Abstract
Introduction
With the widespread availability of a vast number of chemicals and drugs, acute poisoning is a common medical emergency worldwide. In spite of the success of interventions to prevent toxic ingestions, acute poisoning continues to be an important public health problem. Because of weak regulations and limited health care services in developing countries, adverse outcomes from poisoning are more prevalent than in the developed world. Due to the limited Ethiopian literature on this topic, the primary objective of this study was to evaluate and report poisoning cases, their management and outcome in northwest Ethiopia.
Methods
This is a retrospective study of all poisoning cases admitted and managed in the emergency centres of Gondar Teaching Referral Hospital and Metema and Debark district hospitals, from September 2010 to December 2014. Data was collected through retrospective chart review of patients who were admitted due to poisoning.
Results
There were 543 registered poisoning cases listed in the registry during the study period, of which 344 cases (63.4%) had complete data and were included in the final analysis. There were 48,619 emergency centre visits during the study period, with poisoning cases accounting for 1.1%. Females (60%) were predominant among intentional as well as unintentional poisoning cases. Patients between 15 and 24 years of age accounted for 55% of the cases. Patients poisoned with organophosphate and bleaching agents accounted for 35% and 25%, respectively. Among the poisoning patients, 74% were treated with decontamination, while those exposed to organophosphate were treated with atropine 45.5% (55/121) of the time.
Discussion
Young females comprise a group at increased risk for suicidal poisonings. As a developing nation, pesticide and bleaching agents remain a significant cause of acute poisonings in Ethiopia. Intentional poisoning remains the most significant identified cause of poisoning overall.
Abstract
Introduction
Avec la disponibilité largement répandue d’un grand nombre de produits chimiques et de médicaments, les intoxications aiguës constituent une urgence médicale fréquente partout dans le monde. En dépit du succès des interventions visant à prévenir l’ingestion de substances toxiques, l’intoxication aiguë reste un problème de santé publique important. En raison de la faiblesse des réglementations et des services de soins de santé limités dans les pays en voie de développement, les effets indésirables des intoxications y prévalent davantage que dans le monde développé. En raison des limites de la littérature éthiopienne sur cette question, le principal objectif de cette étude était d’évaluer et de rendre compte des cas d’intoxication, de leur traitement et de leurs conclusions dans le Nord-ouest de l’Ethiopie.
Méthodes
Cette étude est une étude rétrospective de tous les cas d’intoxication ayant fait l’objet d’une admission et d’un traitement dans les services des urgences de l’hôpital universitaire de Gondar et des hôpitaux de district de Metema et de Debark de septembre 2010 à décembre 2014. Des données ont été recueillies au moyen d’un examen rétrospectif des dossiers de patients admis pour intoxication.
Résultats
543 cas d’intoxication ont été inscrits dans le registre au cours de la période couverte par l’étude, 344 dossiers (63,4%) qui disposaient de données complètes ont été inclus dans l’analyse finale. Au cours de la période à l’étude, 48 619 visites ont été enregistrées aux services des urgences, les cas d’intoxication totalisant 1,1% de ces visites. Les femmes (60%) étaient prédominantes, tant pour les cas d’empoisonnement intentionnel que d’intoxication non intentionnelle. Les patients âgés de 15 à 24 ans constituaient 55% des cas. Les patients souffrant d’une intoxication aux organophosphates et agents blanchissants totalisaient respectivement 35% et 25% des cas d’intoxication. Parmi les patients souffrant d’intoxication, 74% étaient traités par voie de décontamination et ceux exposés aux organophosphates étaient traités à l’atropine dans 45,5% des cas (55/121).
Discussion
Les jeunes femmes constituent un groupe présentant un risque accru de suicide par empoisonnement. En raison de sa situation de pays en voie de développement, les pesticides et agents de blanchiment restent une cause significative d’intoxication aiguë en Ethiopie. Les empoisonnements intentionnels restent la cause d’intoxication globale la plus importante.
