Abstract
Introduction
Injury accounts for 9.6% of the global mortality burden, disproportionately affecting those living in low- and middle-income countries. In an effort to improve trauma care in Rwanda, the Ministry of Health developed a prehospital service, Service d’Aide Médicale Urgente (SAMU), and established an emergency medicine training program. However, little is known about patients receiving prehospital and emergency trauma care or their outcomes. The objective was to develop a linked prehospital–hospital database to evaluate patient characteristics, mechanisms of injury, prehospital and hospital resource use, and outcomes among injured patients receiving acute care in Kigali, Rwanda.
Methods
A retrospective cohort study was conducted at University Teaching Hospital – Kigali, the primary trauma centre in Rwanda. Data was included on all injured patients transported by SAMU from December 2012 to February 2015. SAMU’s prehospital database was linked to hospital records and data were collected using standardised protocols by trained abstractors. Demographic information, injury characteristics, acute care, hospital course and outcomes were included.
Results
1668 patients were transported for traumatic injury during the study period. The majority (77.7%) of patients were male. The median age was 30 years. Motor vehicle collisions accounted for 75.0% of encounters of which 61.4% involved motorcycles. 48.8% of patients sustained injuries in two or more anatomical regions. 40.1% of patients were admitted to the hospital and 78.1% required surgery. The overall mortality rate was 5.5% with nearly half of hospital deaths occurring in the emergency centre.
Conclusion
A linked prehospital and hospital database provided critical epidemiological information describing trauma patients in a low-resource setting. Blunt trauma from motor vehicle collisions involving young males constituted the majority of traumatic injury. Among this cohort, hospital resource utilisation was high as was mortality. This data can help guide the implementation of interventions to improve trauma care in the Rwandan setting.
Abstract
Introduction
Les blessures comptent pour 9,6% de la mortalité dans le monde, affectant de manière disproportionnée les personnes vivant dans les pays à revenu faible et intermédiaire. Dans un effort pour améliorer la prise en charge des traumatismes au Rwanda, le ministère de la Santé a développé un service préhospitalier, le Service d’Aide Médicale Urgente (SAMU), et mis en place un programme de formation à la médecine d’urgence. Cependant, peu d’informations sont disponibles sur les patients bénéficiant d’une prise en charge préhospitalière et de soins d’urgence ou sur les résultats obtenus. L’objectif était de développer une base de données préhospitalière et hospitalière couplée afin d’évaluer les caractéristiques des patients, les mécanismes des blessures, l’utilisation des ressources préhospitalières et hospitalières et les résultats pour les patients blessés recevant des soins intensifs à Kigali, au Rwanda.
Méthodes
Une étude de cohorte rétrospective a été menée à l’Hôpital universitaire de Kigali, principal centre de prise en charge des traumatismes au Rwanda. Des données ont été incluses sur tous les patients blessés transportés par le SAMU entre décembre 2012 et février 2015. La base de données préhospitalière a été couplée aux dossiers hospitaliers et les données ont été recueillies au moyen de protocoles standardisés par des archivistes formés. Les données démographiques, caractéristiques des blessures, soins intensifs, parcours hospitalier et résultats ont été inclus.
Résultats
1 668 patients ont été transportés pour des lésions traumatiques au cours de la période à l’étude. La majorité des patients étaient des hommes, à 77,7%. L’âge moyen était de 30 ans. Les collisions de véhicules motorisés étaient responsables de 75% des cas, 61,4% de ceux-ci impliquant des motos. 48,8% des patients souffraient de blessures au niveau de deux régions anatomiques ou plus. 40,1% des patients ont été hospitalisés, et 78,1% d’entre eux ont dû être opérés. Le taux de mortalité général était de 5,5%, près de la moitié des décès hospitaliers survenant au service des urgences.
Conclusion
Une base de données préhospitalière et hospitalière couplée a fourni des informations épidémiologiques essentielles décrivant les patients en traumatologie dans un environnement caractérisé par de faibles ressources. Les traumatismes contondants liés à des collisions de véhicules motorisés impliquant des hommes jeunes constituaient la majorité des lésions traumatiques. Au sein de cette cohorte, le recours aux ressources hospitalières était élevé, ainsi que la mortalité. Ces données peuvent aider à guider la mise en œuvre d’interventions visant à améliorer la prise en charge des traumatismes dans le contexte rwandais.
African relevance
-
•
Prehospital and hospital-based emergency services are a key element of a comprehensive acute care health system.
-
•
Little is known about patient characteristics, injury pattern, hospital resource utilisation, or patient outcomes in Kigali, Rwanda.
Introduction
Injuries account for 9.6% of global mortality burden, leading to over five million death annually and over 138 million disability-adjusted life-years (DALYs) [1], [2]. Over 90% of this burden falls upon those living in low- and middle-income countries (LMICs), where trauma system infrastructure is often minimal or absent entirely [2], [3]. Prehospital and hospital-based trauma care are critical components of acute care health services and provide the population with rapid access to life-saving treatments for a diverse set of time-sensitive illnesses. High quality prehospital and emergency care can save lives and minimise the sequelae of injury and acute illness [3].
