Abstract
Introduction
Injuries account for 10% of the global burden of disease, resulting in approximately 5.8 million deaths annually. Trauma registries are an important tool in the development of a trauma system; however, limited resources in low- and middle-income countries (LMIC) make the development of high-quality trauma registries challenging. We describe the development of a LMIC trauma registry based on a robust retrospective chart review, which included data derived from prehospital, emergency centre and inpatient records.
Methods
This paper outlines our methods for identifying and locating patients and their medical records using pragmatic and locally appropriate record linkage techniques. A prehospital database was queried to identify patients transported to University Teaching Hospital – Kigali, Rwanda from December 2012 through February 2015. Demographic information was recorded and used to create a five-factor identification index, which was then used to search OpenClinic GA, an online open source hospital information system. The medical record number and archive number obtained from OpenClinic GA were then used to locate the physical medical record for data extraction.
Results
A total of 1668 trauma patients were transported during the study period. 66.7% were successfully linked to their medical record numbers and archive codes. 94% of these patients were successfully linked to their medical record numbers and archive codes were linked by four or five of the five pre-set identifiers. 945 charts were successfully located and extracted for inclusion in the trauma registry. Record linkage and chart extraction took approximately 1256 h.
Conclusion
The process of record linkage and chart extraction was a resource-intensive process; however, our unique methodology resulted in a high linkage rate. This study suggests that it is feasible to create a retrospective trauma registry in LMICs using pragmatic and locally appropriate record linkage techniques.
Abstract
Introduction
Les blessures sont responsables de 10% de la charge mondiale de morbidité, résultant sur environ 5,8 millions de décès par an. Les registres des traumatismes constituent un outil important pour le développement d’un système sur les traumatismes; cependant, les ressources limitées qui caractérisent les pays à revenu faible et intermédiaire font que le développement de registres des traumatismes de qualité est difficile. Nous décrivons le développement d’un registre des traumatismes dans les pays à revenu faible et intermédiaire à partir d’un examen rétrospectif approfondi des dossiers incluant des données tirées des registres pré-hospitaliers, des services d’urgence et des patients hospitalisés.
Méthodes
Cet article décrit les méthodes dont nous disposons pour identifier et localiser les patients et leurs dossiers médicaux en utilisant des techniques de couplage de dossiers pragmatiques et localement appropriées. Une base de données pré-hospitalières a été interrogée afin d’identifier les patients transportés à l’Hôpital universitaire de Kigali, au Rwanda, de décembre 2012 à février 2015. Les informations démographiques ont été enregistrées et utilisées afin de créer un indice d’identification à cinq facteurs, utilisé ensuite pour mener une recherche dans OpenClinic GA, un système d’information hospitalière en open source accessible en ligne. Les numéros de dossiers médicaux et les codes d’archives obtenu par OpenClinic GA ont été ensuite utilisés pour localiser le dossier médical physique afin d’en extraire les données.
Résultats
Au total, 1668 patients ayant souffert de traumatisme ont été transportés au cours de la période à l’étude. 66,7% ont pu être couplés à leur numéro de dossier médical et code d’archive. 94% de ces patients ont pu être couplés à 4 ou 5 des cinq identifiants préétablis. 945 fichiers ont pu être localisés et extraits pour être intégrés au registre des traumatismes. Le couplage des dossiers et l’extraction des fiches ont nécessité environ 1 256 heures.
Conclusion
Le processus de couplage de dossiers et d’extraction des fiches a nécessité des ressources considérables; cependant, notre méthodologie unique a résulté sur un taux de couplage élevé. Cette étude suggère qu’il est possible de créer un registre des traumatismes rétrospectif dans les pays à revenu faible et intermédiaire en utilisant des techniques de couplage de dossiers localement appropriées.
African relevance
-
•
Trauma registries are an important tool in the development of a trauma system.
-
•
Few trauma registry publications come from the low- and middle income regions, particularly Africa.
-
•
Record linkage is one tool that can be used to help merge information from multiple sources.