African relevance
-
•
Poisoning is a relatively common problem throughout Africa.
-
•
Female patients and young people accounted for the majority of the cases.
-
•
Organophosphates were responsible for the majority of the deaths.
Introduction
Widespread accessibility of chemicals and drugs worldwide contributes to common medical emergencies due to accidental and intentional poisonings [1]. In spite of the success of interventions to prevent toxic ingestions, acute poisoning continues to be an important public health problem [2]. Poison control centres in the United States of America handle an average of one poison exposure every 15 s [3]. Unfortunately, not all countries are equally equipped to treat such cases; many locales may lack the necessary antidotes, screening tests or proper treatment protocols.
Poisoning is very common in low- and middle-income countries; and, because of weak regulations and poor healthcare services, the adverse consequences of poisoning are far greater than in high-income countries [4]. The recently published Global Burden of Disease Study revealed that worldwide, unintentional poisoning was responsible for an estimated 180,000 deaths in 2010. This translates to a mortality rate of 2.6 per 100,000 inhabitants, making poisoning a top 50 cause of death worldwide [5].
Appropriate emergency centre treatment of acute poisoning requires accurate assessment and prompt therapy [6]. The greatest chance for improved outcomes occurs with early diagnosis and treatment [7]. In Ethiopia, few studies have investigated the pattern of acute poisoning cases. This study aims to provide insight into the epidemiology and existing treatment measures of cases of acute poisoning in the North Gondar Zone of northwest Ethiopia.
Methods
This was a retrospective chart review to describe the epidemiology of poisoning evaluated in governmental public hospitals in northwest Ethiopia. This study was conducted in North Gondar administrative zone governmental hospitals.
According to the 2007 Census conducted by the Central Statistical Agency of Ethiopia, the North Gondar Zone in northwest Ethiopia has a population of approximately 3 million people, of whom 51% are males and 49% are females. In this area of approximately 46,000 square kilometres, about 84% of the population lives in rural areas [8]. The main ethnic group reported in Semien Gondar was the Amhara (97.84%); all other ethnic groups made up 2.16% of the population. Amharic was spoken as a first language by 98%. Ninety-five percent practiced Ethiopian Orthodox Christianity, and 4.3% of the population said they were Muslim.
In the North Gondar Zone, three public hospitals with a combined bed capacity of about 2500 provide service for approximately 5 million people, including patients from other regions and zones. These hospitals include University of Gondar Teaching Hospital and Metema and Debark district hospitals. Patients treated at the district hospitals are typically managed by general practitioners and at the university hospital by general practitioners and internal medicine residents.
All patients with acute poisoning presenting to and managed in the emergency centres of three public hospitals in northwest Ethiopia between September 2010 and December 2014 were reviewed for inclusion. Patients transferred from district to referral hospital were only counted in the study once with data describing final outcome and disposition. Patients were not excluded for multiple distinct presentations for poisoning during the study period.
Data was collected by reviewing records from the hospital emergency centre patient registration logs over the four-year and three-month study period. Using a pre-structured format, treatment records for patients identified with poisoning related diagnoses in the emergency centre registers were retrieved and were reviewed for gender, age, season, time of ingestion, causes of poisoning, types of poisons, poisoning route, patient status (conscious, unconscious and semiconscious), treatment, duration of hospital stay and outcome of the treatment. Where charts could not be located or the chart contained incomplete records for the study variables, the visit was excluded. All of the data was analysed using the Statistical Package for Social Science (SPSS) version 20.0. Descriptive statistical tools were used to report percentages and frequency distributions tables. One-way Analysis of Variance (ANOVA) was used to compare the significance of seasonal distribution on this case.
Ethical clearance was acquired from the University of Gondar College of Medicine and Health Science Ethical Review Committee (No: 248/07) and permission to conduct the study at the hospital was obtained separately from each hospital administration. College of Medicine and Health Science Ethical Review Committee waived the need for subject informed consent.
