Abstract
Introduction
Emergency medicine is a relatively new specialty in Africa, with the first emergency medicine training programme only started in South Africa in 2004. Continued emergency centre development and preparedness relies on a better understanding of the quantity and category of emergency centre encounters within the various African regions.
Methods
This study was conducted over four, consecutive months in 2014 using a retrospective chart review, aimed to examine the types of visits made to one emergency centre at the Grande Mbour Hospital in Mbour, Senegal. The New York University Emergency Department Algorithm was used to classify emergency centre encounters. Each diagnosis included in this study was classified per the algorithm as non-emergent; emergent but primary care treatable; emergent with emergency centre care needed but avoidable/preventable; and emergent with emergency centre care needed and not avoidable/preventable. The algorithm also categorised diagnoses of injury, mental health problems, alcohol, or substance abuse.
Results
This study included 1268 diagnoses from the emergency centre. The most common presentations in Mbour, Senegal were injuries, with 302 cases (33%), and from the category: emergent but primary care treatable, with 303 cases (33%). In total, 174 cases (19%) were classified as: non-emergent. While only 93 cases (10%) were considered: emergency care needed/preventable or avoidable, a substantial number (n = 218, 24%) were categorised as: emergent with emergency centre care needed and not avoidable/preventable.
Conclusion
This study provides the first description of patients presenting for care in the emergency centre of Mbour’s hospital and demonstrates the wide range of illnesses and types of trauma that the emergency centre must accommodate while contending with the limited resources available in the area. Understanding the burden of disease will help prioritise resources appropriately.
Keywords: Africa, Senegal, Emergency, Acute, Triage
African relevance
-
•
As seen elsewhere in Africa, injuries remained the dominant presentation.
-
•
Around half of patients could have been cared for elsewhere in the health system.
-
•
Lack of adequate primary care provision results in overburdening of emergency services.
Introduction
In Senegal, severe access disparity hinders essential health care efforts between rural and urban populations [1]. Accessibility to health care is greatly limited in rural areas, often requiring an hour-long walk to reach any sort of medical care [2]. In contrast, urban areas have a greater density of medical providers. While rural citizens may struggle to find a health care provider, the emergency centres in urban centres are inundated with both emergent and non-emergent patients. Often, individuals do not have primary care physicians and instead rely solely on traditional healers, health posts, and emergency centres for primary care concerns [3]. This brings into question how to adequately implement and balance a strong emergency service that can address truly emergent scenarios, while also attending to the primary care needs of a population. Improved emergency centre preparedness critically relies on a better understanding of the quantity and category of emergency centre encounters.
A variety of challenges and barriers exist in establishing robust emergency centres in the hospitals of low- and middle-income countries (LMIC) [4], [5], [6], [7], [8]. The Disease Control Priorities project estimates that 45% of deaths and 36% of disability-adjusted-life-years could be mitigated by effective emergency care systems. Additionally, the World Health Resolution 60.22 has called for the development of such systems in all of its member states [9]. Emergency centres in LMICs must be designed to suit the specific needs of the population in which they serve. However, a lack of resources, transportation, and trained staff often prevents adequate medical treatment from becoming a reality in African emergency centres [5], [8].
Emergency medicine is a relatively new medical field in Africa, with the first emergency medicine specialist training programme beginning in South Africa in 2004. In total, 13 emergency medicine residency programmes currently operate across the continent, suggesting a significant need of emergency medicine-trained physicians [5]. Emergency Medical Services are also limited, existing in only one-third of African countries [10], [11]. The staffing of emergency centres is highly variable between hospitals, with many being run by small teams composed of a single doctor and a few nurses. Training hospitals and academic centres are more likely to have larger teams with emergency-trained physicians and nurses [12]. This is a significant problem considering that, worldwide, Africa has the highest rate of road traffic injury mortality (32.2 per 100,000), as well as high rates of communicable disease and maternal/infant mortality [13], [14]. LMICs increasingly face a double burden of health-related problems, needing to confront the medical problems associated with communicable diseases and injury, as well as those of chronic and non-communicable disease [15]. Emergency medicine is increasingly being recognized globally as a necessary component to healthcare, in order to better address both the acute and chronic health needs of a population [16]. As emergency medicine worldwide becomes more inundated with individuals seeking primary care for non-emergent conditions, understanding what role the specialty plays in an African healthcare framework is important.