It is estimated that 45% of deaths and 36% of disability-adjusted life years (DALYs) in LMICs could be addressed by the implementation of emergency care systems [4]. Unfortunately, most of the world’s population does not have access to these basic services [5], [6]. A recent review of care provided in emergency centres (ECs) across 59 LMICs reported a high in-EC mortality rate in sub-Saharan Africa (up to 3.4%) compared to an in-EC mean mortality rate of 0.04% in the United States (US) [7], [8]. Regional data from Uganda underscores the importance of the development of prehospital and acute care systems in East Africa. Data from Kampala, Uganda revealed that 25% of all in-hospital deaths were attributed to injury [9], while investigators in Rwanda have estimated that approximately 22% of deaths are attributable to traumatic injury [10]. In contrast, in 2007 injury accounted for only 7% of deaths in one US city [11]. Over the past decade, global health policy organisations have begun drawing attention to this needs gap, calling for “rapid and sustainable expansion of emergency treatments” [12], [13], [14].
Despite the fact that LMICs sustain the highest injury morbidity and mortality rates, critical epidemiological data is scant. Several investigators have taken initial steps to describe traumatic injuries in Rwanda, characterising injury patterns among patients at the main teaching hospital in Kigali, Rwanda [15], [16], [17]. A subsequent report by Enumah et al. details two years of prehospital patient demographics and injury patterns in Rwanda [18]. These efforts are informative and need to be expanded to provide a comprehensive picture of trauma care at the hospital, city, and regional level, including prehospital and hospital-based care. Investigators in other parts of the region have recently taken the next step, developing hospital-based trauma registries in several Sub-Saharan African (SSA) countries including Uganda, Tanzania, Cameroon, Malawi, Nigeria and Zambia [19], [20], [21], [22], [23]. Of these, few report information on prehospital and hospital resource utilisation. No national or regional trauma database has been developed in SSA.
In 2007, the Rwandan Ministry of Health (MOH) created a formal prehospital system, Service d’Aide Médicale Urgente (SAMU). Fifty-one ambulances and 370 motorcycles were distributed in central Rwanda to the city of Kigali and the surrounding communities. In 2012, an emergency medicine physician-training programme was instituted [24]. Despite the increased capacity of the Rwandan trauma system, there is limited information on traumatic injuries and associated care in Rwanda. The primary objective of this study was to develop a linked prehospital–hospital database to assess injury patterns, treatment and outcomes along the continuum of care in Kigali, Rwanda.
Methods
This retrospective chart review was conducted at University Teaching Hospital of Kigali (UTH-K) in Kigali, Rwanda. Ethical approval was obtained from the UTH-K Ethics Committee and Lifespan (Rhode Island Hospital) Institutional Review Board. This study was conducted at UTH-K which is a 576 bed urban, tertiary-care teaching hospital. UTH-K is the primary trauma centre for a population of 1.1 million in Kigali and serves as the primary academic referral centre for the entire country, a population of 10.5 million [25]. UTH-K has a 24-h Emergency Centre that sees all adult patients with acute complaints, as well as paediatric and obstetric trauma patients. Resources at UTH-K include 24-h of surgical coverage, 24-h access to radiologic services including X-ray, ultrasound and CT scan, as well as on call orthopaedic and neurological services.
Patients were eligible for inclusion if they were transported by SAMU to UTH-K for a traumatic injury during the 26-month period from December 2012 to February 2015. Paediatric and pregnant trauma patients were included as well as patients who died en route to UTH-K. Exclusion criteria included patients transported for non-traumatic illness (e.g. medical or obstetric complaints).
A composite index of patient identification information including name, age, sex, home district, and date of service was used to link hospital records to the SAMU prehospital database. Data for all SAMU patients transported to UTH-K were analysed, regardless of whether a corresponding hospital record was located. For patient encounters in which neither the medical record number (MRN), nor the hospital chart was locatable; or in whom the identity was not accurately recovered, encounter data was not abstracted.
Data collected included age, sex, transport time, location and mechanism of injury, injury type(s), prehospital and initial hospital vital signs, hospital admissions, surgical interventions, length of stay and disposition. Data were initially collected from archived paper charts and then abstracted and entered into REDCap electronic data capture tools – a secure, web-based application. Study data was analysed using Stata Statistical Software (StataCorp, 2015) [26]. Data were only collected on information generated from the index EC encounter and subsequent hospitalisation when relevant. Post-discharge outcomes, including subsequent EC visits, hospitalisations, or post-discharge death was not collected or recorded.
Anatomical regions of injuries were characterised based on classifications that have been used to calculate standardised injury severity scores [27], [28]. Injury severity was calculated using Revised Trauma Score (RTS) [29]. Continuous variables were summarised using median values with interquartile ranges. Categorical variables were reported as percentages.
Quality assurance testing was performed at four pre-determined intervals throughout the study. 10% of charts were randomly selected and reviewed by trained abstractors blinded to initial abstraction. Nine variables (six categorical and three continuous) were compared. Cohen’s kappa (κ) and percent agreement were used to assess the inter-rater reliability (IRR) between initial and repeat abstraction, with higher values indicating greater IRR for both methods. We set our quality threshold for IRR at a κ of 0.75, or a percent agreement of greater than 85%, or both. A quality improvement strategy was decided a priori: κ values below 0.75 would result in re-training [30].