Results
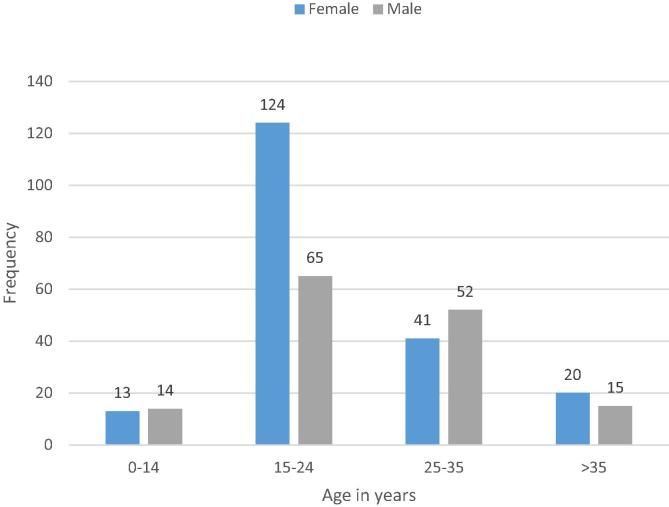
Over the study period, 543 poisoning cases were listed in the hospital registries. Of these, only 344 cases (63.4%) had complete data to be included in the final analysis. There were a total of 48,619 patient visits to the three emergency centres during the study period, with poisoning cases accounting for about 1.1% of these emergency centre visits. Females comprised 60% of all intentional as well as unintentional poisoning cases. Ages ranged from three months to 67 years (mean 23.4, SD of 10.75). Patients aged 15 to 24 years old accounted for 55% of the cases (Fig. 1). Paediatric cases (children aged 0–14 years) accounted for about 7% of the total cases.
Fig. 1.
Frequency of poisonings compared with age distribution and sex. The bar graph indicates the frequency of poisoning cases with their age and sex distribution (n = 344). The blue colour indicates the number of females and the red the number of males in each group.
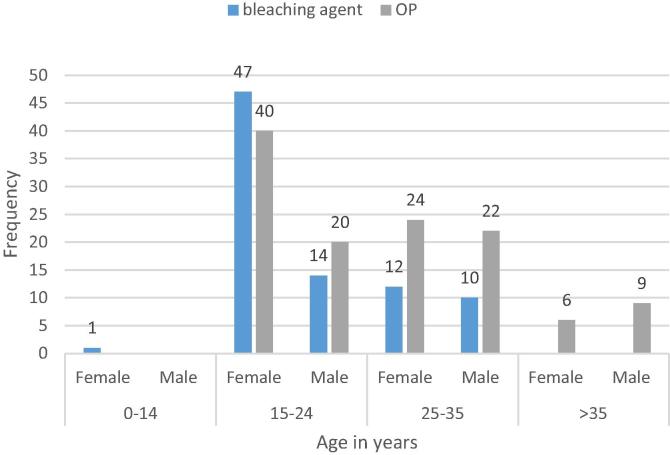
Data regarding intentionality of the poisoning was only available in approximately 31% (105/344) of our cases. Approximately 20% (71/344) of the total number of cases included in this review were known to be intentional. Among the subset of cases where intentionality was documented, females accounted for 47.6% (50/105) of these intentional cases and were found to ingest the most common agents at rates higher than men. In our study, organophosphate pesticides were ingested by women in 57.9% (70/121) of the cases and bleach was ingested by women in 71.4% (60/84) of our cases. When recorded, the main reasons for intentional poisoning were cited to be family disputes (77%) (Table 1). The causative poison was documented in 87% (298/344) of cases. Ingestion of organophosphate pesticides and bleach accounted for 35% (121/344) and 25% (84/344) of cases, respectively (Fig. 2). Other types of poisoning occurred using prescription medications, organochlorines, foodborne toxins, carbon monoxide, alcohol, herbal medications, hydrogen peroxide, kerosene, and benzene (Table 2). The main sources of poison were the home and hotels, accounting for 19% and 3% respectively.