Introduction
Injuries account for 10% of the global burden of disease, resulting in approximately 5.8 million deaths annually [1], [2]. While global morbidity and mortality from trauma has declined significantly since 1990, most of these improvements have been seen in high income countries [3].
Since 2004, the World Health Organization has advocated for improved trauma care particularly in low- and middle-income countries (LMIC) where trauma results in disproportionately high morbidity and mortality rates [4], [5]. In fact, researchers have found that patients with life-threatening but potentially treatable injuries are up to six times more likely to die in countries that lack an organised trauma system [6]. A 2012 review of recent trauma registry publications found few publications emanating from the developing world, particularly in sub-Saharan Africa. The authors also stressed the limited availability of information on the methodology used to develop the trauma registries [7].
Trauma registries are an important tool in the development of a trauma system. Registry data can be used to track health outcomes, assess the impact of system improvements, and compare providers or health facilities across geographic regions [8]. However, limited resources in LMICs make the development of high-quality trauma registries challenging. Barriers to implementation include: poor availability of high-quality or complete medical charts, lack of computerised medical records systems, and personnel limitations [5]. Furthermore, multiple documentation systems (i.e. prehospital run sheets, registry books, billing databases, and paper-based medical charts) which utilise non-integrated identification variables and contain disparate information compound the existing barriers. As a result, data linkage across systems and care settings is limited in the majority of LMICs.
Record linkage is one tool that can be used to help mitigate any discrepancies when merging information from multiple sources, including prehospital and hospital databases [9], [10], [11]. Record linkage techniques aim to identify pairs of records that describe the same patient, when unique identification numbers are lacking across systems. To do so, commonly available identification information, including name, date of birth, and sex, are used to categorise records as links, possible links, or non-links so that they can be appropriately merged to create more comprehensive data repositories.
Here we describe the development of a LMIC trauma registry based on a robust retrospective chart review, which included data derived from prehospital, emergency centre (EC) and inpatient records. This paper outlines our methods for identifying and locating patients and their medical records using pragmatic and locally appropriate record linkage techniques.
Methods
This retrospective chart review was conducted at University Teaching Hospital of Kigali (UTH-K) in Kigali, Rwanda. UTH-K is a 576-bed urban, tertiary-care teaching hospital. It is the primary trauma centre for a population of 1.1 million people in Kigali and serves as the primary academic referral centre for the entire country, a population of 10.5 million [12]. UTH-K has a 24-h EC that sees all adult patients with acute complaints, as well as paediatric and obstetric trauma patients. Available resources at UTH-K include 24-h surgical coverage, access to radiology services including X-ray, ultrasound and CT, and on-call orthopaedic neurosurgical services.
Patients were eligible for inclusion if they were transported by Service d’Aide Médicale Urgente (SAMU), the Rwandan prehospital service, to UTH-K for trauma during the 26-month period from December 2012 through February 2015. SAMU uses trained nurses and anaesthetists to provide prehospital care through a network of ambulances [13]. Patients who died en route to UTH-K and were subsequently registered were included. Exclusion criteria included patients transported for non-traumatic illness, including medical or obstetric complaints, as well as patients transported by SAMU to hospitals other than UTH-K.
SAMU has maintained an electronic database of each patient encounter since 2012. The original SAMU run-sheet is saved and contains additional data not stored in the electronic database. On arrival to the EC, patient names are recorded in a logbook. Shortly after arrival, patients are registered in OpenClinic GA, an online open source hospital information system, which is primarily used for billing but also contains some demographic information [14], [15]. Paper charts are used to document patient care while patients are in the EC or admitted to the hospital.
The SAMU electronic database was queried for all patient encounters classified as trauma response for type of case and UTH-K for transport destination. Paediatric patients were included, as were injured pregnant women, if they were originally classified as trauma response for type of case by the data-entry staff. To enhance capture of injured pregnant women, as this is a very high risk population, a second iterative evaluation was carried out whereby the database was queried for trauma as problem and obstetric-neonatal for type of case. Patients identified through this process were then included in the study.