Results
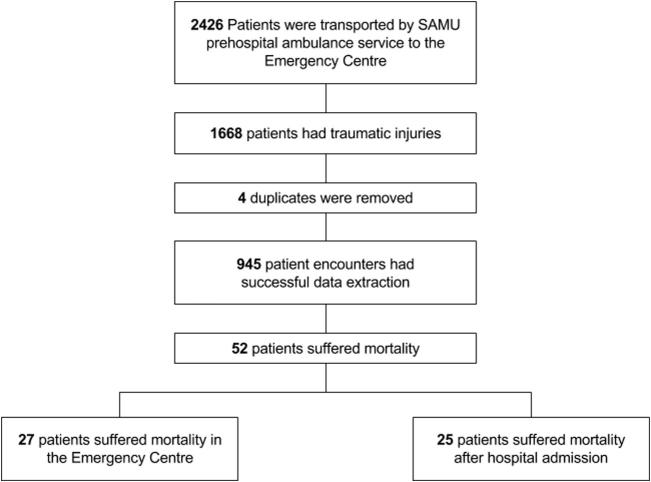
The prehospital database query generated 2426 unique encounters between December 2012 and February 2015, of which 1668 met the inclusion criteria. 757 were excluded because the chief complaint was non-traumatic. Health providers classified injuries as ‘traumatic’ at the time of the patient encounter, irrespective of injury severity. Four duplicate charts were identified and removed. An EC hospital record was located for 945 of these 1668 encounters (57.2%) and data was extracted from these charts (Fig. 1).
Fig. 1.
Inclusion/ exclusion algorithm and make up of study sample.
Ten percent of patients’ charts were randomly selected for repeat data entry as a quality assurance check on the initial data abstraction from the paper medical charts. The κ across all items was 97.8 (95.3–98.2 CI, p < 0.001) signifying excellent agreement between primary and repeat data abstraction.
Prehospital data was available for 1668 patients. The majority of patients were male (76.8%). The median age in years was 30 (IQR 24–36). Median transport time was 32 min (IQR 21–50). Overall, 82.7% of patients were transported to the EC in less than one hour (Table 1).
Table 1.
Patient characteristics
| Characteristic | Prehospitala n (%) | Emergency centreb n (%) |
|---|---|---|
| Sex | ||
| Male | 1272 (76.2) | 733 (77.7) |
| Female | 383 (22.9) | 210 (22.3) |
| Unknown | 14 (0.8) | 2 (0.2) |
| Age (years) | ||
| Overall, median (IQR) | 30 (24–36) | 30 (25–36) |
| 0–11 | 72 (4.3) | 40 (4.2) |
| 12–20 | 148 (8.9) | 77 (8.1) |
| 21–30 | 638 (38.2) | 358 (37.9) |
| 31–50 | 592 (35.5) | 387 (40.9) |
| >51 | 121 (7.2) | 83 (8.9) |
| Unknown | 98 (5.9) | 0 |
| Vital signsc, median (IQR) | ||
| Heart rate | 82 (74–91) | 84 (74–96) |
| Respiratory rate | 18 (16–20) | 20 (18–20) |
| Systolic blood pressure | 126 (115–136) | 128 (115–140) |
| Glasgow Coma Score | ||
| 3–8 | 48 (2.9) | 32 (4.7) |
| 9–12 | 132 (7.9) | 70 (10.3) |
| 13–15 | 1450 (86.9) | 582 (85.1) |
| Unknown | 39 (2.3) | 261 (27.6) |
| Revised Trauma Score | ||
| <4 | 5 (0.3) | 0 (0.0) |
| 4 to <5 | 5 (0.3) | 2 (0.3) |
| 5 to <6 | 37 (2.3) | 31 (5.7) |
| 6 to <7 | 124 (7.4) | 68 (12.4) |
| 7–7.84 | 1398 (83.8) | 447 (81.6) |
| Unknown | 100 (6.0) | 201 (21.3) |
| Prehospital Transport Time | ||
| Median in minutes (IQR) | 32 (21–50) | – |
| <30 min | 592 (35.5) | – |
| 30 to <60 min | 670 (40.1) | – |
| 60 min to <6 h | 253 (15.2) | – |
| >6 h | 12 (0.7) | – |
| Unknown | 142 (8.5) | – |
N = 1668.
N = 945.
Vital signs available for 1626 Service d’Aide Médicale Urgente patients and 744 emergency centre patients; IQR, interquartile range.