Table 1.
Reasons for intentional poisoning (n = 62).
| Reason for intentional poisoning | Frequency | Percentage |
|---|---|---|
| Family dispute | 47 | 77.4 |
| Love affairs | 5 | 8.1 |
| Psychiatry disorder | 4 | 6.5 |
| Unplanned pregnancy | 2 | 3.2 |
| Being an HIV patient | 2 | 3.2 |
| Exam failure & university dismissal | 1 | 1.6 |
| Unemployment | 1 | 1.6 |
Fig. 2.
The two most common poisoning agents with their sex and age distribution. The bar graph indicates the two most common poisoning agents, bleach and organophosphates, with respect to age and sex distribution (n = 205). The blue colour indicates the frequency of bleach and the red the frequency of organophosphate (OP) in each age range.
Table 2.
Type of acute poisoning (n = 344).
| Type of poisoning | Frequency | Percent |
|---|---|---|
| Organophosporous | 121 | 35.2 |
| Bleach (sodium hypochlorite) | 84 | 24.4 |
| Prescription drugs | 21 | 6.1 |
| Organochlorine | 19 | 5.5 |
| Food poisoning | 18 | 5.2 |
| Carbon monoxide | 17 | 4.9 |
| Alcohol | 5 | 1.5 |
| Herbal medication | 4 | 1.2 |
| Hydrogen peroxide | 4 | 1.2 |
| Kerosene | 3 | 0.9 |
| Benzene | 2 | 0.6 |
| Unknown chemicals | 46 | 13.4 |
The gastrointestinal and respiratory tracts were the only routes of poisoning observed. Poisoning by ingestion and inhalation accounted for 82% and 6% of cases, respectively. There was no significant seasonal variation (p = 0.76). The seasonal distribution of all poisoning cases was as follows: spring (26.8%), winter (28.1%), summer (19.8%) and monsoon (22.3%). When separated by month, January showed the highest incidence (11%) and March had the lowest (4%). For the two most common types of poisoning, organophosphate poisoning occurred most in September and bleach occurred in October and January.
Fewer than 15% of the patients arrived to the emergency centre unconscious. Decontamination treatment was utilized in 74% (255/344) of the patients reviewed. Gastric lavage was used in 22% (76/344) and activated charcoal in 5.8% (20/344), while those who took organophosphorus were treated with atropine 45.5% (55/121) of the time. One hundred and five patients received gastric lavage and the time to the procedure was variable. When the timing was known, 36.8% (28/76) received gastric lavage within one hour of ingestion and 47.4% (36/76) within two hours. Another 14.5% (11/76) were known to receive gastric lavage at a time of more than two hours. In one extreme case, gastric lavage was attempted at 72 h after ingestion. Another 30 patients received gastric lavage, though time was not recorded. Of the 344 patients included in our study, 56% (194/344) were admitted and 43% (149/344) were treated and released from the emergency centre. Women accounted for 67% (130/344) of the admitted and 45% (67/344) of the treated and released patients versus 33% (64/344) and 55% (82/344) respectively for men. The majority of admitted patients (68%) had a hospital length of stay (LOS) of less than one day. There was one mortality (0.3%) of the total number of acute poisonings in this study. This patient succumbed to a polysubstance overdose of veterinary drugs and organophosphorus in response to a recent abortion.