Demographic information stored in the electronic SAMU database is not sufficient to provide a direct link to hospital medical records at UTH-K; however, medical records can be located if the patient’s name is recovered from the original run-sheet. SAMU IDs from the electronic database were used to locate the original SAMU run-sheet and recover the patient’s recorded name. Due to the potential for names to be incorrectly reported and recorded (particularly among severely injured patients), we collected additional available identification information in the SAMU database to create a composite index of patient identification information including: name, age, sex, home district, and date of service. The patient five-factor identification index was then used to search OpenClinic GA to obtain the patient’s medical record number (MRN) and Archive Code, which were needed to physically locate the paper medical record.
OpenClinic GA was used to create a list of patients that arrived to the UTH-K EC within a specified range of dates and who were either admitted or had a consultation during their EC course. This was the most efficient way to find a patient in OpenClinic GA. However, if a patient was seen in the EC and then discharged, they did not appear on this list and needed to be searched for individually. These patients were searched for using both first and last name. Due to difficulties with spelling of names and the prevalence of similar names, various search strategies were employed to identify the correct patient. This included switching the first and last names, using known, popular abbreviations, and narrowing search responses by home district. If the name variation algorithm was successful then the record was crosschecked against the four other aspects of the identification index. Occasionally, names were still not found. In these cases, the hospital billing clerks were consulted for assistance and the name was searched for in the EC logbook, a paper notebook in which all EC patients are recorded. In some cases, the EC logbook provided an MRN or more accurate spelling of the name, which could then be used to search OpenClinic GA.
Once patients were located within OpenClinic GA, we used pre-set criteria to confirm that the correct patient was being matched across records. Each patient needed to match across databases at a minimum of four of the five pre-set identifiers – name, age, sex, home district and date of service – in order to be considered links. A patient’s age was considered a match if it was within ±5 years of the age documented by SAMU. Date of service was considered a match if it was within ±1 calendar day of the documented transport date on the SAMU run-sheet. Charts that matched with less than four identifiers were reviewed by study investigators for injury type, time of day and situation to confirm that the correct chart was located.
An iterative review process was used to look for missing charts. OpenClinic GA was searched multiple times for patients we were unable to identify or for those that had missing MRNs or archive numbers. This was done to increase the proportion of patients we were able to link across various records and increase the likelihood that we would then be able to find the physical medical record. Additionally, medical records were not always located in the archive room. Various methods were used to locate the physical chart, including multiple searches of the archive room at various times during the study period and physical searches of the surgical, medical and intensive care units, where unsigned or incomplete charts are often stored.
Record linkage and demographic data extraction was completed by three of the co-authors as well as our in-country data manager/research assistant. Our research assistant was responsible for all primary data extraction with respect to each patient’s clinical course. He is fluent in English, French and Kinyarwanda, and has extensive medical background, which was essential for accurate data extraction.
Quality assurance testing was performed at four pre-determined intervals throughout the study. 10% of charts were randomly selected and reviewed by trained abstractors blinded to initial abstraction; the clinical course was re-abstracted and this data was entered into a separate database. A second research assistant, fluent in English, French and Kinyarwanda, and also with a medical background, was needed to translate charts for three of the co-authors who participated.
Cohen’s kappa (κ) and percent agreement were used to assess the inter-rater reliability (IRR) between initial and repeat abstraction, with higher values indicating greater IRR for both methods. Nine variables were used to assess IRR and included: age, sex, whether the triage form was completed and the EC chart was present in the file, documentation of EC visit date, type of trauma, ultimate EC disposition, and EC and inpatient length of stay. We set our quality threshold for IRR at a κ of 0.75, a percent agreement of 85%, or both. A quality improvement strategy was decided a priori: κ values below 0.75 would result in re-training [16]. The completeness of the data is reported as the median percentage of missing data for the nine variables that were compared in the IRR study; the interquartile range (IQR) and data range is also reported.
