Abstract
Introduction
Increased intracranial pressure is usually measured with invasive methods that are not practical in resource-limited countries. However, bedside ultrasound, a non-invasive method, measures the optic nerve sheath diameter and could be a safe and accurate alternative to measure intracranial pressure, even in children.
Case report
We report a case of a 15-year old patient who presented with severe headache, projectile vomiting, and neck pain for two months. The bedside ultrasound showed a 10 mm optic nerve sheath diameter and a Computed Tomography scan of her brain revealed obstructive hydrocephalus secondary to a mass in the fourth ventricle. After intervening, we were able to monitor the decrease in her optic nerve sheath diameter with ultrasound.
Conclusion
Performing invasive procedures continues to be a challenge in the resource limited setting. However, bedside ultrasound can be a useful tool in emergency centres for early detection and monitoring of intracranial pressure.
Keywords: Ultrasound, ONSD, ICP
Abstract
Introduction
L’hypertension intracrânienne (HTIC) est généralement mesurée au moyen de méthodes invasives qui ne s’avèrent pas pratiques dans des pays caractérisés par des ressources limitées. Cependant, l’échographie au chevet des patients, une méthode non invasive, mesure le diamètre de la gaine du nerf optique (DGNO) et pourrait constituer une alternative sûre et précise pour mesurer l’HTIC, même chez les enfants
Étude de cas
Nous avons étudié le cas d’une patiente de 15 ans qui s’était présentée souffrant de violents maux de tête, de vomissements en jets et de douleurs au cou depuis deux mois. L’échographie au chevet de la patiente a révélé un DGNO de 10 mm et la tomodensitométrie du cerveau a révélé une hydrocéphalie obstructive associée à une masse dans le quatrième ventricule. Après intervention, nous avons pu surveiller la réduction de son DGNO à l’aide de l’échographie
Discussion/Conclusion
La réalisation de procédures invasives reste un défi dans les contextes caractérisés par des ressources limitées. Cependant, l’échographie au chevet du patient peut être un outil utile dans les services d’urgence pour permettre la détection précoce et le suivi de l’HTIC.
African relevance
-
•
Bedside ultrasound can potentially be used to measure increased intracranial pressure in resource-limited settings.
Introduction
Increased intracranial pressure (ICP) is usually measured using invasive methods, which is not practical in Emergency Centres (ECs) in resource limited countries.1 Bedside ultrasound measuring the optic nerve sheath diameter (ONSD) has been used increasingly and advocated as a non-invasive method to measure ICP even in children.2, 3, 4 This method has been validated to indicate direct ICP and has been successfully used in trauma and intensive care patients and in patients with hydrocephalus.5, 6, 7, 8
Case report
A 15-year-old female patient presented to the EC with severe headache, projectile vomiting, and neck pain for two months. The headache was global and she rated it as six out of ten pain that was worsening. She also reported blurry vision. She denied trauma to the head, fever, cough, night sweats, weakness and numbness of the extremities, and changes in bowel or bladder habits.
On examination, she was in moderate distress from pain. Her vital signs were as follows: blood pressure 100/70 mmHg, pulse rate 105 beats per minute, respiratory rate 20 breaths per minute, temperature 36.4 °C, and oxygen saturation of 94% on room air. Her physical examination was unremarkable except for photophobia. She had no neck mass, no conjunctival injection or proptosis. Her extraocular movements were intact and her pupils were equal, round and reactive to light bilaterally.
A complete blood count, chemistry, and hepatic panel were unremarkable. A bedside ultrasound examination (using the 7 MHz linear probe of the portable SonoSite 180plus machine) showed an enlarged ONSD of 10 mm with prominent papilla bilaterally (red arrow in Fig.1A). The patient was examined in the supine position (head of bed approximately 30–45 degrees of elevation). The probe with ultrasound gel was placed lightly over each closed eye after covering each eye with Tegaderm (3M, St. Paul, MN). To align the optic nerve directly opposite to the probe, the patient was directed to look forward with closed eyes. The ONSD was 3 mm behind the optic disc in both transverse and sagittal planes. Three measurements were averaged and recorded after scanning the largest viewed diameter.