The purpose of this study is to characterize Emergency Centre (EC) encounters in a hospital in Mbour, Senegal, through a retrospective review of its EC registry. Emergency centre encounters are defined as visits in which a diagnosis was made and recorded by the EC physician. Our key objectives are to establish a number of emergent versus non-emergent cases in the EC and to examine the extent to which emergent cases were avoidable or preventable.
Methods
Using a retrospective approach, this study examined the EC registry from the Grande Mbour Hospital between June 2014 and October 2014. The registry documented 1268 patients seen in the EC during this period. Mbour, Senegal, is approximately 80 km south of the capital, Dakar. Mbour hospital is a regional medical facility in the Thies region of Senegal. It serves an area of approximately 500 000 people and has approximately 116 inpatient beds, 19 maternity beds, 19 doctors, and approximately 140 staff. The hospital provides both ambulatory and inpatient care. The hospital consists of one main building and a few peripheral buildings, which house the maternity ward, the paediatrics unit, and administrative offices. The Mbour EC is a part of the hospital, which services approximately 20 000 patients per year. The EC can accommodate a maximum of ten patients at any given time. Triage is challenging due to the lack of a standardised triage system. A single physician staffs the EC along with between five to ten nurses.
Nursing staff in the EC completed the registries used in this study. Two medical students conducted the collection of data from the registries. Photos were taken of each page of the registry and then converted to PDF using the application Genius Scan (The Grizzly Labs, Paris, France). The PDFs were then uploaded electronically for data entry. Each page of the registry was numbered and the corresponding PDFs were saved based on this numbering system. The same medical students, assisted by Hospital of Mbour EC staff, entered data on two separate Microsoft Excel (Redmond, WA, USA) charts. The staff assisted the students in clarifying abbreviations and any difficult translations from French to English.
Patient demographic data obtained from the charts included age and gender. Disposition status included discharge, transferred within facility, transferred to surgery, transferred outside of the facility, refused treatment and missing from chart/unknown (note that discharge also included approximately patients who died in the EC). Death registries for the entire hospital are kept separate from the EC registries. The only documentation of death was a separate note on the number of deaths per day during the observation period, however these deaths were not linked to diagnosis or disposition status.
EC encounter categories were coded using the International Statistical Classification of Diseases (ICD-9) as maintained by the World Health Organization. This study utilised an algorithm developed through New York University, the NYU Emergency Department Algorithm, to help classify EC utilisation based on an examination sample of nearly 6000 full EC records in the United States [17]. The rational for using the NYU ED algorithm for this study in Senegal is as follows: 1) It employs globally-used ICD-9 codes 2) It is publically available at no cost 3) It provides an opportunity to replicate EC encounters in other settings including other LMIC settings. Once proof of concept is established, the algorithm can be adapted for further LMIC use.
Applying the NYU ED algorithm
Each ICD-9 diagnosis included in this study was classified using the algorithm as:
-
•
Non-emergent: medical care was not required within twelve hours.
-
•
Emergent but primary care treatable: treatment was required in twelve hours, but could have been provided in a primary care setting.
-
•
Emergent with EC care needed but avoidable/preventable: care was needed within twelve hours however EC level treatment would have been avoidable with appropriate primary care.
-
•
Emergent with EC care needed and not avoidable/preventable: care was needed within twelve hours and the conditional was not avoidable with primary care treatment.