The number of patients identified through the process of record linkage and the number of charts found and extracted is reported as a percentage of all trauma patients transported to UTH-K by SAMU. The overall amount of time required for patient identification and chart extraction is estimated.
Ethics approval was obtained from Rhode Island Hospital Institutional Review Board, the Rwandan National Ethics Committee, and the UTH-K Research Committee (study number: EC/CHUK/175/2015). Informed consent was waived as this was a retrospective chart review.
Results
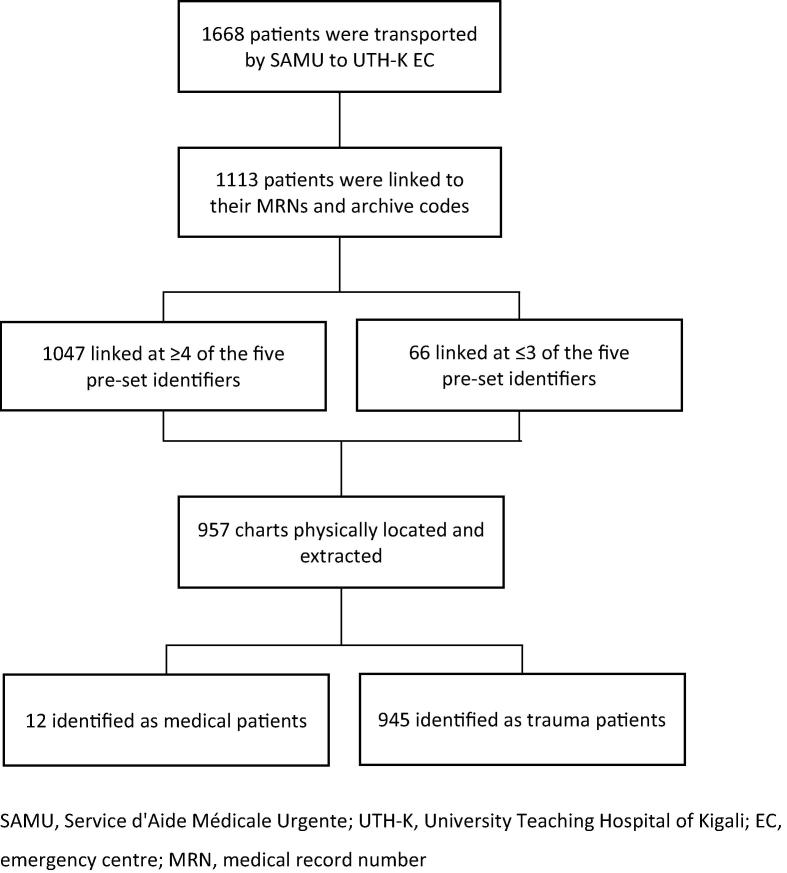
A total of 1668 trauma patients were transported by SAMU to UTH-K during the study period. Four duplicates were eliminated. 1113 of the 1668 patients (66.7%) were successfully linked to their MRNs and archive codes (Fig. 1).
Figure 1.
Flow diagram.
94% of patients (1047/1113) who were successfully linked to their MRNs and archive codes were linked by four or five of the five pre-set identifiers. An additional 66 (5.9%) were matched by only three criteria or less and required further investigation. These 66 charts underwent detailed review by investigators.
Of the 1113 patients we were able to identify, 957 charts were physically located and abstracted for inclusion in the study. Twelve charts were ultimately identified as medical patients and removed. Overall, we were able to include 56.6% (945/1668) of all trauma patients who were transported by SAMU to UTH-K during the study period.
Of the 1668 patients transported to UTH-K during the study period, 91 were identified as ‘unknown’ and did not have corresponding first or last names documented. Unfortunately, we were not able to locate MRNs or archive numbers for this subset of trauma patients and, thus, do not know how they might differ from the larger population.
