-uniform parameters, which made it difficult to aggregate data across facilities. For example, the reporting of in-EC mortality rate was the most frequent measure of death; however, the majority of studies failed to also report patient lengths of stay. When lengths of stays were available, the atypical ranges – up to 117 days in a facility in Brazil40 – and failure to report means and medians for the data made it difficult to compare emergency care across facilities. This heterogeneity in reporting such a critical data element reinforces the importance of having a standard metric for death, such as 24-h mortality.
Likewise, length of stay data were often reported with respect to specific and varying time intervals (e.g., >24 h), rather than averages, complicating comparative analyses.40, 41, 42 Paediatric-adult age cut-offs chosen by individual facilities also varied widely (Fig. 1). This distorted the appropriate classification of these patient groups across different studies and made it difficult to assess the key differences in patient characteristics, their burden of disease, and clinical outcomes.
In addition, there was also discrepancy in reporting burden of disease information. Traumatic and infectious conditions were variably reported with their respective organ systems, i.e., pneumonia categorised with pulmonary disease, or they were grouped together under a broad infectious disease category. This inconsistency in disease categorisation even occurred within a single publication (Table 1). Ideally, having all infectious and traumatic conditions grouped together as standard practice would allow for an accurate understanding of the true burden of disease.
In order to help guide emergency care clinicians and researchers in LMICs, we present a template for manuscript preparation that provides recommendations for how data can be collected, analysed, and reported in a standardised fashion. Consistent research practices across different emergency care settings would maximise the utility of gathered information and allow for more meaningful conclusions to be drawn from aggregated comparable data that could not be gathered in as large a volume from one facility. Furthermore, the ability to aggregate data and to generalise results will make emergency care research in LMICs more useful to other emergency care practitioners who will more confidently be able to assess the ability to translate research findings into their own clinical setting.
Table 2 provides a set of recommendations that stemmed from our systematic review. A publication template can also be found in the Online supplement. Insights from small group discussions at the African Federation of Emergency Medicine consensus conferences have also been incorporated into these recommendations.
Table 2.
Recommendations for data collection, analysis, and reporting based on findings from the systematic review.
| Data category | Recommendations and examples |
|---|---|
| Hospital characteristics | |
| Urban–rural status |
|
| Facility ownership |
|
| Size | |
| Inpatient bed count |
|
| Number of outpatient visits per year |
|
| Catchment area |
|
| Emergency facility characteristics | |
| Size | |
| Layout and number of rooms |
|
| Bed count |
|
| Annual EC patient volume |
|
| Intake | |
| Mode of arrival |
|
| Intake area |
|
| Triage | |
| Availability |
|
| Location |
|
| Triage officer |
|
| Protocol used |
|
| Disposition from triage |
|
| Physician staffing |
|
| Nurse staffing |
|
| Study design | |
| Sampling method | |
| Continuous sampling |
|
| Simple random sampling |
|
| Systematic random sampling |
|
| Convenience sampling |
|
| Study population |
|
| Patient information | |
| Patient demographics | |
| Population served |
|
| Patient age |
|
| Patient outcomes | |
| Length of stay |
|
| Inpatient admission rate |
|
| Mortality rate over a time interval, i.e., 24-h mortality rate |
|
| Mortality rate in the emergency facility |
|
| Patients brought-in-dead |
|
| Burden of disease | |
| Chief complaint |
|
| EC Diagnosis |
|
| Cause of death |
|
| Infectious disease |
|
| Traumatic conditions |
|
EC, emergency centre.
In conclusion, the data elements needed to provide an accurate understanding of the current state of emergency care in LMICs are not being routinely captured. The information that is collected is confounded by dissimilar practices for data acquisition and reporting. Many LMICs lack designated emergency centres altogether, and therefore the ability to accurately describe emergent patient presentations and the acute care delivered is lost. Researchers are bound by the constraints of previously collected administrative data, and lack the tools to initiate prospective data collection in order to answer clinical questions regarding the emergent and life-saving care they provide for their patients. Our goals are to increase the scope of publications from LMICs; facilitate data collection and analysis; improve the ability to translate findings of LMIC emergency care research to other similar settings; gain a better understanding of the burden of disease; and potentially improve patient outcomes by reducing the barriers to clinical research. To do so, we provide a framework for reporting results of emergency care research that is simple to use and which has been tailored to resource-constrained settings in LMICs.