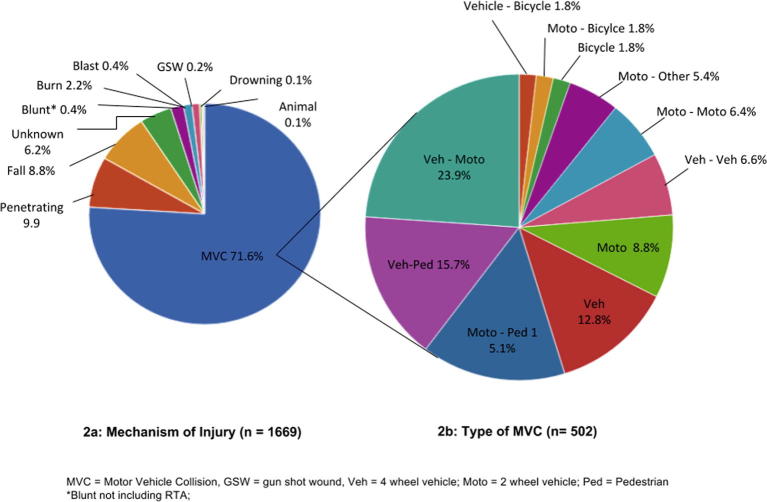
SAMU transports originated from all five provinces in Rwanda: Kigali, North, South, East and West covering a large catchment area (26,338 km2). However, 81% of transports (n = 1356) originated from within the province of Kigali (730 km2), while only 60 transports originated from Northern Provence, 104 from Southern Provence, 54 from Eastern Provence and 35 from Western Provence. Motor vehicle collisions (MVC) were the most common mechanism of injury, followed by penetrating trauma and fall (Fig. 2a). Among patients involved in an MVC, 502 had detailed mechanism reported in the hospital chart. Motorcycles were the most frequently involved, followed by collisions involving pedestrians. Vehicle–vehicle collisions and single vehicle collisions accounted for only a small proportion of injuries (Fig. 2b).
Fig. 2.
Mechanism of injury and type of motor vehicle collision (MVC).
Of 1668 trauma patients transported by SAMU, hospital charts were located for 945 (56.6%) cases. Males represented 77.7% of this cohort and the median age was 30 (IQR 25–36). Trauma at extremes of age was uncommon: patients <12 years and >50 accounted for only 4.2% and 8.9% of encounters, respectively. Vital signs were documented for 78.7% of patients. 85.1% of patients had a Glasgow Coma Score (GCS) of 13–15, while only 4.7% had GCS of 8 or below. 548 records had sufficient information to calculate Revised Trauma Scores (RTS) [29] (Table 1).
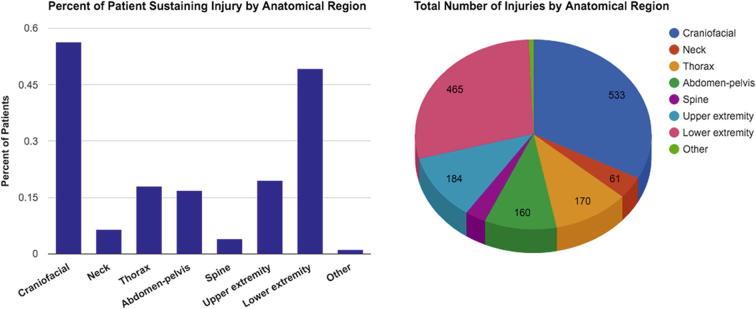
Among the 945 patient encounters, there were 1630 identified anatomic regions injured [16], [17]. In this cohort, 452 patients (47.8%) had a single injury, 268 patients (28.4%) had two anatomical regions injured, 147 patients (15.6%) had three regions injured and 45 patients (4.8%) had >3 regions injured. The most common anatomical region of injury was craniofacial, followed by lower extremity (Fig. 3). Motorcyclist passengers or drivers constituted 207 patients. Median GCS for injured motorcyclists was 15 (IQR 14–15). Mortality rate among motorcyclists was 5.8% (n = 12 deaths).
Fig. 3.
Injuries by anatomical region.
Most patients had at least one imaging test performed in the EC, while about half had laboratory testing completed. The majority of patients had at least one EC procedural intervention, defined as haemorrhage control, local wound care, intubation, thoracostomy, traction or splinting. About a third received intravenous fluids, and only a small minority were transfused blood products. The median EC length of stay (LOS) for admitted patients was 3.25 days (IQR 1–3) versus 2.10 days (IQR 0–2) for those discharged from the EC (Table 2).
Table 2.
Emergency centre and hospital utilisation and outcomes.
| Emergency centre | n (%) N = 945 |
|---|---|
| Imaging performed | 807 (85.4) |
| Laboratory testing | 465 (49.2) |
| IV Crystalloid infusion | 370 (39.2) |
| Blood products transfused | 63 (6.6) |
| Procedural Intervention | 633 (67.0) |
| EC Length of Stay in days, median (IQR) | |
| Non-admitted patients | 2.10 (0–2) |
| Admitted patients | 3.25 (1–3) |
| EC Disposition | |
| Discharged from EC | 355 (37.6) |
| Died in EC | 27 (2.9) |
| Survival time in days, median (IQR) | 0.68 (0–1) |
| Admitted to hospital | 379 (40.1) |
| Other/unknown | 184 (19.5) |
| Inpatient | n (%) N = 379 |
| Admission Ward | |
| Medical | 2 (0.5) |
| Surgical | 332 (88.1) |
| Intensive Care Unit | 26 (6.9) |
| Orthopaedics | 7 (1.9) |
| Other | 10 (2.6) |
| Hospital Intervention | |
| Required transfer to ICU after admission | 15 (4.0) |
| Required operative management | 298 (78.1) |
| Open Reduction with internal fixation | 164 (36.3) |
| Wound debridement | 124 (27.4) |
| Closed Reduction with external fixation | 71 (15.7) |
| Craniotomy | 26 (5.8) |
| Laparotomy | 16 (3.5) |
| Other | 57 (12.6) |
| Hospital length of Stay in days, median (IQR) | |
| All admitted patients | 16 (8–31) |
| Requiring operative management | 27.3 (10–34.5) |
| Inpatient Disposition | |
| Died in hospital | 25 (6.6) |
| Survival Time in days, median (IQR) | 12.6 (2.8–11.5) |
| Discharged | 285 (75.4) |
| Transferred to a different health centre | 60 (15.9) |
| Unknown | 8 (2.2) |
IV, intravenous; EC, emergency centre; IQR, interquartile range; ICU, intensive care unit.