Our primary research assistant spent 1256 h on record linkage and chart extraction during the study period. The number of hours spent on record linkage and data extraction was recorded on a daily basis. A second research assistant provided eight hours of translation work with one of three co-authors who re-extracted data as part of the IRR component. Four of the United States-based co-authors on this study provided 32 weeks of in-country support spanning seven visits to Rwanda. While this study was a primary objective of these visits, the authors also provided support to other on-going educational and research efforts based at UTH-K.
Overall, 10.1% of charts were re-extracted by one of three co-authors trained in data abstraction. Nine variables were compared across charts (six categorical and three continuous). The kappa was very high, indicating agreement across data abstractors (Table 1). Additionally, these nine variables were analysed for completeness. Overall, the median percentage of missing data was 0.74% (IQR = 8.2; range 0.0%–33.8%).
Table 1.
Inter-rater reliability.a
| Kappa | Lower 95% CI | Upper 95% CI | p | |
|---|---|---|---|---|
| Categorical weighted average | 96.8 | 95.0 | 98.5 | <0.0001 |
| Continuous weighted average | 96.1 | 93.3 | 99.0 | <0.0001 |
| Overall weighted average | 96.8 | 95.3 | 98.2 | <0.0001 |
CI, confidence interval.
This is derived from 10.1% of cases and based on nine variables (six categorical and three continuous).
Discussion
Overall, 1113 patients were correctly identified and 945 charts were extracted according to the methods described as part of an effort to develop a retrospective trauma registry in Kigali, Rwanda. While tracking patients through their prehospital, emergency centre and inpatient hospital care proved challenging, we believe we developed robust methodology to ensure that we were extracting the correct patient data.
Compared to other studies investigating the prevalence of trauma within LMICs, our methodology resulted in a high linkage rate [17], [18], [19], [20], [21], [22]. Overall, we were able to link and locate charts for over half of the patients who were transported to UTH-K during the study period. Many other recent trauma studies do not provide detailed information about the percentage of charts that were successfully located [17], [18], [19], [20]. Two recent studies by Thanni et al. and Casey et al. reported rates of 39.5% and 81.6%, respectively [21], [22]. This suggests that our unique methodology is feasible in a low-resource setting with limited technologic support; however, it is important to realise that the process of patient identification and chart extraction was a human resource-intensive process. Overall, our research assistant contributed 1256 h toward record linkage and data extraction over a period of one year.
Additionally, since medical charts were often documented in more than one language, filled with inconsistent abbreviations, and lacked vital information, it was imperative that our research assistant was fluent in French, English and Kinyarwanda, and had significant medical knowledge.
Furthermore, our study covered a 26-month time period and included patients who arrived throughout the day. In comparison, other trauma registries conducted in LMICs often limited enrolment to brief periods of time [17], [19], [23] or did not provide a clear methodological outline of their enrolment process [24]. While prospective studies are generally viewed as superior to retrospective studies, prospective data collection in LMICs typically involves the hiring of a research assistant who may only be available for certain hours of the day, thereby missing patients who arrive on weekends or overnight, or requires clinical staff to complete additional forms. This may be limited by varying experience with research methods or enthusiasm for the study at hand.
One important strength of our study methodology is the fact that we did not rely on a single demographic indicator to link charts. Instead, we used a composite index of available demographic information, and manually reviewed charts that did not link on at least four of the five indicators. While time consuming, we feel that this improves the overall accuracy of patient identification and record linkage. Furthermore, the inclusion of an IRR component, and the fact that the ultimate Cohen’s kappa was high, supports our confidence in the accuracy of data extraction.
There are also weaknesses associated with our design. Information was stored in various on-line databases and in multiple paper charts, all located in different areas of the hospital. Poor handwriting, misplaced charts, and incomplete documentation limited the information that could be gathered. Use of the iterative review process along with multi-lingual fluency of data extractors with medical training served to address some of these limitations. Additionally, unknown patients – many of whom were likely very ill or unable to provide information – were simply documented as “inconnu”, or unknown, by SAMU and in OpenClinic GA. As a result, these patients were frequently very difficult to track across the various databases and through their hospital stay.