The capture of standard data elements and use of common definitions for emergency care indicators facilitates the production of collaborative research networks, and valuable insights can result from analysis of aggregated emergency care data these network produce. Such shared methodology will result in a rapidly growing body of literature capable of painting a clearer picture of the current state of emergency care to inform policymaker decisions. We urge all emergency care researchers in LMICs to adopt such practices to facilitate the growth of such collaborations to help produce the evidence needed to combat the growing global burden of emergency conditions.
Our review aimed to identify all published emergency care literature originating from LMICs; however, our search strategy may have neglected reports that used alternative terminology to signify acute care medicine delivery without using the word stem ‘emerg-’ in the title, keywords, or abstract of articles. The overall paucity of studies that met our inclusion criteria remains our biggest limitation. Our goal during data collection was to record all reported data elements, but the overall infrequency of reporting outside of a few metrics, such as patient volume and demographics, limited the power to draw accurate conclusions from our results. We also acknowledge that the limited data available to researchers, likely related to the overall use of retrospective data collection relying on existing administrative records, is an overarching limitation to this research process, and one that our recommendations aim to change.
Conflicts of interest
The authors declare no conflicts of interest.
Dissemination of results
Results from this research were presented to attendees of the African Federation of Emergency Medicine consensus conferences, Addis Ababa 2014 and Cape Town 2015, both to the general assembly and small group discussion boards. Insights from the group discussions on how to improve data standards were incorporated into our recommendations.
Authors’ contributions
All authors provided substantial contribution to the conception of the work. SA, CYC, and ZO acquired and analysed the data for the study, and all authors interpreted of the data. SA and CYC prepared the manuscript and ZO, TAR, and HM revised the work. All authors gave their final approval of the version to be published.
Footnotes
Peer review under responsibility of African Federation for Emergency Medicine.
Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.afjem.2016.06.003.
Appendix A. Supplementary data
References
- 1.Latest ACEP national, State-level report cards cite ample room for improvement. ED Manage. 2014;26(3):25–27. [PubMed] [Google Scholar]
- 2.Chan T., Sherbino J., McMAP Collaborators The McMaster Modular Assessment Program (McMAP): a theoretically grounded work-based assessment system for an emergency medicine residency program. Acad Med. 2015 doi: 10.1097/ACM.0000000000000707. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 3.Strayer R.J., Shy B.D., Shearer P.L. A novel program to improve patient safety by integrating peer review into the emergency medicine residency curriculum. J Emerg Med. 2014;47(6) doi: 10.1016/j.jemermed.2014.07.035. 696–701.e2. [DOI] [PubMed] [Google Scholar]
- 4.Stevenson E.K., Rubenstein A.R., Radin G.T. Two decades of mortality trends among patients with severe sepsis: a comparative meta-analysis. Crit Care Med. 2014;42(3):625–631. doi: 10.1097/CCM.0000000000000026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boyle A.A., Ahmed V., Palmar C.R. Reductions in hospital admissions and mortality rates observed after integrating emergency care: a natural experiment. BMJ Open. 2012;2:e000930. doi: 10.1136/bmjopen-2012-000930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kellermann A.L., Hsia R.Y., Yeh C. Emergency care: then, now, and next. Health Aff (Millwood) 2013;32(12):2069–2074. doi: 10.1377/hlthaff.2013.0683. [DOI] [PubMed] [Google Scholar]
- 7.Nabel E.G., Braunwald E. A tale of coronary artery disease and myocardial infarction. N Engl J Med. 2012;366(1):54–63. doi: 10.1056/NEJMra1112570. [DOI] [PubMed] [Google Scholar]
- 8.Chang C.J., Abujaber S., Reynolds T., Camargo C.A., Obermeyer Z. Burden of emergency conditions and emergency care utilization: New estimates from 40 countries. EMJ. 2016 doi: 10.1136/emermed-2016-205709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.The World Bank. World development report 1993: investing in health, <https://openknowledge.worldbank.org/handle/10986/5976>; 1993.