A total of 379 (40.1%) patients were admitted to the hospital. For those admitted, 296 (78.1%) required surgical interventions. The most common procedure was open reduction internal fixation, followed by wound debridement. Among admitted patients, median LOS was 16 days (IQR 8–31). In the subset of patients requiring operative management, median LOS was 27.3 days (IQR 10–34.5). Of the 379 patients admitted to the hospital, 25 died (6.6%) (Table 2).
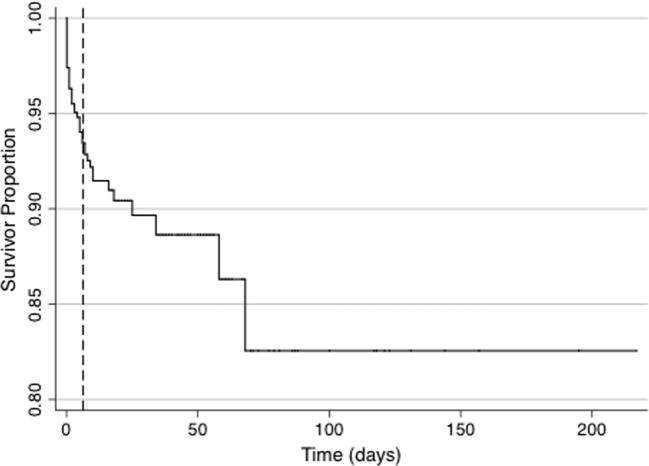
Data sufficient for survival to hospital discharge was available for 769 patients (81.4%). Overall mortality rate at time of discharge was 5.5% with 51.9% of deaths occurring in the EC. Mean survival time of 6.31 days (95% CI 2.55–10.08). Median survival time among those who died in the EC was 0.68 days (IQR 0–1) versus 12.6 days (IQR 2.8–11.5) among hospital deaths. Mortality incidence was 1.90 deaths per person-year of follow-up (95% CI 1.44–2.50) with a total follow up time of 26.86 person-years. The mortality range was 0–68 days with follow up time extending to 241 days (Fig. 4). Follow up data, including death after discharge documented in hospital records, mortuary records or other data sources were not collected.
Fig. 4.
Kaplan-Meier curve representing survival time for mortality (Calculated based on 769 cases with data sufficient to analyse at time of discharge).
Discussion
Advances in emergency care have led to dramatic improvements in outcomes for patients suffering acute injury and illness [31], [32], [33]. These advances have largely benefited populations in high-income countries, while access to emergency care in low-resource settings is often lacking [7]. Additionally, while prehospital care of trauma patients has been reported to be one of the most important factors in determining the ultimate outcome after injury [34], prehospital services are unavailable in most low-resource settings.
The availability of epidemiological and descriptive data on trauma and injury is an important element to improving injury care. However, there are only a small number of trauma registries from LMICs, and even fewer that link prehospital and hospital-based data [35]. Descriptive data on the epidemiology of injury and acute care in Rwanda is sparse, however, initial efforts in uncovering injury patterns, injury mortality rates, and prehospital resource utilisation have been informative [15], [16], [17], [18]. In this retrospective study, a trauma database was used to collect data on key variables from the prehospital, EC and hospital setting. Thus, for this cohort, we were able to follow the patient’s trajectory across the continuum of their acute care and inpatient course. In this way, our study represents an important contribution to the knowledge of traumatic injury and care in Rwanda as well as in SSA. This study demonstrates the feasibility of collecting informative retrospective trauma data in Rwanda, with data extraction rates comparable to similar prospective studies in the region [21], [23], as well as the results of an initial effort at linking patient and injury characteristics to prehospital and hospital resource utilisation and outcome.
Data collected retrospectively over this 26-month period was reflective of injury patterns previously documented in LMICs in the region [21], [22], [23], [34]. The majority of injured patients transported by prehospital ambulance service were victims of MVCs in their productive years. The greatest preponderance of collisions affected motorcyclists (drivers and passengers), which reflects trends documented in other SSA countries [18], [34].