Infrastructure limitations were also a major barrier. Intermittent high speed internet limited online database searches, and the physical infrastructure at UTH-K made locating medical charts difficult. Finally, the patients who were transported via SAMU only represent a subset of all trauma patients brought to UTH-K. This methodology did not include patients who arrived via private vehicle from the injury site or other hospitals or clinics, or those that were transported by the police, and as such the application of this trauma data collection methodology may not be generalisable to the large injured population at the UTH-K. Unfortunately, the total number of trauma patients presenting to UTH-K during the study period is not currently available due to the lack of a national trauma registry and limited computerised medical records. However, this is an area of on-going research at UTH-K.
This paper describes the methodology used in a retrospective chart review of trauma patients presenting to an urban, tertiary care centre. The methods resulted in data capture similar to that presented in prior reports and highlights barriers surrounding retrospective chart reviews, particularly in LMICs. Ultimately, poor record keeping not only hinders research opportunities, but it impairs a hospital’s ability to review charts for process improvements, educational interventions and patient outcomes. Moving forward, the trauma registry data will be used to inform educational and training programmes for our prehospital and emergency medicine colleagues at UTH-K.
Conflicts of interest
Funding for this study was provided by Brown University through the Framework in Global Health Scholarship and by University Emergency Medicine Foundation through the Resident Scholarly Development Awards Program.
Dissemination of results
Results from this study were shared with staff members at UTH-K Department of Emergency Medicine and the Department of Emergency Medicine at Brown University through informal presentations. Additionally, results were shared at ICEM in Cape Town, South Africa, in April 2016, as well as at various conferences in the United States.
Authors’ contributions
AK was primarily responsible for manuscript preparation, with assistance from LK. NG and AL developed the study protocols with assistance from JU, JN, and JB. AK, NG, AA, ZM were responsible for data collection and management. AA provided statistical support. All authors approved the final version of the manuscript.
Footnotes
Peer review under responsibility of African Federation for Emergency Medicine.
References
- 1.Lozano R., Naghavi M., Foreman K. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization Injuries and violence the facts. 2010. http://whqlibdoc.who.int/publications/2010/9789241599375_eng.pdf?ua=1 [Accessed online: 20 March 2016]
- 3.Haagsma J.A., Graetz N., Bolliger I. The global burden of injury: incidence, mortality, disability-adjusted life years and time trends from the Global Burden of Disease study 2013. Inj Prev. 2016;22(1):3–18. doi: 10.1136/injuryprev-2015-041616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hofman K., Primack A., Keusch G. Addressing the growing burden of trauma and injury in low- and middle-income countries. Am J Public Health. 2005;95(1):13–17. doi: 10.2105/AJPH.2004.039354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mock C., Juillard C., Brundage S. World Health Organization; Geneva: 2009. Guidelines for trauma quality improvement programmes. http://whqlibdoc.who.int/publications/2009/9789241597746_eng.pdf. [Accessed online: 15 March 2016] [Google Scholar]
- 6.Mock C.N., Adzotor K.E., Conklin E. Trauma outcomes in the rural developing world: comparison with an urban level I trauma centre. J Trauma. 1993;35:518–523. doi: 10.1097/00005373-199310000-00004. [DOI] [PubMed] [Google Scholar]
- 7.O’Reilly G.M., Joshipura M., Cameron P.A. Trauma registries in developing countries: a review of the published experience. Injury. 2013;44(6):713–721. doi: 10.1016/j.injury.2013.02.003. [DOI] [PubMed] [Google Scholar]