The algorithm also categorised diagnoses of injury, mental health problems, alcohol or substance abuse, or unclassified. According to the algorithm, a single encounter may be classified across more than one NYU Algorithm Categorisation. For example, individuals who were discharged with the final diagnosis of abdominal pain may have presented with stomach pain or chest pain (or possible heart attack), and the categories of: emergent/primary care treatable and EC care needed, not preventable/avoidable are both included. Therefore, in the case of abdominal pain, each case is assigned 67% emergent/primary care treatable and 33% EC care needed, not preventable/avoidable. A second example would be the case of oesophageal reflux, which is categorised as 25% non-emergent and 75% emergent. Other examples that are categorised as both emergent and non-emergent include influenza, headaches, anaemia, urinary tract infections, and acute pharyngitis. Note that while some cases may be distributed across more than one category of the algorithm, no case is double counted.
The diagnoses were categorised by the two medical students, and any diagnostic conflicts were resolved by an attending EC physician in Mbour. Table 1 provides several examples of how each diagnosis was further divided across algorithm categories.
Table 1.
Examples of NYU Algorithm classifications of ICD-9 codes seen at Mbour Hospital.
| NYU Algorithm Categorisation | Example |
|---|---|
| Non-Emergent | Infectious colitis, enteritis, and gastroenteritis |
| Emergent, PC Treatable | Salmonella gastroenteritis |
| EC Care Needed, Preventable/Avoidable | Pulmonary tuberculosis, unspecified |
| EC Care Needed, not Preventable/Avoidable | Obstructive hydrocephalus |
| Injury | Dislocation of knee, unspecified, closed |
| Psychiatric | Simple type schizophrenia, chronic |
| Alcohol | Alcohol abuse, episodic (not seen at hospital) |
| Drug | Cocaine abuse, episodic |
| Unclassified | Urine retention NOS |
Descriptive statistics including means and standard deviations for continuous variables and frequencies, and percentages for categorical variables were employed to assess the demographic characteristics of patients seen in the EC during the observation time and the nature of the encounter based on the algorithm. Encounters were counted as emergent, non-emergent, injury, mental health, or substance use-related if the encounter contained any percentage (>1%) of any category. Descriptive statistics were also employed to describe the distribution of gender and age, and disposition status. All analyses were conducted in SAS 9.4 (SAS Institute Inc., SAS 9.4. Cary, NC). Analyses were performed by the research team with oversight and guidance from the senior author. The ethics committee of the lead author’s institution is an academic medical centre and approved this study. The director of the hospital of MBour also approved this study. All data was kept securely in a locked room and password-protected server.
Results
We included all 1268 cases from the registry. The average age of patients treated in the EC during the observation period was 32.9 years, and the majority of patients were male (n = 681, 53.7%) (Table 2). The majority of patients (n = 760, 60.0%) were discharged from the EC (of which 10, 0.8% were discharged due to death in the EC). Another 97 (7.6%) were transferred to other inpatient units. Approximately 29 (2.3%) were transferred to surgery or to the academic medical centre in the country’s capital, Dakar.
Table 2.
Demographics and transfer status.
| Variable n = 1268 |
Mean (±SD): range | Frequency n (%) |
|---|---|---|
| Age | 32.9 (±22): 2mo-100 yr | |
| Gender | ||
| Male | n = 681 (53.7%) | |
| Female | n = 563 (44.4%) | |
| Unknown | n = 24 (1.9%) | |
| Disposition | ||
| Discharged | n = 760* (60.0%) | |
| Transferred to other inpatient units | n = 97 (7.6%) | |
| Transfer to surgery | n = 29 (2.3%) | |
| Transferred to Dakar | n = 7 (0.6%) | |
| Refused treatment | n = 7 (0.6%) | |
| Disposition missing from chart | n = 368 (29.0%) | |
SD, standard deviation; mo, months; yr, year; *, included patients who died (10 during the observation period).