Our study cohort was unique compared to similar groups in that the majority of injuries were unintentional with a low reported level of assault (n = 71, 7.5%) and sexual violence (n = 0, 0%) as the documented cause of injury [20], [21], [22], [23], [36]. This discrepancy may be due to multiple causes including under-reporting of assault, differential utilisation of prehospital ambulance services depending on mechanism of injury, or may reflect broader injury patterns specific to Rwanda. The overall mortality rate (2.9% deaths in the EC and 5.5% overall) was higher than other single centre trauma registries in SSA have reported [20], [21], [22], [23], [37].
Unlike many other LMICs, Rwanda requires motorcyclists to be licensed and certified, and both passenger and driver are required to wear helmets, however, there are no standards on helmet quality. Data from high-income countries suggest that these safety measures should be associated with decreased injury severity. In this cohort, 55.8% of patients involved in motorcycle crashes sustained head injuries, however, the median GCS for these patients was high and the case fatality rate was relatively low.
This is one of the few studies in the region to describe hospital resource use among injured patients requiring acute care. Hospital resource utilisation for this cohort was found to be high, with 40.1% of patients requiring admission, the majority of whom also required surgical care (78.1%), or ICU care (10%). The hospitalisation rate was slightly lower than the rates observed in similar cohorts [23], [34], [36]. However, the median hospital LOS among admitted patients (16 days) was higher than LOS reported in studies from similar cohorts [23], [38], [39]. One possibility is that the increased median LOS is driven by the extended hospital LOS observed among those requiring surgical intervention (27.3 days). Ultimately, given the absence of standardisation in terms of injury severity scoring and other factors, it is difficult to make any direct comparison across studies.
Finally, to our knowledge, this study represents the only report on the outcomes of injured patients receiving professional prehospital care in Rwanda as well as in east and central Africa. Prehospital care is key to the improvement of outcomes in injured patients, as rapid trauma care after injury has been shown to improve outcomes [40], [41]. In our study of all patients receiving prehospital emergency care in Rwanda, we noted a median transport time of 32 min. The majority of SAMU transports were from within the district of Kigali, which covers over 26,338 km2 – a relatively large catchment area. At the time of this publication, most trauma centres in SSA do not have formal prehospital systems, and transport times for acutely ill or injured patient are largely unknown.
Despite access to prehospital care, mortality rates among this cohort are higher than those observed among injured patients in high-resource settings who also have access to prehospital care. There are many possible explanations for this. SAMU is relatively new to the Rwandan population, and this study was not able to evaluate the quality of care provided to patients during transport. More fundamentally, there are many factors that may affect a laypersons’ decision to call for rescue such as insurance status, financial ability to pay for ambulance, awareness of prehospital services, and perception of injury severity. As of 2013, 85% of Rwandans had some form of health insurance coverage, whether private, military or Mutuelles de Santé – the state-sponsored universal health insurance. Insurance plans in Rwanda offer varying degree of coverage for prehospital and hospital care; Mutuelles de Santé covers 90% of the cost of most hospital and prehospital care. In light of this, it is unclear to what extent cost plays a role in prehospital care utilisation. Perhaps most importantly, mortality rates are affected by numerous factors that remain outside the scope of prehospital care [42].
There are several limitations to note. Missing data is always a limitation to retrospective chart review, particularly in low-resource settings. While prospective data collection was not possible due to resource limitations, our retrospective data recovery rate was comparable to several similar prospectively conducted studies in the region [21], [23]. Missing data may disproportionally represent the sickest patients as they are the least likely to be able to provide accurate (or any) identifying information to hospital registration services and thus the records generated from these encounters may be more likely to be lost or unrecoverable on retrospective review. Similarly, missing demographic data may be disproportionately present in those with low socioeconomic status or those with the least health literacy. Future studies might consider collecting more detailed socio-demographic data. Additionally, the dataset only represents those patients transported via prehospital ambulance and provides limited information on the general epidemiology of injury in Rwanda. Due to resource constraints, follow-up after hospital discharge was not available. While this data set offers initial insight into the scope of Rwanda’s professional prehospital service, including average transport times and total catchment area, more granular data on the type of transport (i.e. on scene versus inter-facility, transfer distances, operational costs, etc.) would be of great use, particularly in developing a model for professional prehospital transport in low-income settings. Finally, this chart review may also be limited by the quality of the data initially recorded by prehospital, emergency centre, and hospital providers. Accurate charting and documentation remain a significant challenge.
A linked prehospital and hospital database can provide critical epidemiological information describing characteristics and outcomes of trauma patients receiving prehospital and hospital-based acute care in low-resource settings. Blunt trauma from MVCs, involving young males constituted the majority of traumatic injuries in the population studied. Among this cohort, hospital resource utilisation and overall mortality was high compared to high-income countries as well as similar reports from SSA, with roughly half of traumatic deaths occurring in the EC setting. Prospective data are needed to more robustly define the epidemiology of injuries and guide interventions to mitigate the burden of traumatic disease in the Rwandan setting.
Conflicts of interest
The authors declare no further conflicts of interest.
Dissemination of findings
Results and conclusions from this work have been disseminated during invited presentations for the following organizations:
Service d’Aide Médicale Urgente (SAMU), Rwanda Emergency Care Organization (RECA), Residency Conference – Department of Accident and Emergency Centre, Hospitalier Universitaire de Kigali, Residency Conference – Brown University, Department of Emergency Medicine and the Global Health Division Meeting – Brown University, Department of Emergency Medicine.