Discussion
This study suggests that the incidence of acute poisoning in North Gondar is at least 1.1% of all emergency centre presentations. Despite incomplete data limiting analysis of all cases recorded in emergency centre log books, those poisonings included in the study still account for 0.7% of all emergency centre presentations. This number is higher than that reported by Abulla et al., who documented a 0.45% incidence of poisoning among emergency presentations in Ethiopia [9]. This difference might be partially explained by the increasing use of chemicals for agricultural productivity in the North Gondar Zone as well as expanding urbanization leading to increased family stressors, unemployment and growing university enrolment in the area. Similar rates of acute poisoning cases were reported in Turkey by se Zoz et al. (0.7% of all emergency admissions) [10]. Female patients and young people accounted for the majority of the cases in our study with 60% and 55% of the cases, respectively. Predominance of women and young people were also reported in studies in Sri Lanka and Nepal [11], [12].
Where intentionality was documented, intentional overdose in an attempt to commit suicide occurred in 20.6% (71/344) of our cases. This is in agreement with the findings described by Shaikh et al. [13]. Poisoning is a common method of attempting suicide because many people believe that poison can terminate life with minimal suffering [14]. In our study, motivations for suicide attempts were similar to that described by Soysal and colleagues (Table 2) [15]. Pokhrel et al. found that suicidal overdoses constituted most poisoning presentations in Nepal [12]. Organophosphates are responsible for the majority of deaths in most self-reported poisonings in Africa [16]. Data derived from the present study revealed 35.2% (121/344) of cases were due to organophosphate when a cause was known, injuring predominantly women (57.9% [70/121]). This was consistent with one previous study, but inconsistent with another in which males were more frequent abusers of organophosphates [17], [13]. These results indicate that public health measures to improve prevention of self-harm could potentially reduce morbidity and mortality related to such chemicals in the North Gondar Zone, with opportunities to encourage both proper personal protection and storage to avoid unintentional exposures, and to increase mental health support to reduce suicidal ingestions.
Route of exposure to toxins and specific agents encountered in our study were similar to other studies in the region [15]. We encountered 82% (283/344) oral ingestions and 6% (21/344) inhalational exposures and found that 6% (21/344) of poisoning incidents were due to medications, namely phenobarbital, amoxicillin, and paracetamol, which is also consistent with previous reports [18]. In the present study, 13% (46/344) of the substances implicated in poisoning cases were not identified. While polysubstance ingestions complicate the picture in both Ethiopia and worldwide, this may reflect the lack of capacity and technology in toxicological assessment in the healthcare systems of Ethiopia as well as a lack of complete record keeping. This is an issue recognized in other developing countries, as seen by Kaale et al. in Tanzania [4]. Limitations in history, lack of skill by clinicians to identify exposures based on toxidromes, ambiguity of substances taken by the patient, and lack of laboratory capacity to facilitate the diagnosis all contribute to the difficulties in confirming the specific substances causing poisoning.
The hospital LOS was less than one day (68%) in the majority of cases, which was similar to studies done in Nepal by Pokhrel et al. [12]. Like other studies showing that death was rare and fewer than 1% of paediatric poisoning were clinically serious, there were no deaths amongst our paediatric patients. Most poisoning was due to unintentional ingestion and was due to improper storage in the home (19% of cases, 66/344). Prevention of such exposures can be promoted at the community level by disseminating information about hazardous substance control at home and in other places [19]. Our overall mortality rate of 0.3%. This rate was much lower than another Ethiopian study by Dessalew focusing on poisoned patients presenting to the capital city referral hospital, which found a mortality rate of 9% in a more urban population [20].
Based on our chart review, clinicians attempted to manage acute poisonings in agreement with general toxicology principles. However, there is a lack of approved treatment protocols at both hospital and national levels to guide these practitioners, and there was often deviation from accepted international best practices [21]. Worldwide, gastric lavage for decontamination of acutely poisoned patients is typically recommended only for a patient presenting within one hour of ingesting a potentially life threatening agent [22]. Unfortunately in our study, clinicians used gastric lavage irrespective of time of ingestion, with fewer than 20% documented as receiving gastric lavage within the recommended one hour from exposure, and in one case up to 72 h after. This might be due to lack of training and knowledge, lack of other treatment options, or lack of available specific antidotes at the time of management. In the case of organophosphate exposures, atropine was regularly administered [23].