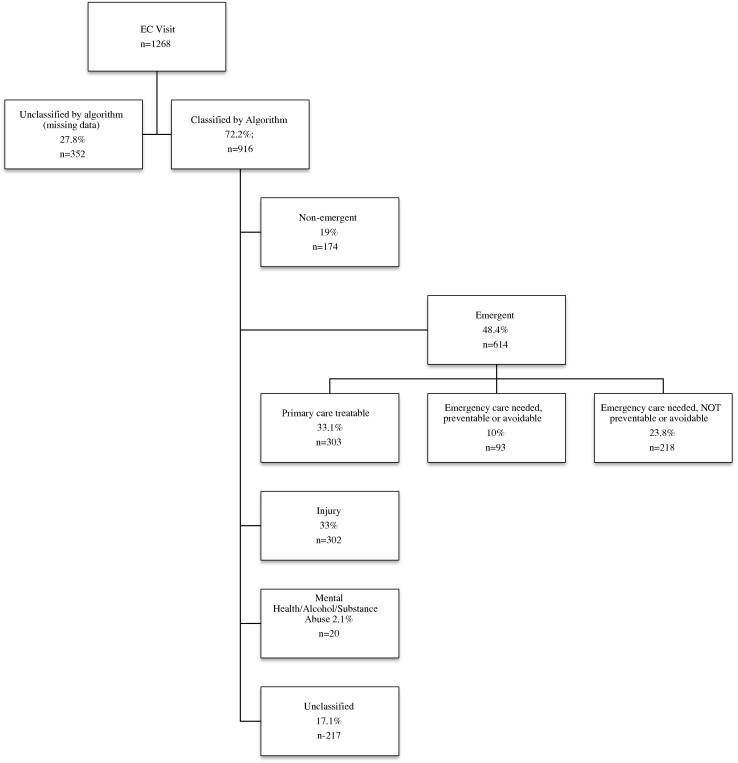
Fig. 1 breaks the encounters into categories falling under emergent or non-emergent. Overall, there were 302 (33%) of encounters that were injury-related, and 174 (19%) were considered non-emergent. Overall, 614 (48.4%) of EC cases were considered emergent. Specifically, 303 cases (33%) were emergent but primary care treatable, 93 cases (7.3%) were emergent but avoidable, and 218 (17.2%) were neither preventable, nor avoidable.
Fig. 1.
Emergent and non-emergent classifications of emergency centre encounters in Mbour, Senegal.
Two different categories of unclassified data are represented in the figure. First, there is unclassified data due to missing data (n = 352, 27.8%), which means that it was not possible to categorise the encounter due to either a missing diagnosis or an inability to translate the chart. A number of cases were not classified because the diagnosis was not entered into the paper registry. The second is data that are complete and corresponds to an ICD-9 code; however, are unclassifiable under the NYU algorithm (n = 217, 17.1%). These including diagnoses of nerve lesions, infections, and a variety of other diseases.
Discussion
This study provides the first description of patients presenting for care to the EC of Mbour hospital. Our findings demonstrate the wide range of illnesses and trauma that the EC must accommodate while balancing the limited resources available in the area. Currently, limited resources make it difficult to properly accommodate, diagnose, and treat the high volume of patients the EC encounters daily. Primary care is not equally distributed or readily accessible in Senegal, and as a result, many patients present to the EC seeking care for non-acute illnesses or diseases that could be managed by routine primary care. This can be a frustrating situation because the physical space in the Mbour EC is highly limited, with patients seeking primary care often occupying a substantial number of the available beds. Emergency medicine is rapidly becoming a globalised entity, but its role in medicine is still difficult to define. Emergency medicine is often interpreted as a medical specialty dedicated to addressing solely life-threatening emergencies [18]. In practice this is often not the case, as the EC sees a large breadth of cases spanning different severities.
Overall, the high incidence of non-emergent cases interspersed with truly emergent encounters highlights the necessity of having trained staff members who are able to effectively triage and manage a diverse array of cases. There are limited numbers of personnel and physical resources to facilitate triage protocols. In Mbour, the EC was staffed solely by physicians and nurses with limited assistance of community or social workers. Nursing staff in Mbour did not have specific training pertaining to EM or triaging protocol. Community and social workers were often involved with the transportation of patients to the EC, and did not have formal training in EMS or triaging skills. This brings into question the ability of the hospital to recruit and train additional personnel who may assist in the triage and administration capabilities of the EC.