- 10.Anderson P.D., Suter R.E., Mulligan T. World Health Assembly resolution 60.22 and its importance as a health care policy tool for improving emergency care access and availability globally. Ann Emerg Med. 2012;60(1):35–44. doi: 10.1016/j.annemergmed.2011.10.018. [DOI] [PubMed] [Google Scholar]
- 11.Razzak J.A., Kellermann A.L. Emergency medical care in developing countries: is it worthwhile? Bull World Health Organ. 2002;80(11):900–905. [PMC free article] [PubMed] [Google Scholar]
- 12.Hsia R., Razzak J., Tsai A.C. Placing emergency care on the global agenda. Ann Emerg Med. 2010;56(2):142–149. doi: 10.1016/j.annemergmed.2010.01.013. [DOI] [PubMed] [Google Scholar]
- 13.Hsia R.Y., Carr B.G. Measuring emergency care systems: the path forward. Ann Emerg Med. 2011;58(3):267–269. doi: 10.1016/j.annemergmed.2011.03.048. [DOI] [PubMed] [Google Scholar]
- 14.Hsia R.Y., Mbembati N.A., Macfarlane S. Access to emergency and surgical care in sub-Saharan Africa: the infrastructure gap. Health Policy Plan. 2012;27(3):234–244. doi: 10.1093/heapol/czr023. [DOI] [PubMed] [Google Scholar]
- 15.Kobusingye O.C., Hyder A.A., Bishai D. Emergency medical systems in low- and middle-income countries: recommendations for action. Bull World Health Organ. 2005;83(8):626–631. [PMC free article] [PubMed] [Google Scholar]
- 16.Mowafi H., Dworkis D., Bisanzo M. Making recording and analysis of chief complaint a priority for global emergency care research in low-income countries. Acad Emerg Med. 2013;20(12):1241–1245. doi: 10.1111/acem.12262. [DOI] [PubMed] [Google Scholar]
- 17.High level meeting on building resilient systems for health in Ebola-affected countries, 10–11 December 2014, Geneva, Switzerland. World Health Organization; Geneva: 2015. Available from: < http://www.who.int/csr/resources/publications/ebola/hs-meeting.pdf?ua=1>. [Google Scholar]
- 18.Obermeyer Z., Abujaber S., Makar M. Emergency care delivery in 60 low- and middle-income countries: systematic review and descriptive analysis. Bull World Health Organ. 2015 doi: 10.2471/BLT.14.148338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Reynolds T.A., Bisanzo M., Dworkis D. Research priorities for data collection and management within global acute and emergency care systems. Acad Emerg Med. 2013;20(12):1246–1250. doi: 10.1111/acem.12261. [DOI] [PubMed] [Google Scholar]
- 20.Hodkinson P.W., Wallis L.A. Emergency medicine in the developing world: a Delphi study. Acad Emerg Med. 2010;17(7):765–774. doi: 10.1111/j.1553-2712.2010.00791.x. [DOI] [PubMed] [Google Scholar]
- 21.Molyneux E., Ahmad S., Robertson A. Improved triage and emergency care for children reduces inpatient mortality in a resource-constrained setting. Bull World Health Organ. 2006;84(4):314–319. doi: 10.2471/blt.04.019505. < http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2627321/pdf/16628305.pdf> [accessed 15 November 2014] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Robison J.A., Ahmad Z.P., Nosek C.A. Decreased pediatric hospital mortality after an intervention to improve emergency care in Lilongwe, Malawi. Pediatrics. 2012;130(3):e676–e682. doi: 10.1542/peds.2012-0026. [DOI] [PubMed] [Google Scholar]
- 23.Mabiala-Babela J.R., Senga P. Consultations de nuit aux urgences pédiatriques du CHU de Brazzaville, Congo. Médecine Tropicale. 2009;69(3):281. [PubMed] [Google Scholar]
- 24.Miranda N.A., Rezende B.D., Oliveira J.S.F. Caracterização de crinças atendidas no pronto-socorro de um hospital universitário. Revista Electrônica Gestâo Saúde. 2013;4(1):1631–1645. [Google Scholar]
- 25.Shakhatreh H., Karim A., Al-Durgam M. Use and misuse of accident and emergency services at Queen Alia Military Hospital. J R Med Serv. 2003;10:44–47. [Google Scholar]
