Introduction
Paratesticular adult rhabdomyosarcoma (RMS) is a rare pathology that has the specificity of being more aggressive than that of the child. It has high malignant potential, quick spread and requires prompt and adequate care. In this context we report the case of an adult paratesticular RMS. We aimed to describe its clinical features and natural history.
Case presentation
A 21-year-old man noticed a right paratesticular mass on June 2017. On clinical examination, the patient had two fixed and painless right lymphadenopathies, measuring 3 × 2 and 2 × 2 cm. The testicular ultrasound showed a tissue mass centered on the right testis of 86 mm long axis extending to the spermatic cord. The Tumor was staged T2bN1M0 according to TNM classification. A right orchiectomy has been practiced on October 2017. The macroscopic examination showed a tumor mass of gelatinous aspect, remodeled by the necrosis, measuring 7 × 4 cm. The tumor was contiguous to the epididymis and testes without invading them and extending to the spermatic cord. On microscopic findings, the tumor corresponded to a poorly differentiated malignant tumor growth made of a rounded or star-shaped mesenchymal cell range with a scanty cytoplasm and rounded or ovoid dense nuclei. These cells are arranged on a myxoid background. There is an alternation of cellulite zones very densely with sometimes per vascular condensation and rather loose zones. These areas alternate with some foci of elongated cells with a more abundant and more acidophilic cytoplasm. There was rarely aspects of cytoplasmic striations. There were 40 mitoses/10 large fields. The tumor was remodeled by the large necrotic areas that account for less than 50% of the tumor. It encompassed without infiltrating the epididymis and testicular parenchyma. It infiltrated the hypoderm while the dermis and the epidermis were respected. The limit of excision of the cord was healthy. Immunohistochemistry revealed negativity of PS100, CD4 and MDM2. There was no evidence of cytokeratin staining. Myogenin, that is a specific marker of rhabdomyosarcoma, gave intense and heterogeneous nuclear staining of tumor cells. Desmin also gave a positive mark. These pathological findings concluded to a grade 3 embryonic rhabdomyosarcoma according to the histological grade system of the French Federation of Comprehensive Cancer Centers (FNCLCC) grading. Postoperative imaging showed external iliac lymphadenopathy of 22 × 10 mm as well as multiple right inguinal ganglia. The largest one was 10 × 8 mm. According to the Risk Stratification for European Soft tissue sarcoma study group, the patient was classified into the subgroup F (high risk). The file was discussed in a multidisciplinary consultation meeting. The decision was to make 6 cycles of Ifosfamide, Oncovin and Actinomycin based chemotherapy (IVA) as well as radiotherapy of the ganglionic areas at a dose of 41.4 Gy with a boost of 9 Gy. However, on February 2018, after completing the 6 cycles of chemotherapy, the patient presented ganglionic progression. He is currently proposed for second-line palliative chemotherapy with Adriamycin.(Fig. 1, Fig. 2, Fig. 3)
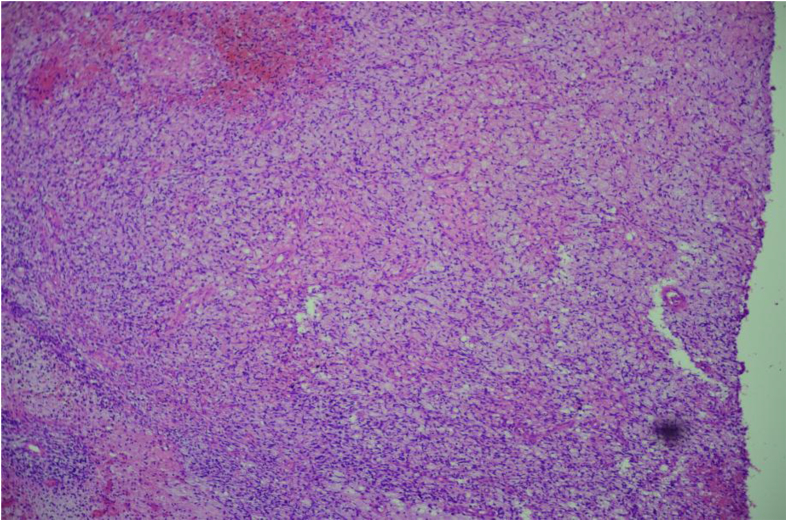
Fig. 1.