As the burden of emergency conditions increases for lower-income countries, there is a push for better training in triage and emergency medical skills [19]. In comparison to Mbour, several other African countries are moving towards using the South African Triage Scale (SATS), which has been found to be an adaptable triage protocol in LMICs [20]. SATS does not rely on computer-based medical records, and has been found to be successful in low resource settings when users are properly trained [21].
Past studies have demonstrated that 90% of global trauma deaths occur in LMICs [20]. The number of injuries in these countries amounts to five million deaths each year, which is equivalent to the number of deaths resulting from HIV/AIDS, malaria, and tuberculosis combined [22]. Economic development is associated with an increasing number of vehicles within a community, and a concomitant increase in traffic-related injuries and morbidities [22]. Our results reflected this finding, as injury was a common EC encounter. A large number of injuries in Mbour were related to vehicle and road incidents. As many Senegalese travel by motorcycle, a variety of foot and lower extremity injuries were documented within the EC registries. It was noted that roads and transportation were not highly regulated within the region and that helmets and other protective gear were rarely worn. Furthermore, cars, carts, and other modes of transportation often had high occupancy, which could increase the risk of vehicle-related accidents. This highlights the critical role that the EC plays in addressing injury-related cases, as well as the potential space for public health intervention.
The EC algorithm category: unclassified, consisted of many complications and symptoms of chronic disease, including diabetic retinopathy, secondary hypertension, neurological symptoms of diabetes, cirrhosis, and unspecified ascites. These findings allude to the notion that Senegal is increasingly facing a double burden of both chronic and acute diseases. While diabetes and hypertension are increasingly being seen in the population, a lack of primary care physicians hinders the ability to address these chronic illnesses [3], [14]. Furthermore, as most health care is paid for out of pocket in Senegal, the high financial burden of chronic disease results in delayed diagnosis and lack of treatment [3].
Interestingly, no alcohol-related cases were present at the Mbour hospital. Among African countries, Senegal is characterised as having a high proportion of abstention from drinking, as well as low rates of heavy drinking among those who consume alcohol [23]. As Senegal is predominately a Muslim country, most individuals do not partake in the use of alcohol or other illicit drugs.
There were several limitations to this study. First, the EC algorithm used to categorise cases is specific to the United States and has not been validated in Senegal. We found that the emergent drug and alcohol categories were non-existent in this population. However, from a clinical perspective, what is considered ambulatory care sensitive or preventable is relevant in the both U.S. and Africa. Second, the EC registries obtained were in paper form and had some illegible and incomplete entries. Furthermore, all of the charts of patients who were seen during the period when the charts were abstracted were not found. Furthermore, although many conditions seen at this hospital may be typical of the region, it is not possible to extenuate the results of this study to be characteristic for Senegal in its entirety. Death registries are separate paper documents from EC registries and we were unable to reconcile these on a case-by-case basis with the EC encounter registries; however, registries showed that there were ten deaths during the observation period, not including those who died after transfer to another unit within the hospital or facility. The inability to classify encounters due to incomplete or missing information in registries was a significant challenge in performing this research. The reasons for missing data were discussed with the director of the Hospital of MBour EC. As the EC is understaffed, there are competing interests (e.g. managing patients in inadequate space), which have led to inconsistent paper record keeping. Paper charts and the lack of a computer also contribute to inconsistent record keeping. The missing data may indeed lead to biases in our analysis. It is possible that charts are less likely to be filled out during high volume episodes such as multiple vehicle accidents. In this case we may be underestimating the number of trauma cases. Additionally, it is possible that charting for non-emergent conditions takes a lesser priority and therefore primary care sensitive conditions that are not emergent are under estimated. Despite the missing data, we believe that this study is valuable in multiple ways: firstly, there is a paucity of data on emergency services in Senegal and other Francophone African countries; secondly, while there is a substantial amount of missing data, there is still a large volume of encounters that represent preventable or ambulatory treatable conditions which warrants attention and further research as to how to increase primary care access and health care seeking behaviours. Lastly, the large amount of missing data sheds light on the need for improved medical record documentation in EC settings including needed resources and training for improved record keeping and the implementation of electronic medical records. While low-cost electronic medical record systems are becoming increasingly available in LMICs, training and positive attitude towards high quality data and chart maintenance is a necessary first step [24]. The equipment, training and a culture of accurate reporting are necessary to maintain medical chart integrity and ultimately improve quality of EC care.