- 26.Garg R., Aggarwal S., Singh H. Study of the relation of clinical and demographic factors with morbidity in a tertiary care teaching hospital in India. Int J Crit Illness Inj Sci. 2013;3(1):12. doi: 10.4103/2229-5151.109411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hanewinckel R., Jongman H.P., Wallis L.A. Emergency medicine in Paarl, South Africa: a cross-sectional descriptive study. Int J Emerg Med. 2010;3(3):143–150. doi: 10.1007/s12245-010-0185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Periyanayagam U., Dreifuss B., Hammerstedt H. Acute care needs in a rural Sub-Saharan African Emergency Centre: a retrospective analysis. Afr J Emerg Med. 2012;2(4):151–158. [Google Scholar]
- 29.Ogah O.S., Akinyemi R.O., Adesemowo A. A two-year review of medical admissions at the emergency unit of a Nigerian tertiary health facility. Afr J Biomed Res. 2013;15(1):59–63. [Google Scholar]
- 30.Ka Sall B., Kane O., Diouf E. Les urgences dans un centre hospitalier et universitaire en milieu tropical. Le point de vue de l’anesthésiste réanimateur. Médecine Tropicale. 2002;62:247–250. [PubMed] [Google Scholar]
- 31.Adesunkanmi A.R., Akinkuolie A.A., Badru O.S. A five year analysis of death in accident and emergency room of a semi-urban hospital. West Afr J Med. 2001;21(2):99–104. [PubMed] [Google Scholar]
- 32.Ibeziako S.N., Ibekwe R.C. Pattern and outcome of admissions in the children’s emergency room of the University of Nigeria Teaching Hospital, Enugu. Niger J Paediatr. 2002;29(4):103–108. [Google Scholar]
- 33.Twomey M., Wallis L.A., Thompson M.L. The South African triage scale (adult version) provides valid acuity ratings when used by doctors and enrolled nursing assistants. Afr J Emerg Med. 2012;2(1):3–12. doi: 10.1016/j.ienj.2011.08.002. [DOI] [PubMed] [Google Scholar]
- 34.Twomey M., de Sá A., Wallis L.A. Inter-rater reliability of the South African Triage Scale: assessing two different cadres of health care workers in a real time environment. Afr J Emerg Med. 2011;1(3):113–118. [Google Scholar]
- 35.Clark M., Spry E., Daoh K. Reductions in inpatient mortality following interventions to improve emergency hospital care in Freetown, Sierra Leone. PLoS One. 2012;7(9):e41458. doi: 10.1371/journal.pone.0041458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bell C.M., Redelmeier D.A. Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Engl J Med. 2001;345:663–668. doi: 10.1056/NEJMsa003376. [DOI] [PubMed] [Google Scholar]
- 37.Bell D., Lambourne A., Percival F. Consultant input in acute medical admissions and patient outcomes in hospitals in England: a multivariate analysis. PLoS One. 2013;8(4):e61476. doi: 10.1371/journal.pone.0061476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Aylin P., Yunus A., Bottle A. Weekend mortality for emergency admissions. A large, multicentre study. Qual Saf Health Care. 2010;19:213–217. doi: 10.1136/qshc.2008.028639. [DOI] [PubMed] [Google Scholar]
- 39.Crisp N., Chen L. Global supply of health professionals. N Engl J Med. 2014;370(10):950–957. doi: 10.1056/NEJMra1111610. [DOI] [PubMed] [Google Scholar]
- 40.Peres R.R., Lima S.B.S., de Souza Magnago T.S.B. Perfil clinico-epidemiologico dos pacientes internados no pronto-socorro de um hospital universitario. Rev Saúde (Santa Maria) 2013;39(1):77–86. [Google Scholar]
- 41.Coelho M.F., Chaves L.D.P., Anselmi M.L. Analysis of the organizational aspects of a clinical emergency department: a study in a general hospital in Ribeirao Preto, SP, v. Revista Latino-Americana de Enfermagem. 2010;18(4):770–777. doi: 10.1590/s0104-11692010000400016. [DOI] [PubMed] [Google Scholar]
- 42.Ribeiro R.C.H.M., Rodrigues C.C., Canova J.C.M. Stay and outcome of the clinical and surgical patient in the emergency service. Rev Enferm (Lisboa) 2013;7(9):5426–5432. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.