Photomicrograph of a histological slide showing primitive small round blue cells. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
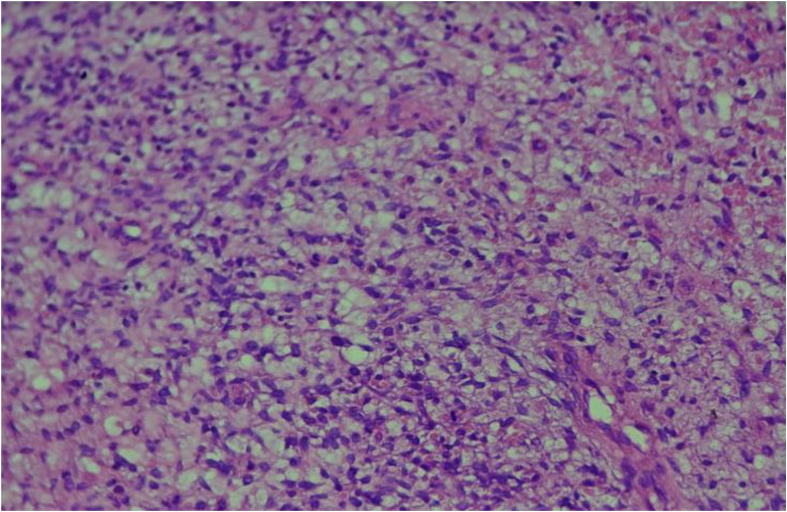
Fig. 2.
A poorly differentiated malignant tumor growth made of a rounded or star-shaped mesenchymal cell range with a scanty cytoplasm and rounded or ovoid dense nuclei.
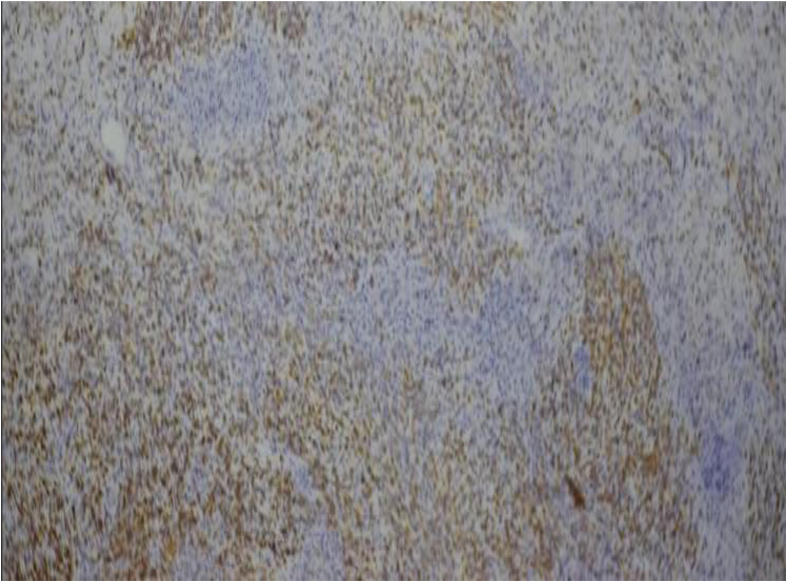
Fig. 3.
Cells are arranged on a myxoid background.
Discussion
Paratesticular localization of RMS represents 7% of all locations. This pathology concerns mainly children and adolescent with a first peak of incidence between 2 and 5 years and a second less common peak on young adolescents that age is less than 20 years old. Adult testicular RMS is a rare and more aggressive entity.
RMS develop mainly where there is skeletal muscle but can appear anywhere. It derives from mesenchymal cells in their different phase of differentiation. Its dissemination concerns essentially lymph nodes (Iliac and para-aortic). It has a lower hematological spread rate (lung, liver, bone and bone marrow: 20%).