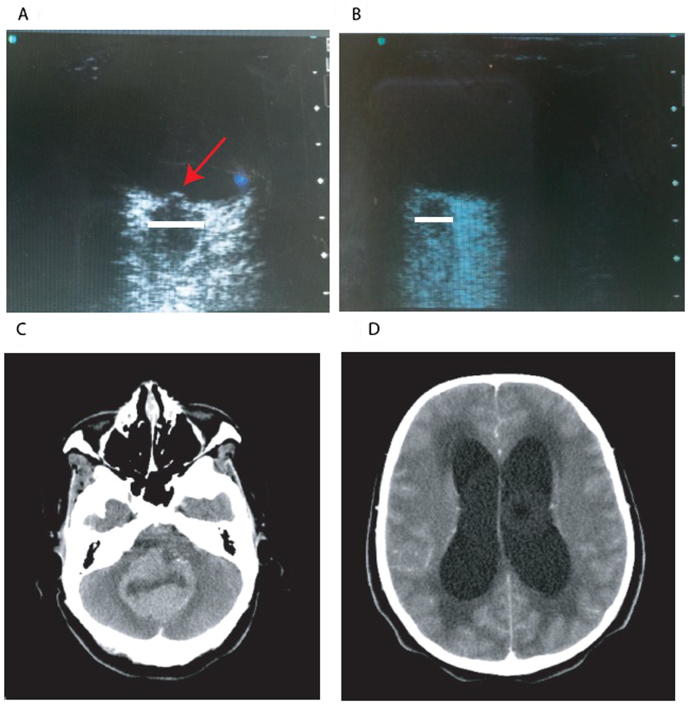
Figure 1.
Ultrasound and Computed Tomography scan images of a patient with obstructive hydrocephalus. (A) Ultrasound image showing enlarged optic nerve sheath diameter of 10 mm with prominent papilla (red arrow) pre-operative; (B) Ultrasound image showing diminished optic nerve sheath diameter of 6 mm with resolution of the papilla prominence post ventriculoperitoneal-shunt insertion; (C) Computed Tomography scan images showing a mass in the fourth ventricle causing obstruction; (D) Computed Tomography scan images showing hydrocephalus.
The increased ONSD prompted obtaining a Computed Tomography (CT) scan of the brain which demonstrated a cerebellar mass originating from the fourth ventricle with obstructive hydrocephalus (Fig.1A–D).
The patient was evaluated by the neurosurgery team and received a ventriculoperitoneal-shunt. Her symptoms improved significantly and a repeat measurement 16 h post-operatively demonstrated an improved measurement of 6 mm ONSD bilaterally. The patient was then discharged home in stable condition and instructed to follow up in the outpatient clinic.
Discussion
Performing invasive procedures is a major challenge in the resource limited setting; health care providers are unable to utilise imaging systems, such as CT scans and MRI, which are available in other settings. In addition to expense, CT scans also expose patients to radiation. MRIs are not particularly ideal in critically ill and unstable patients. Bedside ultrasound, when available, offers a better alternative for this patient population. Ultrasounds have no known risks and are cost-effective and readily available.
Bedside ultrasounds have become more accessible and are used by Emergency Physicians regularly. In the United States, ultrasound training is an integral part of the residency curriculum.9 Findings from a bedside ultrasound can dictate management priorities and can assist with early intervention, especially in trauma. A positive Focused Assessment with Sonography in Trauma, free fluid in the abdomen or pelvis in an unstable trauma patient, may expedite the patient receiving definitive care in the operating room and avoid unnecessary and prolonged testing. Moreover, residents and faculty members are beginning to use the ultrasound in more than just the trauma patient.
We recently encountered a patient with headache and blurry vision where bedside ultrasound revealed increased ONSD. This led to a CT that showed signs of benign intracranial hypertension. She underwent lumbar puncture in the EC and was discharged home in improved condition. The patient returned to the EC with recurrent headache. Repeat ultrasound showed normal ONSD and patient was treated for presumed post LP headache. Her symptoms improved significantly and we were able to avoid repeating a head CT scan.10 Different studies have tested the accuracy of ONSD in detecting ICP by comparing the ONSD with direct ICP measurements.11 A review of these studies showed a sensitivity ranging from 74% to 95% and a specificity of 79–100%. On the other hand, a study by Major et al. reported a sensitivity of 86% and a specificity of 100% when compared to CT scan evidence of raised ICP. In our patient, initial examination showed a symptomatic patient with enlarged ONSD. After placement of a ventriculoperitoneal-shunt, the ONSD diminished with significant symptom improvement. Ultrasound was helpful in both initial evaluation and interval follow up and was a simple, fast adjunct to clinical decision-making.
An alternative for detecting increased ICP is the funduscopic examination. However, unlike bedside ultrasonography, the funduscopic examination requires a cooperative patient and usually dilation of the pupil for better assessment. In addition, papillary oedema or prominence may be interpreted differently by providers based on their experience. This contrasts to ONSD, which is more of an objective measure.