- 8.Moore L., Clark D.E. The value of trauma registries. Injury. 2008;39:686–695. doi: 10.1016/j.injury.2008.02.023. [DOI] [PubMed] [Google Scholar]
- 9.Aldridge R.W., Shaji K., Hayward A.C. Accuracy of probabilistic linkage using the enhanced matching system for public health and epidemiological studies. PLoS One. 2015;10(8):e0136179. doi: 10.1371/journal.pone.0136179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mumma B.E., Diercks D.B., Danielsen B. Probabilistic linkage of prehospital and outcomes data in out-of-hospital cardiac arrest. Prehosp Emerg Care. 2015;19(3):358–364. doi: 10.3109/10903127.2014.980474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gonçalves V.M., Pedroso R., dos Santos A.M. Following up crack users after hospital discharge using record linkage methodology: an alternative to find hidden populations. Biomed Res Int. 2015;2015:973857. doi: 10.1155/2015/973857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National Institute of Statistics; Rwanda: 2012. 2012 Population and housing census. http://statistics.gov.rw/publications/rphc4-thematic-report-population-size-structure-and-distribution. [Accessed online: 10 February 2015] [Google Scholar]
- 13.Enumah S., Scott J.W., Maine R., Uwitonze E. Rwanda’s model prehospital emergency care service: a two-year review of patient demographics and injury patterns in Kigali. Prehosp Disaster Med. 2016;22:1–7. doi: 10.1017/S1049023X16000807. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 14.Verbeke F. OpenClinic GA. http://sourceforge.net/projects/openclinic. [Accessed online: 25 March 2016].
- 15.Karara G., Verbeke F., Nyssen M. The role of hospital information systems in universal health coverage monitoring in Rwanda. Stud Health Technol Inform. 2015;216:193–197. [PubMed] [Google Scholar]
- 16.Reisch L.M., Fosse J.S., Beverly K. Training, quality assurance, and assessment of medical record abstraction in a multisite study. Am J Epidemiol. 2003;157(6):546–551. doi: 10.1093/aje/kwg016. [DOI] [PubMed] [Google Scholar]
- 17.Tadesse B., Tekilu S., Nega B. Pattern of injury and associated variables as seen in the emergency department at Tikur Anbessa Specialized Referral Hospital, Addis Ababa, Ethiopia. East Cent Afr J Surg. 2014;19(1):73–82. [Google Scholar]
- 18.Otieno T., Woodfield J.C., Bird P. Trauma in rural Kenya. Injury. 2004;35(12):1228–1233. doi: 10.1016/j.injury.2004.03.013. [DOI] [PubMed] [Google Scholar]
- 19.Seidenberg P., Cerwensky K., Brown R.O. Epidemiology of injuries, outcomes, and hospital resource utilisation at a tertiary teaching hospital in Lusaka, Zambia. Afr J Emerg Med. 2014;4(3):115–122. [Google Scholar]
- 20.Chalya P.L., Mabula J.B., Dass R.M. Injury characteristics and outcome of road traffic crash victims at Bugano Medical Centre in Northwestern Tanzania. J Trauma Manag Outcomes. 2012;6(1):1. doi: 10.1186/1752-2897-6-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Thanni L.O., Kehinde O.A. Trauma at a Nigerian teaching hospital: pattern and documentation of presentation. Afr Health Sci. 2006;6(2):104–107. doi: 10.5555/afhs.2006.6.2.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Casey E.R., Muro F., Thielman N.M. Analysis of traumatic injuries presenting to a referral hospital emergency department in Moshi, Tanzania. Int J Emerg Med. 2012;5(1):28. doi: 10.1186/1865-1380-5-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sonshine D.B., Shantz J., Kumah-Ametepey R. The implementation of a pilot femur fracture registry at Komfo Anokye Teaching Hospital: an analysis of data quality and barriers to collaborative capacity-building. World J Surg. 2013;37:1506–1512. doi: 10.1007/s00268-012-1726-6. [DOI] [PubMed] [Google Scholar]
- 24.Kobusingye O.C., Lett R.R. Hospital-based trauma registries in Uganda. J Trauma. 2000;48(3):498–502. doi: 10.1097/00005373-200003000-00022. [DOI] [PubMed] [Google Scholar]