This retrospective review of hospital documents is subject to several additional shortcomings that should be noted explicitly. Not all cases of poisoning in North Gondar Zone are brought to an emergency centre of these hospitals, and this may have lead to an underestimation of the prevalence of acute poisonings. In addition, all cases of poisoning may not have been identified as such in the records. Some cases may have been misclassified or missed by clinicians. Furthermore, only 63% (344/543) of the reviewed charts with a presentation for poisoning were available for review, and of those intentionality was unknown for 69.5% (239/344) of patients. Therefore, we must be very careful to avoid making conclusions about the intentionality of all poisonings in the area based on these results. The low mortality rate might also be related to poor documentation, since our study excluded more than one third of patients registered with a diagnosis related to acute poisoning due to incomplete records. Furthermore, it is possible that severe cases may have died at home without presenting to the hospital. In this study, clinicians attempted to treat poisoning cases regularly but there is little data on treatment available for each case.
In conclusion, our study suggests that acute poisoning is more common in Northern Ethiopia than previously documented, and the incidence may be rising. Youths remain most vulnerable to acute poisoning in the North Gondar region, especially young females who represent the most at risk group for intentional self-harm by poisoning. The way cases were managed was generally justifiable and the overall mortality from acute poisoning was low in our sample. However, clinicians lack specific treatment guidelines and protocols that could improve management and the government should prepare and avail these documents at all health institutions to improve the management. Primary prevention of self-harm through improving both public awareness on proper handling of chemicals and prescribed agents, and accessibility of appropriate mental health services are highly recommended.
Conflicts of interest
The study was funded by a grant from the University of Gondar, Ethiopia. The authors declare no further conflicts of interest.
Dissemination of results
The results were disseminated at the University of Gondar Silver Jubilee of Annual Staff and Students Research Conference in Gondar, Ethiopia (June 19–20, 2015), and at the 35th Ethiopian Pharmaceutical Association Annual Conference in Addis Ababa, Ethiopia (August 5–8, 2015).
Authors’ contributions
GM has made substantial contributions to conception and design, acquisition of data, interpretation of data and revising it critically for important intellectual content. MB has been involved in drafting the manuscript. EM has been involved in drafting the manuscript and revising it critically for important intellectual content. AS has given final approval of the version to be published. ED contributed to the analysis of data and manuscript revision.
Acknowledgements
The authors would like to thank the University of Gondar, Ethiopia for the support and funding for this research. We would also like to thank Anna Bazinet for language editing.
Footnotes
Peer review under responsibility of African Federation for Emergency Medicine.
References
- 1.Santosh K.S., Sandesh K.V., Jayram P. Analysis of various retrospective poisoning cases in tertiary care Hospital in Tamil Nadu, Indian. J Pharm Pract. 2013;6(3) [Google Scholar]
- 2.Pillay V. Current views on antidotal therapy in managing cases of poisoning and overdose. JAPI. 2008;56 [PubMed] [Google Scholar]
- 3.Betten D.P., Vohra R.B., Cook M.D. Antidote use in the critically ill poisoned patient. J Intensive Care Med. 2006;21:255–277. doi: 10.1177/0885066606290386. [DOI] [PubMed] [Google Scholar]