Author contribution
NG, GB, JB, RR, and AL conceived the original idea and designed the protocol. NG, GB, AK, NK, AA, NK, OU, ZM, SE, JS, EU, and JDN, carried out analysis of data. NG, GB, AK, NK, AA, NK, OU, ZM, SE, JS, EU, JDN, IK, JN, SJ, JB, RR, AL prepared the manuscript and approved the final draft.
Acknowledgements
Funding for this study was provided by Brown University through the Framework in Global Health Scholarship and by University Emergency Medicine Foundation through the Resident Scholarly Development Awards Program.
Footnotes
Peer review under responsibility of African Federation for Emergency Medicine.
References
- 1.Lozano R., Naghavi M., Foreman K. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chandran A., Hyder A., Peek-Asa C. The global burden of unintentional injuries and an agenda for progress. Epidemiol Rev. 2010;32(1):110–120. doi: 10.1093/epirev/mxq009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization: Injury and violence: the facts online – 2004. Available from: http://www.who.int/violence_injury_prevention/key_facts/VIP_key_facts.pdf. [Accessed December 15th, 2013].
- 4.Murray C.J., Vos T., Lozano R. Disability adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2197–2223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 5.Jamison D.T., Mosley W.H. Disease control priorities in developing countries: health policy responses to epidemiological change. Am J Public Health. 1991;81:15–22. doi: 10.2105/ajph.81.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Smith J., Haile Mariam T. Priorities in global emergency medicine development. Emerg Med Clin North Am. 2005;23(1):11–29. doi: 10.1016/j.emc.2004.09.012. [DOI] [PubMed] [Google Scholar]
- 7.Obermeyer Z., Abujaber S., Makar M. Emergency care in 59 low- and middle-income countries: a systematic review. Bull World Health Organ. 2015;93(8):577G–586G. doi: 10.2471/BLT.14.148338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tang N., Stein J., Hsia R.Y. Trends and characteristics of US emergency department visits, 1997–2007. JAMA. 2010;304:664–670. doi: 10.1001/jama.2010.1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hsia R.Y., Ozgediz D., Mutto M. Epidemiology of injuries presenting to the national hospital in Kampala, Uganda: implications for research and policy. Int J Emerg Med. 2010;3(3):165–172. doi: 10.1007/s12245-010-0200-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim W., Byiringiro J. Vital statistics: estimating injury mortality in Kigali, Rwanda. World J Surg. 2015;40(1):6–13. doi: 10.1007/s00268-015-3258-3. [DOI] [PubMed] [Google Scholar]
- 11.Jayaraman S., Ozgediz D., Miyamoto J. Disparities in injury mortality between Uganda and the United States: comparative analysis of a neglected disease. World J Surg. 2011;35(3):505–511. doi: 10.1007/s00268-010-0871-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kobusingye O.C., Hyder A.A., Bishai D. Emergency medical systems in low- and middle-income countries: recommendations for action. Bull World Health Organ. 2005;83(8):626–631. [PMC free article] [PubMed] [Google Scholar]
- 13.Kobusingye, OC, Hyder AA, Bishai D, et al. Emergency medical services – Disease control priorities in developing countries – NCBI bookshelf; 2012. http://www.ncbi.nlm.nih.gov/books/NBK11744/. [Accessed 1 March 2014].
- 14.Walt G. WHO’s world health report 2003. BMJ (Clinical research ed.) 2004;328(7430):6. doi: 10.1136/bmj.328.7430.6. Available at: http://www.who.int/whr/2003/en/whr03_en.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nsereko E., Brysiewicz P. Injury surveillance in a central hospital in Kigali, Rwanda. J Emerg Nurs. 2010;36(3):212–216. doi: 10.1016/j.jen.2009.07.020. [DOI] [PubMed] [Google Scholar]
- 16.Yamuragiye A., Ibambasi A., Mutuyimana A. Short Communication: Injury profile in an emergency department at a referral hospital in Kigali, Rwanda. Rwanda J Health Sci. 2013;2:61–62. [Google Scholar]
- 17.Twagirayezu E., Teteli R., Bonane A. Road traffic injuries at Kigali University Central Teaching Hospital, Rwanda. East Cent Afr J Surg. 2008;13:73–76. [Google Scholar]
- 18.Enumah S., Scott J.W., Maine R. Rwanda’s model prehospital emergency care service: a two-year review of patient demographics and injury patterns in Kigali. Prehosp Disaster Med. 2016 doi: 10.1017/S1049023X16000807. [in press] [DOI] [PubMed] [Google Scholar]
- 19.Chichom Mefire A., Etoundi Mballa G.A., Azabji Kenfack M. Hospital-based injury data from level III institution in Cameroon: retrospective analysis of the present registration system. Injury. 2013;44:139–143. doi: 10.1016/j.injury.2011.10.026. [DOI] [PubMed] [Google Scholar]
- 20.Samuel J.C., Akinkuotu A., Villaveces A. Epidemiology of injuries at a tertiary care center in Malawi. World J Surg. 2009;33:1836–1841. doi: 10.1007/s00268-009-0113-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Thanni L.O., Kehinde O.A. Trauma at a Nigerian teaching hospital: pattern and documentation of presentation. Afr Health Sci. 2006;6:104–107. doi: 10.5555/afhs.2006.6.2.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Taye M., Munie T. Trauma registry in Tikur Anbessa Hospital, Addis Ababa, Ethiopia. Ethiopia Med J. 2003;41:221–226. [PubMed] [Google Scholar]
- 23.Seidenberg P., Cerwensky K., Brown R.O. Epidemiology of injuries, outcomes, and hospital resource utilisation at a tertiary teaching hospital in Lusaka, Zambia. Afr J Emerg Med. 2014;4:115–122. [Google Scholar]
- 24.Kabeza A., George N., Nyundo M. Development of emergency medicine in Rwanda. Afr J Emerg Med. 2013;3:103–109. [Google Scholar]
- 25.2012 Population and Housing Census, 2012. National Institute of Statistics, Rwanda. Available at http://statistics.gov.rw/publications/rphc4-thematic-report-population-size-structure-and-distribution. [Accessed February 10th, 2015].