Conclusion
While emergency medicine is still a new and developing specialty in West Africa, it has become an integral component of healthcare within Senegal. As Senegal increasingly encounters the double burden of chronic and acute disease, emergency centres must be equipped to readily treat and manage both emergent and non-emergent encounters until more adequate primary care is available. Physicians and other health care personnel working within this environment should be encouraged to undergo training in both emergent and non-emergent components of care.
We recommend that dedicated needs assessment and resource evaluation studies be conducted within Mbour, Senegal, to establish guidelines for emergency care, as well as how best to utilise resources for emergent and non-emergent encounters. Adapting the EC algorithm to the nuances of Senegalese EC encounters will also allow for more accurate monitoring of the nature of EC visits and the resources needed to address them. However, addressing completeness of EC charts is necessary before adapting the algorithm. It is critical that recordkeeping become a more standardised process within the hospital to improve quality of care. Given that the hospital of Mbour may not have the resources to acquire and maintain new electronic medical record equipment, training and updated guidelines regarding use of paper documentation could help eliminate incomplete EC encounter documentation.
Conflict of interest
The authors declare no conflict of interest.
Dissemination of results
Results from this study were shared with physicians and healthcare workers at the Grande Mbour l’Hopital.
Author contribution
RB and FF conceived the original idea. JM and OS collected and translated the data. RB carried out analysis of data. JM and RB prepared the manuscript. All authors revised it critically for important intellectual content, approved the version to be published and agreed to be accountable for all aspects of the work.
Footnotes
Peer review under responsibility of African Federation for Emergency Medicine.
Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.afjem.2017.05.010.
Appendix A. Supplementary data
References
- 1.Diene M. Inequalities in the context of structural transformation: the case of Senegal. Development. 2014;57(3–4):540–546. [Google Scholar]
- 2.Senegalese Survey on the Perception of Poverty (SSPP). Dakar, Senegal: National Agency for Statistics and Demography; 2011.
- 3.Séne L.M., Cissé M. Catastrophic out-of-pocket payments for health and poverty nexus: evidence from Senegal. Int J Health Econ Manage. 2015;15(3):307–328. doi: 10.1007/s10754-015-9170-4. [DOI] [PubMed] [Google Scholar]
- 4.Smith J., Haile-Mariam T. Priorities in global emergency medicine development. Emerg Med Clin North Am. 2005;23:11–29. doi: 10.1016/j.emc.2004.09.012. [DOI] [PubMed] [Google Scholar]
- 5.House D., Nyabera S.L., Yusi K. Descriptive study of an emergency centre in Western Kenya: challenges and opportunities. Afr J Emergency Med. 2014;4(1):19–24. [Google Scholar]
- 6.Periyanayagam U., Dreifuss B., Hammerstedt H. Acute care needs in a rural Sub-Saharan African Emergency Centre: a retrospective analysis. Afr J Emergency Med. 2012 Dec;2(4):151–158. [Google Scholar]
- 7.Levine A.C., Presser D.Z., Rosborough S. Understanding barriers to emergency care in low-income countries: view from the front line. Prehospital Disaster Med. 2007 Oct;22(5):467–470. doi: 10.1017/s1049023x00005240. [DOI] [PubMed] [Google Scholar]
- 8.Razzak J.A., Kellermann A.L. Emergency medical care in developing countries: is it worthwhile? Bull World Health Organ. 2002;80(11):900–905. [PMC free article] [PubMed] [Google Scholar]
- 9.Kobusingye OC, Hyder AA, Bishai D, et al. Disease Control Priorities in Developing Countries. World Bank; 2006. Available from: http://www.ncbi.nlm.nih.gov/books/NBK11744/.