Conclusion
Bedside ultrasound can be a useful tool in the EC in the resource limited setting for early detection of ICP and for interval follow-up. This is supported by the previous studies reporting high sensitivity and specificity of bedside ultrasound for assessment of increased ICP. Residents and other house staff can be easily trained and further large scale studies can be performed in order to evaluate the accuracy and benefits of bedside ultrasound in patients with suspicion for raised ICP.
Conflict of interest
The authors declare no conflict of interest.
Dissemination of results
Findings have been locally disseminated by the authors.
Author contribution
The authors have all contributed equally to the conception of the work; the acquisition, analysis, or interpretation of data; drafting and revising; final approval of the version to be published; and agreed to be accountable for all aspects of the work.
Acknowledgement
The authors wish to thank Dr. Shaw for assisting with editing of this paper.
Footnotes
Peer review under responsibility of African Federation for Emergency Medicine.
References
- 1.Miller J.D. ICP monitoring–current status and future directions. Acta Neurochir (Wien) 1987;85:80–86. doi: 10.1007/BF01456102. [DOI] [PubMed] [Google Scholar]
- 2.Dubourg J., Javouhey E., Geeraerts T. Ultrasonography of optic nerve sheath diameter for detection of raised intracranial pressure: a systematic review and meta-analysis. Intensive Care Med. 2011;37(7):1059–1068. doi: 10.1007/s00134-011-2224-2. [DOI] [PubMed] [Google Scholar]
- 3.Le A., Hoehn M.E., Smith M.E. Bedside sonographic measurement of optic nerve sheath diameter as a predictor of increased intracranial pressure in children. Ann Emerg Med. 2009;53:785–791. doi: 10.1016/j.annemergmed.2008.11.025. [DOI] [PubMed] [Google Scholar]
- 4.Tsung J.W., Blaivas M., Cooper A. A rapid noninvasive method of detecting elevated intracranial pressure using bedside ocular ultrasound: application to 3 cases of head trauma in the pediatric emergency department. Pediatr Emerg Care. 2005;21:94–98. doi: 10.1097/01.pec.0000159052.64930.64. [DOI] [PubMed] [Google Scholar]
- 5.Hansen H.C., Helmke K. Validation of the optic nerve sheath response to changing cerebrospinal fluid pressure: ultrasound findings during intrathecal infusion tests. J Neurosurg. 1997;87:34–40. doi: 10.3171/jns.1997.87.1.0034. [DOI] [PubMed] [Google Scholar]
- 6.Kimberly H.H., Shah S., Marill K. Correlation of optic nerve sheath diameter with direct measurement of intracranial pressure. Acad Emerg Med. 2008;15:201–204. doi: 10.1111/j.1553-2712.2007.00031.x. [DOI] [PubMed] [Google Scholar]
- 7.Newman W.D., Hollman A.S., Dutton G.N. Measurement of optic nerve sheath diameter by ultrasound: a means of detecting acute raised intracranial pressure in hydrocephalus. Br J Ophthalmol. 2002;86:1109–1113. doi: 10.1136/bjo.86.10.1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hassen G.W., Bruck I., Donahue J. Accuracy of optic nerve sheath diameter measurement by emergency physicians using bedside ultrasound. J Emerg Med. 2015;48:450–457. doi: 10.1016/j.jemermed.2014.09.060. [DOI] [PubMed] [Google Scholar]
- 9.Akhtar S., Theodoro D., Gaspari R. Resident training in emergency ultrasound: consensus recommendations from the 2008 Council of Emergency Medicine Residency Directors Conference. Acad Emerg Med. 2009;16(Suppl. 2):S32–S36. doi: 10.1111/j.1553-2712.2009.00589.x. [DOI] [PubMed] [Google Scholar]
- 10.Hassen G.W., Nazeer O., Manizate F. The role of bedside ultrasound in pretherapeutic and posttherapeutic lumbar puncture in patient with idiopathic intracranial hypertension. Am J Emerg Med. 2014;32(1298):e1293–e1294. doi: 10.1016/j.ajem.2014.03.028. [DOI] [PubMed] [Google Scholar]
- 11.Soldatos T., Chatzimichail K., Papathanasiou M. Optic nerve sonography: a new window for the non-invasive evaluation of intracranial pressure in brain injury. Emerg Med J. 2009;26:630–634. doi: 10.1136/emj.2008.058453. [DOI] [PubMed] [Google Scholar]