- 26.Harris P.A., Taylor R., Thielke R. Research electronic data capture (REDCap). A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Baker S.P., O’Neill B., Haddon W., Jr The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187–196. [PubMed] [Google Scholar]
- 28.Copes W.S., Champion H.R., Sacco W.J. The injury severity score revisited. J Trauma. 1988;28(1):69–77. doi: 10.1097/00005373-198801000-00010. [DOI] [PubMed] [Google Scholar]
- 29.Champion H.R., Sacco W.J., Copes W.S. A revision of the trauma score. J Trauma. 1989;29:623–629. doi: 10.1097/00005373-198905000-00017. [DOI] [PubMed] [Google Scholar]
- 30.Reisch L.M., Fosse J.S., Beverly K. Training, quality assurance, and assessment of medical record abstraction in a multisite study. Am J Epidemiol. 2003;157:546–551. doi: 10.1093/aje/kwg016. [DOI] [PubMed] [Google Scholar]
- 31.Stevenson E.K., Rubenstein A.R., Radin G.T. Two decades of mortality trends among patients with severe sepsis: a comparative meta-analysis. Crit Care Med. 2014;42:625–631. doi: 10.1097/CCM.0000000000000026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Boyle A.A., Ahmed V., Palmer C.R. Reductions in hospital admissions and mortality rates observed after integrating emergency care: a natural experiment. BMJ Open. 2012;2 doi: 10.1136/bmjopen-2012-000930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kellermann A.L., Hsia R.Y., Yeh C. Emergency care: then, now, and next. Health Aff (Millwood) 2013;32:2069–2074. doi: 10.1377/hlthaff.2013.0683. [DOI] [PubMed] [Google Scholar]
- 34.Chalya P.L., Mabula J.B., Ngayomela I.H. Motorcycle injuries as an emerging public health problem in Mwanza City, north-western Tanzania. Tanzan J Health Res. 2010;12:214–221. [PubMed] [Google Scholar]
- 35.O’Reilly G., Joshipura M., Cameron P.A. Trauma registries in developing countries: a review of the published experience. Injury. 2013;44:713–721. doi: 10.1016/j.injury.2013.02.003. [DOI] [PubMed] [Google Scholar]
- 36.Tadesse B., Tekilu S., Nega B. Pattern of injury and associated variables as seen in the emergency department at Tikur Anbessa Specialized Referral Hospital, Addis Ababa, Ethiopia. East Cent Afr J Surg. 2014;19:73–83. [Google Scholar]
- 37.Demyttenaere S.V., Nansamba C., Nganwa A. Injury in Kampala, Uganda: 6 years later. Can J Surg. 2009;52:E146–E150. [PMC free article] [PubMed] [Google Scholar]
- 38.Masiira-Mukasa N., Ombito B. Surgical admissions to the Rift Valley provincial general hospital, Kenya. East Af Med J. 2002;79:373–378. doi: 10.4314/eamj.v79i7.8842. [DOI] [PubMed] [Google Scholar]
- 39.Otieno T., Woodfield J., Bird P. Trauma in rural Kenya. Injury. 2004;35(12):1228–1233. doi: 10.1016/j.injury.2004.03.013. [DOI] [PubMed] [Google Scholar]
- 40.Swaroop M., Straus D.C., Agubuzu O. Pre-hospital transport times and survival for hypotensive patients with penetrating thoracic trauma. J Emerg Trauma Shock. 2013;1:16–20. doi: 10.4103/0974-2700.106320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tien H.C., Jung V., Pinto R. Reducing time-to-treatment decreased mortality of trauma patients with subdural hematoma. Ann Surg. 2011;6:1178–1183. doi: 10.1097/SLA.0b013e318217e339. [DOI] [PubMed] [Google Scholar]
- 42.Mock C., Joshipura M., Arreola-Risa C. An estimate of the number of lives that could be saved through improvements in trauma care globally. World J Surg. 2012;36:959–963. doi: 10.1007/s00268-012-1459-6. [DOI] [PubMed] [Google Scholar]