- 10.Mould-Millman N.-K., Dixon J.M., Sefa N. The state of emergency medical services (EMS) systems in Africa. Prehospital Disaster Med. 2017 Feb;23(1):1–11. doi: 10.1017/S1049023X17000061. [DOI] [PubMed] [Google Scholar]
- 11.Nielsen K., Mock C., Joshipura M. Assessment of the status of prehospital care in 13 low- and middle-income countries. Prehospital Emergency Care. 2012 Jun 6;16(3):381–389. doi: 10.3109/10903127.2012.664245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hardcastle T.C., Brysiewicz P. Trauma care in South Africa: from humble beginnings to an afrocentric outreach. Int Emergency Nurs. 2013 Apr;21(2):118–122. doi: 10.1016/j.ienj.2012.05.002. [DOI] [PubMed] [Google Scholar]
- 13.Peden M., Toroyan T., Harvey A. World Health Organization; Geneva: 2009. Global status report on road safety. [Google Scholar]
- 14.Abegunde D.O., Mathers C.D., Adam T. The burden and costs of chronic diseases in low-income and middle-income countries. Lancet. 2007;370:1929–1938. doi: 10.1016/S0140-6736(07)61696-1. [DOI] [PubMed] [Google Scholar]
- 15.Mathers C, Shibuya K, Stein C. Chapter 1: Global health: today’s challenges. In: The World Health Report 2003: shaping the future. Geneva: World Health Organization; 2003. p. 1–22.
- 16.Anderson P.D., Suter R.E., Mulligan T. World health assembly resolution 60.22 and its importance as a health care policy tool for improving emergency care access and availability globally. Ann Emergency Med. 2012 Jul;60(1):35–44.e3. doi: 10.1016/j.annemergmed.2011.10.018. [DOI] [PubMed] [Google Scholar]
- 17.ED Algorithm. New York University Center for Health and Public Service Research; 2000. Available from: http://wagner.nyu.edu/faculty/billings/nyued-background.
- 18.Anderson P. The globalization of emergency medicine and its importance for public health. Bull World Health Organ. 2006;84(10):835–839. doi: 10.2471/blt.05.028548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stewart B., Khanduri P., McCord C. Global disease burden of conditions requiring emergency surgery. Br J Surg. 2014 Jan;101(1):e9–e22. doi: 10.1002/bjs.9329. [DOI] [PubMed] [Google Scholar]
- 20.The South African Triage Scale (SATS) : EMSSA; 2004. Available from: http://emssa.org.za/sats/.
- 21.Gyedu A., Agbedinu K., Dalwai M. Triage capabilities of medical trainees in Ghana using the South African triage scale: an opportunity to improve emergency care. Pan Afr Med J. 2016;24 doi: 10.11604/pamj.2016.24.294.8728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gosselin R.A., Spiegel D.A., Coughlin L.G. Injuries: the neglected burden in developing countries. Bull World Health Organ. 2009;87:246. doi: 10.2471/BLT.08.052290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Clausen T., Rossow I., Naidoo N. Diverse alcohol drinking patterns in 20 African countries. Addiction. 2009;104(7):1147–1154. doi: 10.1111/j.1360-0443.2009.02559.x. [DOI] [PubMed] [Google Scholar]
- 24.Pirkle C., Dumont A., Zunzunegui M. Medical recordkeeping, essential but overlooked aspect of quality of care in resource-limited settings. Int J Qual Health Care. 2012 Jul 13;24(6):564–567. doi: 10.1093/intqhc/mzs034. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.