Clinically it presents as a unilateral painless and swelling inguinal mass that can be mistaken and considered as a benign mass.
At the opposite of other localizations, the biopsy of paratesticular RMS is prohibited because of the high risk of dissemination. The diagnosis will then be made on the orchiectomy piece.
Child RMS treatment is well established whereas the management of adult remains unclear because of its scarcity. From the data of the literature the treatment of choice in case of local disease seems to be a radical orchiectomy followed by a concomitant chemotherapy (CCT) with radiotherapy (RT).
The role of retro peritoneal lymph node dissection (RPLND) is controversial. Some like Ferrari et al. consider that it is not necessary because of the low rate of retro peritoneal lymph node invasion as well as the demonstrated role of CCT in eradicating micro metastatic disease.1
Some consider that it is first necessary for a diagnostic purpose since the sensitivity of the CT scan in the detection of lymph node invasion is not very sensitive. Others have shown benefit in terms of survival: Hamilton et al. demonstrated that CLRPsignificantly improved overall survival (OS) at 5 years In 111 patients aged from 10 to 20 years (92% versus 64%, p = 0.003).2
The role of CCT with RT in children is well demonstrated in terms of OS and progression-free survival (PFS). In the adult population it remains discussed. Hawkins et al. did not find any benefit in patients over than 21 years old. Ferrari et al. Have demonstrated its role as well in terms of PFS as OS in 171 adults with RMS (at any location). The effective drugs were similar as those children (Vincristine, Dactinomycin, Cyclophosphamide, Adriamycin, Epirubicin and Ifosfamide). This benefit was significant in the case of advanced stage and ganglionic invasion with an overall response rate identical to that of children (85%).3
The prognosis of adult para testicular RMS is darker than that of children. It has a high malignant potential with a greater capacity for local and distant recurrence (5-year PHC rate of 28% (versus 40% in children).1, 2, 3
Conclusions
Adult para testicular RMS is an infrequent disease. Its therapeutic management is not yet well established and is currently based on that of the child. Given its high malignant potential it is mandatory to start treatment as soon as possible. The prognosis remains reserved and is characterized by a high risk of recurrence and metastatic spread.
Contributor Information
Amina Mokrani, Email: aidamokrani@yahoo.fr.
Fatma Guermazi, Email: fatmaguermazi21@gmail.com.
Khedija Meddeb, Email: Khedijameddeb@gmail.com.
Yosra Yahyaoui, Email: yosyahyaoui@gmail.com.
Feriel Letaief, Email: feryel.ksontini@gmail.com.
Azza Gabsi, Email: azza_g86@yahoo.fr.
Mouna Ayadi, Email: mounaayadi28@gmail.com.
Nesrine Chraiet, Email: nesrinechraiet@gmail.com.
Henda Raies, Email: henda.rais@yahoo.fr.
Amel Mezlini, Email: amel.mezlini@rns.tn.
References
- 1.Ferrari A., Casanova M., Massimino M., Luksch R., Piva L., Fossati-Bellani F. The management of paratesticular rhabdomyosarcoma: a single institutional experience with 44 consecutive children. J Urol. 1998;159:1031–1034. doi: 10.1016/s0022-5347(01)63830-8. [DOI] [PubMed] [Google Scholar]
- 2.Hamilton E.C., Miller C.C., Joseph M., Huh W.W., Hayes–Jordan A.A., Austin M.T. Retroperitoneal lymph node staging in paratesticular rhabdomyosarcoma—are we meeting expectations? J Surg Res. 2018 Apr 1;224:44–49. doi: 10.1016/j.jss.2017.11.051. [DOI] [PubMed] [Google Scholar]
- 3.Hawkins W.G., Hoos A., Antonescu C.R., Urist M.J., Leung D.H. Clinicopathologic analysis of patients with adult rhabdomyosarcoma. Cancer. 2001;91:794–803. [PubMed] [Google Scholar]