- 4.Kaale E., Mori A., Risha P. A Retrospective study of poisoning at Muhimbili National Hospital in Dar-Es Salaam, Tanzania. J Public Health Front. 2013;2(1):21–26. [Google Scholar]
- 5.Khan N.U., Pérez-Núñez R., Shamim N.A. Intentional and unintentional poisoning in Pakistan: a pilot study using the Emergency Departments surveillance project. BMC Emergency Med. 2015;15(2) doi: 10.1186/1471-227X-15-S2-S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hoving D.J.V., Veale D.J.H., ller G.F.M. Clinical review: emergency management of acute poisoning. Afr J Emergency Med. 2011;1:69–78. [Google Scholar]
- 7.Boyle J.S., Bechtel L.K., Holstege C.P. Management of the critically poisoned patient. Scand J Trauma Resuscitation Emergency Med. 2009;17(29) doi: 10.1186/1757-7241-17-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.CSA . 2007. Compilation of economic statistics in Ethiopia. [Google Scholar]
- 9.Abulla T.Y.W. The pattern of acute poisoning in a teaching hospital, north-west Ethiopia. Ethiop Med J. 2006;44(2):183–189. [PubMed] [Google Scholar]
- 10.se Z.O.z., AyogÏlu F. Etiological and demographical characteristics of acute adult poisoning in Ankara, Turkey. Hum Exp Toxicol. 1999;18:614–618. doi: 10.1191/096032799678839446. [DOI] [PubMed] [Google Scholar]
- 11.Senarathna L., Jayamanna S.F., Kelly P.J. Changing epidemiologic patterns of deliberate self poisoning in a rural district of Sri Lanka. BMC Public Health. 2012;12(593) doi: 10.1186/1471-2458-12-593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pokhrel D., Pant S., Pradhan A. A comparative retrospective study of poisoning cases in central, zonal and district hospitals. Kathmandu Univ J Sci Eng Technol. 2008;1(5):40–48. [Google Scholar]
- 13.Ali P., Anwer A., Bashir B. Clinical pattern and outcome of organophosphorus poisoning. JLUMHS. 2012;11(1) [Google Scholar]
- 14.Zaheer M.S., Aslam M., Gupta V. Profile of poisoning cases, at a north indian tertiary care hospital. Health Popul Perspect Issues. 2009;32(4):176–183. [Google Scholar]
- 15.Soysal D., Karakuş V., Soysal A. Evaluation of cases with acute organophosphate pesticide poisoning presenting at a tertiary training hospital emergency department: intoxication or suicide? JAEM. 2011;10:156–160. [Google Scholar]
- 16.Daly F.F.S., Little M., Murray L. A risk assessment based approach to the management of acute poisoning. Emerg Med J. 2006;23:396–399. doi: 10.1136/emj.2005.030312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eddleston M., Dawson A., Karalliedde L. l. Early management after self-poisoning with an organophosphorus or carbamate pesticide – a treatment protocol for junior doctors. Crit Care. 2004;8 doi: 10.1186/cc2953. R391-R7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Malangu N., Ogunbanjo G. A profile of acute poisoning at selected hospitals in South Africa. South Afr J Epidemiol Infect. 2009;24(2):14–16. [Google Scholar]
- 19.Schwartz L., Howland M.A., Mercurio-Zappala M. The use of focus groups to plan poison prevention education programs for low-income populations. Health Promotion Pract. 2003;4(3):340–346. doi: 10.1177/1524839903004003019. [DOI] [PubMed] [Google Scholar]
- 20.Desalew M., Aklilu A., Amanuel A. Pattern of acute adult poisoning at Tikur Anbessa specialzed teaching hospital, a retrospective study, Ethiopia. Hum Exp Toxicol. 2011;30(7):523–527. doi: 10.1177/0960327110377520. [DOI] [PubMed] [Google Scholar]
- 21.Aggarwal P., Handa R., Wali J.P. Acute poisoning – management guidelines. J Indian Acad Clin Med. 2004;5(2):142–147. [Google Scholar]
- 22.Greene S.L., Dargan P.I., Jones A.L. Acute poisoning: understanding 90% of cases in a nutshell. Postgrad Med J. 2005;81:204–216. doi: 10.1136/pgmj.2004.024794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Eddleston M., Buckley N.A., Eye P. Management of acute organophosphorus pesticide poisoning. Lancet. 2008;371:597–607. doi: 10.1016/S0140-6736(07)61202-1. [DOI] [PMC free article] [PubMed] [Google Scholar]